Abstract
Background
Patients with chronic diseases likely develop severe 2019 coronavirus disease (COVID-19). However, little is known about the effects of COVID-19 on patients with neurological disorders. We conducted a systematic review to evaluate the severity of COVID-19 and its effect on neurological symptoms in patients with preexisting neurological disorder and COVID-19.
Methods
We searched the MEDLINE (PubMed) and medRxiv databases for reports of patients with both preexisting neurological disorders and COVID-19. Studies reporting data on changes in the symptoms of preexisting neurological disorders and/or the severity of COVID-19 were included.
Results
Twenty-six articles with 2278 patients with preexisting neurological disorder and COVID-19 were identified. Of 232 patients, 74 (31.9 %) showed exacerbation of preexisting neurological symptoms of dementia (55/92; 59.5 %), Parkinson’s disease (10/17; 58.8 %), epilepsy (1/1; 100 %), and unspecified neurological disorders (8/106; 7.5 %). Of 2168 patients, 478 (22.0 %) showed severe COVID-19 course. These included patients with cerebrovascular disease (86/445; 19.3 %), dementia (70/316; 22.2 %), Parkinson’s disease (25/214; 11.7 %), multiple sclerosis (28/71; 39.4 %), spinal cord injury (5/7; 71.4 %), epilepsy (10/98; 10.2 %) and unspecified neurological disorders (254/1011; 25 %).
Conclusions
Patients with preexisting neurological disorders and COVID-19 may develop exacerbation of neurological symptoms and severe COVID-19. Clinicians should be aware of the risk of symptom exacerbation and severe COVID-19 in patients with preexisting neurological disease and should focus on the prevention and early care of COVID-19.
Keywords: COVID-19, Neurological disorder, Neurology, Epilepsy, Systematic, Review
1. Introduction
Coronavirus disease (COVID-19) was first reported in China in December 2019 and has rapidly spread around the world. COVID-19 is one of the leading causes of critical pneumonia and death worldwide. Typically, 14–15 % of patients with COVID-19 develop severe pneumonia and 1.5–2.3 % die [1,2]. Risk factors for severe COVID-19 include cardiovascular disease, diabetes mellitus, hypertension, and old age [3].
As for patients with chronic neurological disorder, a few cohort studies have reported that patients with preexisting neurological disorders who contracted COVID-19 developed more severe clinical symptoms and worse outcomes, compared to the general population [4,5]. In addition, some patients with neurological disorders such as Parkinson’s disease and dementia who developed COVID-19 had a worsening of preexisting neurological symptoms [6,7].
However, the overall severity of COVID-19 and the changes in neurological symptoms in patients with preexisting neurological disorders and COVID-19 are unknown due to limited reports (few case reports or small cohort studies). Therefore, we conducted a systematic review to evaluate the exacerbation of neurological symptoms and the severity of COVID-19 in patients with preexisting neurological disorders and COVID-19.
2. Material and methods
A systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [8]. This review protocol was not formally registered. The MEDLINE (accessed from PubMed) and medRxiv databases were searched systematically on May 22, 2020. In PubMed, the following key words (in the title/abstract) were used: (“COVID-19″ OR “Coronavirus” OR “SARS-CoV-2″ OR “2019-nCoV”) AND (“Neurology” OR “Neurologic” OR “Neurological” OR “Neuropathy” OR “Brain” OR “Spine” OR “Stroke” OR “Nerve” OR “Epilepsy” OR “Parkinson’s disease” OR “Dementia” OR “Brain tumor” OR “Multiple Sclerosis” OR “Movement disorder” OR “Headache” OR “Tremor” OR “Amyotrophic lateral sclerosis” OR “Dystonia”)”. In medRxiv, the number of search terms that can be used is limited; therefore, the following key words were used: (“COVID 19″ OR “SARS CoV 2″) AND (“Neurologic” OR “Stroke” OR “Epilepsy” OR “Parkinson” OR “Dementia” OR “Multiple sclerosis”). The aforementioned neurological diseases were selected from among the chronic neurological diseases with a high prevalence [9,10].
We included studies based on the following criteria: (1) those reporting patients who had preexisting neurological disorders and COVID-19; (2) those that documented the severity of COVID-19 and/or changes in preexisting neurological symptoms; and (3) original reports such as case reports, letters, case series, or cohort studies. Case reports were included because so few large population-based studies of patients with preexisting neurological disorders and COVID-19 are available. We defined a severe case as a patient with severe/critical pneumonia or who had been admitted to the intensive care unit. We defined exacerbation as exacerbation of preexisting neurological disease-related symptoms. We excluded studies written in languages other than English. We also excluded studies that only included patients who were critically ill or deceased.
Two reviewers (TK and NK) independently screened the titles and abstracts. After screening, a reviewer (TK) assessed the full texts of the selected articles and included those that met the inclusion criteria. Any disagreements were resolved by discussions between the reviewers (TK and NK).
3. Results
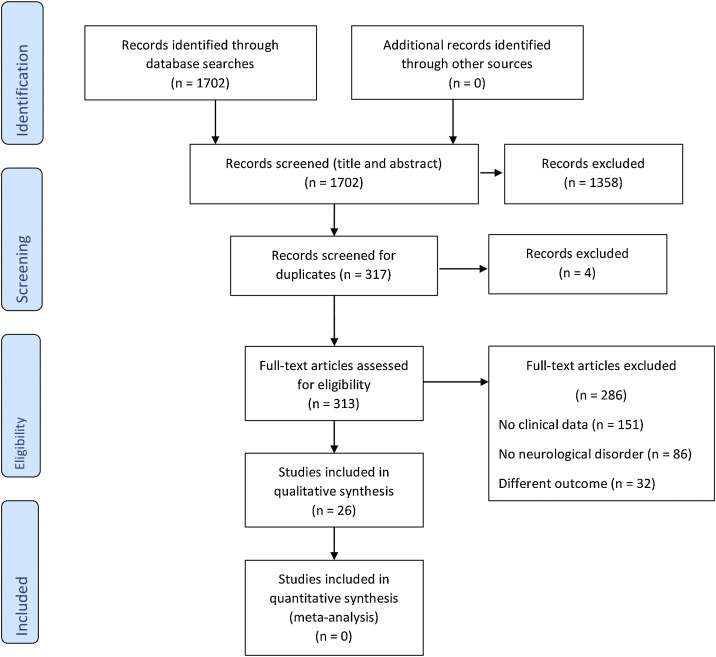
A total of 1702 studies were retrieved (866 papers from MEDLINE and 836 papers from medRxiv) on May 22, 2020. After title and abstract screening and duplicate removal, 313 studies were identified. The full-text screening of these studies led to the exclusion of 286 that did not meet the inclusion criteria. The remaining 26 studies were identified as eligible to be reviewed [6,7,[11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34]]. Fig. 1 outlines the selection process.
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram of this review.
Table 1 lists the characteristics of the included articles. A total of 2278 patients with preexisting neurological disorder and COVID-19 were included. The neurological disorders included cerebrovascular disease, Parkinson’s disease, multiple sclerosis and related disorders, aquaporin-4 (AQP-4)-positive neuromyelitis optica spectrum disorder (NMOSD), dementia and cognitive disorder, epilepsy, spinal cord injury, systemic atrophy, myelopathy, intracranial mass, and unspecified neurological disorders. Since the selected articles did not always report both the exacerbation of neurological symptoms and severity of COVID-19, the patients were divided into two groups: 232 patients with preexisting neurological disorders and COVID-19 for whom the exacerbation of neurological symptoms was reported, and 2168 patients with preexisting neurological disorder and COVID-19 for whom the severe COVID-19 course was reported. Of the 232 patients in the first group, 74 (31.9 %) showed an exacerbation of preexisting neurological symptoms, including patients with dementia (55/92; 59.5 %), Parkinson’s disease (10/17; 58.8 %), epilepsy (1/1; 100 %), and unspecified neurological disorders (8/106; 7.5 %), as shown in Table 2 . Of the 2168 patients in the second group, 478 (22.0 %) exhibited a worsening of COVID-19 severity. These included patients with cerebrovascular disease (86/445; 19.3 %), dementia (70/316; 22.2 %), Parkinson’s disease (25/214; 11.7 %), multiple sclerosis (28/71; 39.4 %), epilepsy (10/98; 10.2 %), spinal cord injury (5/7; 71.4 %), and unspecified neurological disorders (254/1011; 25 %), as shown in Table 3 .
Table 1.
Patients with neurological disorders and COVID-19.
| Author [Reference] | Study design | Neurological disorder, No. | Age (mean ± SD) | Male (%) | Diagnosis of COVID-19 | Neurological disorder, No. | Exacerbation of preexisting neurological symptoms and the severity of COVID-19 No/All neurological disease (%) |
|---|---|---|---|---|---|---|---|
| Rejdak et al [11] | Case report | 27 | NA | 45 | RT-PCR | Multiple sclerosis 15, Parkinson's disease 5, cognitive impairment 7 | Exacerbation of preexisting neurological symptoms 0/22 (0), Severe 0/22 (0) |
| Filatov et al [12] | Case report | 1 | 74 | 100 | Unspecified test for COVID-19 | Stroke and Parkinson’s disease 1 | Severe 1/1 (100) |
| Beyrouti et al [13] | Case report | 1 | 61 | 100 | RT-PCR | Stroke 1 | Exacerbation of preexisting neurological symptoms 0/1 (0), Severe 0/1 (0) |
| Wang et al [14] | Retro | 4 | NA | NA | RT-PCR | Cerebrovascular disease 4 | Severe 2/4 (50) |
| Oxley et al [15] | Case report | 1 | 49 | 100 | Unspecified test for COVID-19 | Stroke 1 | Severe 0/1 (0) |
| Oliver et [16] | Case report | 1 | 62 | 0 | RT-PCR | Transient ischemic attack 1 | Exacerbation of preexisting neurological symptoms 0/1 (0), Severe 0/1 (0) |
| Vollono et al [17] | Case report | 1 | 78 | 0 | RT-PCR | Epilepsy (post HSV-1 encephalitis) 1 | Exacerbation of preexisting neurological symptoms 1/1 (100): status epilepticus 1, Severe 0/1 (0) |
| Novi et al [18] | Case report | 1 | 58 | 100 | RT-PCR | Multiple sclerosis 1 | Exacerbation of preexisting neurological symptoms 0/1 (0), Severe 0/1 (0) |
| Suwanwongse et al [19] | Case report | 1 | 31 | 100 | PCR | Multiple sclerosis 1 | Exacerbation of preexisting neurological symptoms 0/1 (0), Severe 0/1 (0) |
| Gemcioglu et al [20] | Case report | 1 | 31 | 100 | PCR | Multiple sclerosis 1 | Exacerbation of preexisting neurological symptoms 0/1 (0), Severe 0/1 (0) |
| Hughes et al [21] | Case report | 74 | 42.9 (23−59) | 28 | Unspecified test for COVID-19 | Multiple sclerosis 74 (relapsing forms 22, progressive forms 12, not reported 40) | Severe 28/57 (49), Not reported severity 17 |
| Nie et al [22] | Retro | 3 | NA | NA | RT-PCR | Cerebrovascular atherosclerosis 3 | Severe 2/3 (67) |
| Rodriguez et al [23] | Retro | 7 | 68 (34−75) | 71 | RT-PCR | Spinal cord injury 7 (Cervical 5, Thoracic 2. Tracheostomy 4. Need to remove respiratory secretions 2/4) | Severe 5/7 (71) |
| Liao et al [24] | Retro | 4 | NA | NA | RT-PCR | Cerebrovascular disease 4 | Severe 1/4 (25) |
| Bruce et al [25] | Retro | 79 | NA | NA | RT-PCR | Stroke 79 | Severe 19/79 (24) |
| Yin et al [26] | Retro | 106 | 72.7 (±11.8) | 60 | RT-PCR | Cerebral infarction 81, Dementia 20, Acute cerebral infarction 10, Cerebral hemorrhage 5, Intracranial mass lesions 4, Epilepsy 3, Parkinson’s disease 2, and Myelopathy 1 | Exacerbation of preexisting neurological symptoms 8/106 (8), Severe 59/106 (56) |
| Ji et al [27] | Retro | 967 | NA | NA | RT-PCR | Parkinson's disease and movement disorder 209, Dementia and degenerative disease 206, Stroke and Transient cerebral ischemia 349, Epilepsy 97, Systemic atrophy 5, Multiple sclerosis 1 | Severe 162/967 (17) |
| Haimovich et al [28] | Retro | 356 | NA | NA | PCR | Neurologic disorders 356 | Severe 36/356 (10) |
| Berekashvili et al [29] | Retro | 1 | 70−80 | 0 | RT-PCR | Cerebral vascular accident 1 | Severe 1/1 (100) |
| Kim et al [30] | Retro | 548 | NA | NA | Unspecified test for COVID-19 | Neurologic diseases 548 | Severe 158/548 (29) |
| Creed et al [31] | Retro | 1 | 59 | 0 | PCR | Aquaporin-4-positive neuromyelitis optica spectrum disorder 1 | Exacerbation of preexisting neurological symptoms 0/1 (0), Severe 0/1 (0) |
| Beach et al [32] | Case series | 3 | 3 | PCR | Major neurocognitive disorder 1, dementia 1, and dementia with Levy 1 | Exacerbation of preexisting neurological symptoms 0/3 (0), Severe 1/3 (33) | |
| Morassi et al [33] | Case series | 2 | 76 | 50 | RT-PCR | Stroke 1, Transient ischemic attack 1 | Severe 2/2 (100) |
| Hainque et al [34] | Case report | 2 | 78 (73−83) | 50 | RT-PCR | Parkinson’s disease 2 | Exacerbation of preexisting neurological symptoms 2/2 (100): motor symptoms 2, fall 1 |
| Antonini et al [6] | Retro | 10 | 78.3 (61−94) | 60 | NA | Parkinson’s disease 10 | Exacerbation of preexisting neurological symptoms 8/10 (80): motor symptoms 2/10 (20), fall 3/10 (30) nonmotor symptoms 8/10 (80) |
| Bianchetti et al [7] | Retro | 82 | 82.6 (±5.3) | 43 | RT-PCR | Dementia 82 | Exacerbation of preexisting neurological symptoms 55/82 (67): delirium 55, functional status worsening 46, behavioral symptoms 9 |
RT: Reverse transcription. PCR: Polymerase chain reaction. Retro: Retrospective cohort study. NA: Not available.
Table 2.
Exacerbation of preexisting neurological symptoms.
| Disease | All patients, No. | No exacerbation, No. | Exacerbation, No (%) |
|---|---|---|---|
| All Neurological diseases | 232 | 159 | 74 (31.9) |
| Cerebrovascular disease | 2 | 0 | 0 (0.0) |
| Dementia | 92 | 37 | 55 (59.5) |
| Parkinson's disease | 17 | 7 | 10 (58.8) |
| Multiple sclerosis | 13 | 13 | 0 (0.0) |
| AQP-4-positive NMOSD | 1 | 1 | 0 (0.0) |
| Epilepsy | 1 | 0 | 1 (100.0) |
| Not specified neurological disorders | 106 | 98 | 8 (7.5) |
AQP-4: Aquaporin-4. NMOSD: neuromyelitis optica spectrum disorder.
Table 3.
Severity of COVID-19.
| All patients, No. | No severe, No | Severe, No (%) | |
|---|---|---|---|
| All Neurological diseases | 2168 | 1690 | 478 (22.0) |
| Cerebrovascular disease | 445 | 359 | 86 (19.3) |
| Dementia | 316 | 246 | 70 (22.2) |
| Parkinson's disease | 214 | 189 | 25 (11.7) |
| Multiple sclerosis | 71 | 43 | 28 (39.4) |
| AQP-4-positive NMOSD | 1 | 0 | 0 (0.0) |
| Epilepsy | 98 | 88 | 10 (10.2) |
| Spinal cord injury | 7 | 2 | 5 (71.4) |
| Not specified neurological disorders | 1011 | 757 | 254 (25) |
AQP-4: Aquaporin-4. NMOSD: neuromyelitis optica spectrum disorder.
4. Discussion
In this systematic review, our findings suggest that COVID-19 may increases the risk of a worsening of neurological symptoms in patients with preexisting neurological disorders. In addition, our results indicate that patients with preexisting neurological disorders and COVID-19 may likely develop severe COVID-19. To our knowledge, this is the first systematic review to demonstrate the exacerbation of neurological symptoms and the severity of COVID-19 in patients with preexisting COVID-19 and neurological disorders.
We found that 31.9 % of patients with preexisting neurological disorders and COVID-19 experienced a worsening of neurological symptoms. In particular, approximately 60 % of patients with Parkinson’s disease or dementia had an exacerbation of preexisting neurological symptoms. In general, the most common cause of symptom exacerbation in patients with Parkinson’s disease was infection (25.6 %), followed by anxiety (18.6 %), medication errors (13.9 %), and poor adherence to the treatment regimen (13.9 %) [35]. Moreover, symptoms of COVID-19 and changes in the environment, such as hospitalization, may interrupt the scheduled intake of medication, resulting in the deterioration of symptoms. In addition, an infection induces the production of systemic and central nervous system cytokines and prostaglandins that cause acute cognitive declines and delirium in patients with dementia [36]. The presence of cytokines and monokines in the brain has been reported in patients with severe acute respiratory syndrome coronavirus [37]. Consequently, COVID-19 may trigger a cognitive decline or delirium in patients with dementia. Although the number of patients with epilepsy is small, they exhibited an exacerbation in symptoms. The association between seizures and COVID-19 has not been clearly determined; however, infection is a common precipitating factor for the development of seizures in patients with epilepsy [[38], [39], [40]]. Thus, COVID-19 may worsen seizure control in patients with epilepsy. In contrast, patients with multiple sclerosis and related diseases did not exhibit neurological symptom exacerbations in our study. On the other hand, a previous cohort study reported that viral infections were associated with temporal exacerbations in the symptoms of approximately 9% of patients with multiple sclerosis [41]. Our systematic review may not have detected symptom exacerbations in such patients due to the small sample size.
We found that 22.0 % of patients with preexisting neurological disorders and COVID-19 developed severe COVID-19. The frequency of severe COVID-19 among these patients was greater than that of patients in general population studies (22.0 % vs 14.2–15.7 %) [1,2]. Among patients with cerebrovascular disease or dementia, who comprised the majority of patients, 19.3 % and 22.2 %, respectively, developed severe COVID-19. This may be because such patients have risk factors for severe COVID-19, including old age, diabetes mellitus, and hypertension [3]. In patients with multiple sclerosis, the percentage of patients in whom COVID-19 severity increased was as high as 39.4 %. Comorbidities, obesity, age, and progressive forms of multiple sclerosis have been reported as risk factors for severe COVID-19 in patients with preexisting multiple sclerosis [42]. Although the patients with multiple sclerosis in our study were relatively young (23–59 years), they may have had other comorbidities and progressive forms of the disorder. The severity of COVID-19 also increased in 71.4 % of patients with spinal cord injury, although this population was small. Difficulty with spontaneous breathing and clearing respiratory secretions may worsen pneumonia in patients with spinal cord injury. In contrast, the frequency of patients with Parkinson’s disease who experienced increased COVID-19 severity was low, compared to the general population (11.7 % vs 14.2–15.7 %) [1,2]. This low percentage was inconsistent with the frequencies in patients with other predominantly elderly neurological diseases, such as dementia and stroke. In patients with epilepsy, the percentage of patients with severe COVID-19 was low (10.2 %). Although the mean age of these patients is unknown, the studies may have included pediatric patients with epilepsy.
Our study had several limitations. First, most of the included studies were case reports or small cohort studies. Consequently, there may be large differences in the clinical settings between these reports. Second, the studies included in the systematic review may have been subject to selection and presentation bias. For example, severe or complicated cases may have been more likely to be published. Third, mild exacerbation of preexisting neurological symptoms might have been missed and unreported. Fourth, patients with unspecified neurological disorders were reported. Finally, the criterion of severity varied slightly across studies. Therefore, the criteria in our study may not have been completely accurate and uniform.
In conclusion, our results suggest that patients with preexisting neurological disorders and COVID-19 may experience a worsening of neurological symptoms and may likely develop severe COVID-19. Clinicians should be aware of the risks of an exacerbation of neurological symptoms and an increase in COVID-19 severity in patients with preexisting neurological diseases, and should focus on the prevention and early care of COVID-19. Further detailed retrospective and prospective large-cohort studies are needed to confirm the risk of an exacerbation of neurological symptoms and the clinical outcomes in patients with COVID-19 and preexisting neurological disorders.
CRediT authorship contribution statement
Takafumi Kubota: Conceptualization, Data curation, Investigation, Methodology, Software, Writing - original draft. Naoto Kuroda: Conceptualization, Investigation, Methodology, Writing - review & editing.
References
- 1.Guan W., Ni Z., Hu Y.Y.H., Liang W., Ou C., He J., Liu L., Shan H., Lei C., Hui D.S.C., Du B., Li L., Zeng G., Yuen K.Y., Chen R., Tang C., Wang T., Chen P., Xiang J., Li S., Wang J.L.J.M., Liang Z., Peng Y., Wei L., Liu Y., Hu Y.Y.H., Peng P., Wang J.L.J.M., Liu J., Chen Z., Li G., Zheng Z., Qiu S., Luo J., Ye C., Zhu S., Zhong N. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L., Cookingham J., Coppa K., Diefenbach M.A., Dominello A.J., Duer-Hefele J., Falzon L., Gitlin J., Hajizadeh N., Harvin T.G., Hirschwerk D.A., Kim E.J., Kozel Z.M., Marrast L.M., Mogavero J.N., Osorio G.A., Qiu M., Zanos T.P. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA - J. Am. Med. Assoc. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qin C., Zhou L., Hu Z., Yang S., Zhang S., Chen M., Yu H., Tian D.-S., Wang W. Clinical characteristics and outcomes of COVID-19 patients with a history of stroke in Wuhan, China. MedRxiv. 2020 doi: 10.1101/2020.04.24.20078063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benussi A., Pilotto A., Premi E., Libri I., Giunta M., Agosti C., Alberici A., Baldelli E., Benini M., Bonacina S., Brambilla L., Caratozzolo S., Cortinovis M., Costa A., Piccinelli S.C., Cottini E., Cristillo V., Delrio I., Filosto M., Gamba M., Gazzina S., Gilberti N., Gipponi S., Imarisio A., Invernizzi P., Leggio U., Leonardi M., Liberini P., Locatelli M., Masciocchi S., Poli L., Rao R., Risi B., Rozzini L., Scalvini A., Schiano di Cola F., Spezi R., Vergani V., Volonghi I., Zoppi N., Borroni B., Magoni M., Pezzini A., Padovani A. Clinical characteristics and outcomes of inpatients with neurologic disease and COVID-19 in Brescia, Lombardy, Italy. MedRxiv. 2020 doi: 10.1101/2020.04.28.20082735. [DOI] [PubMed] [Google Scholar]
- 6.Antonini A., Leta V., Teo J., Chaudhuri K.R. Outcome of parkinson’s disease patients affected by COVID-19. Mov. Disord. 2020;2019 doi: 10.1002/mds.28104. 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bianchetti A., Rozzini R., Guerini F., Boffelli S., Ranieri P., Minelli G., Bianchetti L., Trabucchi M. Clinical presentation of COVID19 in dementia Patients. J. Nutr. Health Aging. 2020:1–3. doi: 10.1007/s12603-020-1389-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. 2009. The PRISMA Statement for Reporting Systematic Reviews and Meta-analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. [DOI] [PubMed] [Google Scholar]
- 9.B.K. Macdonald, O.C. Cockerell, J.W.A.S. Sander, S.D. Shorvon, The incidence and lifetime prevalence of neurological disorders in a prospective community- based study in the UK, Brain. 123 (200AD) 665–676. https://doi.org/https://doi.org/10.1093/brain/123.4.665. [DOI] [PubMed]
- 10.Feigin V.L., Krishnamurthi R.V., Theadom A.M., Abajobir A.A., Mishra S.R., Ahmed M.B., Abate K.H., Mengistie M.A., Wakayo T., Abd-Allah F., Abdulle A.M., Abera S.F., Mohammed K.E., Abyu G.Y., Asgedom S.W., Atey T.M., Betsu B.D., Mezgebe H.B., Tuem K.B., et al. Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. doi: 10.1016/S1474-4422(17)30299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rejdak K., Grieb P. Adamantanes might be protective from COVID-19 in patients with neurological diseases: multiple sclerosis, parkinsonism and cognitive impairment. Mult. Scler. Relat. Disord. 2020;42 doi: 10.1016/j.msard.2020.102163. 102163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filatov A., Sharma P., Hindi F., Espinosa P.S. Neurological complications of coronavirus disease (COVID-19): encephalopathy. Cureus. 2020;12 doi: 10.7759/cureus.7352. e7352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beyrouti R., Adams M.E., Benjamin L., Cohen H., Farmer S.F., Goh Y.Y., Humphries F., Jäger H.R., Losseff N.A., Perry R.J., Shah S., Simister R.J., Turner D., Chandratheva A., Werring D.J. Characteristics of ischaemic stroke associated with COVID-19. J. Neurol. Neurosurg. Psychiatry. 2020;0:8–11. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang F., Yang Y., Dong K., Yan Y., Zhang S.J., Ren H., Yu X., Shi X. Clinical characteristics of 28 patients with diabetes and Covid-19 in Wuhan, China. Endocr. Pract. 2020 doi: 10.4158/EP-2020-0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P., De Leacy R.A., Shigematsu T., Ladner T.R., Yaeger K.A., Skliut M., Weinberger J., Dangayach N.S., Bederson J.B., Tuhrim S., Fifi J.T. Large-vessel stroke as a presenting feature of Covid-19 in the Young. N. Engl. J. Med. 2020;382 doi: 10.1056/NEJMc2009787. e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Co C.O.C., Yu J.R.T., Laxamana L.C., David-Ona D.I.A. Intravenous thrombolysis for stroke in a COVID-19 positive filipino patient, a case Report. J. Clin. Neurosci. Off. J. Neurosurg. Soc. Australas. 2020 doi: 10.1016/j.jocn.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vollono C., Rollo E., Romozzi M., Frisullo G., Servidei S., Borghetti A., Calabresi P. Focal status epilepticus as unique clinical feature of COVID-19: a case report. Seizure. 2020;78:109–112. doi: 10.1016/j.seizure.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Novi G., Mikulska M., Briano F., Toscanini F., Tazza F., Uccelli A., Inglese M. COVID-19 in a MS patient treated with ocrelizumab: does immunosuppression have a protective role? Mult. Scler. Relat. Disord. 2020;42(102120) doi: 10.1016/j.msard.2020.102120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suwanwongse K., Shabarek N. Benign course of COVID-19 in a multiple sclerosis patient treated with Ocrelizumab. Mult. Scler. Relat. Disord. 2020 doi: 10.1016/j.msard.2020.102201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gemcioglu E., Davutoglu M., Ozdemir E.E., Erden A. Are Type 1 Interferons treatment in Multiple Sclerosis as a potential therapy against COVID-19? Mult. Scler. Relat. Disord. 2020 doi: 10.1016/j.msard.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hughes R., Pedotti R., Koendgen H. COVID-19 in persons with multiple sclerosis treated with ocrelizumab - a pharmacovigilance case series. Mult. Scler. Relat. Disord. 2020 doi: 10.1016/j.msard.2020.102192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nie S., Zhao X., Zhao K., Zhang Z., Zhang Z., Zhang Z. Metabolic disturbances and inflammatory dysfunction predict severity of coronavirus disease 2019 (COVID-19): a retrospective study. MedRxiv. 2020;2019 doi: 10.1101/2020.03.24.20042283. 2020.03.24.20042283. [DOI] [Google Scholar]
- 23.Rodríguez- Cola M., Jiménez-VelascoI R., Gutiérrez-Henares F., López-Dolado (ELD) E., Gambarrutta-Malfatti (CGM) C., Vargas-Baquero E., Gil-Agudo A. Clinical Features of Coronavirus Disease 2019 (COVID-19) in a Cohort of Patients With Disability Due to Spinal Cord Injury. MedRxiv. 2020 doi: 10.11693/hyhz20181000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liao Y., Feng Y., Wang B., Wang H., Huang J., Wu Y., Wu Z., Chen X., Yang C., Fu X., Sun H. Clinical characteristics and risk factors for developed COVID-19 patients transferring to designated hospital in Jianghan Fangcang Shelter Hospital: a retrospective, observational study. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3576896. 1–16. [DOI] [Google Scholar]
- 25.Bruce S.L., Tiao J.R., Baldwin M.R., Gavin N., Bell F.M., Cohen M.F. Characterization and Clinical Course of 1000 Patients with COVID-19 in New York : retrospective case series student medical student assistant professor of medicine 3 Hamilton Southworth professor of epidemiology and medicine 4 assistant assistant professo. MedRxiv. 2020 doi: 10.1101/2020.04.20.20072116. [DOI] [Google Scholar]
- 26.Yin R., Yang Z., Wei Y., Li Y., Chen H., Liu Z., Zhao B., Ma D., Dan M., Zhang Y., Liu X., Leng H., Xiang D. Clinical characteristics of 106 patients with neurological diseases and co-morbid coronavirus disease 2019: a retrospective study. MedRxiv. 2020 doi: 10.1101/2020.04.29.20085415. 2020.04.29.20085415. [DOI] [Google Scholar]
- 27.Ji W., Huh K., Kang M., Hong J., Bae G.H., Lee R., Na Y., Choi H., Gong S., Choi Y.-H., Ko K.-P., Im J.-S., Jung J. Effect of underlying comorbidities on the infection and severity of COVID-19 in South Korea. MedRxiv. 2020 doi: 10.1101/2020.05.08.20095174. 2020.05.08.20095174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haimovich A., Ravindra N.G., Stoytchev S., Young H.P., Wilson F.P., van Dijk D., Schulz W.L., Taylor R.A. Development and validation of the COVID-19 severity index (CSI): a prognostic tool for early respiratory decompensation. MedRxiv. 2020 doi: 10.1101/2020.05.07.20094573. 2020.05.07.20094573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berekashvili K., Dmytriw A.A., Vulkanov V., Agarwal S., Khaneja A., Nandakumar T., Liff J., Turkel-Parrella D., Farkas J., Zhou T., Frontera J.A., Kahn D.E., Kim S., Humbert K.A., Sanger M.D., Yaghi S., Lord A.S., Arcot K.M., Tiwari A., Mph M.D. Etiologic subtypes of ischemic stroke in SARS-COV-2 virus patients in a cohort of New York City hospitals. MedRxiv. 2020 doi: 10.1101/2020.05.03.20077206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim L., Garg S., O’Halloran A., Whitaker M., Pham H., Anderson E., Armistead I., Bennett N., Billing L., Como-Sabetti K., Hill M., Kim S., Monroe M., Muse A., Reingold A., Schaffner W., Sutton M., Talbot H., Torres S., Yousey-Hindes K., Holstein R., Cummings C., Brammer L., Hall A., Fry A., Langley G. Interim analysis of risk factors for severe outcomes among a cohort of hospitalized adults identified through the U.S. Coronavirus disease 2019 (COVID-19)-Associated hospitalization surveillance network (COVID-NET) MedRxiv. 2020 doi: 10.1101/2020.05.18.20103390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Creed M.A., Ballesteros E., Jr L.J.G., Imitola J. Mild COVID-19 infection despite chronic B cell depletion in a patient with aquaporin-4-positive neuromyelitis optica spectrum disorder. Mult. Scler. Relat. Disord. 2020;44 doi: 10.1016/j.msard.2020.102199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beach S.R., Praschan N.C., Hogan C., Dotson S., Merideth F., Kontos N., Fricchione G.L., Smith F.A. Delirium in COVID-19: a case series and exploration of potential mechanisms for central nervous system involvement. Gen. Hosp. Psychiatry. 2020;65:47–53. doi: 10.1016/j.genhosppsych.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morassi M., Bagatto D., Cobelli M., D’Agostini S., Gigli G.L., Bnà C., Vogrig A. Stroke in patients with SARS-CoV-2 infection: case series. J. Neurol. 2020 doi: 10.1007/s00415-020-09885-2. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hainque E., Grabli D. Rapid worsening in Parkinson’s disease may hide COVID-19 infection. Park. Relat. Disord. 2020:1–2. doi: 10.1016/j.parkreldis.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zheng K.S., Dorfman B.J., Christos P.J., Khadem N.R., Henchcliffe C., Piboolnurak P., Nirenberg M.J. Clinical characteristics of exacerbations in parkinson disease. Neurologist. 2012;18:120–124. doi: 10.1097/NRL.0b013e318251e6f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cunningham C. Systemic inflammation and delirium: important co-factors in the progression of dementia. Biochem. Soc. Trans. 2011;39:945–953. doi: 10.1042/BST0390945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu J., Zhong S., Liu J., Li L., Li Y., Wu X., Li Z., Deng P., Zhang J., Zhong N., Ding Y., Jiang Y. Detection of severe acute respiratory syndrome coronavirus in the brain: potential role of the chemokine mig in pathogenesis. Clin. Infect. Dis. an Off. Publ. Infect. Dis. Soc. Am. 2005;41:1089–1096. doi: 10.1086/444461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu L., Xiong W., Liu D., Liu J., Yang D., Li N., Mu J., Guo J., Li W., Wang G., Gao H., Zhang Y., Lin M., Chen L., Shen S., Zhang H., Sander J.W., Luo J., Chen S., Zhou D. New onset acute symptomatic seizure and risk factors in coronavirus disease 2019: a retrospective multicenter study. Epilepsia. 2020 doi: 10.1111/epi.16524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frucht M.M., Quigg M., Schwaner C., Fountain N.B. Distribution of seizure precipitants among epilepsy syndromes. Epilepsia. 2008;41:1534–1539. doi: 10.1111/j.1528-1167.2000.01534.x. [DOI] [PubMed] [Google Scholar]
- 40.Kaddumukasa M., Kaddumukasa M., Matovu S., Katabira E. The frequency and precipitating factors for breakthrough seizures among patients with epilepsy in Uganda. BMC Neurol. 2013;13 doi: 10.1186/1471-2377-13-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.William K.C., Sibley A., Bamford Colin R. Clinical viral infections and multiple sclerosis. Lancet. 1985;1:1313–1315. doi: 10.1007/s00134-020-05991-x.Bizzarro. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Louapre C., Collongues N., Stankoff B., Giannesini C., Papeix C., Bensa C., Deschamps R., Créange A., Wahab A., Pelletier J., Heinzlef O., Labauge P., Guilloton L., Ahle G., Goudot M., Bigaut K., Laplaud D.-A., Vukusic S., Lubetzki C., De Sèze J. Clinical characteristics and outcomes in patients with coronavirus disease 2019. and Multiple Sclerosis, JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.2581. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]