Abstract
Scleritis is an idiopathic condition that may sometimes be associated with systemic immunological like disorders rheumatoid arthritis, Wegener’s granulomatosis and systemic lupus erythematosus. A variety of foreign material has been reported to result in granuloma formation in various parts of the body. We report a case of inflamed episcleral granulomas mimicking severe nodular anterior scleritis in a healthy Caucasian woman who underwent strabismus surgery in her childhood. Foreign body reaction on the episcleral/scleral surface is rare. It is extremely unusual for a non-absorbable suture that was used for childhood strabismus surgery to incite an acute inflammatory episode mimicking nodular anterior scleritis as in our case. As the strabismus surgery was performed 37 years prior to her presentation with anterior scleritis, we were unable to obtain any details of this surgical procedure. We presume that a non-absorbable suture like braided polyester or prolene may have been used.
Keywords: eye, ophthalmology
Background
Nodular scleritis is the second most common clinical presentation of anterior scleritis, accounting for approximately 20% of scleritis cases. The differential diagnosis for anterior scleritis includes episcleritis and severe microbial conjunctivitis. Suture granulomas are a rare complication of surgery. Foreign body granuloma formation on the episcleral/scleral surface is rare. It is extremely unusual for a non-absorbable suture that was used for childhood strabismus surgery to incite an acute inflammatory episode 37 years later mimicking acute nodular anterior scleritis as presented in this case report.
Case presentation
A 45-year-old Caucasian woman presented with a 3-day history of red, tender right eye (RE) associated with frontal headache that was exacerbated by eye movements. There was no history of trauma or any systemic medical illness. Her ocular history was significant for strabismus surgery in the RE at the age of 8 years. Details of the surgical procedure were unavailable. On examination, uncorrected visual acuities were 6/24 in RE and 6/6 in the left eye. Slit lamp examination revealed localised conjunctival and episcleral injection in the superonasal quadrant. Within this inflamed area, there were firm, immobile, nodular masses with no clinical evidence of necrosis (figure 1). Intraocular pressures and dilated fundus examination were unremarkable in both eyes. Ten per cent topical phenylephrine test revealed mild blanching of the conjunctival and episcleral vessels. No evidence of any microbial infection was found on conjunctival swabs. A thorough systemic work up, including detailed personal and family history along with haematological investigations, was performed.
Figure 1.
(A) Slit lamp picture of the right eye (RE) showing localised scleral inflammation in the superonasal quadrant on presentation. (B) Slit lamp picture of the RE following topical steroids and oral non-steroidal anti-inflammatory therapy. Note the mild reduction in the inflammation. (C) Slit lamp picture of the RE showing the areas of suture granulomas over the insertion of medial rectus (red arrows).(D) Resolution of ocular surface inflammation postoperatively.
Investigations
All haematological investigations, namely, complete blood count, erythrocyte sedimentation rate, C reactive protein, rheumatoid factor, antineutrophilic cytoplasmic antibody test, anti-Rho and anti-La antibodies testing was all within normal limits.
Differential diagnosis
Ten per cent topical phenylephrine test revealed mild blanching of the conjunctival and episcleral vessels. No evidence of any microbial infection was found on conjunctival swabs. Based on the appearance, a clinical diagnosis of localised, nodular, non-necrotising anterior scleritis was reached. She was commenced on topical 0.1% dexamethasone drops four times a day and oral ibuprofen 400 mg tablets three times a day for a period of 4 weeks. Due to minimal improvement in signs and symptoms (figure 1), oral ibuprofen was discontinued, and 40 mg of oral steroids was commenced for 4 weeks. Intolerance to the oral steroids developed soon after the commencement of oral steroids and sub-Tenon’s injection of 0.4 mL triamcinolone acetate in OD. Four weeks later, examination revealed reduction in the ocular surface inflammation with localised area of inflammation over the sutures from her previous strabismus surgery (figure 1). These localised inflamed granulomas were unmasked following reduction of the ocular surface inflammation. At this point, a clinical diagnosis of suture-induced episcleral inflammation was entertained, and following informed consent, patient underwent excision of the suture granuloma with reconstruction of the ocular surface with amniotic membrane under local anaesthesia (figure 2).
Figure 2.
(A) Intraoperative photograph showing peritomy and tenectomy. (B) Intraoperative photograph showing the inflamed scleral nodule over the insertion of medial rectus (black arrow). (C) Intraoperative photograph showing the excised scleral nodule (yellow arrow). (D) Intraoperative photograph showing reconstruction of the ocular surface with amniotic membrane.
Treatment
Following informed consent patient underwent excision of the suture granuloma with reconstruction of the ocular surface with amniotic membrane under local anaesthesia (figure 2). The procedure was performed in the operating room under standard aseptic procedures. Following topical 0.5% proxymetacaine and subconjunctival anaesthesia (2% lidocaine with 1 in 10 000 epinephrine) a localised peritomy was performed. Two suture granulomata were identified and excised in toto with the offending suture. Following this, the ocular surface was reconstructed with amniotic membrane. There were no intraoperative complications. Postoperatively, she was treated with topical steroids and antibiotics for a period of 4 weeks. Histological examination confirmed episcleral suture granuloma consisting of granulation tissue containing birefringent multi-stranded suture material surrounded by a foreign body giant cell reaction (figure 3).
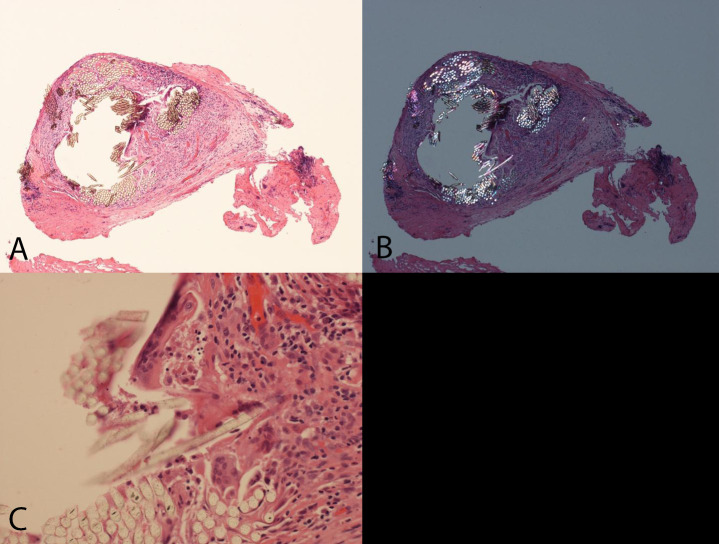
Figure 3.
(A) Suture material surrounded by granulation tissue (H&E, ×100). (B) Suture material is refractile under polarised light (H&E, ×100). (C) Suture material surrounded by a foreign body giant cell reaction (H&E, ×200).
Outcome and follow-up
Postoperative recovery was uneventful and 4 weeks following the surgical procedure there was complete resolution of the ocular surface inflammation and the patient was asymptomatic (figure 1). Six and 12 months follow-up showed a quite ocular surface with no recurrence of any inflammation. The patient is well and alive and attends for yearly review.
Discussion
Scleritis can present as isolated conditions or as part of a systemic inflammatory or infectious disorder. It is a potentially serious ocular condition that can result in vision loss and, therefore, require early diagnosis and treatment. The prevalence of scleritis in the general population is estimated to be 6 cases per 100 000, but has been described in between 0.2% and 6.3% of patients with rheumatoid arthritis and up to 7% of those with granulomatous polyangiitis.1
The Watson and Hayreh classification of scleritis2 divides the disorder into anterior and posterior types based on the anatomic distribution of disease. Anterior scleritis is further subdivided into diffuse, nodular, necrotising with inflammation and necrotising without inflammation (scleromalacia perforans).
Nodular scleritis is the second most common clinical presentation of anterior scleritis, accounting for approximately 20% of scleritis cases.3 The differential diagnosis for anterior scleritis includes episcleritis and severe microbial conjunctivitis. Suture granulomas are a rare complication of surgery.4 The clinical presentation of a suture granuloma may vary from a classic acute inflammatory reaction to a chronic granuloma.5 6 In the ophthalmic literature, suture granuloma has been reported in association with nylon suture following upper blepharoplasty,7 braided polyester suture following post pulley fixation suture and transconjunctival blepharoplasty8 9 and prolene suture following sling surgery.10
Foreign body reaction on the episcleral/scleral surface is rare. One of the authors (SS) reported two cases of episcleral granulomata adjacent to vitrectomy entry sites in patients who underwent vitrectomy with silicone oil tamponade.11 It is extremely unusual for a non-absorbable suture that was used for childhood strabismus surgery to incite an acute inflammatory episode mimicking nodular anterior scleritis as in our case. As the strabismus surgery was performed 37 years prior to her presentation with anterior scleritis, we were unable to obtain any details of this surgical procedure. We presume that a non-absorbable suture like braided polyester or prolene may have been used. No triggers have been identified for the presentation of her symptoms 37 years after the procedure. Although both these sutures have been reported to cause conjunctival granulomata,8–10 we believe that this may be the first report of episcleral granulomata from a non-absorbable suture mimicking nodular anterior scleritis.
Patient’s perspective.
This is been a roller coaster ride for me. I was initially diagnosed with nodular scleritis. Halfway through the treatment—Professor Srinivasan noted some sutures on the surface of my right eye and enquired with my mother (who had accompanied me to one of the clinic visits) whether I had undergone squint surgery as a child. I was too young to remember this. The penny dropped when my mother confirmed to Professor Srinivasan that indeed I had squint surgery as a child. I am so grateful to Professor Srinivasan for making the correct diagnosis and treating me. Since the surgery to remove the nodules from my right eye, I have been symptom free for more than a year now.
Learning points.
Nodular anterior scleritis is usually associated with underlying connective disorders, most commonly rheumatoid arthritis.
Rarely foreign body induced episcleral granulomas can mimic nodular anterior scleritis.
Thorough history may provide clue on previous ocular surgery.
Footnotes
Contributors: LWK and SS were involved in the design and writing of the manuscript. FR provided the expertise for the pathology and helped in providing the pathology pictures and reviewed the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Galor A, Thorne JE. Scleritis and peripheral ulcerative keratitis. Rheum Dis Clin North Am 2007;33:835–54. 10.1016/j.rdc.2007.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watson PG, Hayreh SS. Scleritis and episcleritis. Br J Ophthalmol 1976;60:163–91. 10.1136/bjo.60.3.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jabs DA, Mudun A, Dunn JP, et al. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol 2000;130:469–76. 10.1016/S0002-9394(00)00710-8 [DOI] [PubMed] [Google Scholar]
- 4.Secil M, Mungan U, Yorukoglu K. Suture granuloma after orchiectomy: sonography, doppler and elastography features. Int braz j urol. 2015;41:813–6. 10.1590/S1677-5538.IBJU.2013.0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eldridge PR, Wheeler MH. Stitch granulomata after thyroid surgery. Br J Surg 1987;74:62 10.1002/bjs.1800740119 [DOI] [PubMed] [Google Scholar]
- 6.Jung E, Park W-H, Choi S-O. Mesenteric suture granuloma caused by retained fragments of suture material in a Girl who had a laparotomy 12years previously. J Pediatr Surg 2013;48:e25–7. 10.1016/j.jpedsurg.2012.10.051 [DOI] [PubMed] [Google Scholar]
- 7.Kim YJ, Kim J, Choung H, et al. Conjunctival granuloma with necrosis associated with exposed suture in upper double lid masquerading as ocular surface squamous neoplasia: a case report. BMC Ophthalmol 2017;17 10.1186/s12886-017-0457-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soll SM, Lisman RD, Charles NC, et al. Pyogenic granuloma after transconjunctival blepharoplasty. Ophthalmic Plast Reconstr Surg 1993;9:298–301. 10.1097/00002341-199312000-00013 [DOI] [PubMed] [Google Scholar]
- 9.Mathew AA, Kowal L. Conjunctival granuloma post pulley fixation suture. J AAPOS 2017;21:342–3. 10.1016/j.jaapos.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 10.Mehta A, Naik M, Abrol S, et al. Granuloma after sling surgery: an attempt to answer the ‘why’ and ‘what to do next’. Int Ophthalmol 2017;37:973–7. 10.1007/s10792-016-0342-0 [DOI] [PubMed] [Google Scholar]
- 11.Srinivasan S, Singh AK, Desai SP, et al. Foreign body episcleral granulomas complicating intravitreal silicone oil tamponade. Ophthalmology 2003;110:1837–40. 10.1016/S0161-6420(03)00571-2 [DOI] [PubMed] [Google Scholar]