Abstract
Background
Reducing the need for hospitalisation in patients with chronic obstructive pulmonary disease (COPD) is an important goal in COPD management. The aim of this study was to evaluate re-hospitalisation, treatment, comorbidities and mortality in patients with COPD who were hospitalised for the first time due to a COPD exacerbation.
Methods
This was a retrospective, population-based observational cohort study of Swedish patients using linked data from three mandatory national health registries to assess re-hospitalisation rates, medication use and mortality. Rate of hospitalisation was calculated using the number of events divided by the number of person-years at risk; risk of all-cause and COPD-related mortality were assessed using Cox proportional hazard models.
Results
In total, 51,247 patients were identified over 10 years; 35% of patients were not using inhaled corticosteroid, long-acting muscarinic antagonist or long-acting β2-agonist treatment prior to hospitalisation, 38% of whom continued without treatment after being discharged. Re-hospitalisation due to a second severe exacerbation occurred in 11.5%, 17.8% and 24% of the patients within 30, 90 and 365 days, respectively. Furthermore, 24% died during the first year following hospitalisation and risk of all-cause and COPD-related mortality increased with every subsequent re-hospitalisation. Comorbidities, including ischaemic heart disease, heart failure and pneumonia, were more common amongst patients who were re-hospitalised than those who were not.
Conclusion
Following hospitalisation for first severe COPD exacerbation, many patients did not collect the treatment recommended by current guidelines. Risk of mortality increased with every subsequent re-hospitalisation. Patients with concurrent comorbidities had an increased risk of being re-hospitalised.
Keywords: COPD, re-hospitalisation, management, mortality
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous and progressive disease characterised by chronic airflow limitation.1,2 Patients typically endure intermittent exacerbations of varying frequency that are characterised by acute deterioration in symptoms of chronic breathlessness, cough and sputum production.3,4 Severe exacerbations that result in hospitalisation are resource demanding3 and re-hospitalisation is common following discharge.4 In addition, hospitalisation is associated with a high risk of mortality following discharge.5 Therefore, reducing the risk of hospitalisations is an important goal in COPD management.2
The GOLD 2020 guidelines recommended treating COPD with either monotherapy or combination therapy comprising bronchodilators (long-acting muscarinic antagonists [LAMAs] or long-acting β2-agonists [LABAs]) and inhaled corticosteroids (ICS).2 The exact treatment is based on the nature and severity of an individual’s disease and may be escalated in the event of a deterioration in disease status.2 For patients with exacerbations, ICS/LABA or LAMA/LABA combinations form a vital part of the treatment regimen, with a more aggressive approach required for severe exacerbations, particularly in the event of acute respiratory failure.2,6 Suboptimal treatment may contribute to worse outcomes and increased healthcare burden for the society and the individual patient.
The aim of this study was to evaluate re-hospitalisation, treatment, comorbidities and mortality in patients with COPD who were hospitalised for the first time due to a COPD exacerbation and to identify risk factors for re-hospitalisation and mortality.
Methods
Study Design and Data Sources
This was a population-based observational study in Sweden using data from three mandatory national health registries: The National Patient Register (NPR), covering all hospital admissions since 1987 and outpatient specialist visits since 2001;7 the Prescribed Drug Registry, covering all collected outpatient drug prescriptions since July 2005 using Anatomical Therapeutic Chemical (ATC) codes;8 and the Cause of Death Register, covering data on cause of death from all people registered in Sweden.9 Individual patient data were linked by the Swedish National Board of Health and Welfare using each individual’s unique personal identification number. Exacerbations were defined as either pharmacy collection of oral corticosteroids (OCS) or respiratory antibiotics (tetracyclines or penicillin with extended spectrum), or emergency visits and/or hospitalisations due to COPD. The study protocol was approved by the Stockholm Regional Ethics Committee (registration number 2017/4:2).
Study Population and Follow-Up
The study population included all patients aged ≥40 years hospitalised with a first severe COPD exacerbation as a main diagnosis (International Classification of Diseases-10 diagnosis [ICD-10]10 code J44: [COPD11]) in inpatient secondary care during the observation period between 1 January 2006 and 31 December 2015. The index date was the date of the first hospitalisation with COPD as a primary diagnosis; baseline was the 12-month period pre-index. Patients were followed prospectively from index until date of death, emigration or end of follow-up (up to 11 years), whichever occurred first (Figure 1). Medications were assessed during the 4 months prior to index and for 4 months after. Exclusion criteria included inpatient hospital visits with a diagnosis of COPD between 1 January 1997 and 1 January 2006 and immigration to Sweden <5 years prior to index.
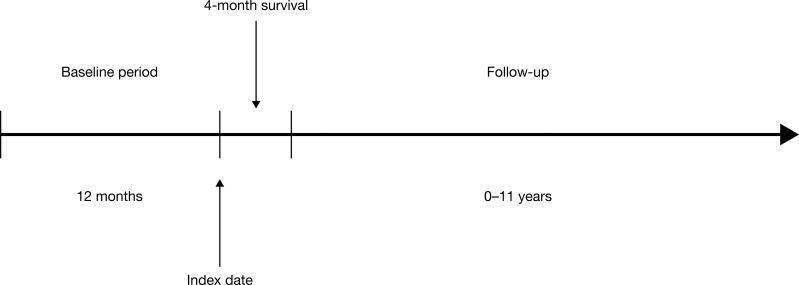
Figure 1.
Study timeline. The index date was date of the first hospitalisation with COPD as a primary diagnosis; baseline was the 12-month period pre-index. Patients had to have survived for ≥4 months post-index and were followed prospectively from index until date of death, emigration or end of follow-up (up to 11 years).
Assessments and Characterisations
Data were collected as follows: demographics (age, sex), mortality (all-cause mortality and COPD-related mortality), healthcare resource utilisation, hospital admissions, hospital outpatient visits and drugs dispensed from pharmacies, comorbidity (respiratory-related conditions [eg, chronic lower respiratory diseases and pneumonia] and other relevant conditions [eg, cancer, diabetes, cardiovascular diseases, rheumatoid arthritis and osteoporosis/fractures] according to ICD-10 codes) and treatment patterns (prescription of drugs for obstructive airway diseases [eg, ICS, LAMA, LABA and short-acting β2-agonists] and relevant concomitant medication [eg, antibiotics, antivirus, anti-allergy, antihistamines and antidepressants] according to ATC codes).
Statistical Analyses
Baseline characteristics were described as mean (standard deviation [SD]) for continuous variables and absolute and relative frequencies for categorical variables. Rate of hospitalisation was calculated using the number of events divided the by number of person-years at risk. Confidence intervals (95% CI) for rates were derived by approximating the Poisson distribution by a normal distribution.
Risk factors for re-hospitalisation within 30, 90 and 365 days were explored by odds ratios (OR) with 95% CI using logistic regression models. Among patients followed for ≥12 months, risk of all-cause and COPD-related mortality by post-index re-hospitalisations was assessed by hazard ratios (HR) with 95% CI using Cox proportional hazard models. Estimates adjusted for sex, index age, baseline comorbidities and baseline COPD treatment were calculated. Change in medication before and after the first hospitalisation was calculated for patients who were not re-hospitalised during up to 4 months of follow-up.
Results
In total, 51,247 patients were included in this study; 54.8% were female, mean age was 74.6 years and 39.3% had experienced moderate exacerbations during the 12 months preceding hospitalisation (the baseline period; Table 1). Of these, 18,167 (35.4%) patients had no previous maintenance treatment with ICS or long-acting bronchodilators, whereas 27.7% were collecting ICS, LAMA and LABA combined as triple therapy. Hypertension (20.7%), heart failure (15.4%) and ischaemic heart disease (14.2%) were the most common comorbidities (Table 1). Concomitant treatment for any cardiovascular-related comorbidities was also common (77.4%) and 42.1% of patients were collecting beta-blockers (online supplementary Table 1). More than a quarter of patients (27.2%) were collecting concomitant antidepressants.
Table 1.
Baseline Patient Demographics and Characteristics
| Patient Population (n=51,247) | |
|---|---|
| Females, n (%) | 28,087 (54.8) |
| Age, mean years (SD) | 74.6 (10.1) |
| Moderate COPD exacerbation, n (%) a,b | 20,157 (39.3) |
| Respiratory treatment, n (%)c | |
| Neither LAMA, LABA or ICS | 18,167 (35.4) |
| ICS monotherapy | 2093 (4.1) |
| LAMA or LABA monotherapy | 6910 (13.5) |
| LAMA/LABA | 1015 (2.0) |
| ICS/LAMA or ICS/LABA | 8857 (17.3) |
| ICS/LAMA/LABA | 14,205 (27.7) |
| SABA monotherapy | 16,367 (31.9) |
| N-acetylcysteine | 14,707 (28.7) |
| PD4 antagonists | 301 (0.6) |
| Comorbidities, n (%)b | |
| Hypertensive diseases | 10,620 (20.7) |
| Heart failure | 7876 (15.4) |
| Ischaemic heart disease | 7253 (14.2) |
| Pneumonia | 6384 (12.5) |
| Diabetes | 5094 (9.9) |
| Malignant neoplasm | 4913 (9.6) |
| Metabolic disorders | 3340 (6.5) |
| Asthma | 3193 (6.2) |
| Other respiratory system diseases | 2901 (5.7) |
| Cerebrovascular diseases | 2632 (5.1) |
Notes: aRequired additional medication in addition to maintenance treatment, eg systemic corticosteroids or antibiotics. bExacerbation and comorbidity data were collected during a 12-month period pre-index date. cCOPD treatments were collected during a 4-month period pre-index date.
Abbreviations: COPD, chronic obstructive pulmonary disease; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; PD4, phosphodiesterase-4; SABA, short-acting β2-agonist; SD, standard deviation.
Treatment Patterns
Of the total patient population, 39,181 patients had ≥12 months of follow-up. Of these, there was an increase in the use of ICS or long-acting bronchodilator maintenance treatments during follow-up versus baseline (Table 2) and the proportion of patients collecting triple therapy increased from 28.1% during baseline to 42.9% during follow-up. However, 16.6% of patients still did not collect maintenance treatment with LAMA, LABA or ICS during follow-up.
Table 2.
Exacerbations, COPD-Related Medication and Hospital-Based Outpatient Visits at Baseline and During Follow-Up (n=39,181)
| Baseline | 12-Month Follow-Up | |
|---|---|---|
| Patients with ≥1 exacerbations, n (%) | ||
| Any | 15,368 (39.2) | 20,544 (52.4) |
| Moderate | 15,368 (39.2) | 16,978 (43.3) |
| Severe | N/A | 9376 (23.9) |
| Respiratory treatment, n (%) | ||
| Neither LAMA, LABA or ICS | 13,970 (35.7) | 6513 (16.6) |
| ICS monotherapy | 1602 (4.1) | 1267 (3.2) |
| LAMA or LABA monotherapy | 5051 (12.9) | 6109 (15.6) |
| LAMA/LABA | 767 (2.0) | 1098 (2.8) |
| ICS/LAMA or ICS/LABA | 6799 (17.4) | 7397 (18.9) |
| ICS/LAMA/LABA | 10,992 (28.1) | 16,797 (42.9) |
| SABA monotherapy | 12,859 (32.8) | 15,429 (39.4) |
| N-acetylcysteine | 10,984 (28.0) | 15,073 (38.5) |
| PD4 antagonists | 243 (0.6) | 359 (0.9) |
| Hospital-based outpatient visits | ||
| Any reason, n (%) | 19,097 (48.7) | 23,354 (59.6) |
| Rate (95% CI) per 100 PY | 136.1 (134.9–137.2) | 196.4 (194.9–197.8) |
| COPD-related, n (%) | 6585 (16.8) | 11,422 (29.2) |
| Rate (95% CI) per 100 PY | 25.2 (24.7–25.7) | 53.4 (52.6–54.1) |
Notes: Patients with ≥12 months of follow-up were included (n=39,181). COPD treatments were collected during a 4-month period pre-index and post-index for the baseline and follow-up period, respectively.
Abbreviations: CI, confidence interval; COPD, chronic obstructive pulmonary disease; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; N/A, not applicable; PD4, phosphodiesterase-4; PY, patient-years; SABA, short-acting β2-agonist.
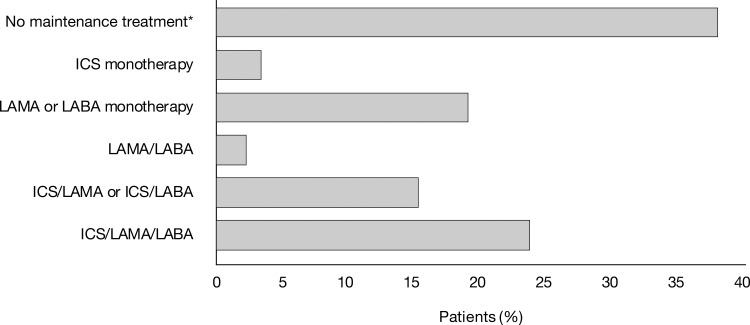
Of the full population, 18,167 (35.4%) patients who did not collect ICS or long-acting bronchodilator treatment during baseline, 37.9% continued without treatment during follow-up, 22.1% collected triple therapy, 21.3% LAMA and/or LABA and 15.3% ICS with LAMA or LABA (Figure 2; online supplementary Table 2). When considering patients collecting LABA and/or LAMA during baseline (n=7925), 40.4% continued with LAMA and/or LABA during follow-up, but less than half (42.5%) switched to an ICS-containing treatment regimen (online supplementary Table 2).
Figure 2.
ICS, LAMA and LABA treatment after hospitalisation for severe COPD exacerbation in patients without COPD treatment during baseline period. *Neither LAMA, LABA or ICS. COPD treatments were collected during a 4-month period pre-index and post-index. All patients (n=18,167) were included irrespective of follow-up time. COPD, chronic obstructive pulmonary disease; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist.
Among patients without maintenance treatment during the baseline period and without any hospitalisation during the first 4 months of follow-up (n=10,008), those that continued without treatment following hospitalisation (n=3239) were older and had more comorbidities (Table 3).
Table 3.
Basic Characteristics of Baseline Untreated Study Population by Post-Index COPD Treatment (n=10,008)
| Post-Index COPD Treatment | |||
|---|---|---|---|
| All (n=10,008) | COPD Treated (n=6769) | COPD Non-Treated (n=3239) | |
| Females, n (%) | 5518 (55.1) | 3828 (56.6) | 1690 (52.2) |
| Age, years | |||
| Mean (SD) | 72.9 (10.8) | 72.3 (10.5) | 74.3 (11.4) |
| Median (IQR) | 74.0 (65.0–81.0) | 73.0 (65.0–80.0) | 76.0 (66.0–83.0) |
| Range | 40–99 | 40–99 | 40–99 |
| Age categories, n (%) | |||
| 40–64 | 2262 (22.6) | 1582 (23.4) | 680 (21.0) |
| 65–79 | 4650 (46.5) | 3318 (49.0) | 1332 (41.1) |
| ≥80 | 3096 (30.9) | 1869 (27.6) | 1227 (37.9) |
| Charlson Comorbidity Index, n (%) | |||
| 0 | 3939 (39.4) | 2886 (42.6) | 1053 (32.5) |
| 1 | 2257 (22.6) | 1523 (22.5) | 734 (22.7) |
| 2 | 1604 (16.0) | 1032 (15.2) | 572 (17.7) |
| ≥3 | 2208 (22.1) | 1328 (19.6) | 880 (27.2) |
| Comorbidities, n (%) | |||
| Heart failure | 1079 (10.8) | 658 (9.7) | 421 (13.0) |
| Ischaemic heart disease | 1059 (10.6) | 684 (10.1) | 375 (11.6) |
| Diabetes | 889 (8.9) | 538 (7.9) | 351 (10.8) |
| Pneumonia | 827 (8.3) | 486 (7.2) | 341 (10.5) |
| Malignant neoplasm | 674 (6.7) | 428 (6.3) | 246 (7.6) |
| Anxiety and depression disorder | 312 (3.1) | 195 (2.9) | 117 (3.6) |
| Osteoporosis/fractures | 183 (1.8) | 103 (1.5) | 80 (2.5) |
| Hospital-based outpatient visits, rate (95% CI) per 100 PY | |||
| Any reason | 100.6 (98.7–102.6) | 89.2 (87.0–91.5) | 124.5 (120.6–128.3) |
| COPD-related | 7.7 (7.2–8.3) | 7.9 (7.3–8.6) | 7.3 (6.3–8.2) |
| Hospitalisations, rate (95% CI) per 100 PY | |||
| Any reason | 63.1 (61.5–64.6) | 55.5 (53.7–57.2) | 78.9(75.9–82.0) |
| Any exacerbation, n (%) | 2018 (20.2) | 1350 (19.9) | 668 (20.6) |
| Exacerbation rate (95% CI) per 100 PY | 53.2 (51.8–54.7) | 48.0 (46.3–49.6) | 64.2 (61.4–66.9) |
Abbreviations: CI, confidence interval; COPD, chronic obstructive pulmonary disease; IQR, inter-quartile range; PY, patient-years; SD, standard deviation.
Outpatient Visits
Among the 39,181 patients with ≥12 months of follow-up, there was an increase in the number of COPD-related outpatient visits during follow-up compared with baseline from 25.2 to 53.4 visits per 100 patient-years (PY) (Table 2); however, 70.8% did not have an outpatient hospital visit due to COPD within the first year post-discharge.
Re-Hospitalisations
Of the 39,181 patients followed for ≥12 months, re-hospitalisation due to a second severe exacerbation occurred in 23.9% of patients (Table 2). Among these patients, there was a higher incidence of ≥1 moderate exacerbation during baseline versus patients who were not re-hospitalised (49.4% versus 36.0%). Comorbidities, including ischaemic heart disease (12.0% versus 14.6%), heart failure (11.3% versus 14.4%) and pneumonia (9.7% versus 14.5%), were more common among patients who were re-hospitalised than those who were not. Anxiety and depression disorder, along with osteoporosis/fractures also occurred more frequently among re-hospitalised patients. Differences in sex and age were minimal (Table 4).
Table 4.
Baseline Patient Demographics and Characteristics Among Patients Re-Hospitalised Due to COPD During 1-Year Follow-Up (n=39,181)
| Number of Re-Hospitalisations During 1-Year Post-Index | ||||
|---|---|---|---|---|
| 0 (n=29,805) | 1 (n=5342) | 2 (n=2084) | ≥3 (n=1950) | |
| Females, n (%) | 16,802 (56.4%) | 3019 (56.5%) | 1174 (56.3%) | 1131 (58.0%) |
| Age, mean years (SD) | 73.1 (10.2) | 74.0 (9.7) | 74.0 (9.7) | 73.5 (9.5) |
| Any COPD exacerbation, n (%) | 10,734 (36.0%) | 2501 (46.8%) | 1031 (49.5%) | 1102 (56.5%) |
| Respiratory treatment during follow-up, n (%) | ||||
| Neither LAMA, LABA or ICS | 11,667 (39.1%) | 1443 (27.0%) | 511 (24.5%) | 349 (17.9%) |
| ICS monotherapy | 1283 (4.3%) | 176 (3.3%) | 69 (3.3%) | 74 (3.8%) |
| LAMA or LABA monotherapy | 3853 (12.9%) | 705 (13.2%) | 255 (12.2%) | 238 (12.2%) |
| LAMA/LABA | 572 (1.9%) | 114 (2.1%) | 49 (2.4%) | 32 (1.6%) |
| ICS/LAMA or ICS/LABA | 5093 (17.1%) | 951 (17.8%) | 382 (18.3%) | 373 (19.1%) |
| ICS/LAMA/LABA | 7337 (24.6%) | 1953 (36.6%) | 818 (39.3%) | 884 (45.3%) |
| Comorbidities, n (%) | ||||
| Ischaemic heart disease | 3582 (12.0) | 780 (14.6) | 317 (15.2) | 289 (14.8) |
| Heart failure | 3381 (11.3) | 768 (14.4) | 342 (16.4) | 280 (14.4) |
| Pneumonia | 2893 (9.7) | 775 (14.5) | 290 (13.9) | 341 (17.5) |
| Diabetes | 2685 (9.0) | 513 (9.6) | 211 (10.1) | 164 (8.4) |
| Malignant neoplasm | 2196 (7.4) | 449 (8.4) | 191 (9.2) | 138 (7.1) |
| Asthma | 1754 (5.9) | 397 (7.4) | 159 (7.6) | 177 (9.1) |
| Anxiety and depression disorder | 1002 (3.4%) | 208 (3.9%) | 106 (5.1%) | 112 (5.7%) |
| Osteoporosis/fractures | 720 (2.4%) | 176 (3.3%) | 93 (4.5%) | 96 (4.9%) |
Notes: Only patients under observation ≥12 months after index date were included (n=39,181). Re-hospitalisation was defined as an inpatient hospital visit with COPD as the primary diagnosis; only re-hospitalisations occurring ≥2 weeks after the index date were included.
Abbreviations: COPD, chronic obstructive pulmonary disease; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; LAMA, long-acting muscarinic antagonist; SD, standard deviation.
Re-hospitalisation due to a second severe exacerbation within 30 (n=48,461) and 90 (n=45,608) days was seen in 11.5% (n=5563) and 17.8% (n=8120) of the patients, respectively (Table 5). Female gender, higher age, comorbidities and previous exacerbations were independently associated with re-hospitalisation at both 30 days, 90 days and 12 months (Table 5).
Table 5.
Risk Factors for Re-Hospitalizations During Follow-Up
| 30 Days OR (95% CI)a | 90 Days OR (95% CI)a | 365 Days OR (95% CI)a | |
|---|---|---|---|
| Population, n | 48,461 | 45,608 | 39,181 |
| Re-hospitalised, n (%) | 5563 (11.5%) | 8120 (17.8%) | 9376 (23.9%) |
| Gender | |||
| Male | 1.00 | 1.00 | 1.00 |
| Females | 1.11 (1.05–1.17) | 1.11 (1.06–1.17) | 1.08 (1.03–1.13) |
| Age | |||
| 40–65 | 1.00 | 1.00 | 1.00 |
| 65–80 | 1.22 (1.13–1.33) | 1.29 (1.20–1.38) | 1.30 (1.22–1.38) |
| 80+ | 1.42 (1.30–1.55) | 1.43 (1.32–1.54) | 1.32 (1.23–1.41) |
| Charlson index | |||
| CCI 0 | 1.00 | 1.00 | 1.00 |
| CCI 1 | 1.36 (1.25–1.48) | 1.48 (1.38–1.59) | 1.59 (1.50–1.70) |
| CCI 2 | 1.23 (1.12–1.35) | 1.34 (1.24–1.45) | 1.48 (1.38–1.59) |
| CCI 3+ | 1.31 (1.21–1.43) | 1.45 (1.35–1.56) | 1.66 (1.56–1.78) |
| Exacerbations | |||
| 0 | 1.00 | 1.00 | 1.00 |
| 1 | 1.20 (1.11–1.29) | 1.28 (1.20–1.37) | 1.33 (1.26–1.41) |
| 2 | 1.21 (1.09–1.35) | 1.41 (1.29–1.54) | 1.53 (1.41–1.66) |
| 3+ | 1.25 (1.16–1.36) | 1.48 (1.39–1.59) | 1.71 (1.60–1.82) |
Note: aIf not otherwise specified.
Abbreviations: OR, odds ratio; CI, confidence interval.
Mortality
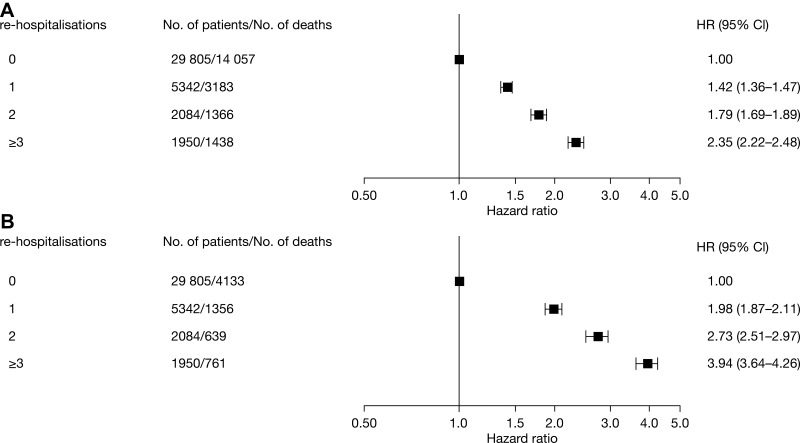
Overall, patients were followed on average for 3.2 years (range, 0 to 11 years). The 1-, 5- and 8-year mortality rate was 23.5%, 61.1%, and 75.9%, respectively. Corresponding mortality rates for the 39,181 patients alive and still under observation after 12 months of follow-up were 15.7% at 1 year and 56.7% at 5 years. The risk of both all-cause mortality and COPD-related mortality increased with each subsequent re-hospitalisation (Figure 3).
Figure 3.
Risk of (A) all-cause death and (B) COPD-related death by history of severe exacerbations during 1-year follow-up. Adjusted for gender, index age, Charlson comorbidity index and COPD treatment. CI, confidence interval; COPD, chronic obstructive pulmonary disease; HR, hazard ratio.
Discussion
In this nationwide observational study of patients in Sweden experiencing their first hospitalisation due to a severe COPD exacerbation, more than one-third of patients did not collect any inhaled ICS or long-acting bronchodilator treatment prior to hospitalisation. Moreover, despite an increase in the proportion of patients collecting maintenance LAMA, LABA or ICS treatment and an increase in the number of outpatient visits, more than one-third of these patients still did not collect the recommended maintenance treatment after 12 months of follow-up. This group of patients were older and had more comorbidities than the patients who started using treatment after their first hospitalisation. Each subsequent re-hospitalisation was associated with an increased risk of both all-cause and COPD-related mortality.
In the present study, we found that patients who continued without appropriate respiratory treatment after their first COPD-related hospitalisation were older and had more comorbidities than patients collecting medications following hospitalization. We can only speculate that this is related to fewer prescriptions from the physicians or non-collection of prescribed medications by the patients, as only data on the collection of drugs are available in our study. It cannot be ruled out that age and comorbidities may affect the behaviour identified.
Guidelines recommend a follow-up appointment takes place within 1 month after discharge following hospitalisation due to COPD2 but, in the present study, only 29% of patients received this care from a hospital-based specialist. Importantly, we found that almost one-quarter of patients had a readmission due to a severe COPD exacerbation within 1 year and almost one-quarter of patients died within 1 year. In common with previous studies,5,12–14 we found that, for patients hospitalised as a result of a severe COPD exacerbation, the risk of mortality increased with every new re-hospitalisation, for both all-cause death and COPD-related death. In addition, in a prospective study in France, 1824 patients hospitalised with a severe exacerbation, the mortality rate during the 4-year follow-up was similar to the rate found in our study (45%).15
In a European dataset of prospectively collected data for patients with severe COPD exacerbations resulting in hospitalisation (European COPD Audit), readmitted patients were found to have a higher mortality than non-readmitted patients and a logistic regression analysis identified patient-related variables such as age, comorbidities and previous admissions as factors that increased the risk of readmission.16 Furthermore, Wang et al described an association between hospitalisation due to a severe COPD exacerbation and an increased risk of cardiovascular events in patients from a Taiwanese healthcare insurance database, providing further confirmation of the urgent need to ensure appropriate treatment of severe COPD exacerbations.17
In the present study, 12% were re-hospitalised within 30 days, 18% within 90 days and 24% of patients were re-hospitalised within one year. Although this was lower than findings from the European COPD Audit, where approximately one-third of patients were re-hospitalised within 90 days,14,16,18 clearly there is room for further improvement. In the US, a policy was created with the aim of improving outcomes by imposing penalties in the event of higher than expected all-cause 30-day readmission rates following hospitalisation for COPD. However, evidence to support specific interventions was found to be inadequate, suggesting that re-hospitalisation may not be preventable in all patients.19,20 Indeed, patients recovering from any form of exacerbation require an array of specific interventions to promote self-management, address existing comorbidities, and coordinate ongoing community care.19
In line with other studies, comorbidities were common among patients who were hospitalised for severe COPD exacerbations.4,14,21–24 Patients with concurrent asthma had a higher risk of re-hospitalisation, a finding that is in accordance with many other studies showing that patients with concomitant asthma and COPD have a higher morbidity than those with COPD alone.25–27 Of note, anxiety and depression disorder was also associated with re-hospitalisation, further supporting the findings from previous studies.18,28,29 It has been suggested that physicians may underestimate the psychological impact of exacerbations on patients30 and only a small proportion of patients with anxiety or depression are offered effective treatment for their comorbidity, which is likely to have a negative impact on their COPD.23 Apart from comorbidities, the risk of re-hospitalisation was also increased for women and older patients compared with men and younger patients, respectively.
The main strengths of this study were the nationwide setting, with high-quality study registers covering all patients with COPD-related inpatient visits in Sweden during the study period. Furthermore, the large sample size with long follow-up strengthened the statistical power of the analysis. In terms of study weaknesses, a lack of information about primary care visits will have led to an underestimate of the observed healthcare utilisation, particularly as some of the patients not seen in hospital-based outpatient care will likely have been followed-up in primary care. In addition, clinical measurements, such as lung function, smoking and cough, are not captured in the registries used in this study. Treatments reported in this study are based on claims from pharmacy, medications provided during hospital admissions could not be captured due to limitations in the registry infrastructure. Finally, patients who died during follow-up may not have survived long enough to have a second COPD-related hospitalisation, which may have reduced the calculated re-hospitalisation rate.
In conclusion, we found that following a first hospitalisation due to severe COPD exacerbation, many patients did not collect the treatment recommended by current guidelines.2 Patients with concurrent ischaemic heart disease, heart failure and pneumonia had an increased risk of being re-hospitalised and risk of mortality increased with every subsequent re-hospitalisation. Hospital admission should provide an opportunity for clinicians to identify at-risk patients and provide them with closer follow-up and the best available preventive treatment to improve outcomes.
Acknowledgments
Editorial support, under the direction of the authors, was provided by Richard Knight, PhD, CMC Connect, McCann Health Medical Communications, and funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines.31
Funding Statement
This study was sponsored by AstraZeneca.
Data Sharing Statement
The dataset supporting the conclusions of this article can be available upon request.
Ethics Approval and Consent to Participate
This study was performed in accordance with the Declaration of Helsinki, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practices, Good Pharmacoepidemiology Practice and the applicable legislation on non-interventional studies and/or observational Studies. All data accessed complied with relevant data protection and privacy regulations. The study protocol was approved by the Stockholm Regional Ethics Committee (registration number 2017/4:2).
Consent for Publication
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
CJ has received payments for educational activities from AstraZeneca, Boehringer Ingelheim, Chiesi, Novartis, and Teva, and has served on advisory boards arranged by AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, and Teva. GT is an employee by AstraZeneca. FW is an employee at Statisticon for which AstraZeneca is a client. The authors report no other conflicts of interest in this work.
References
- 1.Calverley P. Issues at the interface between primary and secondary care in the management of common respiratory disease bullet 5: the challenge of providing better care for patients with chronic obstructive pulmonary disease: the poor relation of airways obstruction? Thorax. 2000;55(1):78–82. doi: 10.1136/thorax.55.1.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease. 2020 Report: global Strategy for the Diagnosis, Management and Prevention of COPD. 2020. https://goldcopd.org. Accessed 17March 2020.
- 3.Pavord ID, Jones PW, Burgel PR, et al. Exacerbations of COPD. Int J Chron Obstruct Pulmon Dis. 2016;11(Spec. Iss):21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gudmundsson G, Gislason T, Janson C, et al. Risk factors for rehospitalisation in COPD: role of health status, anxiety and depression. Eur Respir J. 2005;26:414–419. [DOI] [PubMed] [Google Scholar]
- 5.Gudmundsson G, Ulrik CS, Gislason T, et al. Long-term survival in patients hospitalised for chronic obstructive pulmonary disease: a prospective observational study in the Nordic countries. Int J Chron Obstruct Pulmon Dis. 2012;7:571–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnes PJ. How corticosteroids control inflammation: quintiles Prize Lecture 2005. Br J Pharmacol. 2006;148:245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swedish National Board of Health and Welfare. The Swedish National Patient Register. 2020. https://www.socialstyrelsen.se/en/statistics-and-data/registers/register-information/the-national-patient-register/. accessed 9March 2020.
- 8.Swedish National Board of Health and Welfare. The Swedish Prescribed Drug Register. 2020. https://www.socialstyrelsen.se/en/. accessed 9March 2020.
- 9.Brooke HL, Talbäck M, Hörnblad J, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32(9):765–773. doi: 10.1007/s10654-017-0316-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2019. https://icd.who.int/browse10/2019/en. accessed 12March 2020.
- 11.ICD10data.com. ICD-10-CM Diagnosis Code J44.0; 2020. https://www.icd10data.com/ICD10CM/Codes/J00-J99/J40-J47/J44-/J44.0. accessed 9February 2020.
- 12.Gudmundsson G, Gislason T, Lindberg E, et al. Mortality in COPD patients discharged from hospital: the role of treatment and co-morbidity. Respir Res. 2006;7(1):109. doi: 10.1186/1465-9921-7-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suissa S, Dell’Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957–963. doi: 10.1136/thoraxjnl-2011-201518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Njoku CM, Alqahtani JS, Wimmer BC. et al. Risk factors and associated outcomes of hospital readmission in COPD: A systematic review. Respir Med;2020. 105988. doi: 10.1016/j.rmed.2020.105988 [DOI] [PubMed] [Google Scholar]
- 15.Piquet J, Chavaillon J-M, David P, et al. High-risk patients following hospitalisation for an acute exacerbation of COPD. Eur Respir J. 2013;42(4):946–955. doi: 10.1183/09031936.00180312 [DOI] [PubMed] [Google Scholar]
- 16.Hartl S, Lopez-Campos JL, Pozo-Rodriguez F, et al. Risk of death and readmission of hospital-admitted COPD exacerbations: european COPD Audit. Eur Respir J. 2016;47(1):113–121. doi: 10.1183/13993003.01391-2014 [DOI] [PubMed] [Google Scholar]
- 17.Wang M, Lin EP, Huang L-C, et al. Mortality of cardiovascular events in patients with COPD and preceding hospitalisation for acute exacerbation. Chest. 2020;30443(20):S0012. doi: 10.1016/j.chest.2020.02.046 [DOI] [PubMed] [Google Scholar]
- 18.Alqahtani JS, Njoku CM, Bereznicki B, et al. Risk factors for all-cause hospital readmission following exacerbation of COPD: a systematic review and meta-analysis. Eur Respiratory Rev. 2020;29(156):190166. doi: 10.1183/16000617.0166-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krishnan JA, Gussin HA, Prieto-Centurion V, et al. Integrating COPD into Patient-Centered Hospital Readmissions Reduction Programs. Chronic Obstructive Pulmonary Dis. 2015;2(1):70–80. doi: 10.15326/jcopdf.2.1.2014.0148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prieto-Centurion V, Markos MA, Ramey NI, et al. Interventions to reduce rehospitalisations after chronic obstructive pulmonary disease exacerbations. A systematic review. Ann Am Thorac Soc. 2014;11:417–424. doi: 10.1513/AnnalsATS.201308-254OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gudmundsson G, Gislason T, Janson C, et al. Depression, anxiety and health status after hospitalisation for COPD: a multicentre study in the Nordic countries. Respir Med. 2006;100(1):87–93. doi: 10.1016/j.rmed.2005.04.003 [DOI] [PubMed] [Google Scholar]
- 22.Sin DD, Anthonisen NR, Soriano JB, et al. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–1257. doi: 10.1183/09031936.00133805 [DOI] [PubMed] [Google Scholar]
- 23.Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(4):43S–56S. doi: 10.1378/chest.08-0342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunter LC, Lee RJ, Butcher I, et al. Patient characteristics associated with risk of first hospital admission and readmission for acute exacerbation of chronic obstructive pulmonary disease (COPD) following primary care COPD diagnosis: a cohort study using linked electronic patient records. BMJ Open. 2016;6(1):e009121. doi: 10.1136/bmjopen-2015-009121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Marco R, Marcon A, Rossi A, et al. Asthma, COPD and overlap syndrome: a longitudinal study in young European adults. Eur Respir J. 2015;46(3):671–679. doi: 10.1183/09031936.00008615 [DOI] [PubMed] [Google Scholar]
- 26.Leung JM, Sin DD. Asthma-COPD overlap syndrome: pathogenesis, clinical features, and therapeutic targets. BMJ. 2017;358:j3772. doi: 10.1136/bmj.j3772 [DOI] [PubMed] [Google Scholar]
- 27.Mindus S, Malinovschi A, Ekerljung L, et al. Asthma and COPD overlap (ACO) is related to a high burden of sleep disturbance and respiratory symptoms: results from the RHINE and Swedish GA2LEN surveys. PLoS One. 2018;13(4):e0195055. doi: 10.1371/journal.pone.0195055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dahlén I, Janson C. Anxiety and depression are related to the outcome of emergency treatment in patients with obstructive pulmonary disease. Chest. 2002;122(5):1633–1637. doi: 10.1378/chest.122.5.1633 [DOI] [PubMed] [Google Scholar]
- 29.Montserrat-Capdevila J, Godoy P, Marsal JR, et al. Mental disorders in chronic obstructive pulmonary diseases. Perspect Psychiatr Care. 2018;54:398–404. doi: 10.1111/ppc.12274 [DOI] [PubMed] [Google Scholar]
- 30.Kessler R, Ståhl E, Vogelmeier C, et al. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based study. Chest. 2006;130(1):133–142. doi: 10.1378/chest.130.1.133 [DOI] [PubMed] [Google Scholar]
- 31.Battisti WP, Wager E, Baltzer L, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163(6):461–464. doi: 10.7326/M15-0288 [DOI] [PubMed] [Google Scholar]