Abstract
Objective
A laryngocele is a space that develops as a result of pathological dilatation of the laryngeal saccule. However, the reported management of laryngoceles varies. We conducted a systematic review of the literature regarding the surgical management of laryngoceles and pyolaryngoceles, to understand the evolving nature of treatment for this rare condition.
Methods
We searched for publications in the PubMed, Cochrane Library, JBI Library of Systematic Reviews, and Ovid databases using the terms “laryngocele”, “pyolaryngocele”, and “laryngopyocele”, and reviewed the identified articles.
Results
After removal of repeated studies and filtering for relevance and studies written in English, a total of 227 studies were included in this review. No meta-analyses or randomized controlled trials have been published. The identified studies have been summarized in 14 reviews conducted since 1946. The meta-analysis determined that endoscopy was the preferred approach for internal laryngoceles, while combined laryngoceles benefited from both internal and external surgical approaches.
Conclusions
Laryngocele management has progressed since its initial description, from open surgery to an endoscopic approach, and more recently to a robotic-assisted surgical approach. The uptake of robotic surgery as a possible treatment modality over the last decade shows much promise for the treatment of these conditions.
Keywords: Laryngocele, pyolaryngocele, microlaryngoscopy, transoral robotic surgery, surgery, tracheostomy
Introduction
A laryngocele is a space that develops as a result of the pathological dilatation of the laryngeal saccule. Laryngoceles extend upwards within the false vocal fold communicating with the larynx.1 These rare lesions of the larynx can be classified as internal or combined. Internal laryngoceles expand medially to the thyroid hyoid membrane, while combined laryngoceles are positioned both medial and lateral to the membrane.2 Laryngoceles usually occur in men above 50 years of age, and most are unilateral and combined-type.1,2
There are numerous theories regarding the pathophysiological process leading to laryngoceles. Risk factors include congenital factors, increased laryngeal pressure, and mechanical obstruction.2,3 Mechanical obstruction of the ventricle is particularly concerning, because it is often secondary to a malignant process.1,2
Laryngoceles are typically filled with air; however, they can be filled with mucus if the neck becomes obstructed because of inflammation or mechanical obstruction. The dilated saccule can also become infected, forming a laryngopyocele, which can in turn cause significant laryngeal supraglottic edema and mechanical obstruction. Laryngopyoceles can occasionally present as acute airway emergencies.
The reported management of laryngoceles varies.4,5 We therefore conducted a systematic review of the surgical management of laryngoceles and pyolaryngoceles, to understand the evolving nature of treatment for this rare condition.
Methods
Data search
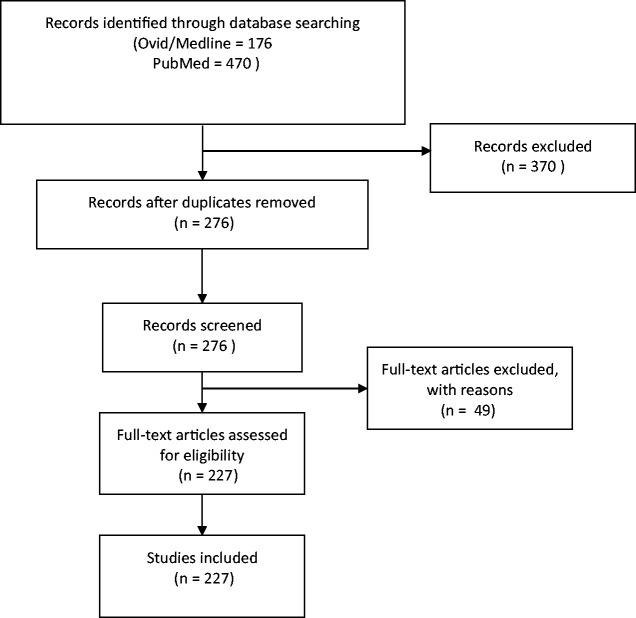
We conducted a systematic review of publications in the PubMed, Cochrane Library, JBI Library of Systematic Reviews, and Ovid databases using the search terms “laryngocele”, “pyolaryngocele”, and “laryngopyocele”, to identify all relevant articles. All articles were reviewed and only those written in English were included. Journal articles published between 1946 and 2019 were included. Studies were excluded if there was no surgical management. This systematic review was carried out according to the Preferred Reporting Items for Systematic reviews and Meta-analysis (PRISMA) guidelines. The PRISMA flow chart is shown in Figure 1.
Figure 1.
Study search criteria and flow chart.
Information on patient demographics, type of laryngocele, presence of pyolaryngocele, treatment, recurrence, airway management, and tracheostomy insertion was collected. Laryngoceles that were considered external were included in the combined group for this review, given that all laryngoceles originate from the internal structure of the saccule.6 Ethical approval was not required for this study because it was based on a review of previous studies.
Statistical analysis
Descriptive statistical analysis was performed using IBM SPSS Statistics for Windows, version 25.0 (IBM, Armonk, NY, USA).
Results
Using the search terms “laryngocele”, “pyolaryngocele”, and “laryngopyocele”, we identified a total of 176 and 470 articles in Ovid Medline and PubMed, respectively. No meta-analyses were found in the Cochrane Library and no systematic reviews in the JBI Library. After removing duplicate studies and filtering for English-only studies and relevance, a total of 227 studies were included in the current review, summarized in 14 reviews conducted since 1946. There were no published meta-analyses or randomized controlled trials.
Laryngocele management
Most internal cases were excised via an endoscopic approach, but 14 cases were treated by open surgery, with no reported complications. Open procedures included a transthyrohyoid membrane approach, thyrotomy with resection of the upper third of the thyroid cartilage, and V-shaped thyrotomy.1,6–8 Open surgery was preferred in patients with complicating etiologic factors, such as malignancy, other etiologies including congenital conditions, Zencker’s diverticulum or secondary to laryngectomy, previous surgery, or emergency surgical requirements.7,9–11
Laryngocele was treated by combined internal and open approaches in 15 cases, with no reported complications. The combined approach involved internal endoscopic laser resection, with a variety of open surgical approaches including a midline transcervical incision or V-shaped lateral thyrotomy.2,12 However, Martinez et al.5 reported on two cases with combined-type laryngocele who were managed solely with endoscopic laser resection. There were no reported complications associated with either approach, and only one post-mortem death, secondary to airway obstruction due to a combined laryngocele.13
Robotic surgery
Seven studies reported the use of robotic surgery to excise laryngoceles, in combination with laser surgery1,14–19 (Table 1). All 18 patients who underwent robotic surgery (13 male, 5 female) had combined-type laryngoceles. One patient required a covering tracheostomy to protect the airway prior to surgery to ensure that there was no intraoperative airway emergency, five required nasogastric feeding, and there was one reported case of perioperative laryngeal bleeding requiring open surgical management and control.17 No patients in any of the studies reported dysphagia, dysphonia, or recurrence at 3–6 months’ follow-up.
Table 1.
Transoral robotic surgery management for laryngocele.
| Study | Total patients |
Males | Females | Age (years, mean) |
Indication for surgery |
Type | Bilateral | Procedure | Discharge (days postoperatively) |
Oral intake postoperatively (days) |
Tracheostomies | Complications | Follow-up (months, mean) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lisan et al.14 | 1 | 1 | 0 | 61 | Laryngomucocele | Combined | TORS + laser resection of ventricular fold. |
1 | 6 | ||||
| Gal et al.15 | 1 | 1 | 0 | 37 | Laryngopyocele | Combined | TORS | 2 | 2 | NG: 1 | 36 | ||
| Kayhan et al.16 |
6 | 6 | 0 | 51.7 (41–62) |
Laryngocele: 3 | Mixed 4 | TORS | 6.5 (3–10) | 2 | 2 | NG >24 hours: 2 |
29 (3–55) | |
| Laryngomucocele: 2 | Internal 2 | ||||||||||||
| Laryngopyocele: 1 | |||||||||||||
| Villeneuve et al.17 |
8 | 4 | 4 | 61.8 (50–84) |
Laryngocele 8 | Combined 3 | 1 | TORS | 5 (1–10) | 1.25 days (0–5) | 1 | Post-operative hemorrhage: 1 (day 11) |
19.7 (1–68) |
| Internal 5 | NG: 3 | ||||||||||||
| Ciabatti et al.18 | 1 | 0 | 1 | 69 | Laryngocele | Mixed | Left | TORS | 2 | 1 | |||
| Patel et al.19 | 1 | 1 | 0 | 43 | Laryngocele | N/A | Right | TORS | 1 |
NG, nasogastric; TORS, transoral robotic surgery.
Airway management
Airway management was generally carried out via an endotracheal tube, with successful intubation by direct laryngoscopy and video laryngoscopy using a fiberoptic method (Table 2). The reviewed literature included four reports of patients with internal pyolaryngoceles requiring tracheostomy to secure the airway,20–22 while six patients with combined laryngoceles required a covering tracheostomy. Covering or elective tracheostomies were performed in all these cases. One case required emergent airway management, and one case used transtracheal jet ventilation. Tracheostomy had no reported effects on surgical outcomes, recurrence, voice, or dysphagia. One patient underwent a tracheostomy prior to developing a combined laryngocele, which was noted following a long tracheostomy inserted due to polio.
Table 2.
Use of tracheostomy for control of airway in laryngocele.
| Study | Number of laryngocele patients |
Mode of treatment |
Number of tracheostomies |
Indication for insertion |
Number of days decannulation |
|---|---|---|---|---|---|
| Kara et al.29 | 1 | Combined approach |
1 | Elective | |
| Raine et al.30 | 1 | Aspiration | 1 | Elective | Discharged home with permanent tracheostomy with a view to definitive resection as an elective procedure |
| Ueha et al.7 | 1 | Open approach | 1 | Elective | 7 days |
| Villeneuve et al.17 | 8 | TORS | 1 | Elective | |
| Kayhan et al.16 | 6 | TORS | 2 | Elective | 10 days |
| Mitroi et al.31 | 1 | Laryngectomy | 1 | Emergency | |
| Herrag et al.32 | 1 | Open approach | 1 | Elective | |
| Felix et al.23 | 1 | Open approach | 1 | Emergency | |
| Martinez et al.5 | 12 | Endoscopic | 2 | Emergency | |
| Pennings et al.10 | 1 | Endoscopic approach |
1 | Emergency | |
| Vasileiadis et al.20 | 1 | Drainage | 1 | Emergency | Discharged with tracheostomy |
TORS, transoral robotic surgery.
Discussion
Laryngoceles were first described as an entity in 1867 by Virchow and were thought to involve a dilatation of the laryngeal ventricle, described as “laryngocele ventricularis”, while the first reported case in 1829 was described by Dominique Larrey as “goitre aeriennes”.23 Laryngoceles are a herniation of the laryngeal ventricle, which communicates with the larynx.23 Specifically, the ventricle is a fusiform dilatation of the larynx between the true and false vocal cords, extending from the thyroid notch to the arytenoids.23 The anterior part communicates with a pouch, namely the saccule, which is where the laryngocele forms.1,23 Its histological structure consists of a membranous sac lined by ciliated pseudo-stratified cylindrical epithelium with a variable number of goblet cells on a thin basal membrane.23
Laryngocele is an extremely rare condition, with an incidence of only one in 2.5 million people per year.22 However, laryngoceles are five times more common in men than women, with a peak incidence between the fifth and sixth decades of life.1 Infection in a laryngocele leading to the accumulation of pus and the formation of a laryngopyocele is even rarer.24 Vasileiadis et al.20 reported on 39 cases, of whom only four developed acute airway obstruction and only one was a laryngopyocele. There have been 64 reported cases of laryngopyocele from 1925 to 2019. Byard and Gilbert25 found that the risk of death due to laryngopyocele was increased not only as a result of obstruction by the mass, but also by the discharge of pus into the airway, leading to aspiration, jugular vein thrombosis, or mediastinal abscess, with three reported deaths.
Management is often directed by the type of laryngocele. All laryngoceles were traditionally excised via an open approach,1 and the types of open approach have not changed dramatically over the last two decades: transthyrohyoid membrane approach, thyrotomy with resection of the upper third of the thyroid cartilage, and V-shaped thyrotomy.1,3,7,8,20,22,26 However, the advent of microlaryngoscopy and CO2 lasers have allowed an endolaryngeal approach.22 This review suggests that most combined laryngoceles are now treated by joint open and endoscopic approaches, with the advantage of greater exposure allowing for a more precise procedure.1,22
While a joint endoscopic and open approach has been advocated for combined laryngoceles, some cases have been treated by an endolaryngeal approach alone.5,27 Martinez et al.5 conducted a retrospective chart review, which included three patients with combined laryngoceles managed via an endoscopic approach, with no complications. They described a technique for combined laryngoceles involving the external component being medialized (i.e., pushed towards the larynx) through laser mobilization, traction, and microsurgical dissection, allowing for complete removal of both internal and external components via an endoscopic procedure.5 Various open surgical approaches have been used for combined laryngoceles, including a recent cartilage-preserving technique described by Aydian et al.,26 which differed from previous approaches that required either sacrificing the thyroid cartilage or exposure. The most commonly reported open approach was a transthyroid approach, which preserves the cartilage but sacrifices exposure. A total of 17 reported cases since 1977 reported the use of the transthyroid approach to manage the external component of the laryngocele, with most open approaches carried out in conjunction with endoscopic procedures to manage a combined laryngocele.
Internal laryngoceles are routinely managed by an endolaryngeal CO2 laser approach, though cold steel and combined pen surgical approaches have also been utilized. The present review found that most patients underwent a CO2 laser approach. Resection with a CO2 laser is the preferred technique, because it is precise, efficient, and safe compared with an open approach.18 Furthermore, rehabilitation is faster in terms of swallowing and speech.16 The endolaryngeal approach for internal laryngoceles has several disadvantages, including limited exposure, scarring, incomplete resection, and the need for specialized equipment. However, internal laryngoceles were rarely managed by an open approach, with only nine reported cases since 1952. These all preceded the regular use of endoscopic techniques, and were all published prior to 1990. The open surgical approaches used to treat internal laryngoceles included transcervical incision or approach through a laryngofissure.14
Seven studies, including five case reports and two case series, examined the use of robotic surgery, including transoral robotic surgery (TORS) for the removal of a combined laryngocele. Ciabatti et al.18 commented that it allowed for greater visualization and mobilization, therefore enabling greater access to the more external components of the combined laryngocele. A prospective study by Kayhan et al.16 including six men who underwent TORS for laryngoceles found no recurrence and significantly reduced dysphagia compared with traditional open techniques. Lisan et al.14 reported on the use of a laser-assisted TORS approach for a combined laryngomucocele , in which both the internal and external components of the were managed successfully via a minimally invasive approach, with no evidence of recurrence.14,15 Most reported cases (45%) resected by TORS were combined laryngoceles,14–19 with no reported recurrences in any cases of combined laryngocele managed by TORS, up to 3 years after treatment. Only three patients required a covering tracheostomy, and they were successfully decannulated an average of 2 days post-procedure.16,17 In this review, TORS enabled a single-access approach to managing combined laryngoceles that would previously have required a dual approach.
Anesthetic airway management during endolaryngeal surgery can be difficult and is often based on institutional, anesthetic, and surgeon preferences. Most reported cases did not comment on the authors’ preferred method of proximal jet ventilation, but there was one case report of the use of transtracheal jet ventilation in a patient with a compromised airway secondary to laryngocele.28 Tracheostomy was rarely used for airway control and management either pre- or post-operatively, but was used for emergency surgical airway protection in eight patients. Seven patients in the literature presented with an emergent airway secondary to an infected laryngocele, requiring tracheostomy insertion,17 while only three patients had elective insertion of a covering tracheostomy, conducted in conjunction with either TORS or endoscopic laryngeal management.30 Successful rapid decompression and anesthetic assistance can allow for minimal airway compromise, thus avoiding the need for a surgical airway in the acute setting.
In conclusion, laryngocele management has progressed since its initial description, from an open to an endoscopic approach, and more recently, to a robotic-assisted surgical approach. Advances in microlaryngoscopy, with increased laser usage, has ushered in a new philosophy in the management of laryngeal disease. Endoscopic treatment has enabled less-invasive procedures to be carried out, with improved surgical outcomes and reduced morbidity. The uptake of TORS in the last decade, as another possible treatment modality, shows great promise. However, microlaryngoscopy currently remains the gold standard for the management of internal laryngoceles.
Footnotes
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Ravjit Singh https://orcid.org/0000-0003-4256-5993
References
- 1.Zelenik K, Stanikova L, Smatanova K, et al. Treatment of laryngoceles: what is the progress over the last two decades? Biomed Res Int 2014; 2014: 819453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mobashir MK, Basha WM, Mohamed AE, et al. Laryngoceles: concepts of diagnosis and management. Ear Nose Throat J 2017; 96: 133–138. [DOI] [PubMed] [Google Scholar]
- 3.Dursun G, Ozgursoy OB, Beton S, et al. Current diagnosis and treatment of laryngocele in adults. Otolaryngol Head Neck Surg 2007; 136: 211–215. [DOI] [PubMed] [Google Scholar]
- 4.Dhaha M, Jbali S, Dhambri S, et al. Laryngocele after subtotal laryngectomy. Iran J Otorhinolaryngol 2018; 30: 305–308. [PMC free article] [PubMed] [Google Scholar]
- 5.Martinez Devesa P, Ghufoor K, Lloyd S, et al. Endoscopic CO2 laser management of laryngocele. Laryngoscope 2002; 112: 1426–1430. [DOI] [PubMed] [Google Scholar]
- 6.Thome R, Thome DC, De La Cortina RA. Lateral thyrotomy approach on the paraglottic space for laryngocele resection. Laryngoscope 2000; 110: 447–450. [DOI] [PubMed] [Google Scholar]
- 7.Ueha R, Nito T, Sakamoto T, et al. Supra-thyroid alar cartilage approach for the complete resection of laryngeal submucosal tumors and postoperative voice quality. Eur Arch Otorhinolaryngol 2015; 272: 2907–2913. [DOI] [PubMed] [Google Scholar]
- 8.Prasad KC, Vijayalakshmi S, Prasad SC. Laryngoceles - presentations and management. Indian J Otolaryngol Head Neck Surg 2008; 60: 303–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birt BD. Dysphagia due to simultaneous laryngocele and Zenker’s diverticulum. Laryngoscope 1985; 95: 1–2. [DOI] [PubMed] [Google Scholar]
- 10.Pennings RJ, Van Den Hoogen FJ, Marres HA. Giant laryngoceles: a cause of upper airway obstruction. Eur Arch Otorhinolaryngol 2001; 258: 137–140. [DOI] [PubMed] [Google Scholar]
- 11.Butskiy O, Anderson DW. Upper airway obstruction due to a change in altitude: first report in fifty years. J Otolaryngol Head Neck Surg 2016; 45: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahdoufi R, Barhmi I, Tazi N, et al. Mixed pyolaryngocele: a rare case of deep neck infection. Iran J Otorhinolaryngol 2017; 29: 225–228. [PMC free article] [PubMed] [Google Scholar]
- 13.Toro K, Kardos M, Dunay G. Fatal asphyxia due to laryngomucocele. Forensic Sci Int 2009; 190: e1–e4. [DOI] [PubMed] [Google Scholar]
- 14.Lisan Q, Hoffmann C, Jouffroy T, et al. Combined laser and robotic approach for the management of a mixed laryngomucocele. J Robot Surg 2016; 10: 81–83. [DOI] [PubMed] [Google Scholar]
- 15.Gal TJ, Hixon B, Zhang P. Transoral robotic resection of a combined laryngocele. J Robot Surg 2017; 11: 263–266. [DOI] [PubMed] [Google Scholar]
- 16.Kayhan FT, Gunes S, Koc AK, et al. Management of laryngoceles by transoral robotic approach. J Craniofac Surg 2016; 27: 981–985. [DOI] [PubMed] [Google Scholar]
- 17.Villeneuve A, Vergez S, Bakhos D, et al. Management of laryngoceles by transoral robotic surgery. Eur Arch Otorhinolaryngol 2016; 273: 3813–3817. [DOI] [PubMed] [Google Scholar]
- 18.Ciabatti PG, Burali G, D’Ascanio L. Transoral robotic surgery for large mixed laryngocoele. J Laryngol Otol 2013; 127: 435–437. [DOI] [PubMed] [Google Scholar]
- 19.Patel KB, Lin C, Kramer S, et al. Transoral robotic excision of laryngocele: surgical considerations. Head Neck 2019; 41: 1140–1143. [DOI] [PubMed] [Google Scholar]
- 20.Vasileiadis I, Kapetanakis S, Petousis A, et al. Internal laryngopyocele as a cause of acute airway obstruction: an extremely rare case and review of the literature. Acta Otorhinolaryngol Ital 2012; 32: 58–62. [PMC free article] [PubMed] [Google Scholar]
- 21.Fröhlich S, OʼSullivan E. Repeated episodes of airway obstruction caused by a pyolaryngocele. Eur J Emerg Med 2011; 18: 179–180. [DOI] [PubMed] [Google Scholar]
- 22.Swain SK, Mallik KC, Mishra S, et al. Laryngocele: experience at a tertiary care hospital of Eastern India. J Voice 2015; 29: 512–516. [DOI] [PubMed] [Google Scholar]
- 23.De Paula Felix JA, Felix F, De Mello LFP. Laryngocele: a cause of upper airway obstruction. Braz J Otorhinolaryngol 2008; 74: 143–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Yahya SN, Baki MM, Saad SM, et al. Laryngopyocele: report of a rare case and systematic review. Ann Saudi Med 2016; 36: 292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Byard RW, Gilbert JD. Lethal laryngopyocele. J Forensic Sci 2014; 60: 518–520. [DOI] [PubMed] [Google Scholar]
- 26.Aydin S, Demir MG. A new preserved technique for laryngocele: modified lateral thyrotomy approach. J Craniofac Surg 2014; 25: 2178–2179. [DOI] [PubMed] [Google Scholar]
- 27.Szwarc BJ, Kashima HK. Endoscopic management of a combined laryngocele. Ann Otol Rhinol Laryngol 1997; 106: 556–559. [DOI] [PubMed] [Google Scholar]
- 28.Parthasarathy S, Nag K, Sivashanmugham T, et al. Anesthetic management of excision of laryngocele-role of transtracheal jet ventilation. J Anaesthesiol Clin Pharmacol 2018; 34: 124–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kara I, Kokoglu K, Cagli S, et al. Bilateral laryngocele causing epiglottic deformity and upper airway obstruction. Turk Arch Otorhinolaryngol 2019; 57: 99–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raine JI, Allin D, Golding-Wood D. Laryngopyocoele presenting with acute airway obstruction. BMJ Case Rep 2014; 2014: bcr2014204102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mitroi M, Capitanescu A, Popescu FC, et al. Laryngocele associated with laryngeal carcinoma. Rom J Morphol Embryol 2011; 52: 183–185. [PubMed] [Google Scholar]
- 32.Herrag M, Lahmiti S, Sajiai H, et al. A laryngocele revealing a small cell lung carcinoma. B-ENT 2010; 6: 215–217. [PubMed] [Google Scholar]