Abstract
We aimed to explore what kind of endocrine treatments are optimal for hormone receptor-positive and human epidermal growth factor receptor 2-negative locally advanced or metastatic breast cancer in some specific clinical situations. We searched randomized controlled trials in Embase, Medline, the Cochrane library, and PubMed from inception to April 1, 2020 and performed a network meta-analysis based on a Bayesian fixed-effects model. Progression-free survival (PFS) with hazard ratios and corresponding 95% confidence interval was defined as the primary endpoint, while overall survival (OS), objective response rate (ORR), clinical benefit rate and serious adverse events were used as secondary endpoints. A total of 35 studies involving 12,285 patients and 24 treatment options were included. In general, most co-treatment options prolonged PFS compared to single-agent therapy, of which aromatase inhibitor (AI) plus everolimus and fulvestrant plus palbociclib were probably the most effective agents, and the latter had the best safety record. However, despite the superior efficacy of fulvestrant plus capecitabine for PFS and OS, palpable toxic effects have been demonstrated for this treatment, so its application must be scrupulously considered. The results of subgroup analysis indicated that fulvestrant combined with palbociclib improved prognosis for phosphatidylinositol 3-kinase (PI3K)-mutated patients, PI3K-unmutated patients, patients with endocrine therapy resistance, and visceral metastatic patients, while no obvious improvement was detected in OS. Moreover, the efficacy of fulvestrant plus cyclin-dependent kinase 4/6 (CDK4/6) inhibitors was slightly better than that of AI plus CDK4/6 inhibitors, while AI plus everolimus was more efficacious than fulvestrant combined with everolimus in terms of PFS, OS, and ORR. In conclusion, our results provide moderate evidence that fulvestrant plus palbociclib and AI plus everolimus were the most effective treatments, while the efficacy and safety of fulvestrant plus palbociclib was obviously superior in some specific clinical situations.
Keywords: Breast, Neoplasms, Prognosis, Safety
INTRODUCTION
Approximately 60%–70% of breast cancer patients present as hormone receptor-positive and human epidermal growth factor receptor 2 (HER2)-negative, with their treatment being based on endocrine therapy (ET) against the estrogen axis [1,2]. Although hormone receptor-positive/HER2-negative patients have a superior prognosis compared with triple-negative and HER2-overexpression breast cancer, the vast majority of patients will eventually progress to metastatic disease with or without ET resistance [3,4].
The activation of the phosphatidylinositol 3-kinase (PI3K)—protein kinase B (PKB/AKT)—mammalian target of rapamycin (mTOR) axis has emerged as a promotor of both tumor cell growth and ET resistance [5], and this pathway is considered to be a reasonable therapeutic target to inhibit tumor growth and revert ET resistance. Furthermore, another therapeutic target, serine/threonine protein kinase mTOR, plays an important role in many solid tumors, including breast cancer, and can regulate cell proliferation, differentiation and apoptosis [6]. In patients who had previously received ET, SOLAR-1 demonstrated that cotreatment with alpelisib, a PI3Kα-specific inhibitor, improved progression-free survival (PFS) among patients with PIK3CA mutations, which are detected in 40% of hormone receptor-positive/HER2-negative breast cancer [7] . The mTOR inhibitor everolimus also shows an anti-tumor effect and can reverse endocrine sensitivity in combination with ET for hormone receptor-positive/HER2-negative advanced breast cancer patients [8].
Dysregulation of the cyclin D–cyclin-dependent kinase (CDK)—retinoblastoma (Rb)—E2F pathway results in cell cycle progression through regulation of the G1-S checkpoint, and is detected in many cancers, especially in hormone receptor-positive breast carcinoma [9,10]. Components of the CDK4/6-Rb-E2F axis are abnormally mutated in 50%–70% of breast cancers, which contributes ET resistance [11]. Currently, in addition to traditional endocrine monotherapy including selective estrogen receptor modulators and aromatase inhibitors (AIs), many phase III randomized controlled trials (RCTs) such as MONALEESA-2 and MONARCH-3, have also demonstrated that cotreatment with cyclin-dependent kinase 4/6 (CDK4/6) inhibitors can significantly improve the prognosis in first-line treatments with manageable toxic effects [12,13]. Additionally, PALOMA-3 and MONARCH-2 showed that fulvestrant combined with CDK4/6 inhibitors was associated with longer PFS in ET-resistant patients [14,15]. Some articles indirectly compared the efficacy and toxicity among three different CDK4/6 inhibitors in the first-line treatment, and they appeared to have a similar benefit without significant difference [16].
In addition to inhibitors described above, there are still many targeted drugs and chemotherapy options that have the potential to improve the prognosis of hormone receptor-positive breast cancer. Notably, it remains unclear which kind of medicine works better under certain clinical conditions and which options are safer. Therefore, the purpose of our systematic review and network meta-analysis was to indirectly compare efficacy and safety between different ET strategies, given the lack of direct comparison for hormone receptor-positive/HER2-negative locally advanced or metastatic breast cancer in different situations.
METHODS
Search strategy
For this network meta-analysis, relevant phase 2 and 3 RCTs published before April 1, 2020 were searched systematically and logically without limitation of language in electronic databases in Embase, Medline, the Cochrane Library, and PubMed. The literature search strategy employed was as follows: breast AND (cancer OR neoplasm OR carcinoma) AND endocrine therapy AND HER2 negative. Meanwhile, related literature and conference abstracts were searched for references to ensure the comprehensiveness of results.
Selection criteria
Two researchers independently examined the literature, screening the title and abstract, and disagreements on eligible studies were resolved by discussion and negotiation or by consulting a third investigator. The inclusion criteria were as follows: 1) the patients had a pathological diagnosis of hormone receptor-positive/HER2-negative locally advanced or metastatic breast cancer; 2) a comparison was reported between different ETs; 3) the literature provided complete data on PFS, overall survival (OS), clinical benefit rate (CBR), objective response rate (ORR), or serious adverse events; 4) the study type was phase 2 or 3 non-single arm RCT. Only the reports with the longest follow-up period or the most comprehensive data were selected in order to omit overlapping populations. Simultaneously, we excluded trials in which the population was hormone receptor-negative or HER2-positive, or had early-stage breast cancer, and unsuitable study types were also deleted, such as reviews, letters, and retrospective studies.
Data extraction and quality assessment
Two researchers independently extracted and tabulated detailed data from eligible studies, including study name, intervention, sample size, patient clinical characteristics, and outcomes. In this network meta-analysis, the primary endpoint was PFS with corresponding hazard ratios (HRs), which was assessed based on the time from randomization to tumor progression or death based on RECIST (version 1.1). OS (time from randomization to death due to any cause), CBR (patients with complete response, partial response and stable disease ≥ 6 months), ORR (patients with complete response and partial response), and serious adverse events were defined as secondary endpoints. The risk of bias in the included literature was also assessed by two researchers independently utilizing the Cochrane collaboration's tool, which consisted of seven elements: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias [17].
Statistical analysis
In this network-meta analysis, HR with corresponding 95% confidence interval (CI) was applied to assess PFS and OS, while relative risk and corresponding 95% CI were used to assess dichotomous data. The entire process was divided into 2 parts: direct comparison and indirect comparison. For direct comparison, the I-squared test was performed to judge heterogeneity originating from data combination. A fixed-effects model was used when I-squared < 50%, indicating slight heterogeneity, otherwise a random-effects model was used. Indirect comparison was performed utilizing a Bayesian fixed-effects model to pool extracted data and evaluate various treatment options. The surface under cumulative ranking curve (SUCRA) was derived to evaluate the ranking possibility of each treatment strategy, and the closer the value of SUCRA was to 1, the better the efficacy and safety of intervention [18]. Moreover, we grouped patients into multiple subtypes based on PIK3CA-mutation status, ET resistance, and metastatic setting to assess the superior treatment in different situations. For all statistical results, p-values of 0.05 or lower were considered to indicate statistical significance. Statistical analysis was conducted using STATA 15.0 (StataCorp LLC, College Station, TX, USA), WinBUGS 14.0 (Imperial College School of Medicine, London, UK), GeMTC 0.14.3 (University of Groningen, Groningen, Netherlands).
Ethics statement
This article does not contain any studies with human participants or animals performed by any of the authors.
RESULTS
Search results
Without restriction of language, a total of 1,014 studies were discovered through the search strategy, including 122 studies in PubMed, 74 in Medline, 576 in the Cochrane Library, 206 in Embase and 37 additional records. After screening the titles and abstracts, 124 remaining records were considered to be eligible for a full text review. Ultimately, 35 articles were selected which met all the inclusion criteria, giving a total of 12,285 patients involved in this network meta-analysis, as shown in [7,8,12,13,14,15,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47]. The search process based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) technique is shown in in Figure 1 [48].
Figure 1. Flow diagram summarizing the selection process.
HER = human epidermal growth factor receptor; ET = endocrine therapy.
Characteristics and quality of study
The clinical characteristics of enrolled studies were similar in that all participations had histologically confirmed hormone receptor-positive/HER2-negative locally advanced or metastatic breast cancer based on the results of biopsy (primary tumor or metastatic disease) and about 85% of patients were post-menopausal. The median age of included patients ranged from 43 to 67 years. The interventions reported consisted of three CDK4/6 inhibitors in 10 reports, PI3K inhibitors in 5, mTOR inhibitor in 4, and anti-vascular endothelial growth factor (VEGF) drug in 2, and the control groups were generally treated with monotherapy, such as AI or fulvestrant. The dosage of fulvestrant in most studies was 500 mg per cycle (28 days), while the dosage in SoFEA and SWOG0226 was half as much. A total of 24 treatment options were involved in this network meta-analysis. In terms of outcomes, all studies, except for that of Howell et al. [19] and KCSG BR10-04, which only provided data on CBR or ORR, provided PFS data in detail. BOLERO-6 was a three-arm study, and all the others are two-arm studies, and all the studies which qualified for inclusion were phase 2 or 3 RCTs. More detailed features are listed in Table 1. A network plot displaying direct comparisons between different treatments is shown in Figure 2.
Table 1. Characteristics of the outcomes of the studies included in this network meta-analysis.
| Study | Treatment | No. of patients | Characteristic | PFS (HR and 95% CI) | OS (HR and 95% CI) | ORR | CBR |
|---|---|---|---|---|---|---|---|
| PALOMA-1 [36] | AI+PALBO | 84 | First-line therapy for postmenopausal women with advanced HR-positive/HER2-negative breast cancer | 0.49 (0.32–0.75) | 0.81 (0.49–1.35) | 36/84 | 68/84 |
| AI | 81 | 27/81 | 47/81 | ||||
| PALOMA-2 [37] | AI+PALBO | 444 | First-line therapy for postmenopausal women with advanced HR-positive/HER2-negative breast cancer | 0.58 (0.46–0.72) | NA | 187/444 | 377/444 |
| AI | 222 | 77/222 | 156/222 | ||||
| PALOMA-3 [14,42,46] | FUL+PALBO | 347 | ET resistant women with HR-positive/HER2-negative advanced or metastatic breast cancer | 0.46 (0.36–0.59) | 0.81 (0.64–1.03) | 66/347 | 231/347 |
| FUL | 174 | 15/174 | 69/174 | ||||
| MONALEESA-2 [13,43] | AI+RIBO | 334 | First-line therapy postmenopausal women with HR-positive/HER2-negative metastatic breast cancer | 0.56 (0.43–0.72) | 0.75 (0.52–1.08) | 135/334 | 205/334 |
| AI | 334 | 97/334 | 176/334 | ||||
| MONALEESA-3 [24] | FUL+RIBO | 484 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.59 (0.48–0.73) | 0.72 (0.57–0.92) | 157/484 | 340/484 |
| FUL | 242 | 52/242 | 152/242 | ||||
| MONALEESA-7 [41,44] | AI+RIBO | 248 | Premenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.57 (0.44–0.74) | 0.70 (0.50–0.98) | NA | NA |
| AI | 247 | ||||||
| MONARCH-2 [15,45] | FUL+ABEMA | 446 | ET resistant women with HR-positive/HER2-negative advanced breast cancer | 0.55 (0.45–0.68) | 0.76 (0.61–0.95) | 157/446 | 322/446 |
| FUL | 223 | 36/223 | 125/223 | ||||
| MONARCH-3 [12] | AI+ABEMA | 328 | First-line therapy postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.54 (0.41–0.72) | NA | 158/328 | 256/328 |
| AI | 165 | 57/165 | 118/165 | ||||
| MONARCH-plus [27] | AI+ABEMA | 207 | ET sensitive postmenopausal women with HR-positive/HER2-negative | 0.50 (0.35–0.72) | NA | 116/176 | 145/176 |
| AI | 99 | 30/83 | 51/83 | ||||
| FUL+ABEMA | 104 | ET resistant postmenopausal women with HR-positive/HER2-negative | 0.38 (0.24–0.59) | NA | 40/80 | 62/80 | |
| FUL | 53 | 4/38 | 16/38 | ||||
| SOLAR-1a [7] | FUL+ALP | 169 | First-line therapy men or postmenopausal women with HR-positive/HER2-negative advanced breast cancer with PI3K mutation | 0.65 (0.50–0.85) | NA | 45/169 | 104/169 |
| FUL | 172 | 22/172 | 78/172 | ||||
| SOLAR-1b [7] | FUL+ALP | 115 | First-line therapy men or postmenopausal women with HR-positive/HER2-negative advanced breast cancer without PI3K mutation | 0.85 (0.58–1.25) | NA | NA | NA |
| FUL | 116 | ||||||
| BELLE-2 [21] | FUL+BUP | 576 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.78 (0.67–0.89) | 0.87 (0.74–1.02) | 68/576 | 252/576 |
| FUL | 571 | 44/571 | 240/571 | ||||
| BELLE-3 [23] | FUL+BUP | 289 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.67 (0.53–0.84) | NA | 22/289 | 71/289 |
| FUL | 143 | 3/143 | 22/143 | ||||
| SANDPIPER a [20] | FUL+TAS | 340 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer with PI3K mutation | 0.70 (0.56–0.89) | NA | 74/264 | 136/264 |
| FUL | 176 | 16/134 | 50/134 | ||||
| SANDPIPER b [20] | FUL+TAS | 77 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer without PI3K mutation | 0.69 (0.44–1.08) | NA | NA | NA |
| FUL | 38 | ||||||
| ACE [28] | AI+TUC | 244 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.75 (0.58–0.98) | NA | 45/244 | 114/244 |
| AI | 121 | 11/121 | 43/121 | ||||
| BOLERO-2 [22,47] | AI+EVE | 485 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.38 (0.31–0.48) | 0.89 (0.73–1.10) | 61/485 | 242/485 |
| AI | 239 | 5/239 | 53/239 | ||||
| BOLERO-6 [8] | AI+ EVE | 104 | ET resistant postmenopausal women with HR-positive/HER2-negative advanced breast cancer | AI+EVE vs EVE: 0.73 (0.56–0.97); AI+EVE vs CAP: 1.15 (0.86–1.52) | NA | NA | NA |
| EVE | 103 | ||||||
| CAP | 102 | ||||||
| FALCON [26] | Ful | 230 | ET-naïve postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.80 (0.64–1.00) | 0.88 (0.63–1.22) | 93/230 | 180/230 |
| AI | 232 | 90/232 | 172/232 | ||||
| SoFEA [39] | FUL+AI | 122 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.95 (0.75–1.22) | 0.95 (0.76–1.17) | NA | NA |
| FUL | 141 | ||||||
| Paul et al. [35] | AI+DAS | 57 | Postmenopausal women with HR-positive/HER2-negative breast cancer with 0–1 prior chemotherapy and no prior AI for advanced disease | 0.69 (0.43–1.09) | NA | NA | 35/55 |
| AI | 63 | 37/61 | |||||
| SWOG0226 [38] | FUL+AI | 266 | Postmenopausal women with HR-positive/HER2-negative untreated advanced breast cancer | 0.81 (0.67–0.98) | 0.81 (0.65–1.00) | NA | NA |
| AI | 270 | ||||||
| PrE0102 [33] | FUL+EVE | 66 | ET resistant postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.61 (0.40–0.92) | 1.31 (0.72–2.38) | 12/66 | 42/66 |
| FUL | 65 | 8/65 | 27/65 | ||||
| KCSG-BR10-04 [30] | FUL | 44 | Premenopausal women with HR-positive/HER2-negative tamoxifen-pretreated advanced breast cancer | NA | 0.85 (0.27–2.74) | 16/30 | NA |
| AI | 47 | 10/24 | |||||
| KCSG-BR15-10 [34] | AI+PALBO | 92 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.64 (0.42–1.00) | NA | NA | NA |
| CAP | 92 | ||||||
| FERGI [25] | FUL+PIC | 88 | ET resistant postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.74 (0.52–1.06) | NA | NA | NA |
| FUL | 79 | ||||||
| FAKTION [29] | FUL+CAP | 69 | ET resistant postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.58 (0.39–0.84) | 0.59 (0.34–1.05) | NA | NA |
| FUL | 71 | ||||||
| AROBASE [40] | AI+BEV | 58 | Postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 1.00 (0.66–1.51) | NA | NA | NA |
| PTX+BEV | 59 | ||||||
| Musolino et al. [32] | FUL+DOV | 47 | ET resistant postmenopausal women with HR-positive/HER2-negative advanced breast cancer | 0.68 (0.41–1.41) | 0.81 (0.39–1.65) | 13/47 | 31/47 |
| FUL | 50 | 5/50 | 21/50 | ||||
| Howell et al. [19] | FUL | 313 | Postmenopausal women with HR-positive/HER2-negative untreated advanced breast cancer | NA | NA | 99/313 | 170/313 |
| TAM | 274 | 93/274 | 170/274 | ||||
| Dickler et al. [31] | AI+BEV | 173 | Women with HR-positive/HER2-negative advanced breast cancer | 0.75 (0.59–0.96) | 0.87 (0.65–1.18) | NA | NA |
| AI | 170 |
PFS = progression-free survival; HR = hazard ratio; CI = confidence interval; OS = overall survival; ORR = objective response rate; CBR = clinical benefit rate; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+AI = fulvestrant plus aromatase inhibitor; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+CAP = fulvestrant plus capecitabine; FUL+DOV = fulvestrant plus dovitinib; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+PIC = fulvestrant plus pictilisib; FUL+RIBO = fulvestrant plus ribociclib; FUL+TAS = fulvestrant plus taselisib; PTX+BEV = paclitaxel plus bevacizumab; TAM = tamoxifen; AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+BEV = aromatase inhibitor plus bevacizumab; AI+DAS = aromatase inhibitor plus dasatinib; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; CAP = capecitabine; EVE = everolimus; NA = not applicable; ET = endocrine therapy.
Figure 2. Network meta-analysis plot of direct comparison. Each circle in the plot represents a treatment option, and the size indicates the number of patients. Solid lines represent direct comparisons between different treatment options, and the thickness indicates the number of studies involved.
FUL = fulvstrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+AI = fulvestrant plus aromatase inhibitor; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+CAP = fulvestrant plus capecitabine; FUL+DOV = fulvestrant plus dovitinib; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+PIC = fulvestrant plus pictilisib; FUL+RIBO = fulvestrant plus ribociclib; FUL+TAS = fulvestrant plus taselisib; PTX+BEV = paclitaxel plus bevacizumab; TAM = tamoxifen; AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+BEV = aromatase inhibitor plus bevacizumab; AI+DAS = aromatase inhibitor plus dasatinib; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; CAP = capecitabine; EVE = everolimus.
Two researchers also independently assessed the risk of bias in the final studies included using the Cochrane Collaboration's tool. The judging criteria were divided into 3 levels (low risk, high risk, and unclear), and no apparently low-quality studies were included. The detailed quality evaluation results are shown in Supplementary Table 1.
Outcomes
Progression-free survival
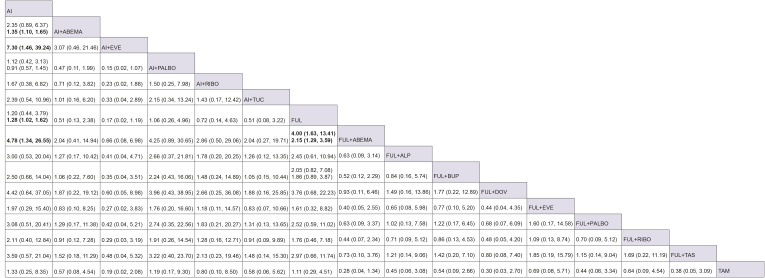
In this network meta-analysis, a total of 27 studies provided detailed data on PFS. Firstly, direct comparisons were calculated using a fixed-effects model to observe the efficacy of multiple treatments including AI or fulvestrant plus three CDK4/6 inhibitors and buparlisib, and the results showed that ET combined with targeted drugs was superior to monotherapy for inoperable patients. Next, an indirect comparison produced a similar conclusion, finding that AI or fulvestrant plus CDK4/6 inhibitors, PI3K inhibitors, everolimus, and capecitabine significantly improved the prognosis regardless of the type of CDK4/6 inhibitors, as shown in Figure 3. However, compared with AI plus CDK4/6 inhibitors, the effect of fulvestrant combined with CDK4/6 inhibitors was superior; and, for everolimus, a combination with AI showed better efficiency than a combination with fulvestrant. Moreover, tucidinostat presented a disappointing result in that no significant difference was found between AI plus tucidinostat and monotherapy. Finally, the SUCRA curve revealed that AI plus everolimus and fulvestrant plus palbociclib were ranked first with similar probabilities (93.5% and 94.3%, respectively) followed by fulvestrant plus abemaciclib or ribociclib. Everolimus alone ranked last, having the worst effect compared to AI, fulvestrant, or capecitabine alone. The results of direct comparison and cumulative probability ranking are shown in Supplementary Figure 1A and Figure 4A, respectively.
Figure 3. Indirect comparison of 23 different treatment options in terms of progression-free survival.
The ladder table displays the indirect comparison of 2 different treatment options. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference. For those with 2 sets of data, the first one compares the results indirectly and the second compares them directly.
HR = hazard ratio; CI = confidence interval; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+AI = fulvestrant plus aromatase inhibitor; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+CAP = fulvestrant plus capecitabine; FUL+DOV = fulvestrant plus dovitinib; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+PIC = fulvestrant plus pictilisib; FUL+RIBO = fulvestrant plus ribociclib; FUL+TAS = fulvestrant plus taselisib; PTX+BEV = paclitaxel plus bevacizumab; AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+BEV = aromatase inhibitor plus bevacizumab; AI+DAS = aromatase inhibitor plus dasatinib; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; CAP = capecitabine; EVE = everolimus.
Figure 4. Surface under cumulative ranking curves of different endocrine treatment options. The horizontal axis represents the ranking, and the vertical axis represents the cumulative possibility. The larger the area under the curve, the more effective the treatment. (A) Curve of 23 treatment options for progression-free survival; (B) curve of 14 options for overall survival; (C) curve of 16 treatment options for objective response rate; (D) curve of 17 treatment options for clinical benefit rate; (E) curve of 14 treatment options for serious adverse events.
AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+BEV = aromatase inhibitor plus bevacizumab; AI+DAS = aromatase inhibitor plus dasatinib; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; CAP = capecitabine; EVE = everolimus; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+AI = fulvestrant plus aromatase inhibitor; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+CAP = fulvestrant plus capecitabine; FUL+DOV = fulvestrant plus dovitinib; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+PIC = fulvestrant plus pictilisib; FUL+RIBO = fulvestrant plus ribociclib; FUL+TAS = fulvestrant plus taselisib; PTX+BEV = paclitaxel plus bevacizumab; TAM = tamoxifen.
Next, the patients were divided into two subgroups, a PIK3CA-mutated and a PIK3CA-unmutated group. The results indicated that fulvestrant combined with palbociclib or PI3K inhibitors including alpelisib, buparlisib, and taselisib had excellent efficacy compared to monotherapy in advanced breast cancer with PIK3CA mutation. However, for patients without PIK3CA mutation, only fulvestrant plus palbociclib or buparlisib prolonged the PFS compared to fulvestrant alone. Detailed results are shown in Supplementary Figures 2 and 3. Fulvestrant combined with palbociclib ranked first while fulvestrant alone ranked last, regardless of the status of PIK3CA mutation, as shown in Supplementary Figure 4A and B.
Similarly, and independent subgroup analysis was performed on ET-resistant participants according to response to prior therapy. Compared to fulvestrant monotherapy, fulvestrant plus CDK4/6 inhibitors or PIK3CA inhibitors achieved excellent outcomes for all except pictilisib, as shown in Supplementary Figure 5. Similar to the above results, fulvestrant combined with palbociclib still ranked first, followed by fulvestrant plus abemaciclib and fulvestrant plus capecitabine, as shown in Supplementary Figure 4C.
Based on the location of the metastatic setting, we extracted PFS data from patients with visceral metastases and presented a subgroup analysis. Compared with endocrine monotherapy, AI or fulvestrant combined with targeted drugs was found to be capable of significantly prolonging PFS in visceral metastasis patients except in the cases of tucidinostat and pictilisib (Supplementary Figure 6). In terms of rankings, the results suggested that fulvestrant plus palbociclib or abemaciclib ranked first (86.2% and 84.7%, respectively) followed by fulvestrant plus buparlisib, and monotherapies including AI and fulvestrant ranked last (Supplementary Figure 4D).
Overall survival
In addition, a total of 16 clinical studies contributed data on OS involving 14 different treatment options. A fixed-effects model was applied for direct comparison due to the low heterogeneity, and only AI plus ribociclib was linked to an effect of prolonging survival time (Supplementary Figure 1B). Similarly, an indirect comparison was performed, and this suggested that fulvestrant plus ribociclib, abemaciclib, or capecitabine, and AI plus ribociclib can improve OS compared to AI alone, and only the results of fulvestrant combined with ribociclib or abemaciclib were statistically different compared to fulvestrant alone (Figure 5). Unexpectedly, fulvestrant plus capecitabine showed the highest probability to rank first, followed by fulvestrant combined with ribociclib or abemaciclib (Figure 4B).
Figure 5. Indirect comparison of 14 different treatment options in terms of overall survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
HR = hazard ratio; CI = confidence interval; AI = aromatase inhibitor; AI+BEV = aromatase inhibitor plus bevacizumab; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+AI = fulvestrant plus aromatase inhibitor; FUL+BUP = fulvestrant plus buparlisib; FUL+DOV = fulvestrant plus dovitinib; FUL+CAP = fulvestrant plus capecitabine; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+RIBO = fulvestrant plus ribociclib.
Objective response rate
Nineteen studies provide detailed data on ORR, involving 16 different treatment options. Direct comparison was performed using a random-effects model due to the obvious heterogeneity of the data, and the results suggested the effectiveness of CDK4/6 inhibitors, including palbociclib and abemaciclib, for advanced breast cancer in ORR (Supplementary Figure 1C). Next, we continuously calculated the results of indirect comparison and cumulative probability of ranking in different treatment strategies. In the indirect comparison, AI combined with everolimus and fulvestrant combined with abemaciclib resulted in higher ORR to some extent (Figure 6). Figure 4C presents the ranking results, showing that AI plus everolimus had the highest probability to rank first followed by fulvestrant combined with abemaciclib.
Figure 6. Indirect comparison of 16 different treatment options in terms of objective response rate. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
HR = hazard ratio; CI = confidence interval; AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+DOV = fulvestrant plus dovitinib; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+RIBO = fulvestrant plus ribociclib; FUL+TAS = fulvestrant plus taselisib; TAM = tamoxifen.
Clinical benefit rate
In this network meta-analysis, a total of 19 clinical trials involving 17 different treatments provided detailed data on CBR. The direct comparison results from a random-effects model showed that fulvestrant plus abemaciclib can significantly improve the CBR in advanced breast cancer. The indirect comparison found no significant differences, and fulvestrant plus palbociclib, fulvestrant plus abemaciclib had the highest probability to rank first (71.6% and 73.0%, respectively), followed by AI plus everolimus, as shown in Figures 4D and 7.
Figure 7. Indirect comparison of 17 different treatment options in terms of clinical benefit rate. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
HR = hazard ratio; CI = confidence interval; AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+DAS = aromatase inhibitor plus dasatinib; AI+EVE = aromatase inhibitor plus everolimus; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+DOV = fulvestrant plus dovitinib; FUL+EVE = fulvestrant plus everolimus; FUL+PALBO = fulvestrant plus palbociclib; FUL+RIBO = fulvestrant plus ribociclib; FUL+TAS = fulvestrant plus taselisib; TAM = tamoxifen.
Safety
Data on serious adverse events were extracted from articles to evaluate the safety of different treatment options. The results of indirect comparison clearly showed that only fulvestrant combined with capecitabine was significantly different compared with fulvestrant alone, in that the former had a higher incidence of serious adverse events (Figure 8). Moreover, fulvestrant plus palbociclib showed the best safety and curative efficacy according to the SUCRA curve (Figure 4E).
Figure 8. Indirect comparison of 14 different treatment options in terms of serious adverse events. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
HR = hazard ratio; CI = confidence interval; AI = aromatase inhibitor; AI+ABEMA = aromatase inhibitor plus abemaciclib; AI+PALBO = aromatase inhibitor plus palbociclib; AI+RIBO = aromatase inhibitor plus ribociclib; AI+TUC = aromatase inhibitor plus tucidinostat; FUL = fulvestrant; FUL+ABEMA = fulvestrant plus abemaciclib; FUL+AI = fulvestrant plus aromatase inhibitor; FUL+ALP = fulvestrant plus alpelisib; FUL+BUP = fulvestrant plus buparlisib; FUL+CAP = fulvestrant plus capecitabine; FUL+PALBO = fulvestrant plus palbociclib; FUL+PIC = fulvestrant plus pictilisib; FUL+RIBO = fulvestrant plus ribociclib.
DISCUSSION
Hormone receptor-positive/HER2-negative is the most common subtype of breast cancer, and ET is the preferred treatment, as it has proven efficacy and tolerable toxicity (except in life-threatening situations) [49]. Recently, many targeted drugs, such as CDK4/6 inhibitors, mTOR inhibitors, PIK3CA inhibitors, etc., have proved to be effective in vivo or in vitro experiments, particularly against advanced hormone receptor-positive/HER2-negative breast cancer. Although targeted drugs with different mechanisms have exhibited superior curative effects leading to improved prognosis, no study has previously carried out a direct comparison of the efficacy and safety of different treatment options. Therefore, we performed a network meta-analysis to indirectly compare 24 different treatment strategies to determine which options are most appropriate under specific circumstances.
Currently, the crucial role of the PI3K/AKT/mTOR pathway in stimulating tumor cell proliferation, changing metabolism, and inhibiting apoptosis is widely accepted in breast cancer [50]. Some potential interactions between estrogen receptors and the PI3K/AKT/mTOR pathway have been documented [51]. Long-term poverty of estrogen is closely related to increased phosphorylation of AKT and activity of mTOR, which is the mechanism by which tumor cells adapt to low estrogen levels and develop resistance to antiestrogen therapeutics [52]. Everolimus, an oral rapamycin derivative, can suppress PI3K/AKT/mTOR cascades to inhibit downstream signaling events, and exhibits anti-tumor activity when combined with AI in advanced breast cancer, particularly in the presence of endocrine resistance [53]. According to our results, although fulvestrant combined with everolimus also exhibited the capacity to prolong the PFS and improve clinical efficacy, AI plus everolimus showed the highest probability of ranking first terms of its effect on PFS and ORR, while no notable effect was found in terms of OS. Moreover, the results showed that everolimus should certainly not be used alone due to poor efficacy compared with AI or fulvestrant alone. PI3k inhibitors (alpelisib, buparlisib, taselisib, and pictilisib) similarly repressed the PI3K/AKT/mTOR pathway, but tumor regression depended on the presence of PIK3CA mutation, unlike in the case of everolimus [54]. In our results, although PI3K inhibitors (except pictilisib) combined with fulvestrant improved the prognosis compared with endocrine monotherapy, the efficacy was still inferior to that of CDK4/6 inhibitors combined with AI or fulvestrant, regardless of PIK3CA-mutation status.
Another crucial pathway, CDK-Rb-E2F, accelerates G1-S transformation through association with increased CDK4/6 activity [55], and p16INK4A, a suppressor for CDK4/6, is a particularly important protein for inducing cell arrest at G1. Gene mutation of p16INK4A or gene amplification of CDK4/6 both activate the CDK-Rb-E2F pathway, leading to excessively cellular proliferation [7], and could provide a potential therapeutic target for the inhibition of CDK4/6 activity. The highly selective inhibitors of CDK4/6 kinases (palbociclib, ribociclib, and abemaciclib) block Rb phosphorylation, reducing cytostasis in G1 in luminal breast cancer [56,57,58]. In this network meta-analysis, although no significant differences were observed in the three CDK4/6 inhibitors combined with AI or fulvestrant, the effects of fulvestrant combined with CDK4/6 inhibitors was slightly better than those of AI plus CDK4/6 inhibitors. The evaluation of OS showed that the efficacy of co-treatment with ribociclib or abemaciclib was superior to that of palbociclib, although no significant difference was found in indirect comparisons. Finally, our safety results indicated that palbociclib, whether combined with AI or fulvestrant, had a more better safety record compared to the other 2 CDK4/6 inhibitors. In addition, our results indicated that the efficacy of palbociclib alone in advanced breast cancer was disappointing. It is worth noting that abemaciclib has been approved to treat breast cancer alone, unlike palbociclib and ribociclib [59].
The results of indirect analysis also included AI plus tyrosine kinase inhibitor, AI plus histone deacetylase (HDAC) inhibitor, AI plus VEGF inhibitor, capecitabine, fulvestrant plus capecitabine, and fulvestrant plus AI. Capecitabine is commonly used as an oral chemotherapy drug for breast cancer patients who have progressed during anti-estrogen therapy, and fulvestrant combined with capecitabine had the most significant effect on prolonging OS, with slightly improved PFS based on our results. The oral HDAC inhibitor (tucidinostat) and dovitinib can promote differentiation and cell cycle arrest, and regulate the tumor microenvironment by inhibiting HDAC1, HDAC2, HDAC3, and HDAC10, and by blocking fibroblast growth factor receptor and the respective downstream signaling pathways of all these proteins [60,61,62]. Our results demonstrated that AI plus bevacizumab, tucidinostat, or fulvestrant, and fulvestrant combined with dovitinib improved clinical outcomes compared with AI alone, but no significant differences were detected compared with fulvestrant alone. Because the dosage of fulvestrant was half of the standard usage in those studies which provided detailed data of fulvestrant combined with AI, the efficacy of fulvestrant plus AI may be more remarkable. In conclusion, the above treatment agents are not recommended for first-line treatment. When the patient responds poorly to multiple treatment strategies, including CDK4/6 inhibitors and everolimus, fulvestrant in combination with capecitabine or dovitinib or AI, or AI in combination with bevacizumab or tucidinostat can be used to achieve a longer survival time.
Based on PIK3CA mutations, ET resistance and visceral metastasis, participants were divided into several subgroups to evaluate which ET regimen was more effective in different situations. In patients with PIK3CA mutations, fulvestrant in combination with palbociclib, alpelisib, buparlisib, or taselisib exhibited excellent curative effect on PFS compared to monotherapy, but pictilisib did not. Fulvestrant plus palbociclib was the most likely to rank first, indicating that CDK4/6 inhibitors still had superior efficacy for patients with PIK3CA mutations. Therefore, PI3K inhibitors can be used to treat patients with hormone receptor-positive/HER2-negative advanced breast cancer who are resistant to CDK4/6 inhibitors. For patients without PIK3CA mutations, only palbociclib and buparlisib exhibited an effect of improving the prognosis compared with fulvestrant alone.
Intrinsic or acquired endocrine resistance remains a tough challenge for breast cancer treatment [63]. Many preclinical models have been used to attempt to elucidate the mechanisms of endocrine resistance. At present, researchers have established that disorder of the PI3K/AKT/mTOR axis and CDK/Rb/E2F pathway is the critical mechanism leading to endocrine resistance [64] In this meta-analysis, fulvestrant combined with palbociclib, abemaciclib, alpelisib, buparlisib, everolimus, or capecitabine showed efficacy in prolonging PFS for patients with ET resistance compared with fulvestrant alone. Although there was no significant difference between the 2 PI3K inhibitors, the efficacy of alpelisib was slightly better than that of buparlisib. Similarly, fulvestrant combined with CDK4/6 inhibitors is the preferred option for ET-resistant patients. Moreover, the results from the visceral metastasis subgroup suggested that fulvestrant combined with CDK4/6 inhibitors or PI3K inhibitors (alpelisib, buparlisib), and AI combined with CDK4/6 inhibitors or tucidinostat can improve the prognosis to different degrees compared with endocrine monotherapy. Although significant differences were not found among the three CDK4/6 inhibitors, the efficacy of palbociclib and abemaciclib was slightly better than that of ribociclib for advanced breast cancer patients with visceral metastasis. Similarly, the curative effect of buparlisib was slightly better to that of alpelisib, although there was no statistical difference.
Our study included a large number of treatment options for hormone receptor-positive/HER2-negative advanced breast cancer, and involved subgroup analysis based on the status of PIK3CA mutation, ET resistance, and visceral metastasis, which no previous study has done [16]. However, there are still many limitations in this network meta-analysis. Firstly, according to the BOLERO-2 study, AI combined with everolimus was extremely effective in patients with visceral metastasis or resistance to ET [22], but everolimus could not be indirectly compared in the ET resistance subgroup and visceral metastasis subgroup due to the lack of complete data. Secondly, we did not distinguish between different dosages of drugs. For example, the standard dosage of fulvestrant was defined as 500 mg fulvestrant on days 1 and 15 of cycle one and then on day one of each subsequent cycle (28 days) [65]. However, the dosage of fulvestrant used in SoFEA and SWOG0226 was 500 mg via intramuscular injection on day 1 followed by 250 mg injections on days 15 and 29, and then 250 mg intramuscular injections were done every 28 days [38,39]. Therefore, the use of non-standard fulvestrant dosages may have influenced the results of indirect comparison. Thirdly, different treatment options were not calculated for premenopausal and perimenopausal patients due to the lack of detailed data. About 85% of the participants in this meta-analysis were post-menopausal, and there may be some differences in the treatment plan for patients with different menstrual conditions.
CONCLUSION
In conclusion, our meta-analysis demonstrated that fulvestrant or AI combined with targeted drugs or other anti-tumor drugs can generally improve the prognosis for hormone receptor-positive/HER2-negative advanced breast cancer with controllable adverse events. Among the options analyzed, the effect of AI combined with everolimus was the most effective for the amelioration of PFS, followed by fulvestrant combined with abemaciclib or palbociclib, and the latter had the smallest incidence of serious adverse events compared to the other 14 treatments. Fulvestrant combined with capecitabine can be used when patients are resistant to everolimus and CDK4/6 inhibitors due to its superior effect on PFS and OS, but application should be scrupulously considered due to its obvious toxic effects. Moreover, fulvestrant combined with CDK4/6 inhibitors was shown to be more effective than AI combined with CDK4/6, and for co-treatment with everolimus, AI combined with everolimus was slightly more effective. PI3K inhibitors are recommended for second-line treatment of patients with PIK3CA mutations.
Footnotes
Conflict of Interest: The authors declare that they have no competing interests.
- Conceptualization: Xu X.
- Data curation: Liu S, Sun X, Xu X, Lin F.
- Formal analysis: Liu S, Sun X, Lin F.
- Funding acquisition: Sun X.
- Investigation: Liu S, Xu X, Lin F.
- Methodology: Liu S, Sun X.
- Project administration: Liu S.
- Resources: Liu S.
- Software: Liu S, Sun X, Xu X.
- Supervision: Xu X, Lin F.
- Validation: Liu S, Xu X, Lin F.
- Visualization: Liu S, Xu X.
- Writing - original draft: Liu S.
- Writing - review & editing: Liu S, Sun X, Xu X, Lin F.
SUPPLEMENTARY MATERIALS
The quality evaluation of included studies
Forest plots of direct comparison. (A) the forest plot of direct comparison for progression-free survival; (B) the forest plot of direct comparison for overall survival; (C) the forest plot of direct comparison for objective response rate; (D) the forest plot of direct comparison for clinical benefit rate.
Indirect comparison of PIK3CA-mutated patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
Indirect comparison of PIK3CA-unmutated patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
Surface under cumulative ranking curve of different endocrine treatment options for progression-free survival. The horizontal ordinate represents the ranking, and the ordinate represents the cumulative possibility. The larger the area under the curve, the better the treatment effect. (A) curve of PI3KCA-mutated patients for progression-free survival; (B) curve of PI3KCA-unmutated patients for progression-free survival; (C) curve of ET resistant patients for progression-free survival; (D) curve of visceral metastasis patients for progression-free survival.
Indirect comparison of ET resistant patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
Indirect comparison of visceral metastases patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
References
- 1.Lindström LS, Karlsson E, Wilking UM, Johansson U, Hartman J, Lidbrink EK, et al. Clinically used breast cancer markers such as estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 are unstable throughout tumor progression. J Clin Oncol. 2012;30:2601–2608. doi: 10.1200/JCO.2011.37.2482. [DOI] [PubMed] [Google Scholar]
- 2.Francis PA, Pagani O, Fleming GF, Walley BA, Colleoni M, Láng I, et al. Tailoring adjuvant endocrine therapy for premenopausal breast cancer. N Engl J Med. 2018;379:122–137. doi: 10.1056/NEJMoa1803164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Milani A, Geuna E, Mittica G, Valabrega G. Overcoming endocrine resistance in metastatic breast cancer: current evidence and future directions. World J Clin Oncol. 2014;5:990–1001. doi: 10.5306/wjco.v5.i5.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanker AB, Sudhan DR, Arteaga CL. Overcoming endocrine resistance in breast cancer. Cancer Cell. 2020;37:496–513. doi: 10.1016/j.ccell.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharifi MN, Anandan A, Grogan P, O'Regan RM. Therapy after cyclin-dependent kinase inhibition in metastatic hormone receptor-positive breast cancer: resistance mechanisms and novel treatment strategies. Cancer. 2020;126:3400–3416. doi: 10.1002/cncr.32931. [DOI] [PubMed] [Google Scholar]
- 6.Grabowsky JA. Drug interactions and the pharmacist: focus on everolimus. Ann Pharmacother. 2013;47:1055–1063. doi: 10.1345/aph.1R769. [DOI] [PubMed] [Google Scholar]
- 7.André F, Ciruelos E, Rubovszky G, Campone M, Loibl S, Rugo HS, et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N Engl J Med. 2019;380:1929–1940. doi: 10.1056/NEJMoa1813904. [DOI] [PubMed] [Google Scholar]
- 8.Jerusalem G, de Boer RH, Hurvitz S, Yardley DA, Kovalenko E, Ejlertsen B, et al. Everolimus plus exemestane vs everolimus or capecitabine monotherapy for estrogen receptor-positive, HER2-negative advanced breast cancer: the BOLERO-6 randomized clinical trial. JAMA Oncol. 2018;4:1367–1374. doi: 10.1001/jamaoncol.2018.2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamilton E, Infante JR. Targeting CDK4/6 in patients with cancer. Cancer Treat Rev. 2016;45:129–138. doi: 10.1016/j.ctrv.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Ciriello G, Gatza ML, Beck AH, Wilkerson MD, Rhie SK, Pastore A, et al. Comprehensive molecular portraits of invasive lobular breast cancer. Cell. 2015;163:506–519. doi: 10.1016/j.cell.2015.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9:153–166. doi: 10.1038/nrc2602. [DOI] [PubMed] [Google Scholar]
- 12.Goetz MP, Toi M, Campone M, Sohn J, Paluch-Shimon S, Huober J, et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. 2017;35:3638–3646. doi: 10.1200/JCO.2017.75.6155. [DOI] [PubMed] [Google Scholar]
- 13.Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med. 2016;375:1738–1748. doi: 10.1056/NEJMoa1609709. [DOI] [PubMed] [Google Scholar]
- 14.Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17:425–439. doi: 10.1016/S1470-2045(15)00613-0. [DOI] [PubMed] [Google Scholar]
- 15.Sledge GW, Jr, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2− advanced breast cancer who had progressed while receiving endocrine therapy. J Clin Oncol. 2017;35:2875–2884. doi: 10.1200/JCO.2017.73.7585. [DOI] [PubMed] [Google Scholar]
- 16.Rossi V, Berchialla P, Giannarelli D, Nisticò C, Ferretti G, Gasparro S, et al. Should all patients with HR-positive HER2-negative metastatic breast cancer receive CDK 4/6 inhibitor as first-line based therapy? A network meta-analysis of data from the PALOMA 2, MONALEESA 2, MONALEESA 7, MONARCH 3, FALCON, SWOG and FACT trials. Cancers (Basel) 2019;11:267–277. doi: 10.3390/cancers11111661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Furlan AD, Pennick V, Bombardier C, van Tulder M Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34:1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 18.Krahn U, Binder H, König J. A graphical tool for locating inconsistency in network meta-analyses. BMC Med Res Methodol. 2013;13:35. doi: 10.1186/1471-2288-13-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howell A, Robertson JF, Abram P, Lichinitser MR, Elledge R, Bajetta E, et al. Comparison of fulvestrant versus tamoxifen for the treatment of advanced breast cancer in postmenopausal women previously untreated with endocrine therapy: a multinational, double-blind, randomized trial. J Clin Oncol. 2004;22:1605–1613. doi: 10.1200/JCO.2004.02.112. [DOI] [PubMed] [Google Scholar]
- 20.Baselga J, Dent SF, Cortés J, Im YH, Diéras Y, Harbeck N, et al. Phase III study of taselisib (GDC-0032) + fulvestrant (FULV) v FULV in patients (pts) with estrogen receptor (ER)-positive, PIK3CA-mutant (MUT), locally advanced or metastatic breast cancer (MBC): Primary analysis from SANDPIPER. J Clin Oncol. 2018;36:LBA1006 [Google Scholar]
- 21.Baselga J, Im SA, Iwata H, Cortés J, De Laurentiis M, Jiang Z, et al. Buparlisib plus fulvestrant versus placebo plus fulvestrant in postmenopausal, hormone receptor-positive, HER2-negative, advanced breast cancer (BELLE-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:904–916. doi: 10.1016/S1470-2045(17)30376-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yardley DA, Noguchi S, Pritchard KI, Burris HA, 3rd, Baselga J, Gnant M, et al. Everolimus plus exemestane in postmenopausal patients with HR+ breast cancer: BOLERO-2 final progression-free survival analysis. Adv Ther. 2013;30:870–884. doi: 10.1007/s12325-013-0060-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Di Leo A, Johnston S, Lee KS, Ciruelos E, Lønning PE, Janni W, et al. Buparlisib plus fulvestrant in postmenopausal women with hormone-receptor-positive, HER2-negative, advanced breast cancer progressing on or after mTOR inhibition (BELLE-3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19:87–100. doi: 10.1016/S1470-2045(17)30688-5. [DOI] [PubMed] [Google Scholar]
- 24.Slamon DJ, Neven P, Chia S, Fasching PA, De Laurentiis M, Im SA, et al. Phase III randomized study of ribociclib and fulvestrant in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: MONALEESA-3. J Clin Oncol. 2018;36:2465–2472. doi: 10.1200/JCO.2018.78.9909. [DOI] [PubMed] [Google Scholar]
- 25.Krop IE, Mayer IA, Ganju V, Dickler M, Johnston S, Morales S, et al. Pictilisib for oestrogen receptor-positive, aromatase inhibitor-resistant, advanced or metastatic breast cancer (FERGI): a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2016;17:811–821. doi: 10.1016/S1470-2045(16)00106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robertson JF, Bondarenko IM, Trishkina E, Dvorkin M, Panasci L, Manikhas A, et al. Fulvestrant 500 mg versus anastrozole 1 mg for hormone receptor-positive advanced breast cancer (FALCON): an international, randomised, double-blind, phase 3 trial. Lancet. 2016;388:2997–3005. doi: 10.1016/S0140-6736(16)32389-3. [DOI] [PubMed] [Google Scholar]
- 27.Jiang Z, Hu X, Zhang Q, Sun T, Yin Y, Li H, et al. LBA25 - MONARCHplus: a phase III trial of abemaciclib plus nonsteroidal aromatase inhibitor (NSAI) or fulvestrant (F) for women with HR+/HER2− advanced breast cancer (ABC) Ann Oncol. 2019;30:v863. [Google Scholar]
- 28.Jiang Z, Li W, Hu X, Zhang Q, Sun T, Cui S, et al. Tucidinostat plus exemestane for postmenopausal patients with advanced, hormone receptor-positive breast cancer (ACE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:806–815. doi: 10.1016/S1470-2045(19)30164-0. [DOI] [PubMed] [Google Scholar]
- 29.Jones RH, Casbard A, Carucci M, Cox C, Butler R, Alchami F, et al. Fulvestrant plus capivasertib versus placebo after relapse or progression on an aromatase inhibitor in metastatic, oestrogen receptor-positive breast cancer (FAKTION): a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2020;21:345–357. doi: 10.1016/S1470-2045(19)30817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim JY, Im SA, Jung KH, Ro J, Sohn J, Kim JH, et al. Fulvestrant plus goserelin versus anastrozole plus goserelin versus goserelin alone for hormone receptor-positive, HER2-negative tamoxifen-pretreated premenopausal women with recurrent or metastatic breast cancer (KCSG BR10-04): a multicentre, open-label, three-arm, randomised phase II trial (FLAG study) Eur J Cancer. 2018;103:127–136. doi: 10.1016/j.ejca.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 31.Dickler MN, Barry WT, Cirrincione CT, Ellis MJ, Moynahan ME, Innocenti F, et al. Phase III trial evaluating letrozole as first-line endocrine therapy with or without bevacizumab for the treatment of postmenopausal women with hormone receptor-positive advanced-stage breast cancer: CALGB 40503 (Alliance) J Clin Oncol. 2016;34:2602–2609. doi: 10.1200/JCO.2015.66.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Musolino A, Campone M, Neven P, Denduluri N, Barrios CH, Cortes J, et al. Phase II, randomized, placebo-controlled study of dovitinib in combination with fulvestrant in postmenopausal patients with HR+, HER2− breast cancer that had progressed during or after prior endocrine therapy. Breast Cancer Res. 2017;19:18. doi: 10.1186/s13058-017-0807-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kornblum N, Zhao F, Manola J, Klein P, Ramaswamy B, Brufsky A, et al. Randomized phase II trial of fulvestrant plus everolimus or placebo in postmenopausal women with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer resistant to aromatase inhibitor therapy: results of PrE0102. J Clin Oncol. 2018;36:1556–1563. doi: 10.1200/JCO.2017.76.9331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park YH, Kim TY, Kim GM, Jung KH, Kang SY, Park IH, et al. A randomized phase II study of palbociclib plus exemestane with GNRH agonist versus capecitabine in premenopausal women with hormone receptorpositive metastatic breast cancer (KCSG-BR 15-10, NCT02592746) J Clin Oncol. 2019;37:1007. [Google Scholar]
- 35.Paul D, Vukelja SJ, Ann Holmes F, Blum JL, McIntyre KJ, Lindquist DL, et al. Randomized phase-II evaluation of letrozole plus dasatinib in hormone receptor positive metastatic breast cancer patients. NPJ Breast Cancer. 2019;5:36. doi: 10.1038/s41523-019-0132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol. 2015;16:25–35. doi: 10.1016/S1470-2045(14)71159-3. [DOI] [PubMed] [Google Scholar]
- 37.Finn RS, Martin M, Rugo HS, Jones S, Im SA, Gelmon K, et al. Palbociclib and letrozole in advanced breast cancer. N Engl J Med. 2016;375:1925–1936. doi: 10.1056/NEJMoa1607303. [DOI] [PubMed] [Google Scholar]
- 38.Mehta RS, Barlow WE, Albain KS, Vandenberg TA, Dakhil SR, Tirumali NR, et al. Combination anastrozole and fulvestrant in metastatic breast cancer. N Engl J Med. 2012;367:435–444. doi: 10.1056/NEJMoa1201622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Johnston SR, Kilburn LS, Ellis P, Dodwell D, Cameron D, Hayward L, et al. Fulvestrant plus anastrozole or placebo versus exemestane alone after progression on non-steroidal aromatase inhibitors in postmenopausal patients with hormone-receptor-positive locally advanced or metastatic breast cancer (SoFEA): a composite, multicentre, phase 3 randomised trial. Lancet Oncol. 2013;14:989–998. doi: 10.1016/S1470-2045(13)70322-X. [DOI] [PubMed] [Google Scholar]
- 40.Trédan O, Follana P, Moullet I, Cropet C, Trager-Maury S, Dauba J, et al. A phase III trial of exemestane plus bevacizumab maintenance therapy in patients with metastatic breast cancer after first-line taxane and bevacizumab: a GINECO group study. Ann Oncol. 2016;27:1020–1029. doi: 10.1093/annonc/mdw077. [DOI] [PubMed] [Google Scholar]
- 41.Tripathy D, Im SA, Colleoni M, Franke F, Bardia A, Harbeck N, et al. Ribociclib plus endocrine therapy for premenopausal women with hormone-receptor-positive, advanced breast cancer (MONALEESA-7): a randomised phase 3 trial. Lancet Oncol. 2018;19:904–915. doi: 10.1016/S1470-2045(18)30292-4. [DOI] [PubMed] [Google Scholar]
- 42.Cristofanilli M, Slamon DJ, Ro J, Bondarenko I, Im SA, Masuda N, et al. Overall survival (OS) with palbociclib plus fulvestrant in women with hormone receptor-positive (HR1), human epidermal growth factor receptor 2-negative (HER2) advanced breast cancer (ABC): analyses from PALOMA-3. Ann Oncol. 2018;29:viii708 [Google Scholar]
- 43.Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, et al. Updated results from MONALEESA-2, a phase 3 trial of first-line ribociclib + letrozole in hormone receptor-positive (HR+), HER2-negative (HER2−), advanced breast cancer (ABC) J Clin Oncol. 2017;35:1038. [Google Scholar]
- 44.Im SA, Lu YS, Bardia A, Harbeck N, Colleoni M, Franke F, et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. N Engl J Med. 2019;381:307–316. doi: 10.1056/NEJMoa1903765. [DOI] [PubMed] [Google Scholar]
- 45.Sledge GW, Jr, Toi M, Neven P, Sohn J, Inoue K, Pivot X, et al. The effect of abemaciclib plus fulvestrant on overall survival in hormone receptor-positive, ERBB2-negative breast cancer that progressed on endocrine therapy-MONARCH 2: a randomized clinical trial. JAMA Oncol. 2019;6:116–124. doi: 10.1001/jamaoncol.2019.4782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Turner NC, Slamon DJ, Ro J, Bondarenko I, Im SA, Masuda N, et al. Overall survival with palbociclib and fulvestrant in advanced breast cancer. N Engl J Med. 2018;379:1926–1936. doi: 10.1056/NEJMoa1810527. [DOI] [PubMed] [Google Scholar]
- 47.Piccart M, Hortobagyi GN, Campone M, Pritchard KI, Lebrun F, Ito Y, et al. Everolimus plus exemestane for hormone-receptor-positive, human epidermal growth factor receptor-2-negative advanced breast cancer: overall survival results from BOLERO-2. Ann Oncol. 2014;25:2357–2362. doi: 10.1093/annonc/mdu456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moher D, Liberati A, Tetzlaff J, Altman D, Antes G, Atkins D, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Rev Esp Nutr Hum Diet. 2014;18:172–181. [Google Scholar]
- 49.Partridge AH, Rumble RB, Carey LA, Come SE, Davidson NE, Di Leo A, et al. Chemotherapy and targeted therapy for women with human epidermal growth factor receptor 2-negative (or unknown) advanced breast cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32:3307–3329. doi: 10.1200/JCO.2014.56.7479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vernieri C, Corti F, Nichetti F, Ligorio F, Manglaviti S, Zattarin E, et al. Everolimus versus alpelisib in advanced hormone receptor-positive HER2-negative breast cancer: targeting different nodes of the PI3K/AKT/mTORC1 pathway with different clinical implications. Breast Cancer Res. 2020;22:33. doi: 10.1186/s13058-020-01271-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schiff R, Massarweh SA, Shou J, Bharwani L, Mohsin SK, Osborne CK. Cross-talk between estrogen receptor and growth factor pathways as a molecular target for overcoming endocrine resistance. Clin Cancer Res. 2004;10:331S–336S. doi: 10.1158/1078-0432.ccr-031212. [DOI] [PubMed] [Google Scholar]
- 52.Boulay A, Rudloff J, Ye J, Zumstein-Mecker S, O'Reilly T, Evans DB, et al. Dual inhibition of mTOR and estrogen receptor signaling in vitro induces cell death in models of breast cancer. Clin Cancer Res. 2005;11:5319–5328. doi: 10.1158/1078-0432.CCR-04-2402. [DOI] [PubMed] [Google Scholar]
- 53.O'Donnell A, Faivre S, Burris HA, 3rd, Rea D, Papadimitrakopoulou V, Shand N, et al. Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol. 2008;26:1588–1595. doi: 10.1200/JCO.2007.14.0988. [DOI] [PubMed] [Google Scholar]
- 54.Baselga J, Campone M, Piccart M, Burris HA, 3rd, Rugo HS, Sahmoud T, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520–529. doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shapiro GI. Cyclin-dependent kinase pathways as targets for cancer treatment. J Clin Oncol. 2006;24:1770–1783. doi: 10.1200/JCO.2005.03.7689. [DOI] [PubMed] [Google Scholar]
- 56.Patnaik A, Rosen LS, Tolaney SM, Tolcher AW, Goldman JW, Gandhi L, et al. Efficacy and safety of abemaciclib, an inhibitor of CDK4 and CDK6, for patients with breast cancer, non-small cell lung cancer, and other solid tumors. Cancer Discov. 2016;6:740–753. doi: 10.1158/2159-8290.CD-16-0095. [DOI] [PubMed] [Google Scholar]
- 57.Kim S, Loo A, Chopra R, Caponigro G, Huang A, Vora S, et al. LEE011: an orally bioavailable, selective small molecule inhibitor of CDK4/6- reactivating Rb in cancer. Mol Cancer Ther. 2013;12:PR02. [Google Scholar]
- 58.Finn RS, Dering J, Conklin D, Kalous O, Cohen DJ, Desai AJ, et al. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro . Breast Cancer Res. 2009;11:R77. doi: 10.1186/bcr2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dickler MN, Tolaney SM, Rugo HS, Cortés J, Diéras V, Patt D, et al. MONARCH 1, a phase II study of abemaciclib, a CDK4 and CDK6 inhibitor, as a single agent, in patients with refractory HR+/HER2− metastatic breast cancer. Clin Cancer Res. 2017;23:5218–5224. doi: 10.1158/1078-0432.CCR-17-0754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Falkenberg KJ, Johnstone RW. Histone deacetylases and their inhibitors in cancer, neurological diseases and immune disorders. Nat Rev Drug Discov. 2014;13:673–691. doi: 10.1038/nrd4360. [DOI] [PubMed] [Google Scholar]
- 61.Dey JH, Bianchi F, Voshol J, Bonenfant D, Oakeley EJ, Hynes NE. Targeting fibroblast growth factor receptors blocks PI3K/AKT signaling, induces apoptosis, and impairs mammary tumor outgrowth and metastasis. Cancer Res. 2010;70:4151–4162. doi: 10.1158/0008-5472.CAN-09-4479. [DOI] [PubMed] [Google Scholar]
- 62.Ning ZQ, Li ZB, Newman MJ, Shan S, Wang XH, Pan DS, et al. Chidamide (CS055/HBI-8000): a new histone deacetylase inhibitor of the benzamide class with antitumor activity and the ability to enhance immune cell-mediated tumor cell cytotoxicity. Cancer Chemother Pharmacol. 2012;69:901–909. doi: 10.1007/s00280-011-1766-x. [DOI] [PubMed] [Google Scholar]
- 63.Khongthong P, Roseweir AK, Edwards J. The NF-κB pathway and endocrine therapy resistance in breast cancer. Endocr Relat Cancer. 2019;26:R369–80. [PubMed] [Google Scholar]
- 64.Verret B, Cortes J, Bachelot T, Andre F, Arnedos M. Efficacy of PI3K inhibitors in advanced breast cancer. Ann Oncol. 2019;36:x12–20. doi: 10.1093/annonc/mdz381. [DOI] [PubMed] [Google Scholar]
- 65.Bergh J, Jönsson PE, Lidbrink EK, Trudeau M, Eiermann W, Brattström D, et al. FACT: an open-label randomized phase III study of fulvestrant and anastrozole in combination compared with anastrozole alone as first-line therapy for patients with receptor-positive postmenopausal breast cancer. J Clin Oncol. 2012;30:1919–1925. doi: 10.1200/JCO.2011.38.1095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The quality evaluation of included studies
Forest plots of direct comparison. (A) the forest plot of direct comparison for progression-free survival; (B) the forest plot of direct comparison for overall survival; (C) the forest plot of direct comparison for objective response rate; (D) the forest plot of direct comparison for clinical benefit rate.
Indirect comparison of PIK3CA-mutated patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
Indirect comparison of PIK3CA-unmutated patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
Surface under cumulative ranking curve of different endocrine treatment options for progression-free survival. The horizontal ordinate represents the ranking, and the ordinate represents the cumulative possibility. The larger the area under the curve, the better the treatment effect. (A) curve of PI3KCA-mutated patients for progression-free survival; (B) curve of PI3KCA-unmutated patients for progression-free survival; (C) curve of ET resistant patients for progression-free survival; (D) curve of visceral metastasis patients for progression-free survival.
Indirect comparison of ET resistant patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.
Indirect comparison of visceral metastases patients in progression-free survival. The values represent HR (95% CI) and bold font indicates that the results had significant statistical difference.