Abstract
Purpose of Review
We explored themes in recent post-stroke dysphagia literature, focusing on the following questions: (1) What does post-stroke dysphagia look like?; (2) Who gets post-stroke dysphagia?; (3) What are the consequences of post-stroke dysphagia?; and (4) How can we improve treatment of post-stroke dysphagia?
Recent Findings
There have been several improvements in quantitative descriptions of swallowing physiology using standard and new evaluation techniques. These descriptions have been correlated with lesion locations, and several factors can predict development of post-stroke dysphagia and its sequelae. Novel treatment paradigms have leveraged post-stroke neuroplastic improvements using neurostimulation and biofeedback techniques. Despite recent findings, the field is limited by lack of standardization and unanswered questions on rehabilitation variables.
Summary
Our improved understanding of post-stroke dysphagia will enhance our ability to prevent, identify, and treat it. Future work should be grounded in swallowing physiology and continue refining treatments, particularly in the acute stage.
Keywords: Stroke, Deglutition, Dysphagia, Rehabilitation
Introduction
Swallowing is a complex sensorimotor process involving the coordination of multiple muscle groups to propel a bolus of food or liquid from the mouth to the stomach while protecting the airway and minimizing residue. Swallowing pattern-generating neural circuitry is situated in the rostral medulla [1], with widespread cortical and subcortical activation associated with movement preparation and sensory processing [2••]. Thus, stroke-related lesions in either cortical hemisphere, subcortical control circuits, or in the brainstem can result in difficulty swallowing or dysphagia [2••, 3]. See Felix and colleagues’ recent review for a tutorial on current practice for screening, evaluation, and treatment of post-stroke dysphagia [4••].
Review of recent literature regarding post-stroke dysphagia underscores four themes of research questions: (1) What does post-stroke dysphagia look like?; (2) Who gets post-stroke dysphagia?; (3) What are the consequences of post-stroke dysphagia?; and (4) How can we improve treatment of post-stroke dysphagia? This review will focus on publications that explored these questions with discussions of potential for implementation into clinical practice and unanswered questions.
What Does Post-stroke Dysphagia Look like?
Swallowing function is typically first evaluated at bedside, either by a dysphagia screen or by thorough evaluation of orofacial structure and function by a speech-language pathologist. Although it is an integral part of swallowing evaluation, there is consensus among the dysphagia community that instrumented approaches are instead the only ways to assess certain aspects of swallowing physiology, such as airway protection, bolus propulsion, and pharyngeal residue, to name a few [5].
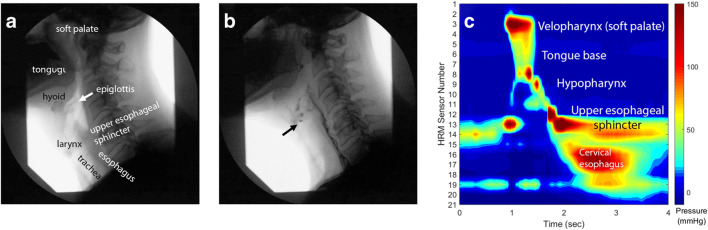
There has been considerable effort to quantify aspects of swallowing physiology visualized on videofluoroscopy, an x-ray evaluation of swallowing physiology (Fig. 1a, b). The Modified Barium Swallow Impairment Profile (MBSImP) operationalizes 17 components of oral, pharyngeal, and esophageal swallowing into Likert-type scales [6]. MBSImP metrics involving bolus transport in the oral cavity, epiglottic movement, and upper esophageal sphincter opening have shown good relationship with improvement in diet levels in the acute stages post-stroke [7]. Swallowing function can also be assessed as coordination of biomechanical movements and bolus passage over time through frame-by-frame video analysis. This level of analysis has revealed significant swallowing discoordination in patients with stroke-related dysphagia compared with healthy controls [8, 9]. Furthermore, this level of analysis identified quantitative swallowing coordination differences in patients with stroke and no dysphagia, showing that stroke may impact swallowing physiology below the threshold of clinical significance [10]. Combined analysis of biomechanics and timing can be achieved through algorithms tracking oropharyngeal structures over time in Computational Analysis of Swallow Mechanics (CASM) [11]. Compared to healthy controls, persons with stroke show quantitative differences in hyoid excursion, laryngeal elevation, tongue base retraction, pharyngeal shortening, and timing of bolus movement [11, 12].
Fig. 1.
Swallowing evaluations in a 58-year-old man in the chronic stage following stroke. (a) Videofluoroscopic swallow study frame in a rest position prior to swallowing with anatomic labels; (b) video frame mid-swallow; arrow identifies aspirated material; and (c) pharyngeal high-resolution manometry spatiotemporal plot displaying pressure generated over the entire swallow; hypopharyngeal pressures are generated at the level of the larynx. Studies were performed on the same patient on the same day
While the quantitative evaluation of videofluoroscopy is still largely subjective, a relatively new technique has been established to objectively and quantitatively measure pressures generated along the pharynx and esophagus during a swallow: high-resolution manometry [13•] (Fig. 1c). Patients with post-stroke dysphagia can have reduced pharyngeal propulsive pressures, abnormal upper esophageal sphincter relaxation pressures, or both [14, 15]. Pharyngeal manometry has revealed interesting compensations to swallowing function in those with brainstem stroke: (1) pharyngeal mis-sequencing [16], where pharyngeal pressures are generated simultaneously instead of in a top-down pattern, and (2) vacuum swallowing [17, 18], where extreme sub-atmospheric pressure generated in the upper esophageal sphincter and esophagus will “suck” the bolus downwards in the setting of low pharyngeal pressures.
Improvements in evaluation techniques will lead to more precise dysphagia diagnoses and better assessment of functional improvement. While these new approaches provide us with enhanced ways of understanding post-stroke swallowing physiology, they do not give information on their own regarding how disruptions of certain neural pathways result in altered physiology or how to best treat these physiologic deficits.
Who Gets Post-stroke Dysphagia?
Stroke is one of the leading causes of dysphagia, with incidence rates up to 80% [19]. Incidence estimates depend on the definition of dysphagia, which can range from failing a dysphagia screen, to prescribed diet modifications, to measures of physiology on an instrumented swallowing study [20].
A common focus of post-stroke dysphagia research in the past 5 years has been to predict what patient characteristics are associated with a greater risk of dysphagia, particularly in the acute and subacute phases. Table 1 summarizes independent predictors of post-stroke dysphagia. Other predictors of post-stroke dysphagia not appearing in multiple sources include male sex [21], higher Glasgow Coma Scale on admission [22], hemorrhagic vs. ischemic stroke [37], anterior or middle cerebral artery involvement [22], large vs. small vessel occlusion [23], and facial palsy [31]. Hyperlipidemia and lesions isolated to the thalamus are reported to occur less frequently in those with post-stroke dysphagia [24, 25], but there is no apparent protective measure of either condition. Many studies excluded patients requiring intubation, but Dunn and colleagues [26] report intensive care unit stay, length of intubation, and need for tracheostomy to also be independent predictors for post-stroke dysphagia. Many publications on predicting dysphagia post-stroke rely on failing a dysphagia screen—or even participating in a screen to begin with—to identify dysphagia. Dysphagia screening is an important part of the clinical process, can reduce rates of aspiration pneumonia [46], and is part of the guidelines set by the American Heart Association and American Stroke Association [47], but its use to identify persons with dysphagia in research is problematic. As with any screen, those for dysphagia consist of observing a patient perform a simple task to identify those who would benefit from further evaluation. Screening tests inherently have high specificity, but many suffer from low sensitivity [48•, 49]. Although the aforementioned guidelines mention the utility of dysphagia, they do not specify types of dysphagia screens or optimal times when dysphagia should be evaluated.
Table 1.
Independent predictors of post-stroke dysphagia across multiple studies
| Older age [21–30] | |
| Greater NIHSS [21, 23, 25, 27, 30–36] | |
| Greater mRS [28, 32, 37] | |
| Lower Barthel index [37, 38] | |
| Malnutrition or lower BMI at admission [28, 37, 39] | |
| Greater lesion volume [27, 31, 36, 40] | |
| Subcortical vs. cortical involvement [24, 41, 42] | |
| Brainstem involvement [3, 24, 25, 32, 34, 41, 43] | |
| Corticobulbar tract involvement [38, 44] | |
| White matter involvement [25, 38, 44] | |
| Presence of dysarthria [31, 32] | |
| Presence of dysphonia or reduced maximum pitch [31, 45] | |
| Cognitive impairment or dementia [22, 29] |
NIHSS, National Institutes of Health Stroke Scale; mRS, Modified Rankin Scale; BMI, body mass index
With refinements on quantitative analysis of video swallowing evaluations, research has begun to investigate infarct locations that are associated with particular physiologic swallowing deficits and their sequelae. While still in early stages, a summary of findings of region of interest-based lesion mapping associated with dysphagia signs is outlined in Table 2. Notably, neither Daniels et al. [3] nor Wilmskoetter et al. [53] reported lesion location relationships when dysphagia physiology metrics were collapsed into a total impairment score. These complex findings highlight the multivariate nature of swallowing and the heterogeneity that can be seen in post-stroke dysphagia. An important limitation of these studies was the exclusion or underrepresentation of patients with brainstem lesions; its exclusion from Table 2 should not be a sign of irrelevance of brainstem lesions. This line of work is also an important step in understanding neural control of separate aspects of swallowing and how it may be disrupted by neurologic damage.
Table 2.
Lesion locations associated with specific signs of dysphagia
| Deficit/sequela | Brain region |
|---|---|
| Prolonged oral bolus transit time |
L inferior frontal lobe [50] L precentral gyrus [50] |
| Prolonged pharyngeal bolus transit time |
Insula [51] R basal ganglia [50] R corona radiata [50] Corticobulbar tract white matter [44] |
| Delayed onset of pharyngeal swallow trigger |
R middle temporal gyrus [52] R superior temporal gyrus [52] R temporal pole [52] R lateral occipital cortex [52] R angular gyrus [52] R supramarginal gyrus [52] R planum temporale [52] R caudate [52] R superior longitudinal fasciculus [52] R parietal operculum cortex [52] Corticobulbar tract white matter [44] |
| Reduced laryngeal elevation |
R precentral gyrus [53] R anterior & posterior insula [53] R external capsule [53] R superior corona radiata [53] R superior longitudinal fasciculus [53] Corticobulbar tract white matter [44] |
| Reduced anterior hyoid excursion |
L amygdala [53] L ansa lenticularis [53] L lenticular fasciculus [53] |
| Reduced laryngeal vestibule closure |
L postcentral gyrus [53] L supramarginal gyrus [53] R anterior & posterior insula R superior corona radiata [53] R external capsule [53] |
| Pharyngeal residue |
R postcentral gyrus [53] R supramarginal gyrus [52, 53] R superior & posterior corona radiata [53] R tapetum [53] R internal capsule [53] R superior longitudinal fasciculus [53] R posterior superior temporal gyrus [52, 53] R middle temporal gyrus [52] R planum temporale [52] R frontal orbital cortex [52] R parietal operculum [52] |
| Penetration/aspiration |
R precentral gyrus [53] R postcentral gyrus [53] R superior longitudinal fasciculus [53] R supramarginal gyrus [40, 53] R superior temporal gyrus [40] R planum temporale [40] Corticobulbar tract white matter [44] |
| Impaired cough response |
R paracingulate gyrus [52] R accumbens [52] R cingulum [52] R amygdala [52] R pallidum [52] R superior longitudinal fasciculus [52] R inferior frontal gyrus [52] L middle temporal gyrus [52] L postcentral gyrus [52] L supramarginal gyrus [52] |
| Impaired oral intake |
Insula [36] Rolandic operculum [36] Superior corona radiata [36] Putamen [36] External capsule [36] Superior longitudinal fasciculus [36] |
| Tube feeding dependence |
Insula [36] Rolandic operculum [36] |
| Pneumonia |
R precentral gyrus [52] R postcentral gyrus [52] R paracingulate gyrus [52] R anterior cingulate gyrus [52] R supplementary motor cortex [52] R superior frontal gyrus [52] R middle frontal gyrus [52] R inferior frontal gyrus [52] R cingulum [52] R amygdala [52] R & L thalamus [52] L anterior thalamic radiation [52] |
R, right; L, left; if there is no demarcation of R or L, there was no significant association of hemisphere
What Are the Consequences of Post-stroke Dysphagia?
Dysphagia is a significant predictor of negative health and psychosocial outcomes. Consequences associated with post-stroke dysphagia mirror those of other dysphagia etiologies and include malnutrition, dehydration, reduced quality of life, and aspiration pneumonia [54]. Furthermore, all-cause dysphagia increases length of inpatient stays by 2.8 days, costs by 34%, and more than doubles in-hospital mortality rate [55].
Recent work in stroke has attempted to predict the influence of post-stroke dysphagia and other patient factors on unfavorable outcomes. There is an association of post-stroke dysphagia with increased mortality [22, 28, 30, 34, 37, 56–58], overall unfavorable outcome [34, 35, 58], greater dependency [30, 36, 57], longer length of stay [33, 36], less likely to discharge home [35, 36, 57, 58], and modified diet or reliance on tube feeding [22, 35, 43, 57]. Longer length of stay due to dysphagia may occur in patients whose medical evaluation is completed, but the medical team is waiting to see if the dysphagia will resolve or a percutaneous gastrostomy tube is needed, as many skilled nursing facilities will not admit patients reliant to tube feeding, but without a permanent feeding tube.
Possibly the most cited sequela of post-stroke dysphagia is an increased risk of pneumonia [21, 30, 34, 36, 56, 57, 59–62]. Development of post-stroke pneumonia is multifactorial [60–62], and dysphagia should thus only be considered a risk factor. Furthermore, patients placed nil per os (NPO) due to severe dysphagia will continue to aspirate saliva and refluxate. NPO status and tube feeding dependence have long been understood as independent predictors of aspiration pneumonia [63•]. Implementing oral care protocols to decrease oral bacteria may help with reducing risk of pneumonia [47], but more studies are needed to assess causation.
Work investigating post-stroke dysphagia outcomes also suffers from the limitation that dysphagia screens are used to identify patients with dysphagia. However, the only study to investigate a particular dysphagia sign and outcomes was with spontaneous saliva swallow rate [35]. More precise understanding of swallowing physiology allows not only for more precise approaches but for better understanding of prognoses.
How Can We Improve Treatment of Post-stroke Dysphagia?
Traditional dysphagia therapy following stroke focuses on compensations and behavioral rehabilitation strategies. Treatment is patient-specific, with successful dysphagia therapies implemented in one patient population not necessarily producing the same results in another population [64]. The understanding of spontaneous swallowing recovery following stroke is constantly evolving, and novel treatment methods are being developed and implemented to better manage and enhance swallowing recovery. Two major themes emerged in reviewing recent post-stroke dysphagia rehabilitation literature: neurostimulation and biofeedback.
Neurostimulation
With evidence of neural repair mechanisms and increased cortical activity playing a significant role in the swallowing recovery process following stroke, noninvasive neurostimulation therapies are of particular interest in treatment in post-stroke dysphagia. Neurostimulation can promote cortical reorganization to accelerate the natural process of stroke recovery and is characterized as peripheral or central stimulation [65]. Stimulation techniques hold promise for implementation in the early stages post-stroke, when patients may not have the language or cognitive barriers that may preclude following complex therapeutic instructions.
Peripheral Stimulation
Pharyngeal Electrical Stimulation
Pharyngeal electrical stimulation (PES) passively stimulates the pharynx with low-amplitude electrical impulses. Using transnasal catheters with electrodes in the pharyngeal region, PES is thought to increase brain activity in areas that control swallowing and promote cortical reorganization of the swallowing motor cortex [66].
Early research in PES established effective stimulation parameters of 5 Hz, 10 min/day for 3 consecutive days at an intensity determined by the patient’s perceptual threshold plus 75% the difference between the patient’s maximum tolerated threshold and perceptual threshold [67]. These parameters have been implemented in recent studies to evaluate PES treatment in hemispheric stroke with dysphagia complications in the early subacute phase. Initially, these studies showed promising results in improving swallowing outcome; however, more recent research has been unable to reproduce such findings, showing no significant improvement in aspiration and clinical dysphagia at 2 weeks and 3 months posttreatment [68, 69].
Despite inconclusive results of the effectiveness of PES, other studies focused on administering PES to tracheostomized stroke patients with dysphagia yielded positive results. PES improved dysphagia enough to enable decannulation in the majority of patients [70•, 71, 72]. The effectiveness of PES may be related to stroke severity, with more severe stroke patients exhibiting better therapeutic response than patients with mild stroke [68, 70•]. However, long-term effects of PES on swallowing outcome, relative effectiveness of active vs. passive PES, optimal timing of PES therapeutic intervention, and the optimal stimulation parameters remain unclear.
Neuromuscular Electrical Stimulation
Another method of peripheral stimulation under exploration is neuromuscular electrical stimulation (NMES). Transcutaneous electrodes pass electrical current to generate muscle contractions in suprahyoid or infrahyoid muscles [65, 73]. Suprahyoid stimulation will activate the geniohyoid, mylohyoid, and anterior belly of the digastric muscles, resulting in elevation of the hyoid bone and larynx, while infrahyoid stimulation will activate the omohyoid, sternohyoid, and sternothyroid, depressing the hyoid bone and larynx [74]. Suprahyoid stimulation is thought to enhance the strength of weak muscles in order to elevate the hyolaryngeal complex to facilitate airway protection for swallowing, whereas infrahyoid stimulation is thought to depress the hyolaryngeal complex as a mechanism to swallow against resistance [73]. A meta-analysis concluded that treatment with NMES was more effective in improving swallowing function in the short-term than treatment without NMES in both acute/subacute and chronic stroke patients [73]. However, there was significant heterogeneity across the studies, which was attributed to variability in stroke type and duration, frequency and intensity of stimulation, and sample size and blinding [73].
NMES for dysphagia treatment is controversial and is not covered by some health insurers [75]. While NMES treatment has generated some positive results in treating dysphagia when coupled with traditional dysphagia therapy in stroke patients, the exact mechanism of NMES is unclear, and there has been little consensus on optimal electrode placement as well as proper frequency and intensity for stimulation. Use of NMES in therapy requires careful consideration of the individual patient’s specific swallowing deficits and clear understanding of which muscles are being targeted.
Central Stimulation
Repetitive Transcranial Magnetic Stimulation
Repetitive transcranial magnetic stimulation (rTMS) uses a copper coil placed on the scalp to deliver magnetic stimulation, resulting in a change to electrical activity on neocortex directly under the coil [76]. Pulses are delivered at a low frequency of ~ 1 Hz, and rTMS slows neuronal excitability and produces an inhibitory effect, whereas pulses delivered at ≥ 3 Hz increase neuronal excitability [76, 77]. Both high-frequency and low-frequency rTMS have been evaluated as treatment methods for post-stroke dysphagia.
Some randomized, controlled trials have explored the effectiveness of rTMS in dysphagia rehabilitation in the acute, subacute, and chronic stages. Meta-analyses by Pisegna et al. and Liao et al. evaluated a total of 11 studies and concluded that rTMS over the pharyngeal motor cortex paired with traditional dysphagia therapy was an effective method to improve swallowing function in stroke patients with dysphagia [76, 77]. rTMS showed therapeutic benefit at 4 weeks posttreatment and was more effective at high-frequency rather than low-frequency [77]. Bilateral or contralesional stimulation may also have a positive effect on dysphagia after stroke, while ipsilesional stimulation showed no effect [77]. There is an ongoing trial evaluating effectiveness of rTMS applied to the cerebellum in post-stroke dysphagia [78]. Consensus has not yet been reached on specific stimulation parameters, number of pulses per session, and length of treatment.
Transcranial Direct Current Stimulation
Transcranial direct current stimulation (tDCS) involves a low-intensity, electrical current (1–2 mA) applied between a cathode and anode placed on the scalp [76, 79]. Anodal tDCS depolarizes the resting membrane potential and thereby increases neuronal excitability, whereas cathodal tDCS hyperpolarizes the resting membrane potential, decreasing neuronal excitability [79]. Anodal tDCS has been explored as a method to enhance swallowing recovery in dysphagic stroke patients. Anodal tDCS can be unilateral or bilateral. Unilateral anodal tDCS involves placing the anode over the affected pharyngeal motor cortex and the cathode over the contralateral supraorbital region, whereas bilateral tDCS places an anode over the pharyngeal motor cortex of both hemispheres and a cathode over each corresponding contralesional supraorbital region [79]. Dual stimulation utilizes both anodal and cathodal tDCS, implementing anodal tDCS over the damaged hemisphere and cathodal tDCS over the contralesional one [80].
Current research on tDCS as a treatment method for dysphagic stroke patients is highly variable. Information regarding the site of electrode placement (ipsilateral vs. contralateral), stimulation parameters (intensity and duration), method of stimulation (unilateral vs. bilateral), time post-stroke, and the type of stroke patient that would most benefit is lacking. A meta-analysis evaluated three small-scale studies that explored the effectiveness of unilateral tDCS on swallowing function in stroke patients and found tDCS treatment to have a moderate but not significant pooled effect size when compared to treatment without tDCS [76]. However, the studies varied in the hemisphere stimulated, treatment protocol, and the outcome measurements obtained [76].
More recent studies exploring bilateral tDCS have resulted in positive findings. Ahn et al. [79] found significant improvement in swallowing function in chronic stroke patients. Additionally, Li et al. found that unilateral and bilateral tDCS of the affected hemisphere combined with traditional dysphagia therapy were both effective in improving swallowing function in chronic stroke patients, with bilateral tDCS resulting in a more substantial improvement [81]. Further studies are needed to compare the effectiveness of unilateral and bilateral stimulation as well as ipsilateral and contralateral stimulation in order to gain a greater insight into the most effective method for tDCS in stroke patients with dysphagia.
Paired Associative Stimulation
Paired associative stimulation (PAS) is a neurostimulation technique that simultaneously implements peripheral and central stimulation methods to induce excitation of the pharyngeal motor cortex [65]. The rationale behind PAS is further built on Hebbian neuroplastic principles through the delivery of stimulation at multiple sites. Hamdy et al. were the first to explore PAS as a treatment method for dysphagic stroke patients. Pairing PES with TMS, they found that PAS led to short-term improvement in swallowing function, increasing excitability of the unaffected pharyngeal cortex and reducing penetration-aspiration scores in chronic stroke patients [82, 83]. Additionally, they determined that repeated stimulation could induce excitability in patients that did not respond to PAS initially and that administering PAS for a shorter time duration (~ 10 min) resulted in more substantial changes in cortical excitability than administering PAS for a longer time duration (~ 30 min) [82, 84].
Recently, little research has been conducted to further explore the effectiveness of PAS as a treatment method for post-stroke dysphagia. In 2019, Zhang et al. reported that TMS paired with NMES was more effective in treating post-stroke dysphagia than NMES alone and that bilateral TMS paired with NMES was more effective than unilateral stimulation [85]. However, this study had a small sample size, and these results would need to be validated by a larger study.
Biofeedback
As swallowing is a complex behavior with many small muscle groups working deep in the oral cavity and pharynx, the patient’s ability to assess their own performance is limited. Biofeedback is an adjunct to swallowing therapy, wherein the patient is provided visual or auditory signals that enable them to alter conscious or subconscious mechanisms involved in the swallowing process and improve their swallowing performance [86•, 87].
The most common biofeedback technique used in post-stroke dysphagia therapy is surface electromyography (sEMG). sEMG biofeedback uses two small electrodes placed on the submental muscles to measure the timing and force of the muscle contraction, which is displayed graphically on a screen [88, 89]. A recent meta-analysis found that sEMG biofeedback coupled with swallowing maneuvers increased hyoid displacement in post-stroke dysphagia patients when compared with controls [88]. sEMG biofeedback has the potential for short-term benefits to dysphagia rehabilitation; however, it has been hypothesized that once patients learn swallowing therapies, biofeedback yields no further benefits. Careful training must be undertaken to ensure that patients can generalize behaviors so they can be replicated without the feedback.
Another novel dysphagia treatment approach using sEMG biofeedback is Biofeedback in Strength and Skill Training (BiSSkiT). BiSSkiT is a training protocol focused on improving the precision of swallowing muscle contraction, whereas typical sEMG biofeedback typically focuses on amplitude of muscle contraction. One of the BiSSkiT treatment methods involves the participants swallowing such that their peak waveform fell within a square target displayed on the computer monitor. This target moves randomly and requires the participants to practice precision and control of their swallowing movements in order to successfully fall within the target. Initial work in neurodegenerative conditions suggests that skill training improved coordination and timing of swallowing and could be effective in dysphagia rehabilitation [90, 91]. While no trials have been published in post-stroke dysphagia, the positive findings of early studies suggest that skill training has potential to be effective in dysphagia rehabilitation, particularly in cases of swallowing dyscoordination.
A Cochrane review in 2018 revealed no subgroup effects for acute/subacute therapy approach (traditional therapy, NMES, PES, tDCS, TMS, acupuncture, drug therapy) on outcomes such as death/dependency/disability, length of inpatient stay, swallowing ability, or aspiration pneumonia [20]. However, this review also identified very low quality evidence for the ability of swallowing treatment to improve swallowing ability or prevent aspiration pneumonia [20]. There is much more work needed to optimize post-stroke dysphagia rehabilitation.
Clinical Implementation
How can post-stroke dysphagia clinical practice be impacted by recent research findings? The field is continually evolving, but a lack of standardized evaluation and treatments and challenges to rapid translation of research findings to clinic can impede practice improvements.
Improvements in our clinical evaluation methods have the potential to revolutionize our understanding of dysphagia pathophysiology. However, implementation of videofluoroscopic quantification methods requires intensive initial and reliability training and can take more time out of a busy clinic day to implement. Further, recent findings of coordination deficits are informative, but the bulk of the traditional dysphagia therapies are built on a foundation of strengthening swallowing musculature, not improving coordination. Acquiring high-resolution manometry equipment is costly and has other institutional barriers, such as a lack of a reimbursable Medicare code that is billable by speech-language pathologists [92]. Clinicians are the drivers of change and need to be persistent and persuasive with hospital and clinic leadership to move the field forward and ensure patient care happens at the leading edge of the evidence base.
Predictive modeling—both for determining risk for dysphagia and consequences thereof—is helpful to know for clinical practice, particularly for triaging patients who may require more urgent, swallowing evaluation. However, a takeaway should not be that a patient with none of the risk factors will not develop dysphagia. The impetus remains on clinicians to use critical thinking and sound judgment to examine each patient as a case study and work to treat their specific deficits.
In the current climate, another barrier to implementing ideal clinical practices is the very real threats associated with COVID-19. Telehealth for swallowing therapy has been deemed “safe and effective” [93]. However, this does not take into account the need for imaging assessments, particularly in the acute phases of stroke, where a patient’s status is in a constant state of flux. See the recent taskforce report put forth by the Dysphagia Research Society and an international effort derived from physical therapy for best practice recommendations in the setting of COVID-19 [94, 95].
Overall, there are barriers to adoption of new practices hospital-wide, including obtaining needed equipment, supplies, and training, limiting the ability of the US medical system to reimburse novel treatment paradigms. These limitations make it difficult for clinicians to practice at the cutting edge of the evidence base [96•].
Unanswered Questions
There are still many unanswered questions that limit the practicing speech-language pathologist and intraprofessional team from answering: What do we need to do for the patient now? In the upcoming weeks/months? Long-term?
Due to the enhanced neuroplasticity that occurs early after stroke onset, it is highly beneficial to implement treatments in acute and subacute phases of stroke [97]. From a practical perspective, interventions intended to decrease the length of hospital stay or occurrence of dysphagia-related aspiration pneumonia would likely need to be initiated early following stroke. However, the neurophysiology of dysphagia recovery following stroke is complex and incompletely understood, and inpatient speech-language pathologists often have very little time or resources to implement dysphagia treatment protocols [96•]. This presents challenges to managing dysphagia, particularly in the acute and subacute phases, especially since many of these studies are focused on the chronic period of recovery and there is not a universally accepted method for evaluating post-stroke dysphagia in the inpatient setting. Determining the optimal treatment methods to implement in individual patients and understanding the neurophysiological effects of more novel methods remain unclear. Studies have widely varying parameters and intervention timings, and their results are confounded by many factors including mixed types of stroke, stages of stroke, and types and severity of dysphagia.
While the novel methods reviewed in this paper present a growing consensus for the effectiveness of neurostimulation and biofeedback in enhancing dysphagia rehabilitation, there are many questions and uncertainties that need to be explored. By nature, stroke severity is influenced by multiple factors, and due to the complexity of the treatment interventions, it is difficult to determine what exactly led to recovery [98]. Studies reviewed here consisted of stroke patients with a mix of subacute and chronic stroke who will naturally recover at different rates making it difficult to determine the effectiveness of novel therapies. Additionally, stimulation parameters and treatment times greatly varied in the studies with suboptimal parameters or late intervention yielding neutral results for promising neurostimulation methods. Lastly, the majority of literature reviewed were small-scale studies or eliminated patients who had multiple strokes or comorbidities that could result in dysphagia; thus, they were not fully representative of stroke populations, and their results could fail to accurately represent their effectiveness.
With the exception of PES, a particular gap in the rehabilitation literature is on rehabilitation commencing in the acute phases, when the patient may not be able to participate in active rehabilitation or take an oral diet. There are many unknowns about the degree of decompensation that can happen in the absence of eating and drinking, or if there is a critical window for rehabilitation in patients who go on to develop chronic and treatment-refractory dysphagia. Questions on timing of dysphagia intervention might be better explored with animal models of stroke. Cullins and Connor [99] used a middle cerebral artery occlusion rat model to specifically investigate post-infarct dysphagia with validated, species-specific swallowing physiology measures. This and other animal models will improve our understanding of the pathophysiology of post-stroke dysphagia and explore questions regarding timing, dose, and other unknown aspects of post-stroke swallowing rehabilitation. With dysphagia being associated with increased hospital stay and the development of aspiration pneumonia, treatments that could be effective in the acute period of recovery may be of particular interest. Interventions that can potentially decrease the length of hospital stay or prevent aspiration pneumonia, particularly during the COVID-19 pandemic, would likely be especially relevant to the clinical community.
Systematic research programs are needed with rigorous, prospective, well-designed studies to answer these questions. Clinicians need to take an active role in staying up to date with the literature and being proactive with implementing change in a standardized way.
Conclusions
Stroke can have significant negative consequences on swallowing physiology. Great strides have been taken in the past few years in an effort to better characterize post-stroke dysphagia, to predict which stroke variables and patient factors lead to dysphagia and negative sequelae, and to address rehabilitation from a neuroplastic perspective. Several challenges to implementation and questions regarding post-stroke dysphagia evaluation and treatment remain and will be aided with continued focus on defining dysphagia by swallowing physiology rather than screening failure or diet level. Creative and interdisciplinary work will continue to reduce stroke risk, prevent negative consequences of post-stroke dysphagia, and help rehabilitate patients back to functional swallowing.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Neurorehabilitation and Recovery
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Jean A. Brain stem control of swallowing: neuronal network and cellular mechanisms. Physiol Rev. 2001;81(2):929–969. doi: 10.1152/physrev.2001.81.2.929. [DOI] [PubMed] [Google Scholar]
- 2.Wilmskoetter J, Daniels SK, Miller AJ. Cortical and subcortical control of swallowing-can we use information from lesion locations to improve diagnosis and treatment for patients with stroke? Am J Speech-Lang Pathol. 2020;29(2s):1030–1043. doi: 10.1044/2019_ajslp-19-00068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniels SK, Pathak S, Mukhi SV, Stach CB, Morgan RO, Anderson JA. The relationship between lesion localization and dysphagia in acute stroke. Dysphagia. 2017;32(6):777–784. doi: 10.1007/s00455-017-9824-0. [DOI] [PubMed] [Google Scholar]
- 4.Felix CC, Joseph ME, Daniels SK. Clinical decision making in patients with stroke-related dysphagia. Semin Speech Lang. 2019;40(3):188–202. doi: 10.1055/s-0039-1688815. [DOI] [PubMed] [Google Scholar]
- 5.Garand KL, McCullough G, Crary M, Arvedson JC, Dodrill P. Assessment across the life span: the clinical swallow evaluation. Am J Speech-Lang Pathol. 2020;29(2S):919–933. doi: 10.1044/2020_AJSLP-19-00063. [DOI] [PubMed] [Google Scholar]
- 6.Martin-Harris B, Brodsky MB, Michel Y, Castell DO, Schleicher M, Sandidge J, Maxwell R, Blair J. MBS measurement tool for swallow impairment-MBSImp: establishing a standard. Dysphagia. 2008;23(4):392–405. doi: 10.1007/s00455-008-9185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilmskoetter J, Bonilha L, Martin-Harris B, Elm JJ, Horn J, Bonilha HS. Factors influencing oral intake improvement and feeding tube dependency in patients with poststroke dysphagia. J Stroke Cerebrovasc Dis. 2019;28(6):1421–1430. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saconato M, Leite FC, Lederman HM, Chiari BM, Gonçalves MIR. Temporal and sequential analysis of the pharyngeal phase of swallowing in poststroke patients. Dysphagia. 2019;35:598–615. doi: 10.1007/s00455-019-10069-y. [DOI] [PubMed] [Google Scholar]
- 9.Nakao M, Oshima F, Maeno Y, Izumi S. Disruption of the obligatory swallowing sequence in patients with Wallenberg syndrome. Dysphagia. 2019;34(5):673–680. doi: 10.1007/s00455-018-09970-9. [DOI] [PubMed] [Google Scholar]
- 10.Montaldi MR, Dantas RO. Swallowing evaluation in patients without restriction of oral food three months after ischemic stroke. NeuroRehabilitation. 2019;45(1):37–43. doi: 10.3233/nre-192775. [DOI] [PubMed] [Google Scholar]
- 11.May NH, Pisegna JM, Marchina S, Langmore SE, Kumar S, Pearson WG., Jr Pharyngeal swallowing mechanics secondary to hemispheric stroke. J Stroke Cerebrovasc Dis. 2017;26(5):952–961. doi: 10.1016/j.jstrokecerebrovasdis.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tadavarthi Y, Hosseini P, Reyes SE, Focht Garand KL, Pisegna JM, Pearson WG Jr. Pilot study of quantitative methods for differentiating pharyngeal swallowing mechanics by dysphagia etiology. Dysphagia. 2020:1–11. 10.1007/s00455-020-10123-0. [DOI] [PMC free article] [PubMed]
- 13.Omari TI, Ciucci M, Gozdzikowska K, Hernandez E, Hutcheson K, Jones C, et al. High-resolution pharyngeal manometry and impedance: protocols and metrics-recommendations of a high-resolution pharyngeal manometry international working group. Dysphagia. 2020;35(2):281–295. doi: 10.1007/s00455-019-10023-y. [DOI] [PubMed] [Google Scholar]
- 14.Lan Y, Xu G, Dou Z, Lin T, Yu F, Jiang L. The correlation between manometric and videofluoroscopic measurements of the swallowing function in brainstem stroke patients with dysphagia. J Clin Gastroenterol. 2015;49(1):24–30. doi: 10.1097/mcg.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 15.Lee T, Park JH, Sohn C, Yoon KJ, Lee YT, Park JH, Jung IS. Failed deglutitive upper esophageal sphincter relaxation is a risk factor for aspiration in stroke patients with oropharyngeal dysphagia. J Neurogastroenterol Motil. 2017;23(1):34–40. doi: 10.5056/jnm16028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huckabee ML, Lamvik K, Jones R. Pharyngeal mis-sequencing in dysphagia: characteristics, rehabilitative response, and etiological speculation. J Neurol Sci. 2014;343(1–2):153–158. doi: 10.1016/j.jns.2014.05.064. [DOI] [PubMed] [Google Scholar]
- 17.Juan J, Hind J, Jones C, McCulloch T, Gangnon R, Robbins J. Case study: application of isometric progressive resistance oropharyngeal therapy using the Madison oral strengthening therapeutic device. Top Stroke Rehabil. 2013;20(5):450–470. doi: 10.1310/tsr2005-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kunieda K, Kubo S, Fujishima I. New swallowing method to improve pharyngeal passage of a bolus by creating negative pressure in the esophagus-vacuum swallowing. Am J Phys Med Rehabil. 2018;97(9):e81–ee4. doi: 10.1097/phm.0000000000000872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takizawa C, Gemmell E, Kenworthy J, Speyer R. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson's disease, Alzheimer's disease, head injury, and pneumonia. Dysphagia. 2016;31(3):434–441. doi: 10.1007/s00455-016-9695-9. [DOI] [PubMed] [Google Scholar]
- 20.Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018;10(10):Cd000323. doi: 10.1002/14651858.CD000323.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henke C, Foerch C, Lapa S. Early screening parameters for dysphagia in acute ischemic stroke. Cerebrovasc Dis. 2017;44(5–6):285–290. doi: 10.1159/000480123. [DOI] [PubMed] [Google Scholar]
- 22.Leite KKA, Sassi FC, Medeiros GC, Comerlatti LR, Andrade CRF. Clinical swallowing prognostic indicators in patients with acute ischemic stroke. Arq Neuropsiquiatria. 2019;77(7):501–508. doi: 10.1590/0004-282x20190080. [DOI] [PubMed] [Google Scholar]
- 23.De Cock E, Batens K, Hemelsoet D, Boon P, Oostra K, De Herdt V. Dysphagia, dysarthria and aphasia following a first acute ischaemic stroke: incidence and associated factors. Eur J Neurol. 2020. 10.1111/ene.14385. [DOI] [PubMed]
- 24.Flowers HL, AlHarbi MA, Mikulis D, Silver FL, Rochon E, Streiner D, et al. MRI-based neuroanatomical predictors of dysphagia, dysarthria, and aphasia in patients with first acute ischemic stroke. Cerebrovasc Dis Extra. 2017;7(1):21–34. doi: 10.1159/000457810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fandler S, Gattringer T, Eppinger S, Doppelhofer K, Pinter D, Niederkorn K, Enzinger C, Wardlaw JM, Fazekas F. Frequency and predictors of dysphagia in patients with recent small subcortical infarcts. Stroke. 2017;48(1):213–215. doi: 10.1161/strokeaha.116.015625. [DOI] [PubMed] [Google Scholar]
- 26.Dunn K, Rumbach A. Incidence and risk factors for dysphagia following non-traumatic subarachnoid hemorrhage: a retrospective cohort study. Dysphagia. 2019;34(2):229–239. doi: 10.1007/s00455-018-9934-3. [DOI] [PubMed] [Google Scholar]
- 27.Fernández-Pombo A, Seijo-Raposo IM, López-Osorio N, Cantón-Blanco A, González-Rodríguez M, Arias-Rivas S, Rodríguez-Yáñez M, Santamaría-Nieto A, Díaz-Ortega C, Gómez-Vázquez E, Martínez-Olmos MÁ. Lesion location and other predictive factors of dysphagia and its complications in acute stroke. Clin Nutr ESPEN. 2019;33:178–182. doi: 10.1016/j.clnesp.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 28.Gandolfo C, Sukkar S, Ceravolo MG, Cortinovis F, Finocchi C, Gradaschi R, et al. The predictive dysphagia score (PreDyScore) in the short- and medium-term post-stroke: a putative tool in PEG indication. Neurol Sci. 2019;40(8):1619–1626. doi: 10.1007/s10072-019-03896-2. [DOI] [PubMed] [Google Scholar]
- 29.Moon HI, Yoon SY, Yi TI, Jeong YJ, Cho TH. Lesions responsible for delayed oral transit time in post-stroke dysphagia. Dysphagia. 2018;33(3):321–328. doi: 10.1007/s00455-017-9856-5. [DOI] [PubMed] [Google Scholar]
- 30.Souza JT, Ribeiro PW, de Paiva SAR, Tanni SE, Minicucci MF, Zornoff LAM, et al. Dysphagia and tube feeding after stroke are associated with poorer functional and mortality outcomes. Clin Nutr. 2019. 10.1016/j.clnu.2019.11.042. [DOI] [PubMed]
- 31.Lapa S, Luger S, Pfeilschifter W, Henke C, Wagner M, Foerch C. Predictors of dysphagia in acute pontine infarction. Stroke. 2017;48(5):1397–1399. doi: 10.1161/strokeaha.116.015045. [DOI] [PubMed] [Google Scholar]
- 32.Chang MC, Kwak SG, Chun MH. Dysphagia in patients with isolated pontine infarction. Neural Regen Res. 2018;13(12):2156–2159. doi: 10.4103/1673-5374.241466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abubakar SA, Jamoh BY. Dysphagia following acute stroke and its effect on short-term outcome. Niger Postgrad Med J. 2017;24(3):182–186. doi: 10.4103/npmj.npmj_96_17. [DOI] [PubMed] [Google Scholar]
- 34.Beharry A, Michel P, Faouzi M, Kuntzer T, Schweizer V, Diserens K. Predictive factors of swallowing disorders and bronchopneumonia in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2019;28(8):2148–2154. doi: 10.1016/j.jstrokecerebrovasdis.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 35.Carnaby G, Sia I, Crary M. Associations between spontaneous swallowing frequency at admission, dysphagia, and stroke-related outcomes in acute care. Arch Phys Med Rehabil. 2019;100(7):1283–1288. doi: 10.1016/j.apmr.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 36.Galovic M, Leisi N, Müller M, Weber J, Tettenborn B, Brugger F, Abela E, Weder B, Kägi G. Neuroanatomical correlates of tube dependency and impaired oral intake after hemispheric stroke. Eur J Neurol. 2016;23(5):926–934. doi: 10.1111/ene.12964. [DOI] [PubMed] [Google Scholar]
- 37.Ortega Barrio MÁ, Valiñas Sieiro F, Almarza Fernández MT, Bravo Santamaría S, Moreno MR. Effect of stroke on nutritional status and its relationship with dysphagia. Rev Científica Soc Enfermería Neurol (English Ed) 2020;51:13–21. doi: 10.1016/j.sedeng.2019.04.003. [DOI] [Google Scholar]
- 38.Im S, Han YJ, Kim SH, Yoon MJ, Oh J, Kim Y. Role of bilateral corticobulbar tracts in dysphagia after middle cerebral artery stroke. Eur J Neurol. 2020. 10.1111/ene.14387. [DOI] [PubMed]
- 39.Shimizu A, Maeda K, Koyanagi Y, Kayashita J, Fujishima I, Mori N. The global leadership initiative on malnutrition-defined malnutrition predicts prognosis in persons with stroke-related dysphagia. J Am Med Dir Assoc. 2019;20(12):1628–1633. doi: 10.1016/j.jamda.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 40.Suntrup S, Kemmling A, Warnecke T, Hamacher C, Oelenberg S, Niederstadt T, et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 1: dysphagia incidence, severity and aspiration. Eur J Neurol. 2015;22(5):832–838. doi: 10.1111/ene.12670. [DOI] [PubMed] [Google Scholar]
- 41.Dehaghani SE, Yadegari F, Asgari A, Chitsaz A, Karami M. Brain regions involved in swallowing: evidence from stroke patients in a cross-sectional study. J Res Med Sci. 2016;21:45. doi: 10.4103/1735-1995.183997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park T, Kim Y, Oh BM. Laryngeal closure during swallowing in stroke survivors with cortical or subcortical lesion. J Stroke Cerebrovasc Dis. 2017;26(8):1766–1772. doi: 10.1016/j.jstrokecerebrovasdis.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Calvo I, Pizzorni N, Gilardone G, Mayer F, Vanacore N, Buraschi V, Gilardone M, Corbo M. Predictors of oral feeding resumption after stroke in a rehabilitation hospital: a retrospective study. J Stroke Cerebrovasc Dis. 2019;28(7):1958–1970. doi: 10.1016/j.jstrokecerebrovasdis.2019.03.040. [DOI] [PubMed] [Google Scholar]
- 44.Moon HI, Kim GS, Lee E. Is the location of white matter lesions important in the swallowing function of older patients with mild stroke? Dysphagia. 2019;34(3):407–414. doi: 10.1007/s00455-018-9955-y. [DOI] [PubMed] [Google Scholar]
- 45.Rajappa AT, Soriano KR, Ziemer C, Troche MS, Malandraki JB, Malandraki GA. Reduced maximum pitch elevation predicts silent aspiration of small liquid volumes in stroke patients. Front Neurol. 2017;8:436. doi: 10.3389/fneur.2017.00436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schrock JW, Lou L, Ball BAW, Van Etten J. The use of an emergency department dysphagia screen is associated with decreased pneumonia in acute strokes. Am J Emerg Med. 2018;36(12):2152–2154. doi: 10.1016/j.ajem.2018.03.046. [DOI] [PubMed] [Google Scholar]
- 47.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–e418. doi: 10.1161/str.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 48.Benfield JK, Everton LF, Bath PM, England TJ. Accuracy and clinical utility of comprehensive dysphagia screening assessments in acute stroke: a systematic review and meta-analysis. J Clin Nurs. 2020;29(9-10):1527–1538. doi: 10.1111/jocn.15192. [DOI] [PubMed] [Google Scholar]
- 49.Mulheren RW, González-Fernández M. Swallow screen associated with airway protection and dysphagia after acute stroke. Arch Phys Med Rehabil. 2019;100(7):1289–1293. doi: 10.1016/j.apmr.2018.12.032. [DOI] [PubMed] [Google Scholar]
- 50.Jang S, Yang HE, Yang HS, Kim DH. Lesion characteristics of chronic dysphagia in patients with supratentorial stroke. Ann Rehabil Med. 2017;41(2):225–230. doi: 10.5535/arm.2017.41.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Im I, Jun JP, Hwang S, Ko MH. Swallowing outcomes in patients with subcortical stroke associated with lesions of the caudate nucleus and insula. J Int Med Res. 2018;46(9):3552–3562. doi: 10.1177/0300060518775290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Suntrup-Krueger S, Kemmling A, Warnecke T, Hamacher C, Oelenberg S, Niederstadt T, et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 2: oropharyngeal residue, swallow and cough response, and pneumonia. Eur J Neurol. 2017;24(6):867–874. doi: 10.1111/ene.13307. [DOI] [PubMed] [Google Scholar]
- 53.Wilmskoetter J, Bonilha L, Martin-Harris B, Elm JJ, Horn J, Bonilha HS. Mapping acute lesion locations to physiological swallow impairments after stroke. Neuroimage Clin. 2019;22:101685. doi: 10.1016/j.nicl.2019.101685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Logemann JA. Evaluation and treatment of swallowing disorders. 2. Pro-Ed: Austin; 1998. [Google Scholar]
- 55.Patel DA, Krishnaswami S, Steger E, Conover E, Vaezi MF, Ciucci MR, Francis DO. Economic and survival burden of dysphagia among inpatients in the United States. Dis Esophagus. 2018;31(1):1–7. doi: 10.1093/dote/dox131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Feng MC, Lin YC, Chang YH, Chen CH, Chiang HC, Huang LC, et al. The mortality and the risk of aspiration pneumonia related with dysphagia in stroke patients. J Stroke Cerebrovasc Dis. 2019;28(5):1381–1387. doi: 10.1016/j.jstrokecerebrovasdis.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 57.Galovic M, Stauber AJ, Leisi N, Krammer W, Brugger F, Vehoff J, Balcerak P, Müller A, Müller M, Rosenfeld J, Polymeris A, Thilemann S, de Marchis GM, Niemann T, Leifke M, Lyrer P, Saladin P, Kahles T, Nedeltchev K, Sarikaya H, Jung S, Fischer U, Manno C, Cereda CW, Sander JW, Tettenborn B, Weder BJ, Stoeckli SJ, Arnold M, Kägi G. Development and validation of a prognostic model of swallowing recovery and enteral tube feeding after ischemic stroke. JAMA Neurol. 2019;76(5):561–570. doi: 10.1001/jamaneurol.2018.4858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Scrutinio D, Battista P, Guida P, Lanzillo B, Tortelli R. Sex differences in long-term mortality and functional outcome after rehabilitation in patients with severe stroke. Front Neurol. 2020;11:84. doi: 10.3389/fneur.2020.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eltringham SA, Kilner K, Gee M, Sage K, Bray BD, Smith CJ, et al. Factors associated with risk of stroke-associated pneumonia in patients with dysphagia: a systematic review. Dysphagia. 2019:1–10. 10.1007/s00455-019-10061-6. [DOI] [PMC free article] [PubMed]
- 60.Hoffmann S, Harms H, Ulm L, Nabavi DG, Mackert BM, Schmehl I, Jungehulsing GJ, Montaner J, Bustamante A, Hermans M, Hamilton F, Göhler J, Malzahn U, Malsch C, Heuschmann PU, Meisel C, Meisel A, PREDICT Investigators Stroke-induced immunodepression and dysphagia independently predict stroke-associated pneumonia - the PREDICT study. J Cereb Blood Flow Metab. 2017;37(12):3671–3682. doi: 10.1177/0271678x16671964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Li J, Wang Y, Sun X, Lin J, Lai R, Liang J, et al. AND score: a simple tool for predicting infection in acute ischemic stroke patients without a ventilator in the Chinese population. J Int Med Res. 2019. 10.1177/0300060519888303. [DOI] [PMC free article] [PubMed]
- 62.Mao L, Liu X, Zheng P, Wu S. Epidemiologic features, risk factors, and outcomes of respiratory infection in patients with acute stroke. Ann Indian Acad Neurol. 2019;22(4):395–400. doi: 10.4103/aian.AIAN_212_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998;13(2):69–81. doi: 10.1007/PL00009559. [DOI] [PubMed] [Google Scholar]
- 64.Felix CC, Joseph ME, Daniels SK. Clinical decision making in patients with stroke-related dysphagia. Semin Speech Lang. 2019;40(3):188–202. doi: 10.1055/s-0039-1688815. [DOI] [PubMed] [Google Scholar]
- 65.Dysphagia Diagnosis and Treatment. 2nd ed: Springer International; 2019.
- 66.Restivo DA, Hamdy S. Pharyngeal electrical stimulation device for the treatment of neurogenic dysphagia: technology update. Med Devices (Auckl) 2018;11:21–26. doi: 10.2147/MDER.S122287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fraser C, Power M, Hamdy S, Rothwell J, Hobday D, Hollander I, Tyrell P, Hobson A, Williams S, Thompson D. Driving plasticity in human adult motor cortex is associated with improved motor function after brain injury. Neuron. 2002;34(5):831–840. doi: 10.1016/s0896-6273(02)00705-5. [DOI] [PubMed] [Google Scholar]
- 68.Bath PM, Scutt P, Love J, Clavé P, Cohen D, Dziewas R, Iversen HK, Ledl C, Ragab S, Soda H, Warusevitane A, Woisard V, Hamdy S, Swallowing Treatment Using Pharyngeal Electrical Stimulation (STEPS) Trial Investigators Pharyngeal electrical stimulation for treatment of dysphagia in subacute stroke: a randomized controlled trial. Stroke. 2016;47(6):1562–1570. doi: 10.1161/STROKEAHA.115.012455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Scutt P, Lee HS, Hamdy S, Bath PM. Pharyngeal electrical stimulation for treatment of poststroke dysphagia: individual patient data meta-analysis of randomised controlled trials. Stroke Res Treat. 2015;2015:429053. doi: 10.1155/2015/429053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Dziewas R, Stellato R, van der Tweel I, Walther E, Werner CJ, Braun T, et al. Pharyngeal electrical stimulation for early decannulation in tracheotomised patients with neurogenic dysphagia after stroke (PHAST-TRAC): a prospective, single-blinded, randomised trial. Lancet Neurol. 2018;17(10):849–859. doi: 10.1016/S1474-4422(18)30255-2. [DOI] [PubMed] [Google Scholar]
- 71.Muhle P, Suntrup-Krueger S, Bittner S, Ruck T, Claus I, Marian T, Schröder JB, Minnerup J, Warnecke T, Meuth SG, Dziewas R. Increase of substance P concentration in saliva after pharyngeal electrical stimulation in severely dysphagic stroke patients - an indicator of decannulation success? Neurosignals. 2017;25(1):74–87. doi: 10.1159/000482002. [DOI] [PubMed] [Google Scholar]
- 72.Suntrup S, Marian T, Schröder JB, Suttrup I, Muhle P, Oelenberg S, et al. Electrical pharyngeal stimulation for dysphagia treatment in tracheotomized stroke patients: a randomized controlled trial. Intensive Care Med. 2015;41(9):1629–1637. doi: 10.1007/s00134-015-3897-8. [DOI] [PubMed] [Google Scholar]
- 73.Chen YW, Chang KH, Chen HC, Liang WM, Wang YH, Lin YN. The effects of surface neuromuscular electrical stimulation on post-stroke dysphagia: a systemic review and meta-analysis. Clin Rehabil. 2016;30(1):24–35. doi: 10.1177/0269215515571681. [DOI] [PubMed] [Google Scholar]
- 74.Humbert IA, Poletto CJ, Saxon KG, Kearney PR, Crujido L, Wright-Harp W, Payne J, Jeffries N, Sonies BC, Ludlow CL. The effect of surface electrical stimulation on hyolaryngeal movement in normal individuals at rest and during swallowing. J Appl Physiol. 2006;101(6):1657–1663. doi: 10.1152/japplphysiol.00348.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Humbert IA, Michou E, MacRae PR, Crujido L. Electrical stimulation and swallowing: how much do we know? Semin Speech Lang. 2012;33(3):203–216. doi: 10.1055/s-0032-1320040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pisegna JM, Kaneoka A, Pearson WG, Kumar S, Langmore SE. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol. 2016;127(1):956–968. doi: 10.1016/j.clinph.2015.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liao X, Xing G, Guo Z, Jin Y, Tang Q, He B, McClure M, Liu H, Chen H, Mu Q. Repetitive transcranial magnetic stimulation as an alternative therapy for dysphagia after stroke: a systematic review and meta-analysis. Clin Rehabil. 2017;31(3):289–298. doi: 10.1177/0269215516644771. [DOI] [PubMed] [Google Scholar]
- 78.Wilkinson G, Sasegbon A, Smith CJ, Rothwell J, Bath PM, Hamdy S. An exploration of the application of noninvasive cerebellar stimulation in the neuro-rehabilitation of dysphagia after stroke (EXCITES) protocol. J Stroke Cerebrovasc Dis. 2020;29(3):104586. doi: 10.1016/j.jstrokecerebrovasdis.2019.104586. [DOI] [PubMed] [Google Scholar]
- 79.Ahn YH, Sohn HJ, Park JS, Ahn TG, Shin YB, Park M, Ko SH, Shin YI. Effect of bihemispheric anodal transcranial direct current stimulation for dysphagia in chronic stroke patients: a randomized clinical trial. J Rehabil Med. 2017;49(1):30–35. doi: 10.2340/16501977-2170. [DOI] [PubMed] [Google Scholar]
- 80.Pingue V, Priori A, Malovini A, Pistarini C. Dual transcranial direct current stimulation for Poststroke dysphagia: a randomized controlled trial. Neurorehabil Neural Repair. 2018;32(6–7):635–644. doi: 10.1177/1545968318782743. [DOI] [PubMed] [Google Scholar]
- 81.Li Y, Feng H, Li J, Wang H, Chen N, Yang J. The effect of transcranial direct current stimulation of pharyngeal motor cortex on swallowing function in patients with chronic dysphagia after stroke: a retrospective cohort study. Medicine (Baltimore) 2020;99(10):e19121. doi: 10.1097/MD.0000000000019121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Michou E, Mistry S, Jefferson S, Singh S, Rothwell J, Hamdy S. Targeting unlesioned pharyngeal motor cortex improves swallowing in healthy individuals and after dysphagic stroke. Gastroenterology. 2012;142(1):29–38. doi: 10.1053/j.gastro.2011.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Singh S, Mistry S, Jefferson S, Davies K, Rothwell J, Williams S, et al. A magnetic resonance spectroscopy study of brain glutamate in a model of plasticity in human pharyngeal motor cortex. Gastroenterology. 2009;136(2):417–424. doi: 10.1053/j.gastro.2008.10.087. [DOI] [PubMed] [Google Scholar]
- 84.Michou E, Mistry S, Rothwell J, Hamdy S. Priming pharyngeal motor cortex by repeated paired associative stimulation: implications for dysphagia neurorehabilitation. Neurorehabil Neural Repair. 2013;27(4):355–362. doi: 10.1177/1545968312469837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang C, Zheng X, Lu R, Yun W, Yun H, Zhou X. Repetitive transcranial magnetic stimulation in combination with neuromuscular electrical stimulation for treatment of post-stroke dysphagia. J Int Med Res. 2019;47(2):662–672. doi: 10.1177/0300060518807340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.• Archer SK, Smith CH, Newham DJ. Surface electromyographic biofeedback and the effortful swallow exercise for stroke-related dysphagia and in healthy ageing. Dysphagia. 2020. 10.1007/s00455-020-10129-8This article evaluates patient motivation and performance using swallowing biofeedback, bringing an interesting perspective. [DOI] [PMC free article] [PubMed]
- 87.Li CM, Wang TG, Lee HY, Wang HP, Hsieh SH, Chou M, et al. Swallowing training combined with game-based biofeedback in poststroke dysphagia. PM R. 2016;8(8):773–779. doi: 10.1016/j.pmrj.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 88.Benfield JK, Everton LF, Bath PM, England TJ. Does therapy with biofeedback improve swallowing in adults with dysphagia? A systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;100(3):551–561. doi: 10.1016/j.apmr.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 89.Park JS, Hwang NK, Kim HH, Lee G, Jung YJ. Effect of neuromuscular electrical stimulation combined with effortful swallowing using electromyographic biofeedback on oropharyngeal swallowing function in stroke patients with dysphagia: a pilot study. Medicine (Baltimore) 2019;98(44):e17702. doi: 10.1097/MD.0000000000017702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Athukorala RP, Jones RD, Sella O, Huckabee ML. Skill training for swallowing rehabilitation in patients with Parkinson's disease. Arch Phys Med Rehabil. 2014;95(7):1374–1382. doi: 10.1016/j.apmr.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 91.Perry SE, Sevitz JS, Curtis JA, Kuo SH, Troche MS. Skill training resulted in improved swallowing in a person with multiple system atrophy: an endoscopy study. Mov Disord Clin Pract. 2018;5(4):451–452. doi: 10.1002/mdc3.12628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Rogus-Pulia NM, Jones CA, Forgues AL, Orne J, Macdonald CL, Connor NP, et al. Perceived professional and institutional factors influencing clinical adoption of pharyngeal high-resolution manometry. Am J Speech-Lang Pathol. 2020. 10.1044/2020_ajslp-19-00134. [DOI] [PMC free article] [PubMed]
- 93.Morrell K, Hyers M, Stuchiner T, Lucas L, Schwartz K, Mako J, et al. Telehealth stroke dysphagia evaluation is safe and effective. Cerebrovasc Dis (Basel, Switzerland) 2017;44(3–4):225–231. doi: 10.1159/000478107. [DOI] [PubMed] [Google Scholar]
- 94.Miles A, Connor NP, Desai RV, Jadcherla S, Allen J, Brodsky M, et al. Dysphagia care across the continuum: A multidisciplinary Dysphagia Research Society taskforce report of service-delivery during the COVID-19 global pandemic. Dysphagia. 2020:1–13. 10.1007/s00455-020-10153-8. [DOI] [PMC free article] [PubMed]
- 95.Namasivayam-MacDonald AM, Riquelme LF. Speech-language pathology management for adults with COVID-19 in the acute hospital setting: Initial recommendations to guide clinical practice. Am J Speech-Lang Pathol. 2020:1–16. 10.1044/2020_ajslp-20-00096. [DOI] [PubMed]
- 96.• Eltringham SA, Smith CJ, Pownall S, Sage K, Bray B. Variation in dysphagia assessment and management in acute stroke: an interview study. Geriatrics. 2019;4(4). 10.3390/geriatrics4040060Survey study highlighting day-to-day challenges faced by medical professionals treating dysphagia in stroke. [DOI] [PMC free article] [PubMed]
- 97.Coleman ER, Moudgal R, Lang K, Hyacinth HI, Awosika OO, Kissela BM, Feng W. Early rehabilitation after stroke: a narrative review. Curr Atheroscler Rep. 2017;19(12):59. doi: 10.1007/s11883-017-0686-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Macciocchi SN, Diamond PT, Alves WM, Mertz T. Ischemic stroke: relation of age, lesion location, and initial neurologic deficit to functional outcome. Arch Phys Med Rehabil. 1998;79(10):1255–1257. doi: 10.1016/s0003-9993(98)90271-4. [DOI] [PubMed] [Google Scholar]
- 99.Cullins MJ, Connor NP. Reduced tongue force and functional swallowing changes in a rat model of post stroke dysphagia. Brain Res. 2019, 1717:160–6. 10.1016/j.brainres.2019.04.023. [DOI] [PMC free article] [PubMed]