Abstract
Background
Afterschool interventions have been found to improve the nutritional quality of snacks served. However, there is limited evidence on how these interventions affect children’s snacking behaviors.
Objective
To determine the impact of an afterschool intervention focused at the school district, site, family, and child levels on dietary consumption of foods and beverages served at snack.
Design
Secondary analysis of a group-randomized controlled trial.
Participants/setting
Data were collected from 400 children at 20 Boston, MA afterschool sites before (fall 2010) and after (spring 2011) intervention implementation.
Intervention
The Out-of-School Nutrition and Physical Activity intervention aimed to promote fruits, vegetables, whole grains, and water, while limiting sugary drinks and trans fats. Researchers worked with district foodservice staff to change snack foods and beverages. Teams of afterschool staff participated in three three-hour learning collaborative sessions to build skills and created action plans for changing site practices. The intervention included family and child nutrition education.
Main outcome measures
Research assistants observed dietary snack consumption using a validated measure on two days per site at baseline and follow-up.
Statistical Analyses Performed
This study used multivariable regression models, accounting for clustering of observations, to assess the intervention effect, and conducted post-hoc stratified analyses by foodservice type.
Results
Children in intervention sites had greater decreases in consumption of juice (−0.61 ounces/snack, 95% CI −1.11 – −0.12), beverage calories (−29.0 kcal/snack, 95% CI −40.1 – −17.9), foods with trans fats (−0.12 servings/snack, 95% CI −0.19 – −0.04), total calories (−47.8 kcal/snack, 95% CI −68.3 – −27.3) and increases in consumption of whole grains (0.10 servings/snack, 95% CI 0.02–0.18) compared to controls. In post hoc analyses, sites with on-site foodservice had significant improvements for all outcomes (p<0.001), with no effect for sites with satellite foodservice.
Conclusions
Results demonstrate that an afterschool intervention can improve children’s dietary snack consumption, particularly at sites with on-site foodservice.
Keywords: Nutrition, afterschool, snack, childhood obesity, group randomized trial
INTRODUCTION
Addressing obesity prevention in community settings early in life is an essential strategy for population impact given that obesity prevalence in the United States (U.S.) has steadily increased over the past two decades. Today obesity affects over one third of children and youth and disproportionately impacts minority and economically disadvantaged children.1–3 Dietary intake has been strongly linked to childhood obesity via caloric imbalance,4 particularly due to excess calories from sugary beverages.5–7 The American Academy of Pediatrics and recent Dietary Guidelines for Americans suggest that children limit consumption of sugar-sweetened drinks and 100% juice; eat a diet rich in fruits, vegetables, calcium, and fiber; limit consumption of energy-dense foods; and limit portion size.8,9
Afterschool sites are an important community setting for addressing childhood obesity prevention.10–12 The Afterschool Alliance estimates that 10.2 million U.S. children are enrolled in afterschool programming,13 and 46% of school foodservice directors report their district provides afterschool snacks for students.14 Moreover, afterschool settings have the potential to address racial/ethnic and socioeconomic disparities; the highest participation rates in U.S. afterschool programming are among low income, Black/African-American, and Hispanic/Latino children.15
Improving children’s snacking behaviors is a relatively unexplored area of intervention; however, evidence suggests that investments in this area are worthwhile. Foods and drinks children consume outside of traditional meals make up over 25% of their daily consumption16 and the nutritional quality of snacks children consume has declined over the past three decades.17 In afterschool settings more specifically, recent evidence has documented that snacks do not meet the National Afterschool Association Healthy Eating Standards.18 The majority of sites served sugar-sweetened foods and beverages, while fruits and vegetables were served infrequently.12 Even given these needs for improvement, afterschool program-provided snacks have been shown to be of greater quality than snacks from home19 and changes to afterschool sites have potentially greater reach than working with individual families.
Although a number of obesity prevention studies have been situated in afterschool settings, many of these interventions have been limited in duration and scope or focused exclusively on individual behavior and attitude change (e.g. increasing children’s nutrition knowledge) rather than environmental approaches (e.g. improving the healthfulness of foods and beverages served on-site).20–22 Some promising interventions have taken a more comprehensive approach via changes to foods and beverages served in afterschool sites over a longer time course, but these studies have not measured changes in foods and beverages consumed.23–28 Prior studies found that weekly servings of fruits, vegetables, and water increased and foods with added sugars and trans fats decreased after afterschool sites participated in a YMCA-driven learning collaborative.29 There is also prior evidence of high fruit and vegetable consumption after an afterschool/grocery store partnership intervention.30 This current study fill a gap in the research by determining whether afterschool interventions that rely on foodservice operators and vendors, rather than independent program purchasing or grocery store partnerships, are similarly effective.
The Out-of-School Nutrition and Physical Activity (OSNAP) intervention is a community-based participatory research study aimed at the school district, afterschool, family, and child levels designed to identify and support sustainable policy and environmental strategies that promote increased access to and consumption of healthy snacks and physical activity in afterschool settings.31 This study is the first of its kind to examine the impact of an intervention in afterschool settings on children’s dietary intake when snacks are served. Our hypothesis was that children who attended intervention sites would have greater increases in fruit and vegetable and whole grain consumption and greater decreases in juice, beverage calories, foods with trans fats, and total calories than children who attended control sites. Secondarily, post-hoc stratified analyses were conducted to determine if the type of foodservice operations used for afterschool snack influenced changes in snack consumption.
MATERIALS AND METHODS
Design
The study was a group-randomized controlled trial in 20 afterschool sites in Boston, Massachusetts. The flow diagram in Figure 1 shows details on enrollment. Eligible sites enrolled at least 39 children, served elementary grades, and ran throughout the school year. The study team designated 10 matched pairs, matching sites first on sponsoring agency (e.g. YMCA), then on size, and finally on foodservice type (e.g. on-site, satellite, independent) and physical activity facilities (e.g. gym, playground, pool). With only 10 pairs, matching was imperfect but it was used to improve the chance of well-balanced intervention and control groups. One site from each matched pair was randomized to the intervention condition by someone not involved in the study using a computer-based random number generator after baseline data collection was complete. Researchers were not blinded to intervention status; data collectors conducting observations were blinded. OSNAP was implemented in 10 intervention sites during the 2010–2011 school year, and 10 sites served as controls. The control group was offered a similar intervention during the subsequent 2011–2012 school year. The trial was powered with the primary outcome of increased moderate and vigorous physical activity31 with secondary outcomes of improved quality of food and beverage consumption. All human subjects study protocols were approved by the Harvard T.H. Chan School of Public Health Office of Human Research Administration (Trial Registration: NCT01396473).
Figure 1.
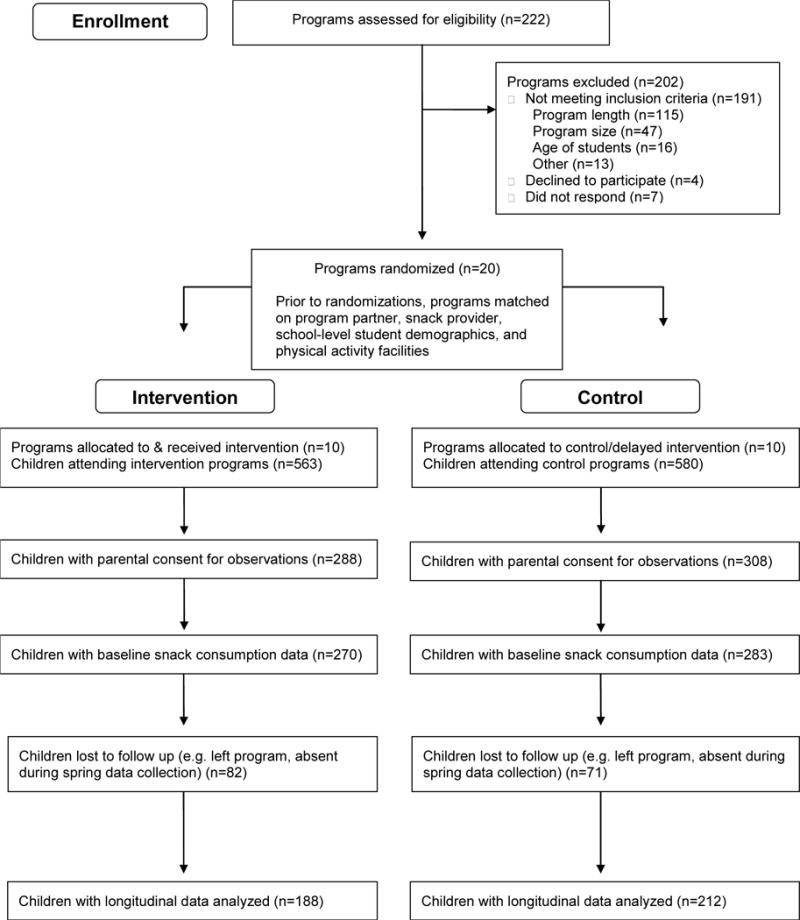
Out-of-school Nutrition and Physical Activity (OSNAP) Randomized Control Trial Site Recruitment and Child Participation for Dietary Outcomes
Study population
All children five years and older attending the 20 afterschool sites were eligible to participate in a direct observation protocol to evaluate the intervention impact on dietary intake. At baseline, trained research assistants obtained parents’ or guardians’ written informed consent and verbal child assent for participating in dietary intake observations. Parental consent was obtained for 52% (596) of children who attended the 20 afterschool sites at baseline. The final longitudinal sample of 400 children had known age and gender and at least one day of snack consumption data at both baseline and follow-up. Figure 1 provides additional details on the recruitment of participants. All children enrolled in intervention sites were considered exposed to the multi-level environmental and policy intervention.
Intervention
The social ecological model guided the study’s design, implementation, and evaluation.32 OSNAP targeted multiple levels of change—school district, afterschool site, family, and child. The intervention aimed to increase children’s consumption of fruits, vegetables, whole grains, and water and decrease consumption of sugary drinks (including large servings of 100% juice) and trans fats. Figure 2 depicts each of the intervention levels of change, activities, and anticipated outcomes. Intervention materials and measures were piloted in spring 2010 at four Boston-based afterschool sites with similar sponsoring agencies, foodservice, enrollment size, and demographics. An advisory board, consisting of school foodservice personnel, afterschool leaders, and other community partners helped guide OSNAP planning and implementation.
Figure 2.
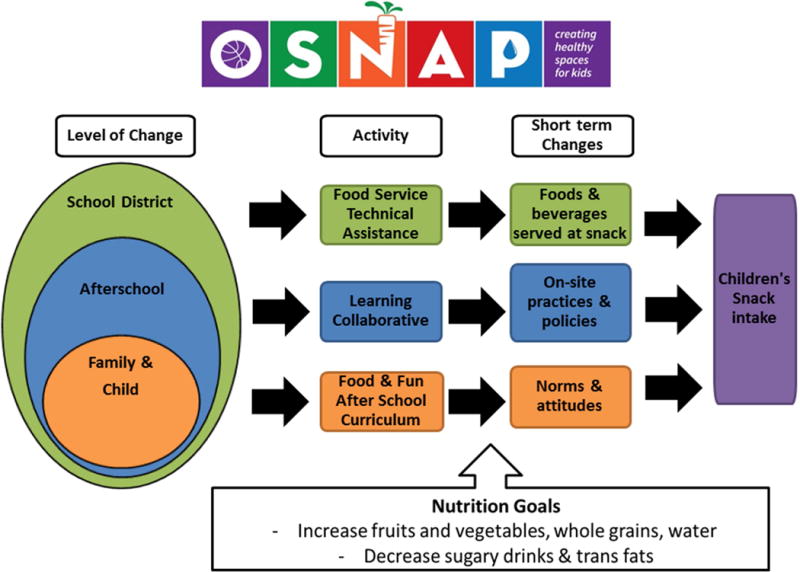
Out-of-school Nutrition and Physical Activity (OSNAP) Multilevel Intervention
School district foodservice intervention
After baseline data collection, intervention sites received technical assistance from the research team to change foods and beverages offered at afterschool snack. The research team worked with the Boston Public Schools Food and Nutrition Services Department to revise four-week snack cycle menus to increase the frequency of servings and variety and quality of fruits and vegetables like bananas, apples, oranges, canned pears and peaches; reduce the frequency of 100% juice and limit servings to 4oz; remove foods with partially hydrogenated oils; and include more whole grain foods at intervention sites. Changes were informed by the finding that replacing juice with water contributes considerable cost savings that can be put towards purchasing fruits and vegetables.33 All revised menus, an example of which can be found on the OSNAP website,34 met the USDA’s National School Lunch Program35 snack guidelines. Implementation included meeting with intervention site school foodservice directors prior to a regularly scheduled all-district staff meeting to describe the intervention aims and menus changes. Food vendor bids were used to identify healthy, low-cost changes for the snack menus. We assumed that these changes could be made at all intervention sites served by the district, regardless of their foodservice operation type. Seven on-site foodservice sites (four intervention, three control) had their snacks prepared in full-service kitchens at the school where the afterschool site was situated, while 11 satellite foodservice sites (five intervention, six control) that did not have the facilities to cook meals received pre-prepared snacks delivered from an outside vendor via a contract with the school system. Two sites that did not receive their snacks from the district received menu planning guidance during the learning collaborative sessions for the snacks they procured independently.14
Afterschool learning collaborative intervention
Directors and support staff from intervention sites were invited to participate in three, three-hour learning collaborative sessions during the 2010–2011 school year. All sessions focused on creating changes to on-site afterschool practices and policies that promote consumption of fruits, vegetables, and whole grains and limit sugary drinks and trans fats (see Figure 3 for detailed content). To meet the time and location needs of staff, learning collaboratives were delivered via three tracks in afterschool spaces through Boston. Attendees received a $40 stipend for attendance at each session. The research team developed the intervention content and facilitated sessions, which were designed consistent with the Institute for Healthcare Improvement Breakthrough Series Collaborative model, originally designed to bring teams together for making complex organizational changes in clinical settings,36 and used constructs from social cognitive theory to drive behavior change.37 Sessions were designed to improve participants’ behavioral capability via the development of knowledge and skills related to specific intervention targets. Goals setting and the identification of perceived barriers and facilitators for change were used at each session to increase self-efficacy and ultimately improve the afterschool nutrition and physical activity environment. Afterschool staff were encouraged to share promising practices and worked in teams to implement two to four of the OSNAP goals with corresponding practice, policy, and communication action steps to be implemented throughout the year. Technical assistance between meetings included emails and calls reminding participants of the goals they set with supporting materials (e.g. curriculum, equipment, sample policy language) to achieve each step on their action plan. Free intervention tools are available on the OSNAP website.38 Examples of these materials include the OSNAP Policy Writing Guide,39 Whole Grain Tip Sheet,40 Fruit and Vegetable Fast Map decision aid,41 and Guide to Working with Food Service.42
Figure 3.
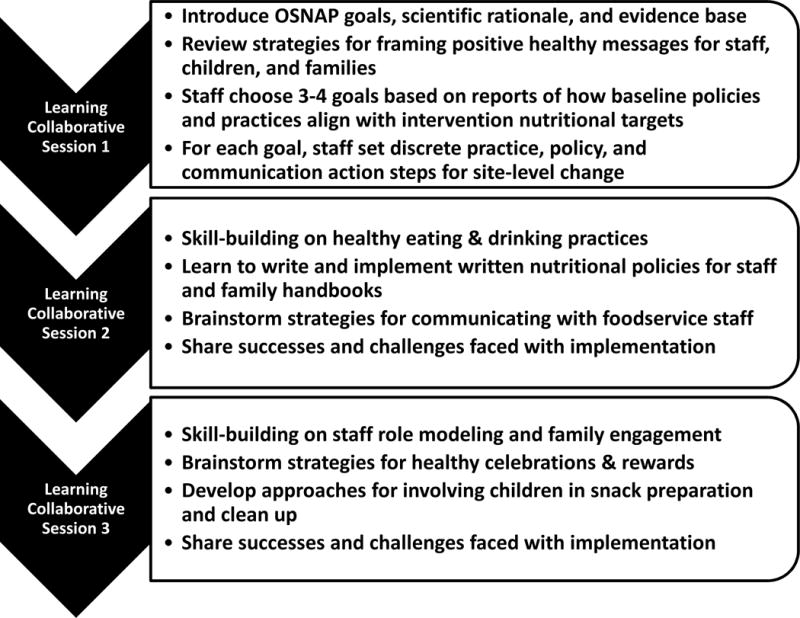
Out-of-school Nutrition and Physical Activity (OSNAP) Learning Collaborative Content
Child and family educational intervention
To address the knowledge and attitudes of children and their families around fruits, vegetables, whole grains, sugary drinks and fats, staff received the free Food and Fun After School curriculum43 and were invited to participate in a two-hour training. The curriculum was developed using social cognitive theory with activities designed to increase knowledge and build self-efficacy for healthy decision-making among children and families.37 It includes lessons that encourage healthy behaviors through active play, literacy and math skills development, creative learning, and snack time activities. Each unit includes newsletters, email templates, and handouts (available in English, Spanish, and Chinese) to communicate nutrition messages to families.
Measures
Dietary consumption
Data were collected in fall 2010 (baseline) and again in spring 2011 (follow-up). The type, size, and brand of all food and beverage items served each day (Monday – Friday) were documented via direct observation during one week at baseline and one week at follow-up at each site. Additionally, during these weeks, child-level snack consumption was measured via direct observation on a paper and pencil form on two non-consecutive days within a one-week period. After training by the project manager, two to four data collectors assessed how much of each program-provided food or drink each consented child consumed at each site. Plates of leftover snack were collected and each snack component served was rated as none, some, most, or all consumed. Digital photography was used to assist in assessing observations made on site. Direct observation measures have been found reliable and valid in a number of school-based studies44–47 and the protocol used in this study showed strong validity when compared with weighed estimates (correlation range 0.92–0.93) as well as high inter-rater reliability (correlation range 0.84–0.92).48 Dietary intake among the 20 sites was observed across multiple weeks before and after the intervention, which ensured all weeks of the school district cycle menu were captured. Matched pairs were observed during the same week.
Observers’ rating of none, some, most, or all of items consumed were converted to corresponding approximate proportions of servings of items consumed: 0%, 33%, 66%, and 100%. Foods and drinks were classified as a fruit or vegetable, 100% juice, foods containing trans fats, or whole grain with a protocol developed by Mozaffarian et. al. for previous snack analyses.29 Nutritional information, including calories, was obtained from the Boston Public Schools Food and Nutrition Services bids lists of specific products, manufacturer’s websites, or from similar product listings in the USDA National Nutrient Database for Standard Reference (Release 20, 2007).49 Beverage calorie estimates included calories from water, milk, and juice. Total calories included all program-provided foods and beverages.
Process measures
Process data were collected at learning collaborative sessions throughout the year. Attendance lists, action plans, and reports of nutrition and physical activity curriculum (e.g. specific activities from Food & Fun; cooking classes) implemented each month were collected at each session to determine the dose and implementation of the afterschool, family, and child intervention components.
Sociodemographic measures
Child age, gender, and race/ethnicity were reported by parents on consent forms at baseline. Race/ethnicity was collected via an open response format and was subsequently categorized as white, Hispanic/Latino, black/African American, Asian, Cape Verdean, black Hispanic, and multiracial.
Statistical analysis
Multivariable regression models were estimated to determine whether the afterschool intervention yielded greater improvements in the nutritional quality of snacks consumed compared with the control condition. Children were required to have at least one day of data at baseline and follow-up to be included in the longitudinal sample; most children had two baseline (83%) and two follow-up (61%) observations. Person-period datasets were constructed,50 to include repeated daily measures of dietary intake within the same children followed over time, and analyses conducted on the person-day unit accounted for the clustering of days within person over time and persons within site. Analysis was conducted with SAS PROC MIXED (SAS Institute, Cary NC).51–53 We used a random intercepts model assuming compound symmetry and using the repeated option to account for nesting of repeated days of observation within children. The model included terms for the period, the intervention sites (=1) (versus control=0), and the period by intervention interaction. Analyses controlled for potentially confounding variables including age in years, gender as a binary variable (0 female, 1 male), indicator variables for six race/ethnicity categories (Black, Hispanic/Latino, Asian, Multiracial, Cape Verdean, and Black Hispanic) with White as the reference, indicator variables for matched pairs, and day of data collection as a binary variable (0 not first day, 1 first day) to control for any effects of order of data collection. To assess the post-hoc hypothesis that snack consumption was influenced by type of foodservice operation, statisticians calculated similar stratified mixed models with SAS PROC MIXED. Due to the small number of children (N=27) in the two sites that purchased snack independent of the school system, stratified results for these sites are not presented. All analyses were conducted using an intention to treat protocol with participants analyzed in their original condition.54
RESULTS
Baseline characteristics
Baseline characteristics of the longitudinal sample are shown in Table 1. The average child was eight years old and half (46% intervention; 52% control) were boys. Most children were identified by their parents as Black/African American (23% intervention; 34% control) or Hispanic/Latino (35% intervention; 29% control). There were no significant baseline differences in age or gender between intervention and control longitudinal samples and no differences in the proportion of Hispanic/Latino, Asian, Cape Verdean, Black Hispanic, or multiracial children; however, intervention sites had fewer White (3.2% vs. 11.3%) and Black (23.4% vs. 33.5%) children than control sites. At baseline, children consumed less than one serving of fruits and vegetables or whole grains each week during afterschool snack; there were no significant differences in consumption by intervention status (Table 1). No sugar-sweetened beverages were served. There were no significant differences in age, gender, or race/ethnicity between baseline and longitudinal samples.
Table 1.
Baseline characteristics and afterschool snack consumption of the longitudinal sample of children in 20 Boston afterschool sites with snack intake data in fall 2010 and spring 2011(N=400)a, b
| Intervention (N=188) |
Control (N=212) |
P value | |
|---|---|---|---|
|
| |||
| Age (years), mean (standard deviation) | 7.80 (1.80) | 7.60 (1.65) | 0.23 |
|
| |||
| Male (%) | 46.2% | 51.9% | 0.27 |
|
| |||
| Race/ethnicity (%)c | |||
| White | 3.2% | 11.3% | <0.01 |
| Black/African American | 23.4% | 33.5% | 0.03 |
| Hispanic/Latino | 35.1% | 28.8% | 0.20 |
| Asian | 5.3% | 2.4% | 0.19 |
| Cape Verdean | 1.1% | 4.3% | 0.67 |
| Black Hispanic | 3.7% | 2.8% | 0.77 |
| Multiracial | 5.9% | 3.8% | 0.36 |
| Missing | 22.3% | 13.2% | |
|
| |||
| Ounces of 100% juice consumed per snack, mean (standard deviation) | 1.63 (2.00) | 1.88 (1.89) | 0.94 |
|
| |||
| Servings of fruits & vegetables consumed per snack, mean (standard deviation) | 0.07 (0.21) | 0.10 (0.22) | 0.28 |
|
| |||
| Servings of foods with trans fats consumed per snack, mean (standard deviation) | 0.19 (0.28) | 0.05 (0.19) | 0.25 |
|
| |||
| Servings of whole grains consumed per snack, mean (standard deviation) | 0.14 (0.26) | 0.19 (0.31) | 0.71 |
|
| |||
| Calories(kcals) consumed per snack, mean (standard deviation) | 157.7 (96.3) | 136.2 (88.5) | 0.52 |
|
| |||
| Beverage calories(kcals) consumed per snack, mean (standard deviation) | 58.2 (52.9) | 46.4 (39.9) | 0.37 |
p values are from t-tests for age and chi square Fisher’s exact test for gender and race/ethnicity.
Baseline consumption means, standard deviations are based on child 2-day means. Baseline p values are derived from person day data: 27 children with one day of data & 161 children with 2 days of data in intervention sites, 40 children with one day of data and 172 children with 2 days of data in control sites; tested for differences in baseline consumption with PROC MIXED to account the clustered sample (within person and within site).
Researchers asked parents to identify race and ethnicity using an open-ended question.
Changes in snack consumption
The OSNAP intervention showed evidence for positive changes to the nutritional quality of snacks consumed (Table 2). After controlling for baseline covariates, children in intervention sites had greater decreases in consumption of 100% juice (−0.61 oz./snack, 95% CI −1.11 – −0.12) and foods with trans fats (−0.12 servings/snack, 95% CI −0.19 – −0.04) and greater increases in whole grain consumption (0.10 servings/snack, 95% CI 0.02–0.18) than controls. However, there was no difference in fruit and vegetable consumption (p=0.55) compared to controls. Average total calories consumed per snack had a greater decrease (−47.8 kcals/snack, 95% CI −68.3 – −27.3) among children who attended intervention sites compared to controls, with most reductions driven by a decrease in beverage calories (−29.0 kcals/snack, 95% CI −40.1 – −17.9).
Table 2.
Estimated intervention impact on dietary consumption from baseline to follow-up among 400 children in intervention (n=10) and control sites (n=10)a
| Baseline | Follow-up | Crude Change | Adjusted Changeb | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Mean | Standard Error | Mean | Standard Error | Beta | Standard Error | 95% Confidence Interval Lower | 95% Confidence Interval Upper | P value | ||
|
| ||||||||||
| Ounces of 100% juice consumed per snack | ||||||||||
| Control | 1.88 | 0.12 | 2.22 | 0.17 | +0.44 | – | – | – | ||
| Intervention | 1.57 | 0.12 | 1.34 | 0.12 | −0.43 | −0.61 | 0.25 | −1.11 | −0.12 | 0.02 |
|
| ||||||||||
| Servings of fruits & vegetables consumed per snack | ||||||||||
| Control | 0.10 | 0.02 | 0.38 | 0.06 | +0.28 | – | – | – | ||
| Intervention | 0.07 | 0.01 | 0.32 | 0.03 | +0.25 | −0.04 | 0.06 | −0.16 | 0.09 | 0.55 |
|
| ||||||||||
| Servings of foods with trans fats consumed per snack | ||||||||||
| Control | 0.05 | 0.01 | 0.09 | 0.02 | +0.04 | – | – | – | ||
| Intervention | 0.20 | 0.02 | 0.12 | 0.02 | −0.08 | −0.12 | 0.04 | −0.19 | −0.04 | 0.002 |
|
| ||||||||||
| Servings of whole grains consumed per snack | ||||||||||
| Control | 0.19 | 0.02 | 0.13 | 0.02 | −0.06 | – | – | – | ||
| Intervention | 0.15 | 0.02 | 0.19 | 0.02 | +0.04 | 0.10 | 0.04 | 0.02 | 0.18 | 0.02 |
|
| ||||||||||
| Calories(kcals) consumed per snack | ||||||||||
| Control | 138.0 | 5.2 | 139.6 | 5.0 | +1.6 | – | – | – | ||
| Intervention | 158.8 | 6.6 | 112.6 | 4.9 | −46.2 | −47.8 | 10.4 | −68.3 | −27.3 | <0.0001 |
|
| ||||||||||
| Beverage calories(kcals) consumed per snack | ||||||||||
| Control | 46.5 | 2.5 | 44.4 | 3.1 | −2.1 | – | – | – | ||
| Intervention | 59.0 | 3.8 | 27.5 | 2.3 | −31.5 | −29.0 | 5.7 | −40.1 | −17.9 | <0.0001 |
Restricted to children with at least 1 day of data at baseline and 1 day of data at follow-up. 738 person days among 212 children in control sites and 639 person days among 188 children in intervention sites.
Adjusted for baseline continuous age, binary gender (0 female, 1 male), dummy variable for 6 race/ethnicity categories, binary indicator for day data collected (1 first day, 0 any other day), and indicator variables for matched pairs. Regression estimates account for the clustered sampling design at the child and site level.
Note: Boldface indicates statistical significance (p<0.05).
Snack consumption changes by foodservice operation
Secondary analyses showed that the estimated effect of the OSNAP intervention differed according to foodservice operation (Table 3). At sites with on-site foodservice, there were significant changes for all consumption outcomes studied (p<0.001), all of which were greater than those found in the main analyses. For instance, children who attended an intervention site with on-site foodservice had greater decreases in 100% juice consumption (−2.52 vs. −0.61 oz./snack) and greater increases in fruits and vegetable consumption (0.31 servings/snack, 95% CI 0.20–0.42) compared to children at control site. In contrast, we observed no change for most of the intake outcomes and a small negative change (p<0.001) in intake of whole grains among children who attended satellite sites that get their snacks pre-prepared and delivered from an outside vendor.
Table 3.
Estimated intervention impact on dietary consumption measured from baseline to follow-up among children in intervention and control sites, stratified by foodservice operation typea,b
| Baseline | Follow-up | Crude Change | Adjusted Modelc | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Mean | Standard Error | Mean | Standard Error | Beta | Standard Error | 95% Confidence Intervals | P value | ||
|
| |||||||||
| On-Site Foodservice (4 intervention, 3 control) N=143 children | |||||||||
|
| |||||||||
| Ounces of 100% juice consumed per snack | |||||||||
| Control | 0.63 | 0.15 | 2.53 | 0.37 | +1.90 | – | |||
| Intervention | 0.89 | 0.15 | 0.37 | 0.09 | −0.52 | −2.52 | 0.35 | −3.22, −1.83 | <0.0001 |
|
| |||||||||
| Servings of fruits/vegetables consumed per snack | |||||||||
| Control | 0.12 | 0.04 | 0.13 | 0.03 | +0.01 | – | |||
| Intervention | 0.05 | 0.02 | 0.38 | 0.03 | +0.33 | 0.31 | 0.06 | 0.20, 0.42 | <0.0001 |
|
| |||||||||
| Servings of trans fats consumed per snack | |||||||||
| Control | 0.14 | 0.05 | 0.15 | 0.05 | +0.01 | – | |||
| Intervention | 0.31 | 0.03 | 0.01 | 0.01 | −0.30 | −0.31 | 0.07 | −0.45, −0.16 | <0.0001 |
|
| |||||||||
| Servings of whole grains consumed per snack | |||||||||
| Control | 0.29 | 0.05 | 0.16 | 0.05 | −0.13 | – | |||
| Intervention | 0.05 | 0.02 | 0.28 | 0.03 | +0.23 | 0.37 | 0.07 | 0.22, 0.51 | <0.0001 |
|
| |||||||||
| Calories(kcals) consumed per snack | |||||||||
| Control | 194.9 | 11.9 | 177.6 | 9.38 | −17.3 | – | |||
| Intervention | 178.2 | 11.1 | 70.4 | 3.99 | −107.8 | −93.2 | 19.4 | −131.4, −55.1 | <0.0001 |
|
| |||||||||
| Beverage calories(kcals) consumed per snack | |||||||||
| Control | 67.4 | 6.62 | 62.4 | 5.81 | −5.0 | – | |||
| Intervention | 65.3 | 6.27 | 5.3 | 1.31 | −60.0 | −56.8 | 10.6 | −77.7, −36.0 | <0.0001 |
|
| |||||||||
| Satellite Foodservice (5 Intervention, 6 control) N=227 children | |||||||||
|
| |||||||||
| Ounces of 100% juice consumed per snack | |||||||||
| Control | 2.28 | 0.14 | 2.23 | 0.19 | −0.05 | – | |||
| Intervention | 2.24 | 0.17 | 2.39 | 0.21 | +0.15 | 0.19 | 0.36 | −0.51, 0.90 | 0.59 |
|
| |||||||||
| Servings of fruits/vegetables consumed per snack | |||||||||
| Control | 0.08 | 0.02 | 0.45 | 0.08 | +0.37 | – | |||
| Intervention | 0.08 | 0.02 | 0.29 | 0.04 | +0.21 | −0.16 | 0.11 | −0.37, 0.06 | 0.15 |
|
| |||||||||
| Servings of trans fats consumed per snack | |||||||||
| Control | 0.02 | 0.01 | 0.08 | 0.02 | +0.06 | – | |||
| Intervention | 0.08 | 0.02 | 0.20 | 0.04 | +0.12 | 0.06 | 0.04 | −0.02, 0.15 | 0.15 |
|
| |||||||||
| Servings of whole grains consumed per snack | |||||||||
| Control | 0.15 | 0.02 | 0.13 | 0.02 | −0.02 | – | |||
| Intervention | 0.28 | 0.04 | 0.13 | 0.03 | −0.15 | −0.15 | 0.06 | −0.26, −0.05 | <0.0001 |
|
| |||||||||
| Calories(kcals) consumed per snack | |||||||||
| Control | 119.7 | 5.62 | 128.9 | 5.87 | +9.2 | – | |||
| Intervention | 138.0 | 7.95 | 147.4 | 8.06 | +9.4 | −1.72 | 13.0 | −27.2, 23.8 | 0.90 |
|
| |||||||||
| Beverage calories(kcals) consumed per snack | |||||||||
| Control | 40.4 | 2.45 | 40.2 | 3.66 | −0.2 | – | |||
| Intervention | 56.6 | 4.67 | 49.1 | 3.80 | −7.5 | −6.18 | 7.09 | −20.1, 7.74 | 0.38 |
Stratified data shown for sites with snacks from on-site or satellite foodservice operation types only.
Restricted to children with at least 1 day of data at baseline and 1 day of data at follow-up. At sites with on-site foodservice, 181 person days among 51 children in control sites and 320 person days among 92 children in intervention sites. At sites with satellite foodservice, 509 person days among 147 children in control sites and 276 person days among 80 children in intervention sites.
Adjusted for baseline continuous age, binary gender (0 female, 1 male), dummy variable for 6 race/ethnicity categories, binary indicator for day data collected (1 first day, 0 any other day). Regression estimates account for the clustered sampling design at the child and site level.
Note: Boldface indicates statistical significance (p<0.05).
Intervention Implementation Process Evaluation
School district foodservice
Fidelity to the foodservice intervention varied by operation type. For sites with on-site foodservice, menus were revised jointly with the Boston Public Schools Food and Nutrition Services staff to improve the nutritional quality of snacks and fit within the department’s budget and then provided to school foodservice directors for product ordering and implementation. Observations at sites with on-site food service indicated significant decreases in 100% juice and foods with trans fats served and increases in whole grain snacks served. For satellite sites, suggested menus were sent to the vendor, but research staff could not meet with them directly. Observations did not detect significant changes in the foods and beverages served at sites with satellite food service. This differential implementation led the research team to conduct post-hoc stratified analyses by foodservice type.
Afterschool learning collaborative
All intervention sites (100%) participated in at least one learning collaborative session; eight sites (80%) participated in all three sessions. One to three staff members (mean 1.5) from each site attended each of these meetings. Thirty-nine staff accumulated an average of 6 training hours (range one to 12). All intervention sites (100%) set goals to promote healthier beverages and five (50%) set goals to promote healthier foods. On action plans, afterschool staff reported a variety of on-site practice changes aligned with the OSNAP goals they set. These included building relationships with cafeteria managers to improve the quality and frequency of fruits and vegetables served, teaching healthy recipes during cooking classes, and ensuring staff model healthy behaviors in front of children.
Child/family educational intervention
Sites reported communicating new health-promoting policies via parent handbooks, student contracts, letters to families, and staff meetings. Eight intervention and three control sites reported using the Food and Fun After School curriculum. On average, these sites delivered five activities throughout the school year. Units on promoting fruits and vegetables, limiting sugary drinks, and choosing healthy fats were most commonly implemented. Five on-site foodservice sites and five satellite sites used Food and Fun nutrition lessons.
DISCUSSION
This study indicates that the OSNAP intervention yielded improvements in the nutritional quality of foods and beverages consumed by children during afterschool snack. After a multicomponent intervention, which worked with a school foodservice department to implement menu changes and engaged afterschool directors and staff in education, skill building, and action planning around specific health objectives, children at intervention sites decreased their juice and trans fat food consumption, while increasing whole grain consumption relative to controls. Children in intervention sites also consumed fewer calories at each snack compared to controls, driven primarily by a decrease in beverage calories. This evidence for healthier snack consumption of procured foods and beverages can be coupled with previous results showing a substantial increase in water consumption55, demonstrating the overall positive impact of the OSNAP intervention on children’s dietary intake. Previous analyses also show that participation in OSNAP increased vigorous physical activity,31 indicating improved energy balance among children.
These results indicate the promise of the afterschool setting for promoting dietary change among children. While some studies have shown no intervention effects on snacks served afterschool,23,27 these findings align with two interventions, which also included activities focused on targeted, low cost changes to snacks served, that have shown improvements in the foods and beverages served in out-of-school settings.29,30 Calorie reductions from 159 to 113 calories consumed per snack align with the Institute of Medicine meal pattern recommendation of 126 calories at snack for five to 13 year olds.56 The comprehensive multilevel intervention, which included partnership between a school foodservice department and public health experts to change menus and work with site staff to influence afterschool practices, is an approach communities should consider to make a successful impact on children’s dietary intake.
The difference in intervention impact between sites with on-site foodservice and satellite sites points to the influence that afterschool inner setting57 (e.g. organizational context, resources) can have on the success of nutrition interventions. Sites with the local control to implement menu changes, adequate refrigeration facilities, and staff and equipment to assemble snacks saw improvements across all dietary outcomes, including fruits and vegetables. These are promising findings, as 92% of U.S. school districts have these site-based kitchens.14 In contrast, children who attended sites with satellite foodservice (present in 17% of U.S. school districts)14 did not have improvements in dietary outcomes. At these sites, control was constrained by communication with the outside vendor and contracts set ahead of the intervention period. Foodservice operation type has been noted as influential to the delivery of school-based nutrition policies and interventions58,59 and related foodservice barriers, such as limited delivery and storage, have been found to impact a similar afterschool nutrition intervention.60 Unfortunately, the research team did not anticipate the influence of foodservice delivery type in the design of the intervention; however, the findings from the secondary analysis allow this study to highlight the importance of addressing the complex logistics of foodservice operations for long-term changes.61
This study has a number of notable strengths. First, data on changes in snack consumption were collected as part of a group randomized trial and measured with a validated direct observation method.48 By following 400 children across four data collection points, two before the intervention and two after, this study also had a large enough longitudinal sample to detect behavior change. Engaging community partners in the design of the intervention ensured that intervention activities were acceptable to afterschool staff and would be feasible to translate into real world implementation. Taking a systems approach to changing the foods and beverages the school district served and leveraging on-site practices and policies to promote healthy eating, successfully influenced child consumption. The study design had benefits for researchers and foodservice administrators: the randomized design with control group ensured the ability to detect consumption changes from the intervention with more certainty than if no control group had been used. The control group was later offered the intervention after the study was complete, and the foodservice department was thus able to test the delivery of new, healthier items on a small scale before rolling out menu changes across the entire district the following year.
Because randomization occurred at the site level there is a possibility of residual confounding at the individual level; however, gender, age, race/ethnicity and baseline intake were included in all analyses of intervention effects. Because only half of respondents who attended sites agreed to participate in data collection and the retention rate was 67%, it is not certain that these results generalize to the population of children attending these sites; however, the practice and policy changes in this intervention are not dependent on individual children or parents and we would expect similar results on the average child. This low response rate and loss to follow up can be explained, in part, by the variable attendance and high turnover in afterschool sites. Results may not generalize beyond the study context to sites that do not use a foodservice program to procure afterschool snacks or are situated in different geographic areas. While the study experienced some loss to follow-up, a comparison of baseline and longitudinal samples indicates internal validity was likely not compromised by differential loss to follow-up. Some dietary estimates were based on one day of consumption data, which could impact the precision of our estimates; however, measures in the study had strong criterion validity. Finally, sites were not matched exactly on foodservice type and foodservice changes were not implemented as planned at satellite foodservice sites.
CONCLUSIONS
The study results demonstrate that an afterschool nutrition intervention, particularly when based in sites that engage in snack menu changes with an on-site school foodservice, can successfully improve dietary intake among the children they serve. The intervention worked with existing staff to develop practices and policies for change that can be sustained. This study is the first to our knowledge to identify the potential importance of this contextual implementation consideration in the out-of-school time setting. In the future, researchers and practitioners should consider how flexibility of ordering and menu planning (e.g. serving fresh produce early in the week, the ability to change menus mid-year) and writing health standards into vendor contracts (e.g. requiring daily fruit and vegetable servings, limiting juice size) impact the nutritional quality of afterschool snacks served and consumed.62
OSNAP is unique in its strong focus on creating change in a real world afterschool setting that can be implemented and disseminated broadly. OSNAP intervention materials are available for afterschool sites to adopt OSNAP on their own. Additionally, health departments and YMCA Associations have begun to implement OSNAP via community partnerships. Online and in-person training models for dissemination are currently being tested in hopes that similar changes will be taken up among the thousands of afterschool sites that serve children each day.
Research Snapshot.
Research Question
What is the impact of an afterschool intervention on children’s snack consumption?
Key Findings
The group randomized control trial found that children in intervention sites had significantly greater decreases in consumption of juice (−0.61 ounces/snack), beverage calories (−29.1 calories/snack), foods with trans fats (−0.12 servings/snack), total calories (−47.7 calories/snack) and greater increases in consumption of whole grains (0.10 servings/snack) compared to controls.
Acknowledgments
We thank our research assistants for their help collecting data and the enthusiastic afterschool staff for their willingness to open their doors to this research. We also remember and thank Arthur Sobol and James Ware from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102) for reviewing SAS programs. This work is solely the responsibility of the authors and does not represent the offıcial views of the CDC, Harvard Catalyst, or the National Institutes of Health. Trial Registration: NCT01396473,Clinicaltrials.gov, January 27, 2011.
Funding statement
The work of Lee, Giles, Cradock, Kenny, Thayer, and Gortmaker were supported by Cooperative Agreement 1U48DP001946 (including NOPPREN) from the CDC Prevention Research Centers Program and the Robert Wood Johnson Foundation (No. 66284). Lee and Gortmaker were also supported by the Donald and Sue Pritzker Nutrition and Fitness Initiative and NIH 5R21CA201567-02. Okechukwu was funded by grant NIH 3U01AG027669-S1 and Emmons was funded by NIH K05CA124415.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions:
RML and SLG are responsible for formulating the research question(s), designing the study, carrying it out, analyzing and interpreting the data, and drafting the article. CMG, ALC, ELK, and JT are responsible for formulating research questions, designing the study, carrying it out, and drafting the article. KME and CO are responsible for interpreting data and drafting the article.
Conflict of Interest Disclosures
Rebekka M. Lee: no competing financial interests exist.
Catherine M. Giles: no competing financial interests exist.
Angie L. Cradock: no competing financial interests exist.
Karen M. Emmons: no competing financial interests exist.
Cassandra Okechukwu: no competing financial interests exist.
Erica L. Kenney: no competing financial interests exist.
J Thayer: no competing financial interests exist.
Steven L. Gortmaker: no competing financial interests exist.
References
- 1.Gordon-Larsen P, Adair LS, Popkin BM. The Relationship of Ethnicity, Socioeconomic Factors, and Overweight in U.S. Adolescents. Obes Res. 2003;11(1):121–129. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- 2.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286(22):2845–2848. doi: 10.1001/jama.286.22.2845. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang YC, Gortmaker SL, Sobol AM, Kuntz KM. Estimating the Energy Gap Among US Children: A Counterfactual Approach. J Pediatr. 2006;118(6):e1721–e1733. doi: 10.1542/peds.2006-0682. [DOI] [PubMed] [Google Scholar]
- 5.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nut. 2006;84(2):274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebbeling CB, Feldman HA, Chomitz VR, et al. A Randomized Trial of Sugar-Sweetened Beverages and Adolescent Body Weight. N Engl J Med. 2012;367(15):1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A Trial of Sugar-free or Sugar-Sweetened Beverages and Body Weight in Children. N Engl J Med. 2012;367(15):1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 8.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for Prevention of Childhood Obesity. J Pediatr. 2007;120(Supplement 4):S229–S253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. (8th) 2015 Dec; http://health.gov/dietaryguidelines/2015/guidelines/. Accessed May 25, 2017.
- 10.U.S. Department of Health and Human Services. The Surgeon General’s Vision for a Healthy and Fit Nation. 2010 http://www.surgeongeneral.gov/library/obesityvision/obesityvision2010.pdf. Accessed August 23, 2017.
- 11.White House Task Force on Childhood Obesity. Solving the Problem of Childhood Obesity Within a Generation White House Task Force on Childhood Obesity Report to the President. 2010 doi: 10.1089/bfm.2010.9980. [DOI] [PubMed] [Google Scholar]
- 12.Beets MW, Weaver RG, Tilley F, et al. Salty or Sweet? Nutritional Quality, Consumption, and Cost of Snacks Served in Afterschool Programs. J Sch Health. 2015;85(2):118–124. doi: 10.1111/josh.12224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afterschool Alliance. America After 3PM: Afterschool Programs in Demand. Washington, D.C.: 2014. [Google Scholar]
- 14.School Nutrition Association. School Nutrition Operations Report 2011: The State of School Nutrition. 2011 [Google Scholar]
- 15.Carver PR, Iruka IU, Chapman C. National Household Education Surveys Program of 2005: After-School Programs and Activities. Washington, D.C.: 2006. [Google Scholar]
- 16.Popkin BM, Duffey KJ. Does hunger and satiety drive eating anymore? Increasing eating occasions and decreasing time between eating occasions in the United States. Am J Clin Nutr. 2010;91(5):1342–1347. doi: 10.3945/ajcn.2009.28962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piernas C, Popkin BM. Trends In Snacking Among U.S. Children. Health Aff. 2010;29(3):398–404. doi: 10.1377/hlthaff.2009.0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National AfterSchool Association. Healthy Eating and Physical Activity Standards. 2011 https://naaweb.org/images/NAA_HEPA_Standards_new_look_2015.pdf. Accessed April 13, 2018.
- 19.Kenney EL, Austin SB, Cradock AL, et al. Identifying sources of children’s consumption of junk food in Boston after-school programs, April–May 2011. Prev Chronic Dis. 2014;11:E205. doi: 10.5888/pcd11.140301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melnyk BM, Small L, Morrison-Beedy D, et al. The COPE Healthy Lifestyles TEEN Program: Feasibility, Preliminary Efficacy, & Lessons Learned from an After School Group Intervention with Overweight Adolescents. J Pediatr Health Care. 2007;21(5):315–322. doi: 10.1016/j.pedhc.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Story M, Sherwood NE, Himes JH, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn & Dis. 2003;13(1 Suppl 1):S54–S64. [PubMed] [Google Scholar]
- 22.Freedman MR, Nickell A. Impact of After-school Nutrition Workshops in a Public Library Setting. J Nut Ed Behav. 2010;42(3):192–196. doi: 10.1016/j.jneb.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Kelder S, Hoelscher DM, Barroso CS, Walker JL, Cribb P, Hu S. The CATCH Kids Club: a pilot after-school study for improving elementary students’ nutrition and physical activity. Public Health Nutr. 2005;8(02):133–140. doi: 10.1079/phn2004678. [DOI] [PubMed] [Google Scholar]
- 24.Gutin B, Yin Z, Johnson M, Barbeau P. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: The Medical College of Georgia Fitkid Project. Int J Pediatr Obes. 2008;3(s1):3–9. doi: 10.1080/17477160801896457. [DOI] [PubMed] [Google Scholar]
- 25.Yin Z, Moore JB, Johnson MH, Vernon MM, Gutin B. The impact of a 3-year after-school obesity prevention program in elementary school children. Child Obes. 2012;8(1):60–70. doi: 10.1089/chi.2011.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Economos CD, Hyatt RR, Goldberg JP, et al. A Community Intervention Reduces BMI z-score in Children: Shape Up Somerville First Year Results. Obesity (Silver Springs) 2007;15(5):1325–1336. doi: 10.1038/oby.2007.155. [DOI] [PubMed] [Google Scholar]
- 27.Dzewaltowski D, Rosenkranz R, Geller K, et al. HOP’N after-school project: an obesity prevention randomized controlled trial. Int J Behav Nutr Phys Act. 2010;7(1):90. doi: 10.1186/1479-5868-7-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beets MW, Weaver RG, Turner-McGrievy G, et al. Making Healthy Eating Policy Practice: A Group Randomized Controlled Trial on Changes in Snack Quality, Costs, and Consumption in After-School Programs. Am J Health Promot. 2016;30(7):521–531. doi: 10.4278/ajhp.141001-QUAN-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mozaffarian RS, Wiecha JL, Roth BA, Nelson TF, Lee RM, Gortmaker SL. Impact of an Organizational Intervention Designed to Improve Snack and Beverage Quality in YMCA After-School Programs. Am J Public Health. 2010;100(5):925–932. doi: 10.2105/AJPH.2008.158907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beets MW, Tilley F, Weaver RG, Turner-McGrievy G, Moore JB, Webster C. From Policy to Practice: Addressing Snack Quality, Consumption, and Price in After-School Programs. J Nutr Ed Behav. 2014;46(5):384–389. doi: 10.1016/j.jneb.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cradock AL, Barrett JL, Giles CM, et al. Promoting physical activity with the out of school nutrition and physical activity (osnap) initiative: A cluster-randomized controlled trial. JAMA Pediatr. 2016;170(2):155–162. doi: 10.1001/jamapediatrics.2015.3406. [DOI] [PubMed] [Google Scholar]
- 32.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 33.Mozaffarian RS, Andry A, Lee RM, Wiecha JL, Gortmaker SL. Price and healthfulness of snacks in 32 YMCA after-school programs in 4 US metropolitan areas, 2006–2008. Prev Chronic Dis. 2012;9:E38. doi: 10.5888/pcd9.110097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Afterschool snack sample menu 1 (National School Lunch Program) The Out-of-School Nutrition and Physical Activity Initiative by the Harvard Prevention Research Center at the Harvard TH Chan School of Public Health website. http://osnap.org/wp-content/uploads/2013/02/Sample-Snack-Menu.pdf. Accessed March 23, 2018.
- 35.United States Department of Agriculture. National School Lunch Program website. https://www.fns.usda.gov/nslp/national-school-lunch-program-nslp. Accessed April 13, 2018.
- 36.Kilo CM. A framework for collaborative improvement: lessons from the Institute for Healthcare Improvement’s Breakthrough Series. Qual Manag Health Care. 1998;6(4):1–13. doi: 10.1097/00019514-199806040-00001. [DOI] [PubMed] [Google Scholar]
- 37.Bandura A. Social Foundations of Thought and Action. Inglewood Cliffs, New Jersey: Prentice-Hall; 1986. [Google Scholar]
- 38.The Out-of-School Nutrition and Physical Activity Initiative by the Harvard Prevention Research Center at the Harvard TH Chan School of Public Health website. http://osnap.org/. Accessed March 23, 2018.
- 39.Policy language: beverages & snacks. The Out-of-School Nutrition and Physical Activity Initiative by the Harvard Prevention Research Center at the Harvard TH Chan School of Public Health website. http://osnap.org/resources/policy-writing-guide/policy-language-snacks/. Accessed March 23, 2018.
- 40.Tips & information: whole grains. The Out-of-School Nutrition and Physical Activity Initiative by the Harvard Prevention Research Center at the Harvard TH Chan School of Public Health website. http://osnap.org/wp-content/themes/osnap.1.0/tip-sheets/wholegrains.pdf. Accessed March 23, 2018.
- 41.Fast map: improving fruit & vengetable consumption. The Out-of-School Nutrition and Physical Activity Initiative by the Harvard Prevention Research Center at the Harvard TH Chan School of Public Health website. http://osnap.org/wp-content/themes/osnap.1.0/fast-maps/fruitveg.pdf. Accessed March 23, 2018.
- 42.Working with school food service: working toward healthy snacks. The Out-of-School Nutrition and Physical Activity Initiative by the Harvard Prevention Research Center at the Harvard TH Chan School of Public Health website. http://osnap.org/wp-content/uploads/2013/06/Working-with-Food-Service.pdf. Accessed March 23, 2018.
- 43.Food & Fun Afterschool Curriculum. Food & Fun afterschool website. http://www.foodandfun.org/?p=learn/staff/info&subject=About. Accessed March 23, 2018.
- 44.Swanson M. Digital photography as a tool to measure school cafeteria consumption. J Sch Health. 2008;78(8):432–437. doi: 10.1111/j.1746-1561.2008.00326.x. [DOI] [PubMed] [Google Scholar]
- 45.Williams CL, Bollella MC, Strobino BA, et al. Healthy-Start: Outcome of an Intervention to Promote a Heart Healthy Diet in Preschool Children. J Am Coll Nutr. 2002;21(1):62–71. doi: 10.1080/07315724.2002.10719195. [DOI] [PubMed] [Google Scholar]
- 46.Williamson DA, Allen HR, Martin PD, Alfonso AJ, Gerald B, Hunt A. Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Nutr Diet. 2003;103(9):1139–1145. doi: 10.1016/s0002-8223(03)00974-x. [DOI] [PubMed] [Google Scholar]
- 47.Williamson DA, Copeland AL, Anton SD, et al. Wise Mind Project: A School-based Environmental Approach for Preventing Weight Gain in Children. Obesity (Silver Springs) 2007;15(4):906–917. doi: 10.1038/oby.2007.597. [DOI] [PubMed] [Google Scholar]
- 48.Kenney EL, Davison KK, Austin SB, et al. Validity and Reliability of a Simple, Low-Cost Measure to Quantify Children’s Dietary Intake in Afterschool Settings. J Acad Nutr Diet. 2015;115(3):426–432. doi: 10.1016/j.jand.2014.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.U.S. Department of Agriculture ARS. USDA National Nutrient Database for Standard Reference, Release 20. 2007 [Google Scholar]
- 50.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- 51.Fitzmaurice GM, Laird NM, Ware JH. Applied Longitudinal Analysis. 2nd. Hoboken NJ: John Wiley and Sons; 2011. [Google Scholar]
- 52.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;24:323–355. [Google Scholar]
- 53.The SAS system for Windows. Cary, NC: SAS Institute; 2013. (Release 9.4). [Google Scholar]
- 54.Pocock SJ. Clinical Trials: A practical approach. New York: Wiley; 1993. [Google Scholar]
- 55.Lee RM, Okechukwu C, Emmons KM, Gortmaker SL. Impact of implementation factors on children’s water consumption in the Out-of-School Nutrition and Physical Activity group-randomized trial. New Dir Youth Devent. 2014;2014(143):79–101. doi: 10.1002/yd.20105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.IOM (Institute of Medicine) Child and Adult Care Food Program: Dietary Guidence for All. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 57.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4 doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Osganian SK, Ebzery MK, Montgomery DH, et al. Changes in the Nutrient Content of School Lunches: Results from the CATCH Eat Smart Food Service Intervention. Preve Med. 1996;25(4):400–412. doi: 10.1006/pmed.1996.0072. [DOI] [PubMed] [Google Scholar]
- 59.Brown KM, Akintobi TH, Pitt S, et al. California School Board Members’ Perceptions of Factors Influencing School Nutrition Policy. J Sch Health. 2004;74(2):52–58. doi: 10.1111/j.1746-1561.2004.tb04199.x. [DOI] [PubMed] [Google Scholar]
- 60.Beets MW, Weaver RG, Turner-McGrievy G, et al. Two-Year Healthy Eating Outcomes: An RCT in Afterschool Programs. American Journal of Preventive Medicine. doi: 10.1016/j.amepre.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nanney MS, Olaleye TM, Wang Q. Incorporating a Healthy Reimbursable Snack in an Afterschool Homework Program for Middle School Students: A Case Study. Health Education & Behavior. 2012;39(2):127–130. doi: 10.1177/1090198111404066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nanney MS, Glatt C. Exploring implementation of the 2010 Institute of Medicine’s Child and Adult Food Care Program recommendations for after-school snacks. Public Health Nutr. 2013;16(06):1140–1146. doi: 10.1017/S1368980011002722. [DOI] [PMC free article] [PubMed] [Google Scholar]


