Abstract
Background
Research comparing sex differences in the effects of antipsychotic medications on acute ischemic heart disease (IHD) is limited and the findings ambiguous. This study aimed to investigate these associations within a primary care setting.
Methods
Hong Kong public general outpatient electronic records of patients aged 45+ during 2007–2010 were extracted, with the last consultation date as the baseline for a 4-year follow-up period to observe acute IHD hospitalizations (2011–2014). Antipsychotic use was defined as any prescription over the previous 12 months from a list of 16 antipsychotics, while acute IHD was defined by ICD-9: 410.00–411.89. Both sex-specific and sex-combined (both sexes) mixed-effects Cox models (random intercept across 74 clinics) were implemented to examine the association and test the interaction between antipsychotics and sex.
Results
Among 1,043,236 included patients, 17,780 (1.7%) were prescribed antipsychotics, and 8342 (0.8%) developed IHD. In sex-specific analyses, antipsychotic prescription was associated with a 32% increased hazard rate of acute IHD among women (95% CI 1.05–1.67) but not among men. A likelihood ratio test comparing sex-combined models with and without the interaction between antipsychotic use and sex suggested significant interaction (χ2 = 4.72, P = 0.030). The association between antipsychotic use and IHD among women attenuated and became non-significant when haloperidol was omitted from the operationalization of antipsychotic use (HR = 1.23, 95% CI 0.95–1.60).
Conclusion
Our results suggest that antipsychotic prescription is moderately associated with an increased risk of acute IHD among women in primary care and this relationship may be explained by specific antipsychotics. Further research should observe and capture the potential intermediary mechanisms and the dose-response relationship of this association to provide more rigorous evidence to establish causality and inform clinical practices.
Keywords: Cardiovascular diseases, Community psychiatry, Myocardial infarction, Primary health care, Psychotic disorders, Schizophrenia
Background
Antipsychotic medications commonly prescribed for patients with a variety of mental disorders such as schizophrenia, bipolar disorder, and dementia are generally believed to entail a heightened risk of acute ischemic heart disease (IHD) [1]. However, meta-analyses have reported conflicting results on this association [2–5]. For instance, in a review of 399,868 participants from nine observational studies [2], antipsychotic medications were found to be associated with 121%-elevated odds of myocardial infarction, whereas in another meta-analysis [3], no significant association was observed. These mixed findings may be due to a heterogeneity across study populations [4], suggesting that this association may only be present in populations with certain characteristics.
Several intermediary mechanisms have been proposed in support of the association, for example, the higher prevalence of metabolic abnormalities among patients on antipsychotic medications [6] and the blockade of specific neurotransmitter receptors which has been identified to be related to IHD risks [7]. Although it is difficult to observe and incorporate all potential mediators to examine the relative importance of the mechanisms, the comparison of the presence or absence, as well as the varying strength, of this association between specific subpopulations or sociodemographic strata may inform the inquiry about the potential underlying mechanisms considerably. This is because some mechanisms may operate more strongly in certain subpopulations, indicated by stronger statistical associations.
Sex difference in the association between antipsychotics and IHD, in particular, has been little examined in previous research, despite the growing evidence of potentially different physiological mechanisms in the development of cardiovascular diseases [8] and different prevalence of tobacco [9] and alcohol use [10] as well as sedentary lifestyle [11] between men and women. There is also a lack of large-scale studies in primary care populations, whose needs typically arouse much less medical attention because of the seemingly milder risks compared with inpatients who have already experienced an acute episode [12].
In this study, we used a large multicenter public primary care database of over one million middle-aged and older patients in Hong Kong to examine the association between antipsychotics and acute IHD incidence and tested for the potential sex difference of this association.
Methods
Study design and sample selection
We adopted a retrospective cohort design for this investigation which was under a broader project on health care for older people commissioned by the Hong Kong Government, and were allowed access to the clinical records of patients aged 45 or above from the public health care sector. The Hospital Authority (HA), a major provider of public outpatient services and the sole provider of public inpatient services in Hong Kong, provided data for the analysis. We examined the records of all patients aged 45 or more who visited any of the 74 general outpatient clinics run by the HA during January 1, 2007, to December 31, 2010, for data extraction to form the closed cohort.
We took the last visit by these patients during the period as the baseline and retrieved the corresponding outpatient clinical records over the 12 months prior to the baseline (including baseline visit records). We excluded patients with an existing diagnosis of IHD (International Classification of Primary Care (ICPC) codes K74, K75, and K76) or any previous admission to public hospitals to enable the results to better inform primary care practice for those who had not presented with recent acute health problems or with an existing IHD diagnosis, who typically received less medical attention.
The patients were then followed up until they were admitted to any public hospitals through the Accident and Emergency Unit due to IHD or any other reasons, or until 4 years after the baseline (January 2011–December 2014).
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Survey and Behavioral Ethics Committee of the Chinese University of Hong Kong (dated 25 August 2015, Project Code: Elderly Care – CUHK). As only secondary analysis of the anonymized unidentifiable patient records was involved, no written consent was required.
Study outcome—time to acute hospitalization due to IHD
The time duration from the baseline to the first hospital admission through the Accident and Emergency Unit with a primary diagnosis of IHD (defined by International Classification of Diseases, Ninth Revision (ICD-9)) was used as the outcome of the analysis. The ICD-9 codes used to identify acute IHD ranged from 410.00 to 411.89 (down to two decimal places when applicable).
Exposure—antipsychotic use
Antipsychotic use was the main exposure in the analysis. It was defined by any prescriptions of the following 16 antipsychotic medications (generic drug name) over the 12 months prior to the baseline: amisulpride, aripiprazole, chlorpromazine, clozapine, fluphenazine, haloperidol, olanzapine, paliperidone, perphenazine, quetiapine, risperidone, sulpiride, thioridazine, thiothixene, trifluoperazine, and ziprasidone.
Effect modifier—biological sex
Biological sex (women as referent) was tested as an effect modifier of the association between antipsychotics on time to acute IHD hospitalization.
Multivariable adjustment
We included other baseline variables (according to the records over the 12 months prior to the baseline) to adjust for their potential confounding effects. First, baseline morbidities diagnosed by primary care physicians including schizophrenia (ICPC code P72), dementia (ICPC code P70), depression (ICPC codes P03, P76, and P77), bipolar disorder (ICPC code P73), diabetes (ICPC codes T89 and T90), hypertension (ICPC codes K86 and K87), atrial fibrillation (ICPC code K78), stroke (ICPC codes K89 and K90), and lipid disorder (ICPC code T93) were adopted. Second, we further included tobacco abuse (ICPC code P17) to proxy the unobserved smoking status. Third, we included the prescription of any antidepressants (amitriptyline, clomipramine, citalopram, dosulepin, doxepin, fluoxetine, imipramine, lofepramine, mirtazapine, moclobemide, nortriptyline, paroxetine, phenelzine, reboxetine, sertraline, tranylcypromine, trazodone, venlafaxine) over the past year as antidepressants have been shown to be related to IHD and are sometimes used in combination with antipsychotics [13, 14]. Fourth, we included the prescription of statin (atorvastatin, cerivastatin, fluvastatin, lovastatin, pravastatin, pitavastatin, simvastatin, rosuvastatin) as a dichotomized variable (prescribed or not prescribed over the 12 months) and specified an interaction between lipid disorder and statin prescription.
Statistical analysis
We ran a mixed-effects Cox model (with random intercept across the 74 general outpatient clinics) to examine the hazard ratios of acute hospitalization due to IHD between those prescribed antipsychotics and those who were not, with potential confounders adjusted (both with sex-stratified and with sex-combined samples). Based on this model, we further constructed an extended model in which the interaction between antipsychotics and sex was specified. Likelihood ratio test was used to test for this interaction.
We conducted multiple sets of sensitivity analyses to test for the robustness of the results. First, we adopted the leave-one-out approach to replicate the main analysis multiple times in each of which we removed one of the antipsychotic medications in the definition of antipsychotic use. Likewise, we used a similar approach to replicate the analysis repeatedly with patients admitted for each subtype of acute IHD (ICD-9: 410.00–411.89) excluded. These replications could reveal the potential changes in the results with alternative operationalization of the outcome and main exposure, respectively. Motivated by the results of the leave-one-out analysis on specific antipsychotic medications, we further replicated the analysis with antipsychotic use replaced by only haloperidol prescription as main exposure, with the prescription of other antipsychotics adjusted, for a comparison. We then replicated the analysis with the sample restricted to only those prescribed antipsychotics and examined the association of each antipsychotic with acute IHD. Second, we varied the threshold of the number of antipsychotic medications for the operationalization of antipsychotic use from one to eight for another set of replicated analyses. Third, we replicated the main analysis on a larger sample selected without applying the exclusion criteria of previous hospital admission and IHD diagnosis to examine the impact of those exclusion criteria on the results. Fourth, the main analysis was replicated without including the preexisting diagnoses of diabetes, hypertension, and lipid disorder (and statin prescription) which may potentially act as the intermediary mechanisms between antipsychotic use and IHD.
The mixed-effects Cox model was implemented using the “coxme” package [15] in R, version 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria). Two patients with incomplete data were excluded from the analysis.
Results
Descriptive results
During January 1, 2007, to December 31, 2010, a total of 15,054,785 general outpatient clinic visits by 1,312,229 patients aged 45 or above were recorded. We removed 255,475 patients with hospital admission history over the past 12 months, then further excluded 13,518 having the diagnoses of IHD. Eventually, 1,043,236 primary care patients were included for analysis. The mean (standard deviation) follow-up period was 1216.7 (454.7) days. Figure 1 shows the procedures of data selection for this study.
Fig. 1.
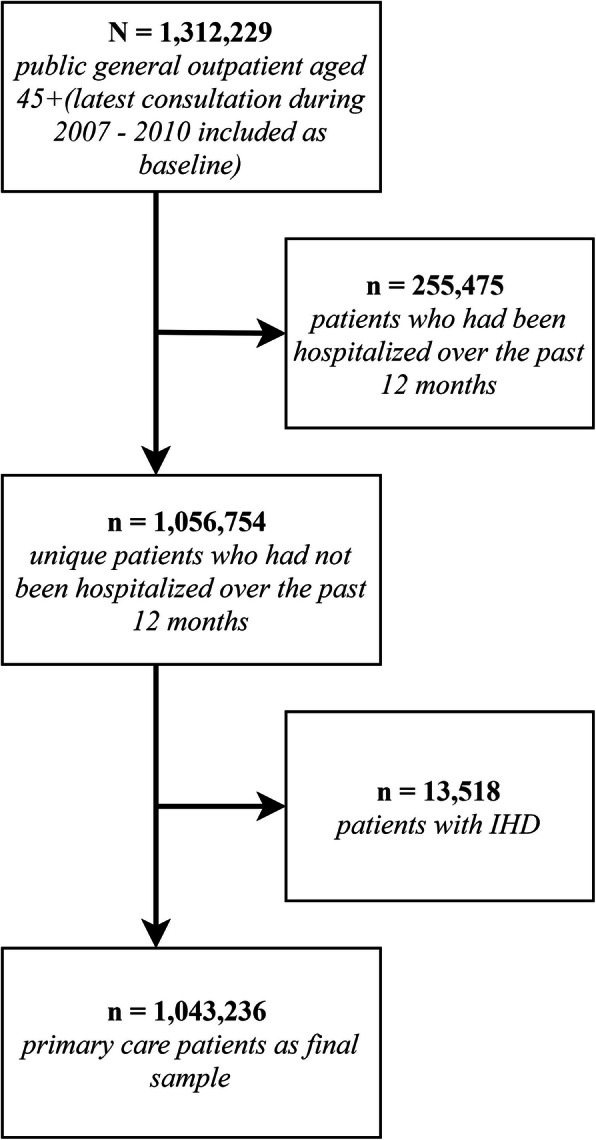
Flow chart showing the procedures of the sample selection for this study
Table 1 shows the descriptive statistics of the cohort. In total, there were 17,780 patients being prescribed antipsychotics and 0.8% of them were admitted due to IHD through the Accident and Emergency Unit within 4 years, compared similarly with those without antipsychotic prescriptions without any multivariable adjustment. Sex ratios between the two groups were similar, with around 40% men. There was a higher prevalence of diabetes (17.8% versus 14.4%, P < 0.001) and stroke (2.2% versus 1.2%, P < 0.001) but a lower prevalence of hypertension (31.9% versus 36.9%, P < 0.001) among those prescribed antipsychotics than those who were not. Both lipid disorder prevalence (7.2% versus 9.9%, P < 0.001) and statin prescription rate (6.6% versus 7.6%, P < 0.001) were lower among those on antipsychotics. A notably higher rate of antidepressant prescription was observed among those on antipsychotics too (27.6% versus 2.8%, P < 0.001).
Table 1.
Descriptive statistics of the sample (N = 1,043,236)
| Without antipsychotic prescriptions | With antipsychotic prescriptions | P value* | |
|---|---|---|---|
| n | 1,025,456 | 17,780 | |
| Sex (%) | < 0.001 | ||
| Men | 436,623 (42.6) | 7110 (40.0) | |
| Women | 588,833 (57.4) | 10,670 (60.0) | |
| Age (%) | < 0.001 | ||
| 45–54 | 341,743 (33.3) | 6614 (37.2) | |
| 55–64 | 306,180 (29.9) | 5037 (28.3) | |
| 65–74 | 200,401 (19.5) | 2421 (13.6) | |
| 75–84 | 138,672 (13.5) | 2354 (13.2) | |
| 85+ | 38,460 (3.8) | 1354 (7.6) | |
| International Classification of Primary Care Diagnoses (%) | |||
| Schizophrenia | 69 (0.0) | 156 (0.9) | < 0.001 |
| Depression | 1845 (0.2) | 36 (0.2) | 0.539 |
| Bipolar disorder | 5 (0.0) | 3 (0.0) | < 0.001 |
| Dementia | 1338 (0.1) | 326 (1.8) | < 0.001 |
| Tobacco abuse | 6209 (0.6) | 116 (0.7) | 0.453 |
| Diabetes | 147,949 (14.4) | 3160 (17.8) | < 0.001 |
| Hypertension | 378,476 (36.9) | 5663 (31.9) | < 0.001 |
| Atrial fibrillation | 3738 (0.4) | 78 (0.4) | 0.118 |
| Stroke | 12,388 (1.2) | 384 (2.2) | < 0.001 |
| Lipid disorder | 101,192 (9.9) | 1285 (7.2) | < 0.001 |
| Statin prescription (%) | 77,410 (7.6) | 1169 (6.6) | < 0.001 |
| Antidepressant prescription (%) | 29,166 (2.8) | 4905 (27.6) | < 0.001 |
| Acute ischemic heart disease hospitalization within 4 years (%) | 0.691 | ||
| Not hospitalized | 1,017,251 (99.2) | 17,643 (99.2) | |
| Hospitalized | 8205 (0.8) | 137 (0.8) | |
*P value of chi-square tests/Fisher’s exact tests for the difference between patients on antipsychotics and those who were not
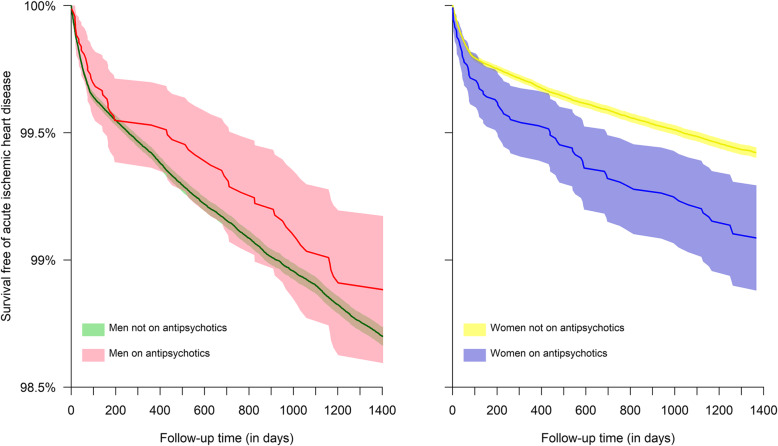
Figure 2 shows the acute IHD-free survival patterns across follow-up time by sex and by the prescription of antipsychotics. The impact of antipsychotics on the patterns differed drastically by sex. Antipsychotics were associated with a significantly worse survival pattern among women, whereas men on antipsychotics had a similar survival pattern compared with those not prescribed antipsychotics.
Fig. 2.
Patterns of survival free of acute hospitalization due to ischemic heart disease by sex and prescription of antipsychotics. Shaded area represents 95% confidence intervals
Mixed-effects Cox model
Table 2 shows the results of the mixed-effects Cox regression analysis without specifying the interaction between antipsychotic use and sex. When men and women were separately analyzed (sex-specific models: first and second columns of Table 2), antipsychotics were associated with an increased hazard rate of acute IHD among women (HR = 1.32, 95% CI 1.05–1.67) but not among men. When both men and women were included in the analysis (sex-combined model: third column of Table 2), antipsychotics were associated with acute IHD with a hazard ratio of 1.19 (95% CI 1.00–1.41).
Table 2.
Adjusted hazard ratios [95% confidence intervals] of acute ischemic heart disease
| Sex-specific models | Sex-combined model | ||
|---|---|---|---|
| Men only | Women only | Men + women | |
| Antipsychotic prescription | 0.95 [0.73, 1.23] | 1.32 [1.05, 1.67]* | 1.19 [1.00, 1.41]* |
| Men (women as referent) | 2.19 [2.10, 2.29]*** | ||
| Age (in 10 years) | 1.55 [1.51, 1.59]*** | 2.37 [2.30, 2.44]*** | 1.86 [0.55, 6.32]** |
| Antidepressant prescription | 1.14 [0.94, 1.39] | 1.15 [0.96, 1.37] | 1.16 [1.01, 1.32]* |
| International Classification of Primary Care Diagnoses as baselinea | |||
| Dementia | 0.99 [0.47, 2.08] | 0.54 [0.30, 0.99]* | 0.78 [0.49, 1.23] |
| Tobacco abuse | 1.55 [1.28, 1.88]*** | 3.16 [1.83, 5.46]*** | 1.68 [1.40, 2.01]*** |
| Diabetes | 1.29 [1.20, 1.38]*** | 1.62 [1.49, 1.76]*** | 1.43 [1.35, 1.50]*** |
| Hypertension | 1.60 [1.50, 1.70]*** | 1.50 [1.39, 1.63]*** | 1.55 [1.47, 1.62]*** |
| Atrial fibrillation | 1.20 [0.86, 1.67] | 1.06 [0.72, 1.55] | 1.16 [0.90, 1.49] |
| Stroke | 1.31 [1.11, 1.55]** | 1.49 [1.23, 1.82]*** | 1.37 [1.20, 1.55]*** |
| Lipid disorder without any statin prescriptionb | 1.12 [1.01, 1.24]* | 1.15 [1.03, 1.28]* | 1.14 [1.06, 1.23]*** |
| Statin prescription for those without lipid disorderb | 1.62 [1.46, 1.80]*** | 1.59 [1.38, 1.82]*** | 1.59 [1.47, 1.73]*** |
| Lipid disorder with statin prescriptionb | 0.73 [0.61, 0.87]*** | 0.63 [0.50, 0.78]*** | 0.69 [0.60, 0.79]*** |
***P < 0.001, **P < 0.01, *P < 0.05
aHazard ratio for schizophrenia, depression, and bipolar disorder is not shown because of extremely wide non-significant confidence intervals due to low prevalence
bReferent group: those without lipid disorder and without any statin prescription
Table 3 shows the results of the sex-combined model with an additionally estimated interaction between antipsychotic use and sex. The increase of hazard rate of acute IHD associated with antipsychotics was only observed among women (HR = 1.43, 95% CI 1.13–1.79) but not among men (HR = 2.21, 95% CI 2.11–2.31 for those who were not on antipsychotics versus HR = 2.16, 95% CI 1.67–2.80 for those who were prescribed antipsychotics). Likelihood ratio test result suggested significant interaction between antipsychotic use and sex (χ2 = 4.72, P = 0.030).
Table 3.
Adjusted hazard ratios [95% confidence intervals] of acute ischemic heart disease estimated from a mixed-effects Cox model with the specification of the interaction between antipsychotic use and sex
| Antipsychotic prescription for womena | 1.43 [1.13, 1.79]** |
| Men who were not on antipsychoticsa | 2.21 [2.11, 2.31]*** |
| Men with antipsychotic prescriptiona | 2.16 [1.67, 2.80]*** |
| Age (in 10 years) | 1.86 [1.83, 1.90]*** |
| Antidepressant prescription | 1.15 [1.01, 1.32]* |
| International Classification of Primary Care Diagnoses as baselineb | |
| Dementia | 0.76 [0.48, 1.22] |
| Tobacco abuse | 1.67 [1.40, 2.01]*** |
| Diabetes | 1.43 [1.35, 1.50]*** |
| Hypertension | 1.55 [1.47, 1.62]*** |
| Atrial fibrillation | 1.16 [0.90, 1.49] |
| Stroke | 1.37 [1.20, 1.55]*** |
| Lipid disorder without any statin prescriptionc | 1.14 [1.06, 1.23]*** |
| Statin prescription for those without lipid disorderc | 1.59 [1.47, 1.73]*** |
| Lipid disorder with statin prescriptionc | 0.69 [0.60, 0.79]*** |
***P < 0.001, **P < 0.01, *P < 0.05
aReferent group: women who were not on antipsychotics
bHazard ratio for schizophrenia, depression, and bipolar disorder is not shown because of extremely wide non-significant confidence intervals due to low prevalence
cReferent group: those without lipid disorder and without any statin prescription
According to this model (Table 3), antidepressant prescriptions (HR = 1.15, 95% CI 1.01–1.32), tobacco abuse (HR = 1.67, 95% CI 1.40–2.01), diabetes (HR = 1.43, 95% CI 1.35–1.50), hypertension (HR = 1.55, 95% CI 1.47–1.62), stroke (HR = 1.37, 95% CI 1.20–1.55), lipid disorder (HR = 1.14, 95% CI 1.06–1.23), and statin prescription for those without lipid disorder (HR = 1.59, 95% CI 1.47–1.73) were associated with a greater risk of acute IHD, while statin prescription for those with lipid disorder was associated with a reduced risk (HR = 0.69, 95% CI 0.60–0.79). No substantial sex differences were observed in the results regarding the potential confounders.
Sensitivity analysis
As shown in Fig. 3, in the 16 replications of the main analysis with each of the antipsychotic medications omitted in defining antipsychotic use, the hazard ratios for antipsychotic use among women remained similar, except for the analysis with haloperidol omitted: the association between antipsychotic use and IHD attenuated and became non-significant (HR = 1.23, 95% CI 0.95–1.60).
Fig. 3.
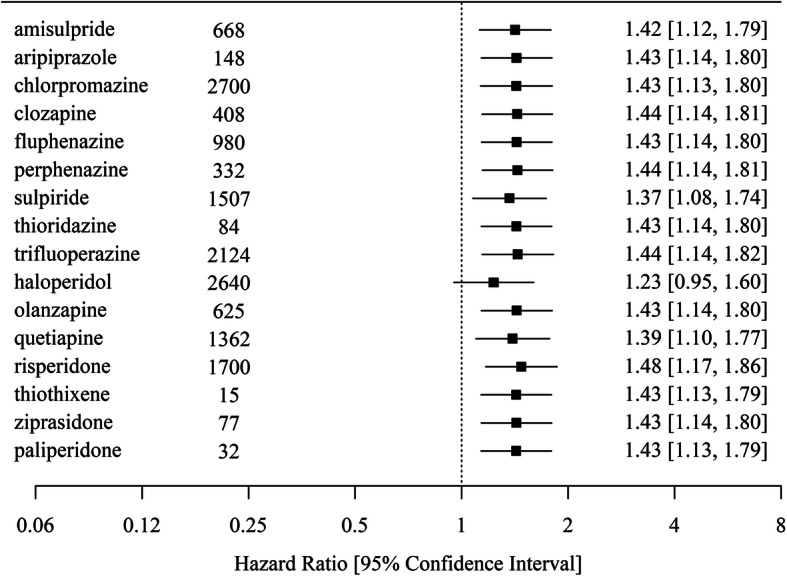
Forest plot showing the hazard ratios of ischemic heart disease for antipsychotic use among women from the replicated main analysis with each of the listed 16 antipsychotics omitted. The number of patients in the cohort who were prescribed the antipsychotic at least once in the past 12 months is also shown
When haloperidol was adopted as the main exposure, the hazard ratio for antipsychotic use among women was 2.51 (95% CI 1.65–3.79).
Among those prescribed antipsychotics at least once and each specific antipsychotic medication included as an independent variable, no interaction between antipsychotics and sex or main effects of antipsychotic use were significant (P > 0.05).
Additional file 1 Table S1 shows the hazard ratios for antipsychotic use among women with each specific type of acute IHD omitted in defining the outcome. The strength of association remained largely consistent with the omission of the eight specific types of IHD (HR ranged from 1.37 to 1.49).
With the threshold of the number of antipsychotic prescriptions adopted to define antipsychotic use varying from one to eight, Additional file 2: Table S2 shows the hazard ratios for antipsychotic use among women estimated from the sex-combined model (with interaction between antipsychotic use and sex). The strength of association remained similar across this range of thresholds (HR ranged from 1.39 to 1.64).
The replicated analysis on a sample selected without applying the exclusion criteria of previous hospital admission and IHD diagnosis showed that the hazard ratio for antipsychotic use among women was estimated at 1.43 (95% CI 1.24–1.65), which was the same as the main analysis but with a narrower confidence interval.
The analysis replicated with diabetes, hypertension, lipid disorder, and statin prescription excluded as potential confounders also provided highly similar results with the main analysis, with the hazard ratio for antipsychotic use among women estimated at 1.38 (95% CI 1.10–1.73).
Discussion
In this study, we identified a higher risk of acute IHD among Hong Kong Chinese middle-aged and older primary care recipients on antipsychotics, and this heightened risk was only evident among women but not among men. Sensitivity analyses also suggested that a specific antipsychotic medication, i.e., haloperidol, may explain this elevated risk in women.
Relationship with the literature
To the best of our knowledge, this is the largest study on the sex difference of the association between antipsychotics and IHD incidence in a primary care population. Our results are consistent with a previous study of 277,817 adults which showed a more substantial elevation of the risk of IHD among women with various psychiatric disorders treated with antipsychotics compared with men [16], but are inconsistent with a meta-analysis which showed that the association was slightly stronger among men than among women in a pooled analysis [5]. This inconsistent finding may have been due to the different patient populations adopted by the included studies. In fact, most reviewed studies only included patients with certain psychiatric disorders, such as schizophrenia, unlike our current study which observed a much more diverse population of primary care patients [5].
The sensitivity analysis of the current study extends this result to suggest that a specific antipsychotic medication, i.e., haloperidol, rather than antipsychotics in general, may underlie this sex difference.
Interpretations
With no randomization procedures conducted, there is a risk of confounding-by-indication: the observed association between antipsychotic use and IHD may only be a consequence of an underlying factor which induced antipsychotic use and caused IHD. The observed sex moderation, nevertheless, possibly suggests potentially different mechanisms of the physiological responses to antipsychotics (or to the unobserved underlying factors which prompted antipsychotic use) and the shaping of cardiovascular risks between men and women. Our findings should inform further research hypotheses on the underlying mechanisms of the relationship between antipsychotics and IHD and the clinical practices in managing the cardiovascular risks among patients on antipsychotics.
Increased metabolic abnormalities are the most widely accepted intermediary mechanisms in previous research to explain the observed elevated risk of IHD among people on antipsychotics [17]. These abnormalities include weight gain and obesity [18], elevated glucose levels [19], and lipid disorders [20]. Animal research has suggested a potential physiological difference between male and female in the development of these abnormalities [21], with being female associated with higher risks in general. While the animal-to-human interpolation of the physiological differences is subject to further verification, epidemiological research has observed significantly higher prevalence of antipsychotic-associated metabolic abnormalities, such as elevated glucose levels [22] and weight gain among women [23]. Further research with a longer follow-up period should investigate the potential intermediary role of different metabolic condition diagnoses in the association between antipsychotic use and IHD.
Previous studies have also shown that, to achieve the same degree of psychotic symptom reduction, a lower dose of antipsychotics is typically needed for women than for men [24]. It is possible that the observed sex moderation of the association between antipsychotics and IHD was due to doses that were higher than necessary to achieve the same anticipated clinical response in women as in men. Limited by data availability, nevertheless, we did not include antipsychotic dosage and severity of psychotic symptoms in the analysis to investigate this possibility. Future research should incorporate these factors in the statistical analyses.
Another possible explanation of the sex difference of the association between antipsychotics and IHD is the different levels of medication adherence between men and women. There is research showing that men with mental disorders like schizophrenia and bipolar disorders demonstrated lower adherence to antipsychotic prescriptions than women did [25]. Hence, the observed effect modification could be a consequence of a greater proportion of men not taking their antipsychotics as instructed compared with women. Further research should include measures of medication adherence to adjust for this bias.
Limitations
Despite consistent coding of diseases by registered physicians in the database and the large sample size with sociodemographic characteristics similar to previous primary care research in Hong Kong [26], there are several limitations to this study that require caution while interpreting the results. First, we did not implement any randomization procedures to isolate the independent effect of antipsychotics. Results should be interpreted as possibly confounded by the factors which are conducive to the prescription of antipsychotics, such as severity of the condition. Second, the moderate effect size of the association and the lack of evidence of a dose-response relationship between antipsychotic use and IHD should be taken into consideration while inferring about causality. Third, the coding of psychiatric disorders in the data is scarce and likely underestimates the true prevalence judging by the wide prescription of antipsychotics typically for treating those disorders. This problem renders the delineation of the respective independent effects of antipsychotics and the disorders infeasible. Fourth, we did not have access to lifestyle and more detailed sociodemographic information of the patients to capture the potential behavioral pathways of the investigated association. Likewise, no intermediary biometric parameters such as weight gain or blood glucose levels were available for an examination of the potential underlying metabolic mechanisms. Fifth, we only had access to the data from the public health care sector. Patients who visited private clinics or admitted to private hospitals were not recorded. However, the public sector constitutes about 90% of the total inpatient services in Hong Kong [27] and general outpatients of public clinics are unlikely to be admitted to private hospitals. In addition, ambulances, which are publicly funded, only take patients to the Accident and Emergency Units of public hospitals.
Implications
If substantiated by further research with a more rigorous design, our study results and the generated hypothesis may have the potential to inform primary care physicians’ practices in their management of cardiovascular risks among patients on antipsychotics. Our results also suggest that the prescription of haloperidol, which may possibly underlie the association between antipsychotics and IHD, warrants further investigation. In fact, consistent with our own findings, there has already been previous research showing a higher risk of adverse events, including cardiovascular mortality, associated with the use of haloperidol [28, 29].
Conclusion
In conclusion, we found a moderate association between antipsychotics and IHD among female but not among male primary care patients in Hong Kong. As we lack further data on the potential intermediary variables to infer about the causal relationships between the included factors, further research should observe and capture the potential intermediary mechanisms and the dose-response relationship of this association to provide more rigorous evidence to inform clinical practices.
Supplementary information
Additional file 1 : Table S1. Adjusted hazard ratios [95% confidence intervals] of ischemic heart disease for antipsychotics use among women estimated from mixed effects Cox models with each type of ischemic heart disease omitted in the operationalization.
Additional file 2 : Table S2. Adjusted hazard ratios [95% confidence intervals] of ischemic heart disease for antipsychotic use among women with the threshold of the number of antipsychotic prescriptions for the operationalization of antipsychotic use varying from one to eight.
Acknowledgements
We gratefully acknowledge the Hospital Authority of Hong Kong for the facilitation of data access.
Abbreviations
- CI
Confidence interval
- HA
Hospital Authority
- HR
Hazard ratio
- ICD-9
International Classification of Diseases, Ninth Revision
- ICPC
International Classification of Primary Care
- IHD
Ischemic heart disease
Authors’ contributions
F.T.T.L., B.H.K.Y., and S.Y.S.W. designed the study. G.K.K.C. and P.Y.K.C were responsible for the data collection and cleaning. F.T.T.L., B.G., and S.W.M. implemented the analyses, and all authors including D.J.S., K.P.L., R.Y.C., E.L.Y.W., and E.K.Y. contributed to the interpretation of results. F.T.T.L. drafted the manuscript which all authors commented on and approved for submission.
Funding
The work described in this paper was fully supported by a commissioned grant from the Health and Medical Research Fund (HMRF) of the Food and Health Bureau of the Government of the Hong Kong Special Administrative Region and the Research Grants Council of the Hong Kong Special Administrative Region, China (Project Code: Elderly Care – CUHK).
Availability of data and materials
The data that support the findings of this study are available from the Hospital Authority of Hong Kong, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
Ethics approval and consent to participate
Ethical approval for the secondary analysis of anonymized data was obtained from the Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong (dated 25 August 2015).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Francisco T. T. Lai, Email: franciscottlai@cuhk.edu.hk
Bruce Guthrie, Email: bruce.guthrie@ed.ac.uk.
Stewart W. Mercer, Email: stewart.mercer@ed.ac.uk
Daniel J. Smith, Email: daniel.smith@glasgow.ac.uk
Benjamin H. K. Yip, Email: benyip@cuhk.edu.hk
Gary K. K. Chung, Email: gchung@link.cuhk.edu.hk
Kam-Pui Lee, Email: lkp032@cuhk.edu.hk.
Roger Y. Chung, Email: rychung@cuhk.edu.hk
Patsy Y. K. Chau, Email: patsychau@cuhk.edu.hk
Eliza L. Y. Wong, Email: lywong@cuhk.edu.hk
Eng-Kiong Yeoh, Email: yeoh_ek@cuhk.edu.hk.
Samuel Y. S. Wong, Email: yeungshanwong@cuhk.edu.hk
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12916-020-01765-w.
References
- 1.Barbui C, Gastaldon C, Papola D, Ostuzzi G. Antipsychotic drug exposure and risk of myocardial infarction. Epidemiol Psychiatr Sci. 2017;26:18–21. doi: 10.1017/S204579601600086X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papola D, Ostuzzi G, Gastaldon C, Morgano GP, Dragioti E, Carvalho AF, et al. Antipsychotic use and risk of life-threatening medical events: umbrella review of observational studies. Acta Psychiatr Scand. 2019;140:227–243. doi: 10.1111/acps.13066. [DOI] [PubMed] [Google Scholar]
- 3.Rotella F, Cassioli E, Calderani E, Lazzeretti L, Ragghianti B, Ricca V, et al. Long-term metabolic and cardiovascular effects of antipsychotic drugs. A meta-analysis of randomized controlled trials. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol. 2020;32:56–65. doi: 10.1016/j.euroneuro.2019.12.118. [DOI] [PubMed] [Google Scholar]
- 4.Zivkovic S, Koh CH, Kaza N, Jackson CA. Antipsychotic drug use and risk of stroke and myocardial infarction: a systematic review and meta-analysis. BMC Psychiatry. 2019;19:189. doi: 10.1186/s12888-019-2177-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang K-L, Fang C-J, Hsu C-C, Wu S-I, Juang JJM, Stewart R. Myocardial infarction risk and antipsychotics use revisited: a meta-analysis of 10 observational studies. J Psychopharmacol. 2017;31:1544–1555. doi: 10.1177/0269881117714047. [DOI] [PubMed] [Google Scholar]
- 6.Correll CU, Frederickson AM, Kane JM, Manu P. Does antipsychotic polypharmacy increase the risk for metabolic syndrome? Schizophr Res. 2007;89:91–100. doi: 10.1016/j.schres.2006.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shuai-Ting L, Cheng-Chung C, Hin-Yeung T, Chee-Siong L, Pinchen Y, Kai-Da C, et al. Association between antipsychotic use and risk of acute myocardial infarction. Circulation. 2014;130:235–243. doi: 10.1161/CIRCULATIONAHA.114.008779. [DOI] [PubMed] [Google Scholar]
- 8.Reckelhoff JF, Samson WK. Sex and gender differences in cardiovascular, renal and metabolic diseases. Am J Physiol Integr Comp Physiol. 2015;309:R1057–R1059. doi: 10.1152/ajpregu.00417.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang XY, Zhang RL, Pan M, Chen DC, Xiu MH, Kosten TR. Sex difference in the prevalence of smoking in Chinese schizophrenia. J Psychiatr Res. 2010;44:986–988. doi: 10.1016/j.jpsychires.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Keyes KM, Li G, Hasin DS. Birth cohort effects and gender differences in alcohol epidemiology: a review and synthesis. Alcohol Clin Exp Res. 2011;35:2101–2112. doi: 10.1111/j.1530-0277.2011.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bellettiere J, Carlson JA, Rosenberg D, Singhania A, Natarajan L, Berardi V, et al. Gender and age differences in hourly and daily patterns of sedentary time in older adults living in retirement communities. PLoS One. 2015;10:e0136161. doi: 10.1371/journal.pone.0136161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lai FTT, Wong SYS, Yip BHK, Guthrie B, Mercer SW, Chung RY, et al. Multimorbidity in middle age predicts more subsequent hospital admissions than in older age: a nine-year retrospective cohort study of 121,188 discharged in-patients. Eur J Intern Med. 2019;61:103–111. doi: 10.1016/j.ejim.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Gobbi G, Ghabrash MF, Nuñez N, Tabaka J, Di Sante J, Saint-Laurent M, et al. Antidepressant combination versus antidepressants plus second-generation antipsychotic augmentation in treatment-resistant unipolar depression. Int Clin Psychopharmacol. 2018;33:34–43. doi: 10.1097/YIC.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 14.Lai FTT, Mercer SW, Guthrie B, Yip BHK, Chung GKK, Zou D, et al. Sociodemographic moderation of the association between depression and stroke incidence in a retrospective cohort of 0.4 million primary care recipients with hypertension. Psychol Med. 2020;1–9. 10.1017/S0033291720001920. [DOI] [PubMed]
- 15.Therneau TM. Mixed effects Cox models [R package coxme version 2.2–16]. 2018.
- 16.Wu S-I, Chen S-C, Liu S-I, Sun F-J, JJM J, Lee H-C, et al. Relative risk of acute myocardial infarction in people with schizophrenia and bipolar disorder: a population-based cohort study. PLoS One. 2015;10:e0134763. doi: 10.1371/journal.pone.0134763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riordan HJ, Antonini P, Murphy MF. Atypical antipsychotics and metabolic syndrome in patients with schizophrenia: risk factors, monitoring, and healthcare implications. Am Heal drug benefits. 2011;4:292–302. [PMC free article] [PubMed] [Google Scholar]
- 18.Bak M, Fransen A, Janssen J, van Os J, Drukker M. Almost all antipsychotics result in weight gain: a meta-analysis. PLoS One. 2014;9:e94112. doi: 10.1371/journal.pone.0094112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hasnain M, Vieweg WVR, Hollett B. Weight gain and glucose dysregulation with second-generation antipsychotics and antidepressants: a review for primary care physicians. Postgrad Med. 2012;124:154–167. doi: 10.3810/pgm.2012.07.2577. [DOI] [PubMed] [Google Scholar]
- 20.Chaggar PS, Shaw SM, Williams SG. Effect of antipsychotic medications on glucose and lipid levels. J Clin Pharmacol. 2011;51:631–638. doi: 10.1177/0091270010368678. [DOI] [PubMed] [Google Scholar]
- 21.Davey KJ, O’Mahony SM, Schellekens H, O’Sullivan O, Bienenstock J, Cotter PD, et al. Gender-dependent consequences of chronic olanzapine in the rat: effects on body weight, inflammatory, metabolic and microbiota parameters. Psychopharmacology. 2012;221:155–169. doi: 10.1007/s00213-011-2555-2. [DOI] [PubMed] [Google Scholar]
- 22.Chen DC, Zhou MA, Zhou DH, Xiu MH, Wu GY, Kosten TR, et al. Gender differences in the prevalence of diabetes mellitus in chronic hospitalized patients with schizophrenia on long-term antipsychotics. Psychiatry Res. 2011;186:451–453. doi: 10.1016/j.psychres.2010.07.054. [DOI] [PubMed] [Google Scholar]
- 23.Coccurello R, Moles A. Potential mechanisms of atypical antipsychotic-induced metabolic derangement: clues for understanding obesity and novel drug design. Pharmacol Ther. 2010;127:210–251. doi: 10.1016/j.pharmthera.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 24.Crawford M, DeLisi LE. Issues related to sex differences in antipsychotic treatment. Curr Opin Psychiatry. 2016;29:211–217(7). doi: 10.1097/YCO.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 25.Ngui AN, Vasiliadis H-M, Tempier R. Factors associated with adherence over time to antipsychotic drug treatment. Clin Epidemiol Glob Heal. 2015;3:3–9. doi: 10.1016/j.cegh.2013.11.001. [DOI] [Google Scholar]
- 26.Xu RH, Cheung AW-L, Wong EL-Y. Development and validation of an instrument to measure patient engagement in Hong Kong Special Administrative Region. China Patient Prefer Adherence. 2018;12:1667–1675. doi: 10.2147/PPA.S171026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leung GM, Tin KYK, O’Donnell O. Redistribution or horizontal equity in Hong Kong’s mixed public–private health system: a policy conundrum. Health Econ. 2009;18:37–54. doi: 10.1002/hec.1342. [DOI] [PubMed] [Google Scholar]
- 28.Lao KSJ, Wong AYS, Wong ICK, Besag FMC, Chang WC, Lee EHM, et al. Mortality risk associated with haloperidol use compared with other antipsychotics: an 11-year population-based propensity-score-matched cohort study. CNS Drugs. 2020;34:197–206. doi: 10.1007/s40263-019-00693-5. [DOI] [PubMed] [Google Scholar]
- 29.Park Y, Bateman BT, Kim DH, Hernandez-Diaz S, Patorno E, Glynn RJ, et al. Use of haloperidol versus atypical antipsychotics and risk of in-hospital death in patients with acute myocardial infarction: cohort study. BMJ. 2018;360:k1218. doi: 10.1136/bmj.k1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 : Table S1. Adjusted hazard ratios [95% confidence intervals] of ischemic heart disease for antipsychotics use among women estimated from mixed effects Cox models with each type of ischemic heart disease omitted in the operationalization.
Additional file 2 : Table S2. Adjusted hazard ratios [95% confidence intervals] of ischemic heart disease for antipsychotic use among women with the threshold of the number of antipsychotic prescriptions for the operationalization of antipsychotic use varying from one to eight.
Data Availability Statement
The data that support the findings of this study are available from the Hospital Authority of Hong Kong, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.