Abstract
PURPOSE
This study evaluated the shear bond strength between 3D printed provisional resin and conventional provisional resin depending on type of conventional provisional resin and different surface treatments of 3D printed resin.
MATERIALS AND METHODS
Ninety-six disc-shaped specimens (Ø14 mm × 20 mm thickness) were printed with resin for 3D printing (Nextdent C&B, Vertex-Dental B. V., Soesterberg, Netherlands). After post-processing, the specimens were randomly divided into 8 groups (n=12) according to two types of conventional repair resin (methylmethacrylate and bis-acryl composite) and four different surface treatments: no additional treatment, air abrasion, soaking in methylmethacrylate (MMA) monomer, and soaking in MMA monomer after air abrasion. After surface treatment, each repair resin was bonded in cylindrical shape using a silicone mold. Specimens were stored in 37℃ distilled water for 24 hours. The shear bond strength was measured using a universal testing machine at a crosshead speed of 0.5 mm/min. Failure modes were analyzed by scanning electron microscope. Statistical analysis was done using one-way ANOVA test and Kruskal-Wallis test (α=.05).
RESULTS
The group repaired with bis-acryl composite without additional surface treatment showed the highest mean shear bond strength. It was significantly higher than all four groups repaired with methylmethacrylate (P<.05). Additional surface treatments, neither mechanical nor chemical, increased the shear bond strength within methylmethacrylate groups and bis-acryl composite groups (P>.05). Failure mode analysis showed that cohesive failure was most frequent in both methylmethacrylate and bis-acryl composite groups.
CONCLUSION
Our results suggest that when repairing 3D printed provisional restoration with conventional provisional resin, repair with bis-acryl composite without additional surface treatment is recommended.
Keywords: 3D printing, Provisional restoration, Shear bond strength, Surface treatment
INTRODUCTION
Computer-aided design/computer-aided manufacturing (CAD/CAM) technology has created a new modality for fabricating provisional prostheses.1 On the first visit in clinic, the patient's information is acquired using an intraoral scanner. Using the CAD program, fabrication of prostheses is easily done, and the saved data allow the clinicians to modify and reproduce the prostheses at any time. Compared to conventional laboratory work, efficiency and predictability for the definitive restoration are also important advantages of the new CAD/CAM methods.2,3
There are two methods in fabricating provisional prostheses in CAD/CAM technology: subtractive and additive manufacturing. In subtractive manufacturing, also known as milling, a computer controlled machine cuts away material from a prefabricated block using specific cutting tools. The limitation of this method is that the fabrication of prostheses is affected by the smallest milling tool radius, and thus complex geometries are difficult to reproduce.4 Also, used tools show signs of wear after repeated use, which can lead to cracks in the prostheses.5 From an ecological view, milling method produces more waste regarding how much is used in the final product.6
On the other hand, additive manufacturing, also known as 3D printing, creates a 3D object by stacking materials layer upon layer. In contrast to the subtractive method, additive method saves material as it only uses as much the amount as the final product, and is able to produce more complex geometries. Furthermore, 3D printed provisional restorations are known to have sufficient mechanical properties for intraoral use compared to conventionally cured provisional materials.7 As a result, this additive manufacturing method, 3D printing, is now a suitable option in fabricating prostheses in the dental field.5
Despite the many advantages of 3D printed provisional prostheses, chairside modification is still necessary in clinical practice. Because the provisional crown and bridge are prefabricated before tooth preparation, chairside relining after tooth preparation is required to improve the fit of the margin area. Also, for gradual molding of the soft tissue under ovate pontic, correction of the proximal contact and occlusion based on treatment plan, and repair of the damaged prostheses, adding of conventional provisional resin to 3D printing resin is inevitable.8 Although it would be ideal to remake the provisional restoration, it is economically advantageous to repair it at the chairside.9 Provisional resins such as monomethacrylates and dimethacrylates are commonly used for chairside modification.10 Although creating a durable bond between the 3D printed restoration and the conventional repair resin is crucial for its success, limited information is available on the compatibility between two materials.
The aim of this study was to evaluate the shear bond strength between 3D printed provisional resin and conventional provisional resin depending on two types of conventional provisional resin (methylmethacrylate and bis-acryl composite) and four different surface treatments (no additional treatment, air abrasion, soaking in methylmethacrylate (MMA) monomer, and MMA monomer soaking after air abrasion) of 3D printed resin. The null hypotheses were that (i) there is no difference in the shear bond strength depending on the type of conventional repair resin and (ii) there is no difference in the shear bond strength depending on different surface treatments of 3D printed resin.
MATERIALS AND METHODS
Materials in this study were selected based on usage and long-term verification in clinical practice (Table 1).11 96 discshaped specimens of 3D printing resin were fabricated in size of 20 mm in diameter and 14 mm in thickness using a 3D printer (cara Print 4.0, Kulzer, Hanau, Germany) by digital light processing (DLP) method. Specimens were printed in 0 degree angle, where supports were placed on the opposite side of the testing surface. After removing the supports, the specimens were cleaned in distilled water for 20 minutes using an ultrasonic cleaner (SD-120H, Mujigae Co., Seoul, Korea) and dried with oil-free compressed air for 20 seconds.
Table 1. Materials experimented in this study.
| Material | Composition | Manufacturer | |
|---|---|---|---|
| 3D printing resin | Nextdent C&B | Monomethacrylate (Polymethylmethacrylate resin) | Vertex-Dental B. V., Soesterberg, Netherlands |
| Conventional resin | Jet | Methylmethacrylate (Polymethylmethacrylate resin) | Lang, Wheeling, IL, USA |
| Luxatemp | Dimethacrylate (Bis-acryl composite resin) | DMG, Hamburg, Germany | |
| Monomer liquid | Jet | Methylmethacrylate | Lang, Wheeling, IL, USA |
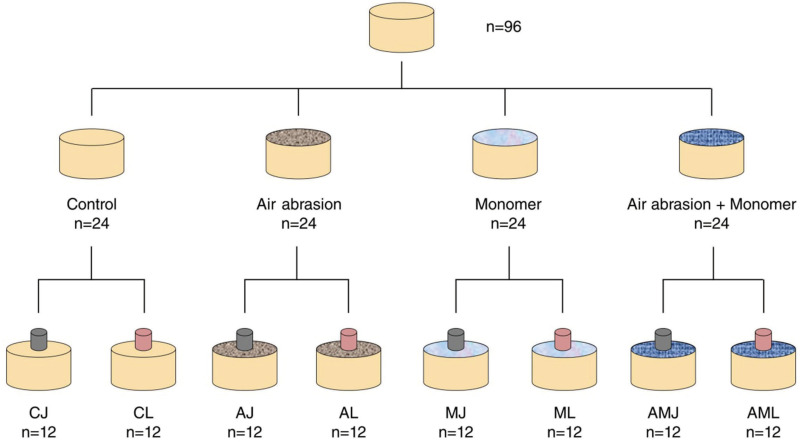
The cleaned specimens were randomly divided into 8 groups of 12 specimens based on 2 types of conventional repair resins and 4 different surface treatments (Table 2). The surface treatments were as follows:
Table 2. Classification and abbreviations of test groups.
| Surface treatments | |||||
|---|---|---|---|---|---|
| Control | Air abrasion | Monomer | Air abrasion + Monomer | ||
| Type of repair resin | Jet (methylmethacrylate) | CJ | AJ | MJ | AMJ |
| Luxatemp (bis-acryl composite) | CL | AL | ML | AML | |
(1) Control: no additional surface treatment.
(2) Air abrasion: air abrasion with 50-µm aluminum oxide(Al2O3) particles using an airborne-particle abrasion device (Cobra, Renfert GmbH, Hilzinge, Germany) from a distance of 10 mm, at a pressure of 0.2 MPa for 10 seconds. The specimen was rinsed with water for 10 seconds using a steam cleaner (SESY2014 New Beginning, SEKI Industry, Seoul, Korea) and dried with oil-free compressed air for 10 seconds.
(3) Monomer: specimen was soaked in methylmethacrylate monomer liquid for 60 seconds.
(4) Monomer soaking after air abrasion (Air abrasion + Monomer): air abrasion process was done under the same condition as above. Then, the specimen was soaked in monomer liquid for 60 seconds.
The experiment design is presented in Fig. 1.
Fig. 1. Experiment design.
One specimen from each surface treatment group was randomly selected for surface examination. The conditioned surfaces of specimens were observed at × 500 and × 1000 magnification using a scanning electron microscope (SEM) (ZEISS GeminiSEM 500, Carl Zeiss Corp., Oberkochen, Germany).
The bonding of conventional provisional resins was performed using a customized silicone mold (Mold master ultra, Molkang, Yangju, Korea) to reduce the error in bonding (Fig. 2). The repair resin was in a cylindrical shape of 2.38 mm in diameter and 3 mm in thickness and was left to polymerize at 23℃ for 60 minutes. The bonded specimens were stored in distilled water at 37℃ for 24 hours.
Fig. 2. Silicone mold for bonding conventional resins.
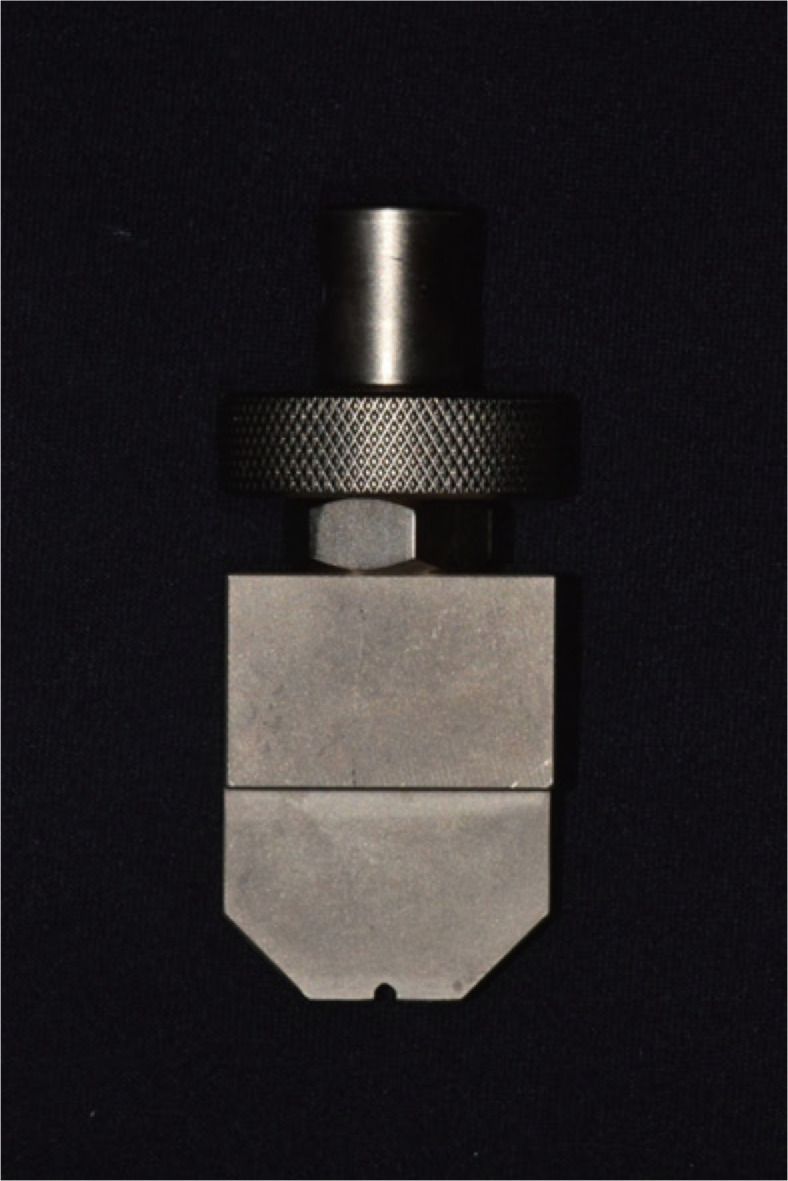
Shear bond strength was measured on a universal testing machine (QM100TS, QMESYS, Seoul, Korea). Custom rod was fabricated (Fig. 3) for exact measurement and loaded at the crosshead speed of 0.5 mm/min on the bonding interface. The maximum load (N) was recorded when fracture occurred. The shear bond strength was calculated by applying the obtained values into the following equation:
Fig. 3. Customized rod for shear bond strength test.
| σ = F / A |
where σ is the bond strength (MPa), F is the load at failure (N), and A is the repaired area (mm2).
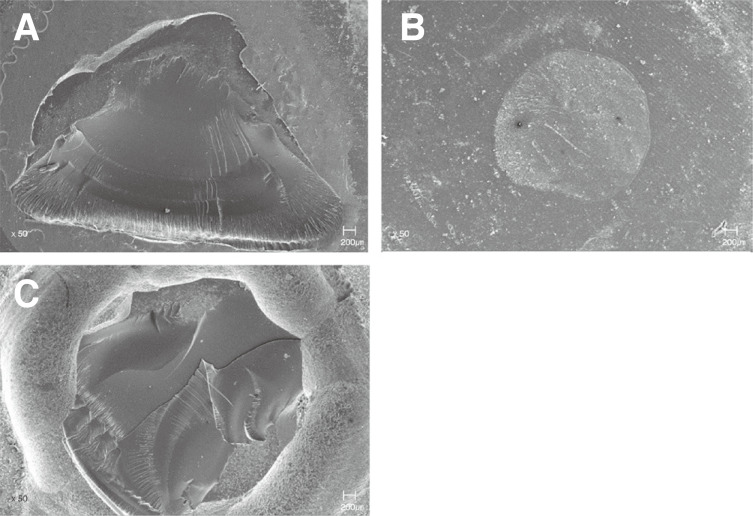
After shear bond strength test, the interfacial fractured surfaces were observed at × 50 magnification using a scanning electron microscope (ZEISS GeminiSEM 500, Carl Zeiss Corp., Oberkochen, Germany). The specimens were classified into 3 groups according to fracture patterns: cohesive failure, adhesive failure, and mixed failure (combination of cohesive and adhesive failure).
The statistical analysis was done using IBM SPSS Statistics v23.0 (IBM Corp., Armonk, NY, USA). Kruskal-Wallis test was performed to assess the effect of different surface treatments on shear bond strength among Jet groups, and one-way ANOVA test for Luxatemp groups. Post hoc test was done using Mann-Whitney U test and Tukey HSD test. The level of statistical significance was set at 5%.
RESULTS
Table 3 shows the mean and standard deviation of shear bond strength.
Table 3. Mean and standard deviation of shear bond strengths (unit: MPa).
| Materials | Surface treatment | Total mean | |||
|---|---|---|---|---|---|
| Control | Air abrasion | Monomer | Air abrasion + Monomer | ||
| Jet | 1.64a (0.80) | 2.07ac (0.89) | 1.45a (0.50) | 1.68ad (1.08) | 1.71 (0.84) |
| Luxatemp | 2.77b (0.61) | 2.38bc (0.85) | 2.76bc (1.08) | 2.25bcd (0.56) | 2.54 (0.81) |
Same superscripted letters indicate no significant difference at level of 0.05.
When comparing the total mean shear bond strength between Jet and Luxatemp, the total mean of Luxatemp was significantly higher (Table 3). Within Luxatemp groups, group CL showed the highest bond strength and group AML showed the lowest bond strength, but the results showed no statistically significant difference among different surface treatments (P > .05). Within Jet groups, group AJ showed the highest bond strength and group MJ showed the lowest bond strength, but there was also no statistically significant difference among different surface treatments (P > .05). When all 8 groups were compared, the shear bond strength of group CL was significantly higher than all of the Jet groups. Group AJ did not show significant difference in bond strength compared to group AL, ML, and AML.
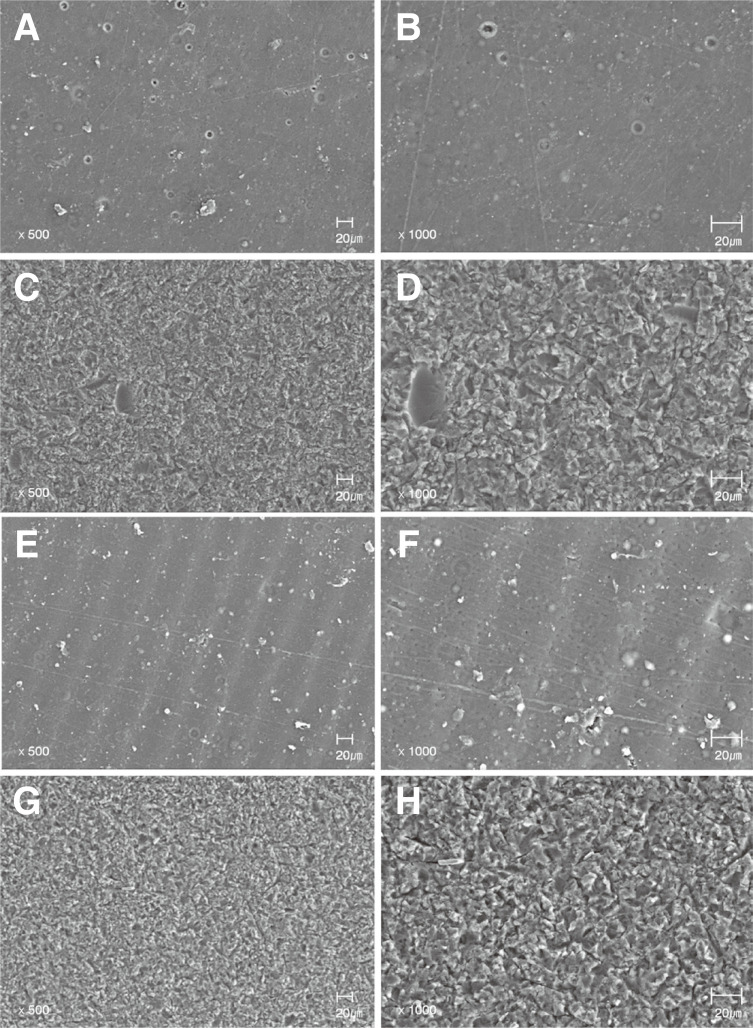
SEM images showed different topographic patterns among specimens (Fig. 4A to 4H). The surface of Control group was relatively smooth (Fig. 4A and 4B), whereas Air abrasion group showed roughened surface (Fig. 4C and 4D). The Monomer group showed micro-irregularities (Fig. 4E and 4F) and the Air abrasion + Monomer group showed the roughness more clearly (Fig. 4G and 4H).
Fig. 4. Scanning electron micrographs of specimens. (A) Control group (magnification × 500), (B) Control group (magnification × 1000), (C) Air abrasion group (magnification × 500), (D) Air abrasion group (magnification × 1000), (E) Monomer group (magnification × 500), (F) Monomer group (magnification × 1000), (G) Air abrasion + Monomer group (magnification × 500), (H) Air abrasion + Monomer group (magnification × 1000).
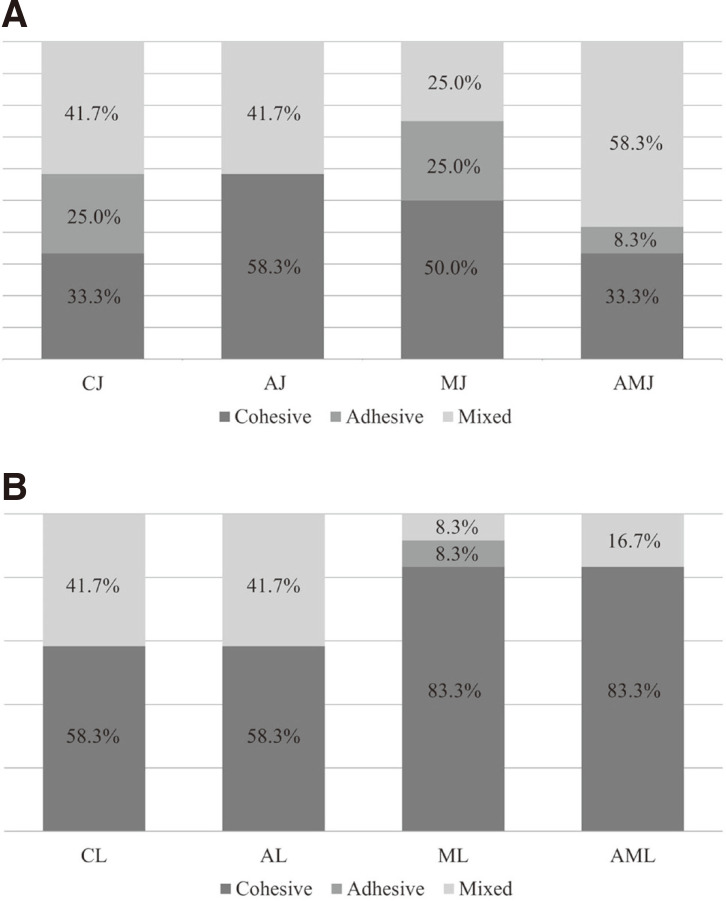
SEM images in Fig. 5 represent each failure mode. Failure mode distribution of the experiment groups are shown in Fig. 6. Cohesive failure was the most frequent in both Jet and Luxatemp groups. The percentage of cohesive failure was higher in Luxatemp groups than that of Jet groups. All of the cohesive failures occurred in 3D printed resin layer, not the repair resin layer.
Fig. 5. Scanning electron micrographs of failure modes. (A) Cohesive failure (magnification × 50), (B) Adhesive failure (magnification × 50), (C) Mixed failure (magnification × 50).
Fig. 6. Failure mode distribution. (A) Jet groups, (B) Luxatemp groups.
CJ: Control Jet, AJ: Air abrasion Jet, MJ: Monomer Jet, AMJ: Air abrasion + Monomer Jet. CL: Control Luxatemp, AL: Air abrasion Luxatemp, ML: Monomer Luxatemp, AML: Air abrasion + Monomer Luxatemp.
DISCUSSION
The aim of this study was to evaluate the shear bond strength between 3D printed provisional resin and conventional provisional resin depending on (1) the type of conventional provisional resin and (2) different surface treatments. The null hypotheses were that (i) there is no difference in the shear bond strength depending on the type of conventional resin and (ii) there is no difference in the shear bond strength depending on different surface treatments. The first null hypothesis was rejected as the Luxatemp showed better shear bond strength compared to Jet. The second null hypothesis was accepted as there was no statistically significant difference depending on different surface treatments within both Jet and Luxatemp groups.
Measurement of shear bond strength may differ in same material according to the shape of the loading rod.12 In the study of Oliveira et al.,13 shear bond strength of composite resin bonded to enamel surface showed significantly higher value when the width of the shearing blade was smaller. Sinhoreti et al.14 also reported that tensions were initially concentrated close to the loading area and then evolved to more complex tensions in the entire system (cleavage effort). Thus in the present study, custom rod was fabricated to match the diameter of bonding specimen for accurate measurement.
Improving the bond strength between two materials involves increasing the surface roughness to promote mechanical retention and application of a bonding agent to promote chemical bonding.11,15,16,17 In the present study, airborne particle abrasion using 50 µm Aluminum oxide (Al2O3) was selected for mechanical treatment. To evaluate the sole effect of airborne particle abrasion, other means of mechanical surface treatment, such as polishing or grinding with silicone carbide paper, were excluded. Although Air abrasion groups showed micro-retentive features in SEM images, there was no statistically significant difference in shear bond strength compared to Control groups. This was different from the previous study experimenting with the same 3D printed resin (Nextdent C&B, Vertex-Dental B. V., Soesterberg, Netherlands). Jeong and Kim11 reported that air abrasion (50 µm aluminum oxide (Al2O3), 10 mm distance, 10 seconds) after grinding with 220-grit silicon-carbide paper improved the shear bond strength of Luxatemp to 3D printed resin when compared with the non-treated (control) group. The reason for this difference may be due to additional surface roughness by silicon-carbide paper grinding. Thus in clinical practice, air abrasion alone may be not enough to improve mechanical bonding of repair resin. Furthermore, although specimens of group AJ and AL had the same surface roughness under the same air abrasion condition, group AJ showed improved shear bond strength compared to group CJ, while group AL showed lower shear bond strength compared to group CL. This implies air abrasion may be effective for Jet, but not for Luxatemp. The reason for this difference may be due to (1) the viscosity of the conventional provisional resins or (2) the layered structure of the 3D printed resin. Papacchini et al.18 reported that the shear bond strength of repair resin improved when the viscosity decreased due to its ability to flow into the micro-retentions. Jet showed lower viscosity compared to Luxatemp in this study (Jet was mixed in 4:3 p/l ratio in present study), and thus was able to achieve higher result in Air abrasion group. For another explanation, materials with layered structure may show different bonding behaviors according to different regions within the material, depending on the extent of cross-linking of the resin molecules and the structural layering of the resin.19 The exposed surface of 3D printing resin after air abrasion may show different bonding behaviors to methylmethacrylate and bis-acryl composite resin. Further studies should investigate this difference.
In previous studies, various bonding agents were suggested to promote chemical bonding between CAD/CAM polymethylmethacrylate (PMMA) resin and conventional resin.11,20,21,22 Some studies have suggested the use of all-in-one bonding agent such as Single bond universal (3M ESPE, St. Paul, MN, USA), but it did not strengthen the bond.11,16,17,23 The hydrophilic monomers in the bonding agent, such as HEMA, tend to absorb water and weaken the interfacial bond.11,16 Other studies suggested using bonding agents containing methylmethacrylate (MMA) monomer, which significantly improved the shear bond strength compared to the non-pretreated group.20,21,22,24 MMA monomers dissolve the surface of CAD/CAM PMMA blank resin, creating free carbon double bonds that form new polymer chains with the repair resin. For this reason, MMA monomer was chosen as the intermediate to promote chemical bonding in this study. Also, it had the advantage of not having to purchase an additional primer for bonding.
By applying MMA monomer, the surface of 3D printed resin was dissolved and swelled. In SEM images of Monomer group, long groove-like-microretentive features were observed. Therefore, it was expected that MMA monomer treated groups may increase the shear bond strength both mechanically and chemically. However, group MJ and ML did not show significant increase in bond strength compared to group CJ and CL. Unlike CAD/CAM PMMA milling block, 3D printed PMMA resin is a light curing material with bifunctional monomers. Palitsch et al.25 reported that methylmethacrylate does not appropriately copolymerize with the bifunctional monomers of the light-curing denture base materials, and thus MMA is not an appropriate conditioning liquid. Therefore, MMA may not be an appropriate intermediate for 3D printed provisional resin. This may also explain why Jet showed lower mean bond strength compared to Luxatemp. Jet contains MMA monomer in its compound, which counteracts with the bonding process to 3D printed resin.
In failure mode analysis, cohesive failure was the most frequent in both Jet and Luxatemp groups. All of the cohesive failures occurred in 3D printed resin layer. Thus, chairside repair with both Jet and Luxatemp is expected to show satisfactory result in clinical practice. Furthermore, Luxatemp showed more cohesive and less adhesive failures compared to Jet. Therefore, repair with bis-acryl composite will show more reliable bond compared to methylmethacrylate to 3D printed resin.
In the present study, none of the test methods represented the intraoral environment. Thermocycling may act in two different ways on the bonding behaviors between 3D printing resin and conventional provisional resin. On one hand, it may lead to mechanical stress on the bonding interface, creating cracks and impairment of the bonding.26 On the other hand, thermocycling may increase the shear bond strength by intensifying the process of post-polymerization between 3D printing resin and conventional repair resin.27 Further studies should evaluate the effect of long-term aging of the bonded conventional provisional resin to 3D printed restoration.
CONCLUSION
Within the limitation of present study, the following conclusions were drawn. Bis-acryl composite resin showed higher shear bond strength to 3D printed resin compared to methylmethacrylate. Additional surface treatments, neither mechanical nor chemical, increased the shear bond strength between 3D printed provisional resin and conventional provisional resin. Thus, when repairing 3D printed provisional restoration with conventional provisional resin, repair with bis-acryl composite without additional surface treatment is recommended.
References
- 1.Mainjot AK, Dupont NM, Oudkerk JC, Dewael TY, Sadoun MJ. From artisanal to CAD-CAM blocks: State of the art of indirect composites. J Dent Res. 2016;95:487–495. doi: 10.1177/0022034516634286. [DOI] [PubMed] [Google Scholar]
- 2.Beuer F, Schweiger J, Edelhoff D. Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J. 2008;204:505–511. doi: 10.1038/sj.bdj.2008.350. [DOI] [PubMed] [Google Scholar]
- 3.Gilbert S, Keul C, Roos M, Edelhoff D, Stawarczyk B. Bonding between CAD/CAM resin and resin composite cements dependent on bonding agents: three different in vitro test methods. Clin Oral Investig. 2016;20:227–236. doi: 10.1007/s00784-015-1494-4. [DOI] [PubMed] [Google Scholar]
- 4.Strub JR, Rekow ED, Witkowski S. Computer-aided design and fabrication of dental restorations: current systems and future possibilities. J Am Dent Assoc. 2006;137:1289–1296. doi: 10.14219/jada.archive.2006.0389. [DOI] [PubMed] [Google Scholar]
- 5.Kessler A, Hickel R, Reymus M. 3D Printing in Dentistry-State of the Art. Oper Dent. 2020;45:30–40. doi: 10.2341/18-229-L. [DOI] [PubMed] [Google Scholar]
- 6.van Noort R. The future of dental devices is digital. Dent Mater. 2012;28:3–12. doi: 10.1016/j.dental.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 7.Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, Ferracane JL, Bertassoni LE. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018;34:192–200. doi: 10.1016/j.dental.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burns DR, Beck DA, Nelson SK Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J Prosthet Dent. 2003;90:474–497. doi: 10.1016/s0022-3913(03)00259-2. [DOI] [PubMed] [Google Scholar]
- 9.Koumjian JH, Nimmo A. Evaluation of fracture resistance of resins used for provisional restorations. J Prosthet Dent. 1990;64:654–657. doi: 10.1016/0022-3913(90)90290-s. [DOI] [PubMed] [Google Scholar]
- 10.Revilla-León M, Meyers MJ, Zandinejad A, Özcan M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J Esthet Restor Dent. 2019;31:51–57. doi: 10.1111/jerd.12438. [DOI] [PubMed] [Google Scholar]
- 11.Jeong KW, Kim SH. Influence of surface treatments and repair materials on the shear bond strength of CAD/CAM provisional restorations. J Adv Prosthodont. 2019;11:95–104. doi: 10.4047/jap.2019.11.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mondragon E, Söderholm KJ. Shear strength of dentin and dentin bonded composites. J Adhes Dent. 2001;3:227–236. [PubMed] [Google Scholar]
- 13.Oliveira AC, Oshima HM, Mota EG, Grossi ML. Influence of chisel width on shear bond strength of composite to enamel. Revista Odonto Ciência. 2009;24:19–21. [Google Scholar]
- 14.Sinhoreti MA, Consani S, De Goes MF, Sobrinho LC, Knowles JC. Influence of loading types on the shear strength of the dentin-resin interface bonding. J Mater Sci Mater Med. 2001;12:39–44. doi: 10.1023/a:1013848901553. [DOI] [PubMed] [Google Scholar]
- 15.da Costa TR, Serrano AM, Atman AP, Loguercio AD, Reis A. Durability of composite repair using different surface treatments. J Dent. 2012;40:513–521. doi: 10.1016/j.jdent.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 16.Ha SR, Kim SH, Lee JB, Han JS. Improving shear bond strength of temporary crown and fixed dental prosthesis resins by surface treatments. J Mater Sci. 2016;51:1463–1475. [Google Scholar]
- 17.Brosh T, Pilo R, Bichacho N, Blutstein R. Effect of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent. 1997;77:122–126. doi: 10.1016/s0022-3913(97)70224-5. [DOI] [PubMed] [Google Scholar]
- 18.Papacchini F, Magni E, Radovic I, Mazzitelli C, Monticellia F, Goracci C, Polimeni A, Ferrari M. Effect of intermediate agents and pre-heating of repairing resin on composite-repair bonds. Oper Dent. 2007;32:363–371. doi: 10.2341/06-105. [DOI] [PubMed] [Google Scholar]
- 19.Papazoglou E, Vasilas AI. Shear bond strengths for composite and autopolymerized acrylic resins bonded to acrylic resin denture teeth. J Prosthet Dent. 1999;82:573–578. doi: 10.1016/s0022-3913(99)70056-9. [DOI] [PubMed] [Google Scholar]
- 20.Gilbert S, Keul C, Roos M, Edelhoff D, Stawarczyk B. Bonding between CAD/CAM resin and resin composite cements dependent on bonding agents: three different in vitro test methods. Clin Oral Investig. 2016;20:227–236. doi: 10.1007/s00784-015-1494-4. [DOI] [PubMed] [Google Scholar]
- 21.Bähr N, Keul C, Edelhoff D, Eichberger M, Roos M, Gernet W, Stawarczyk B. Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent Mater J. 2013;32:492–501. doi: 10.4012/dmj.2012-329. [DOI] [PubMed] [Google Scholar]
- 22.Keul C, Martin A, Wimmer T, Roos M, Gernet W. Tensile bond strength of PMMA- and composite-based CAD/CAM materials to luting cements after different conditioning methods. Inter J Adhe Adhe. 2013;46:122–127. [Google Scholar]
- 23.Hisamatsu N, Atsuta M, Matsumura H. Effect of silane primers and unfilled resin bonding agents on repair bond strength of a prosthodontic microfilled composite. J Oral Rehabil. 2002;29:644–648. doi: 10.1046/j.1365-2842.2002.00899.x. [DOI] [PubMed] [Google Scholar]
- 24.Vallittu PK, Lassila VP. Wetting the repair surface with methylmethacrylate affects the transverse strength of repaired heat-polymerized resin. J Prosthet Dent. 1994;72:639–643. doi: 10.1016/0022-3913(94)90297-6. [DOI] [PubMed] [Google Scholar]
- 25.Palitsch A, Hannig M, Ferger P, Balkenhol M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: the role of conditioning liquids. J Dent. 2012;40:210–221. doi: 10.1016/j.jdent.2011.12.010. [DOI] [PubMed] [Google Scholar]
- 26.Torstenson B, Brännström M. Contraction gap under composite resin restorations: effect of hygroscopic expansion and thermal stress. Oper Dent. 1988;13:24–31. [PubMed] [Google Scholar]
- 27.Piwowarczyk A, Lauer HC, Sorensen JA. In vitro shear bond strength of cementing agents to fixed prosthodontic restorative materials. J Prosthet Dent. 2004;92:265–273. doi: 10.1016/j.prosdent.2004.06.027. [DOI] [PubMed] [Google Scholar]