Abstract
Background and Objective: Nausea, vomiting, and anorexia are the most common side effects reported in cancer patients undergoing chemotherapy. The present study aimed to determine the effect of peppermint extract on the severity of nausea, vomiting, and anorexia in patients with breast cancer undergoing chemotherapy. Methods and Materials: In this randomized controlled trial, we selected 84 patients with breast cancer undergoing chemotherapy. They were then assigned to 2 groups of experimental and control (n = 42, each) using block randomization. Patients in the experimental group received 40 drops of peppermint extract mixed in 20 cc of tap water every 8 hours, while patients in the control group received 40 drops of distilled water mixed in 20 cc of tap water every 8 hours. The severity of nausea, vomiting, and anorexia was measured and recorded before the intervention, and immediately, 24 and 48 hours after the chemotherapy using the Visual Analogue Scale. Statistical analysis of the data was conducted using SPSS software version 21. Results: The results of the present study revealed that there was a significant difference between the 2 groups at 24 and 48 hours after the chemotherapy (P < .05), so that the mean score of the severity of nausea, vomiting, and anorexia in the experimental group was lower than in the control group (P < .05). Conclusion: The use of peppermint as a method in complementary medicine may improve nausea, vomiting, and anorexia in patients with breast cancer undergoing chemotherapy. Further studies with greater sample size and longer follow-up period are needed to confirm the current findings.
Keywords: peppermint, nausea, vomiting, anorexia, breast cancer, chemotherapy
Introduction
The prevalence of cancer as a life-threatening disease is currently on the rise, so that cancer mortality is projected to rise by about 45% in developed countries by 2035.1 Breast cancer is the most frequent cancer among females, impacting 2.1 million women each year.2 Patients with breast cancer receive various treatments including radiotherapy, chemotherapy, and surgery. Among these, chemotherapy is a long-term and repetitive treatment that causes many side effects by damaging both normal and cancer cells.3,4 Nausea, vomiting, and anorexia are common side effects of chemotherapy and frequently encountered by cancer patients.5 Nausea and vomiting are associated with side effects such as dehydration, fluid and electrolyte imbalance, malnutrition, chemotherapy intolerance, and treatment refusal in patients. Uncontrollable nausea and vomiting can delay the chemotherapy schedule and decrease patients’ quality of life.6 Moreover, anorexia and weight loss occur in cancer patients due to reduced dietary intake and abnormal metabolism.7 These conditions are life-threatening as they increase mortality, reduce the treatment success rate, and cause severe psychological distress in patients and their families.8 Despite many advances in breast cancer treatment, patients still suffer from the physical and psychological symptoms of the disease. Therefore, efforts to alleviate the complications and side effects of cancer treatment are of great importance. Regarding the adverse effects and low efficacy of antiemetics used for chemotherapy-induced nausea and vomiting, 1 of the basic and low-risk measures to use is the complementary and alternative medicine (CAM).9 Based on the results of recent research, complementary medicine causes fewer side effects and cuts the treatment costs. It is also more effective, less invasive, and more accessible compared to other treatments. Recent studies have also indicated the increasing use of CAM in cancer treatment.10-12 Mentha piperita is a well-known herb in the food and pharmaceutical industries and is mostly used in the form of oily products or essential oils. The active ingredient in peppermint essential oil is called menthol and about 70% of peppermint essential oil is free menthol and menthol esters.13 Mentha piperita is utilized as a remedy for spasm, cramp, headache, migraine, indigestion, nausea, and flatulence. It also has antibacterial activity.14
Considering the fact that a large number of breast cancer patients undergoing chemotherapy suffer from nausea, vomiting, and anorexia, the present study aimed to determine the effect of peppermint extract on the severity of nausea, vomiting and anorexia in these patients.
Methodology and Materials
Design
This study was a triple-blinded randomized placebo-controlled trial conducted from November 2018 to July 2019 in one of the educational hospitals in Arak, Iran.
Ethical Considerations
Full ethical approval was obtained from the Ethics Committee of Arak University of Medical Sciences (with approval No. IR.ARAKMU.REC.1396.314). The study was also registered in the Iranian Registry of Clinical Trials (with registry No. IRCT20130731014229N7). Prior to the beginning of the study, all participants were provided with clear explanations of the study objectives and methodology, and the possibility of withdrawal from the study. They were then assured of the confidentiality of the data and the anonymity of the questionnaires. Subsequently, written informed consent was obtained from all participants. The study protocol was written in accordance with the principles of the Declaration of Helsinki.
Participants
We recruited a total of 84 patients with breast cancer undergoing chemotherapy who met clinical inclusion criteria. We determined the study sample size using the formula of compare means t-test and G*Power tool,15 and in accordance with the results of a study by Haddadi et al9 in which the nausea mean scores ± standard deviation (SD) were 2.9 ± 1.78 and 1.96 ± 1.24 in the control and the experimental group, respectively. The minimum sample size for each group was calculated to be 34 with 95% confidence interval and 80% power. Regarding the probability of sample attrition, the final sample size for each group was considered as 42. Inclusion criteria consisted of the followings: (a) patient with definite diagnosis of breast cancer by an oncologist, (b) having a history of receiving at least 1 cycle of chemotherapy, (c) having a history of nausea following chemotherapy sessions, (d) having no comorbidity causing nausea such as high blood pressure, hepatic and renal failure, and gastrointestinal disorders, (e) receiving no total-dose/upper abdominal radiotherapy concomitant with chemotherapy, and (f) having no sensitivity to peppermint. Exclusion criteria consisted of the followings: (a) forgetting to take peppermint oral drop 3 or more times in a row, (b) using medications or other treatments to reduce nausea severity other than the antiemetics prescribed for chemotherapy, (c) patient with refractory nausea and vomiting, (d) being affected by severe gastrointestinal side effects during the study period, and (e) premature withdrawal from the study. Eligible patients were enrolled in the study using convenience sampling. The participants were then randomly assigned to 4 homogeneous subgroups (blocks) of intervention (n = 2) and control (n = 2) using block randomization by statistical staff. Two blocks named “A” and 2 blocks named “B” were allocated the intervention (A, A) and the control group (B, B), respectively. Then, the group of each patient was determined by telephone consultation the statistical staff.
Intervention
The intervention was performed during 1 cycle of chemotherapy. Before the intervention, the severity of nausea and anorexia and the frequency of vomiting episodes in the 2 groups were measured using the Visual Analogue Scale (VAS) and the frequency table, respectively. Patients in both groups performed the intervention from 12 hours before16 up to 48 hours after chemotherapy so that, in addition to routine antiemetics, patients in the experimental group received 40 drops of peppermint extract (Supermint oral drop produced by Barij Essence Pharmaceutical Co., Kashan, Iran) mixed in 20 cc of tap water every 8 hours, and patients in the control group received 40 drops of distilled water mixed in 20 cc of tap water every 8 hours.17 For blinding, the peppermint oil and distilled water were dispensed in identical bottles with equal volume. The measurements were conducted again using the same tools immediately, 24 and 48 hours after the chemotherapy. Confounding variables, especially the antiemetics and other medications administered, were controlled using random assignment.
Data Collection
Data collection tools included a standard demographic survey, patients’ medical records, frequency table (for measuring the frequency of vomiting episodes), and the VAS (for assessing the severity of nausea and anorexia).
The VAS for appetite measurement consists of a 10-cm line in which the extremities were anchored by 0 being “not at all hungry” to 10 being “very hungry,” and the VAS for nausea severity measurement is also made up of a 10-cm line anchored with extreme nausea perceptions on the both ends from “0 = no feeling of nausea” to “10 = severe feeling of nausea.” The reliability and validity of this scale have been established in previous studies.18-20 Moreover, the reliability of this tool was approved by Shahinfar et al21 with a Cronbach’s alpha of 0.88. So, patients were able to assess and self-report the severity of their nausea and anorexia using this scale. We used this scale to assess the severity of nausea and anorexia in patients at 4 time-points of before the intervention, and immediately, 24 and 48 hours after the chemotherapy.
Statistical Analysis
Statistical analysis of the data was conducted using SPSS software version 21 (IBM Corp., Armonk, NY, USA). Data were described using descriptive statistics including mean, standard deviation, and frequency distribution. Moreover, analytical statistics including χ2 test, independent t-test, paired t-test, and repeated measures Analysis of Variance (ANOVA) were used to analyze the differences between and within the 2 groups.
Results
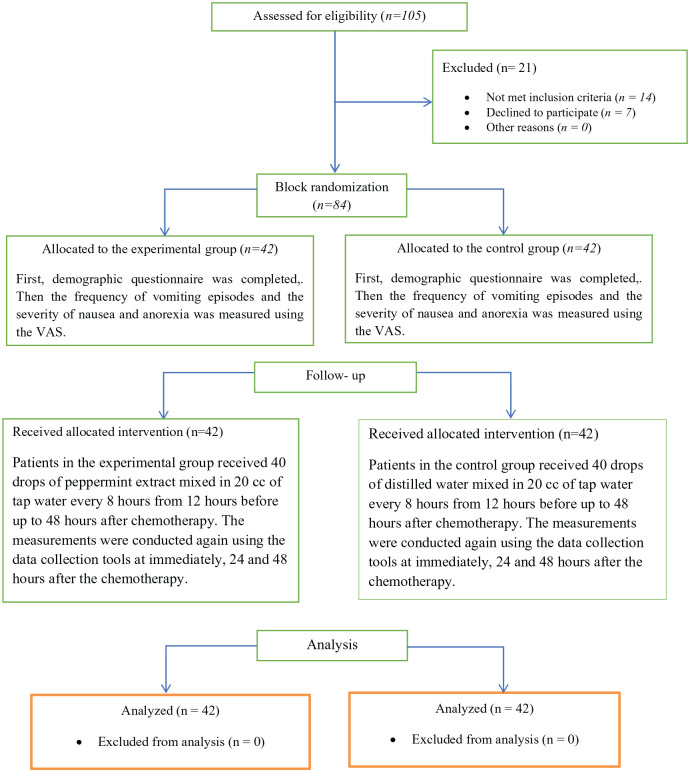
Of the 105 eligible patients, 14 did not meet the inclusion criteria and 7 refused to participate. Of the remaining 84 patients, all adhered to the study protocol and were included in the final analysis and none of the patients had any specific side effects due to the intervention performed during the study (Figure 1).
Figure 1.
The CONSORT flow diagram of the patients’ recruitment.
The mean age of the patients in the intervention group was 11.78 ± 49.60 years and in the control group was 9.52 ± 51.90 years. The mean number of chemotherapy cycles prior to the study in the intervention group was 5 ± 2.69 and in the control group was 5.40 ± 2.97 (P = .515). The educational level of 59% of the patients was less than high school diploma. Moreover, 88% of the participants were married and 85% were housewives. The mean duration of the illness in the experimental and the control group was 24.24 and 20.71 months, respectively. Both groups were homogeneous in terms of disease and demographic characteristics P > .05 (Table 1).
Table 1.
Demographic Characteristics in the Experimental and Control Groups.
| Group | Experimental group |
Control group |
P-value* | |||
|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | |||
| Demographic characteristics | ||||||
| Marital status | Single | 6 | 14.3 | 4 | 9.5 | .369 |
| Married | 36 | 85.7 | 38 | 90.5 | ||
| Educational level | Illiterate | 5 | 11.9 | 3 | 7.1 | .539 |
| Less than diploma | 18 | 42.9 | 24 | 57.1 | ||
| Diploma | 15 | 35.7 | 13 | 31 | ||
| Collegiate | 4 | 9.5 | 2 | 4.8 | ||
| Occupation | House wife | 34 | 81 | 38 | 90.5 | .361 |
| Employee | 7 | 16.7 | 4 | 9.5 | ||
| Self-employed | 1 | 2.4 | 0 | 0 | ||
| Medication regimens used for nausea | Granisetron, metoclopramide, dexamethasone | 37 | 88.1 | 40 | 95.2 | .216 |
| Ondansetron, granisetron, dexamethasone | 5 | 11.9 | 2 | 4.8 | ||
| Chemotherapy drugs | Trastuzumab | 5 | 11.9 | 4 | 9.5 | .104 |
| Doxorubicin, cyclophosphamide | 32 | 76.2 | 25 | 59.5 | ||
| Doxorubicin, cyclophosphamide, docetaxel | 5 | 11.9 | 13 | 31 | ||
Obtained from independent t-test or K2 test, where appropriate.
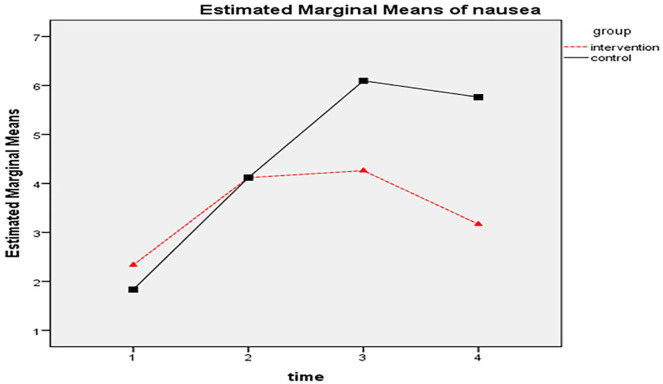
There was no significant difference in the mean score of nausea severity between the two groups before the intervention (P > .05). However, the difference was statistically significant at 24 and 48 hours after the chemotherapy (P < .05) so that the mean score of nausea severity in the experimental group was lower than in the control group (P = .001). In this regard, the results of repeated measures ANOVA with a Greenhouse-Geisser correction (1959) also showed that the Time effect, Group effect, and the Time × Group interaction were significant (P = .001) (Table 2; Figure 2).
Table 2.
The Mean Scores of Nausea Severity in the Experimental and Control Groups.
| Group |
P-value (repeated measures ANOVA) | |||
|---|---|---|---|---|
| Experimental group (n = 42) | Control group (n = 42) | |||
| Intervention time | Before the intervention | 2.33 ± 1.73 | 1.83 ± 2.17 | .247 |
| Immediately after the chemotherapy | 4.12 ± 1.72 | 4.12 ± 2.47 | 1.000 | |
| 24 h after the chemotherapy | 4.26 ± 2.06 | 6.10 ± 2.30 | <.001 | |
| 48 h after the chemotherapy | 3.17 ± 1.97 | 5.76 ± 2.91 | <.001 | |
| Group effect | F = 6.231542 | <.001 | ||
| Time effect | F = 69.629765 | <.001 | ||
| Time × Group interaction | F = 21.364054 | <.001 | ||
Figure 2.
The mean scores of nausea severity at 4 time-points (before the intervention, and immediately, 24 and 48 hours after the chemotherapy) in the experimental and control groups.
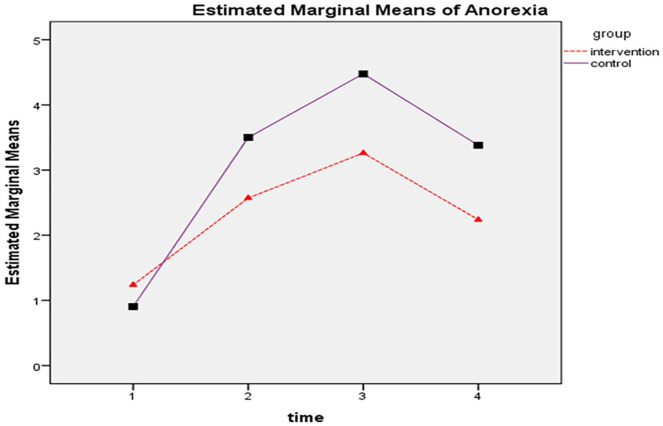
The difference in the mean score of anorexia severity between the 2 groups was not statistically significant before the intervention (P > .05). However, the difference was statistically significant at immediately, 24 and 48 hours after the chemotherapy (P < .05) so that the mean score of anorexia in the experimental group was lower in than the control group (P = .001). Based on the results of repeated measures ANOVA with a Greenhouse-Geisser correction, it was revealed that the Time effect, Group effect and the Time × Group interaction were significant (P < .05) (Table 3; Figure 3).
Table 3.
The Mean Scores of Anorexia Severity in the Experimental and Control Groups.
| Group |
P-value (repeated measures ANOVA) | |||
|---|---|---|---|---|
| Experimental group (n = 42) | Control group (n = 42) | |||
| Intervention time | Before the intervention | 1.24 ± 1.69 | 0.9 ± 1.16 | .296 |
| Immediately after the chemotherapy | 2.57 ± 1.97 | 3.50 ± 1.89 | .031 | |
| 24 h after the chemotherapy | 3.26 ± 2.03 | 4.48 ± 2.02 | .008 | |
| 48 h after the chemotherapy | 2.24 ± 1.75 | 3.38 ± 2.02 | .007 | |
| Group effect | F = 6.539992 | .012 | ||
| Time effect | F = 53.013599 | .003 | ||
| Time × Group interaction | F = 21.364054 | .001 | ||
Figure 3.
The mean scores of anorexia severity at 4 time-points (before the intervention, and immediately, 24 and 48 hours after the chemotherapy) in the experimental and control groups.
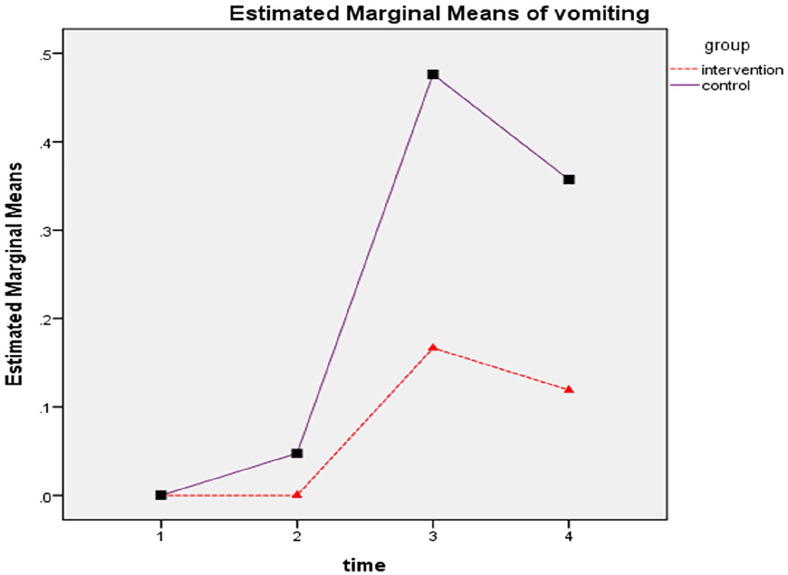
There was no significant difference in the mean frequency of vomiting episodes between the 2 groups before the intervention (P > .05). However, the results showed a significant difference between the 2 groups at 24 and 48 hours after the chemotherapy (P < .05) as the mean frequency of vomiting episodes was lower in the experimental group compared to the control group (P = .001). Moreover, the results of repeated measures ANOVA with a Greenhouse-Geisser correction indicated that the Time effect, Group effect and the Time × Group interaction were significant (P < .05) (Table 4; Figure 4).
Table 4.
Comparison of the Mean Frequencies of Vomiting Episodes in the Experimental and Control Groups.
| Group |
P-value (repeated measures ANOVA) | |||
|---|---|---|---|---|
| Experimental group (n = 42) | Control group (n = 42) | |||
| Intervention time | Before the intervention | 0.0 ± 0.0 | 0.0 ± 0.0 | |
| Immediately after the chemotherapy | 0.0 ± 0.0 | 0.05 ± 0.216 | .156 | |
| 24 h after the chemotherapy | 0.17 ± 0.537 | 0.48 ± 0.707 | .026 | |
| 48 h after the chemotherapy | 0.12 ± 0.395 | 0.36 ± 0.557 | .030 | |
| Group effect | F = 6.857105 | .011 | ||
| Time effect | F = 16.242982 | <.001 | ||
| Time × Group interaction | F = 3.559584 | .035 | ||
Figure 4.
The mean frequencies of vomiting episodes at 4 time-points (before the intervention, and immediately, 24 and 48 hours after the chemotherapy) in the experimental and control groups.
Discussion
In this study, we aimed to determine the effect of peppermint extract on the severity of nausea, vomiting and anorexia in patients with breast cancer undergoing chemotherapy. Based on the results of this study, no significant difference in the demographic variables was found between the 2 groups. It was also found that there was no statistically significant difference in the severity of nausea and anorexia, and the frequency of vomiting episodes between the 2 groups before the intervention. This was indicative of the similarity between the study groups. The results of this study showed a significant difference in the severity of nausea between the 2 groups at 24 and 48 hours after the chemotherapy as the severity of nausea in the experimental group was lower than in the control group. The results of repeated measures ANOVA also indicated that the severity of nausea decreased over the study period as there was a further significant reduction in the severity of nausea in the experimental group compared to the control group.
The results of a study by Haddadi et al9 showed that sucking ice bits containing mint extract during chemotherapy significantly decreased the severity of nausea. Eghbali et al22 revealed that aromatherapy with peppermint essential oil has led to a significant reduction in the severity of nausea during the acute phase of chemotherapy in patients with breast cancer. Based on the results of a study by Zorba and Ozdemir,23 it was found that the severity of nausea was significantly lower among patients in the inhalation aromatherapy group compared to the control group. In a study on the effect of aromatherapy with 3 types of essential oils including peppermint, ginger, and a combination of both on postoperative nausea and vomiting, Firington et al24 indicated that aromatherapy with the 3 types (each alone or in combination) could reduce the severity of postoperative nausea and there was no significant difference between the 3 types of inhalers used. The results of the above studies are consistent with the results of our study. However, in the above studies, mint aromatic inhalers were used to decrease the severity of nausea. Moreover, various studies have been conducted on the effect of mint on the severity of nausea in other patients.
In a study by Shahinfar et al,21 25 drops of 2% mint extract mixed in 30 cc of water were given to the patients in the experimental group. The results showed that the incidence and mean severity of nausea during cesarean section in the experimental group was significantly lower than in the control group. However, there was no statistically significant relationship between the 2 groups regarding the incidence and mean severity of nausea and vomiting at 2 and 4 hours after the surgery.25 Briggs et al26 found that peppermint oil inhalation is a viable treatment for postoperative nausea in patients undergoing cardiac surgery. The above studies confirm the positive effect of mint extract on nausea severity. Ferruggiari et al27 stated that inhalation aromatherapy with peppermint oil is not effective in decreasing the frequency and severity of postoperative nausea and vomiting. Najafi et al28 concluded that inhalation aromatherapy with peppermint essential oil does not affect postoperative nausea and vomiting in patients undergoing abdominal surgeries. In a study by Joulaeerad et al,29 it was found that aromatherapy with peppermint oil has no effect on the severity of nausea in pregnant women. The results of the above studies are not in line with our findings. These discrepancies are due to the diversity of the study populations, research settings, and methods of intervention. In our study, the patients received 40 drops of 2% peppermint extract mixed in 20 cc of tap water every 8 hours. Regarding the greater efficacy of gastrointestinal absorption, it seems that the oral administration of peppermint extract is more effective than inhalation.
The results of our study showed a statistically significant difference in the frequency of vomiting episodes between the 2 groups at 24 and 48 hours after the chemotherapy, so that the frequency of vomiting episodes significantly reduced in the experimental group compared to the control group. The results of repeated measures ANOVA also showed that the frequency of vomiting episodes decreased over the study period. In line with our findings, Ghani and Ibrahim30 showed that inhalation aromatherapy with lavender and peppermint oils resulted in a significant reduction in the frequency of vomiting episodes. Shahinfar et al21 indicated that the incidence and mean severity of vomiting episodes during cesarean section was significantly lower in the experimental group compared to the control group. In a study by Eghbali et al,22 it was also found that the frequency of vomiting episodes during the acute phase of chemotherapy was lower in the experimental group compared to the control group. However, this reduction was not statistically significant cancer.22 Haddadi et al9 stated that sucking ice bits containing mint extract has no effect on the frequency of chemotherapy-induced vomiting episodes. Pasha et al31 found that peppermint essential oil does not affect nausea and vomiting during pregnancy. In a study by Najafi et al,28 the findings showed that inhalation of peppermint essential oil has no effect on postoperative vomiting in patients undergoing abdominal surgeries. Joulaeerad et al29 revealed that aromatherapy with peppermint oil has no effect on the severity of vomiting in pregnant women. The results of the above studies are not in line with the results of our study. The reason for this discrepancy can be attributed to the study populations, types of intervention, and the mint dosage. In the present study, a high dose of peppermint was used, which can be more effective in reducing the severity of nausea and vomiting.
There are limited studies about the effect of CAM on anorexia in cancer patients. The results of the present study showed that the difference in the mean score of anorexia severity between the 2 groups was statistically significant after the chemotherapy so that the mean severity of anorexia in the experimental group was lower than in the control group. Furthermore, based on the results of repeated measures ANOVA, it was revealed that the severity of anorexia decreased over the study period so that there was a further significant reduction in the severity of anorexia in the experimental group. The results of a study by Jung and Lee32 demonstrated that aromatherapy with mint extract was effective in reducing the intensity of anorexia in cancer patients undergoing chemotherapy. Delavar et al33 found that peppermint oil capsules are effective in alleviating gastrointestinal complaints caused by premenstrual syndrome. Various studies have investigated the positive effects of peppermint on the gastrointestinal tract.34-36 The results of a study by Mizuno et al37 revealed that oral administration of peppermint oil decreases spasm at the esophagus, lower stomach, and duodenal bulb. Considering that the participants and the mechanism causing anorexia in the above studies are different from the ones in the present study, it is difficult to draw a comparison between the studies. Anorexia in patients undergoing chemotherapy can be caused by activation of the hypothalamic inflammatory pathways secondary to intestinal inflammation (inflammation triggers anorexia) or to dehydration from diarrhea.38
Based on the results of our study, it seems that a standard dose of peppermint extract (oral drop) causes no side effects and can be used as a treatment along with other medication treatments to reduce chemotherapy-induced nausea and vomiting. Since this study was conducted on patients with breast cancer, further studies are recommended to be conducted on patients with different types of cancer to clarify more points about the use of this approach.
Study Limitations
One of the limitations of this study is the effect of confounders on the results. To eliminate the confounding factors, random sampling was used to select identical samples. Moreover, the mean score of the severity of nausea, vomiting and anorexia was measured before the intervention and after the chemotherapy, and the mean scores were then compared. The second limitation is that this study was conducted on women with breast cancer undergoing chemotherapy. Therefore, it is not possible to generalize the study results to other patients undergoing chemotherapy. The third limitation is the small number of samples. Further studies with greater sample size are needed to confirm the current findings. A fourth limitation was the potential that patients guessed the type of intervention performed because of the smell of peppermint essential oil, a factor for which there is no control in this study.
Conclusion
We concluded that peppermint extract has the effect of reducing the severity of nausea and vomiting and improving the appetite in patients with breast cancer undergoing chemotherapy. Peppermint extract thus has the potential to be used as a non-invasive and low-cost nursing intervention along with other treatments to reduce the severity of nausea and vomiting and improve the appetite in cancer patients undergoing chemotherapy. Further studies with greater sample size and longer follow-up period are needed to confirm the current findings.
Acknowledgments
The authors would like to appreciate the patients and colleagues in oncology unit of Ayatollah Khansari hospital in Arak city, as well as the assistant of the Vice Chancellor for Research and Technology of Arak University of Medical Sciences. The authors would like to sincerely thank the assistants of deputy of research in Arak University of Medical Sciences and all the respected colleagues who helped us in this study. In addition to obtaining written consent, this study attempted to observe the provisions of ethical codes related to research and in particular respect for the freedom of individuals to refuse to continue studying and confidentiality of all personal information.
Footnotes
Authors’ Contribution: HJM, MA, MZ and MH: Study conception and design, data collection, data interpretation, and critical revision of the paper; MH, HJM and RH(clinical supervision): study conception and design; HJM and MH: study conception and design, and critical revision of the paper; MH and HJM: study conception and design, data analysis and interpretation, manuscript preparation, and critical revision of the paper. All the authors read and approved the final manuscript for submission.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Arak University of Medical Sciences, Arak, Iran (No: 2857).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical confirmation: The Ethics Committee of Arak University of Medical Sciences, Arak, Iran, approved this study (IR.ARAKMU.REC.1396.314).
Trial registration: This trial was registered in the Iranian Registry of Clinical Trials (IRCT20130731014229N7).
ORCID iD: Mehdi Harorani  https://orcid.org/0000-0002-9467-5986
https://orcid.org/0000-0002-9467-5986
References
- 1. Dadkhah B, Anisi E, Mozaffari N, Amani F, Pourghasemian M. Effect of music therapy with periorbital massage on chemotherapy-induced nausea and vomiting in gastrointestinal cancer: a randomized controlled trail. J Caring Sci. 2019;8:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bray F, Ferlay J, Soerjomataram I, Siegel R, Torre L, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [DOI] [PubMed] [Google Scholar]
- 3. Irmak Z, Tanrıverdi Ö, Ödemiş H, Uysal DD. Use of complementary and alternative medicine and quality of life of cancer patients who received chemotherapy in Turkey. Complement Ther Med. 2019;44:143-150. [DOI] [PubMed] [Google Scholar]
- 4. Yoon HG, Park H. The effect of auricular acupressure on sleep in breast cancer patients undergoing chemotherapy: a single-blind, randomized controlled trial. Appl Nurs Res. 2019;48:45. [DOI] [PubMed] [Google Scholar]
- 5. Hsu H-T, Lin K-C, Wu L-M, et al. Symptom cluster trajectories during chemotherapy in breast cancer outpatients. J Pain Symptom Manage. 2017;53:1017-1025. [DOI] [PubMed] [Google Scholar]
- 6. Hu J, Shen Y, Zhang G, et al. Effect of acupoint therapies on chemotherapy-induced nausea and vomiting: a systematic review protocol. Medicine. 2019;98:e17109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Le-Rademacher JG, Crawford J, Evans WJ, Jatoi A. Overcoming obstacles in the design of cancer anorexia/weight loss trials. Crit Rev Oncol Hematol. 2017;117:30-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Borner T, Liberini CG, Lutz TA, Riediger T. Brainstem GLP-1 signalling contributes to cancer anorexia-cachexia syndrome in the rat. Neuropharmacology. 2018;131:282-290. [DOI] [PubMed] [Google Scholar]
- 9. Haddadi M, Ganjloo J, Hashemifard HR, Tabarraie Y. The effect of sucking bits of ice containing mint (mentha) extract on nausea and vomiting resulted of chemotherapy in patients suffering from malignant cancer. Iran J Breast Dis. 2017;9:7-14. [Google Scholar]
- 10. Farahani MA, Afsargharehbagh R, Marandi F, et al. Effect of aromatherapy on cancer complications: a systematic review. Complement Ther Med. 2019; 47:102169. [DOI] [PubMed] [Google Scholar]
- 11. Harorani M, Zamenjani MN, Golitaleb M, et al. Effects of relaxation on self-esteem of patients with cancer: a randomized clinical trial. Support Care Cancer. 2020;28:405-411. [DOI] [PubMed] [Google Scholar]
- 12. Masmouei B, Harorani M, Ghafarzadegan R, Davodabady F, Zahedi S, Davodabady Z. The effect of progressive muscle relaxation on cancer patients’ self-efficacy. Complement Ther Clin Pract. 2019;34:70-75. [DOI] [PubMed] [Google Scholar]
- 13. Brown RP, Gerbarg PL. Herbs and nutrients in the treatment of depression, anxiety, insomnia, migraine, and obesity. J Psychiatr Pract. 2001;7:75-91. [DOI] [PubMed] [Google Scholar]
- 14. Bellassoued K, Hsouna AB, Athmouni K, et al. Protective effects of Mentha piperita L. leaf essential oil against CCl 4 induced hepatic oxidative damage and renal failure in rats. Lipids Health Dis. 2018;17:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Erdfelder E, Faul F, Buchner A. GPOWER: a general power analysis program. Behav Res Methods Instrum Comput. 1996;28:1-11. [Google Scholar]
- 16. Kiani M, Sabbagh M, Najafi M, et al. Effect supermint oil (peppermint oil) on patient satisfaction and the colonoscopy team during colonoscopy. Int J Pediatr. 2014;2:25-25. [Google Scholar]
- 17. Fazel N. The effect of supermint oil on pain severity after cesarean section. Babol Univ Med Sci. 2005;7:28-33. [Google Scholar]
- 18. Heruc GA, Little TJ, Kohn M, et al. Appetite perceptions, gastrointestinal symptoms, ghrelin, peptide YY and state anxiety are disturbed in adolescent females with anorexia nervosa and only partially restored with short-term refeeding. Nutrients. 2019;11:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Naito Y, Kai Y, Ishikawa T, et al. Chemotherapy-induced nausea and vomiting in patients with breast cancer: a prospective cohort study. Breast Cancer. 2020;27:122-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Elsacker T, Van Den Berghe S, De Groot M, Langius J. MON-P112: cut-off values for the Faact-A/CS and the VAS for appetite for the assessment of anorexia in cancer patients. Clin Nutr. 2017;36:S220. [Google Scholar]
- 21. Shahinfar J, Zeraati H, Vafaei S, Hashemi F. The incidence and severity of nausea and vomiting after surgery under general anesthesia induced by different doses of propofol. Anesthesiol Pain. 2017;8:107-117. [Google Scholar]
- 22. Eghbali M, Varaei S, Hosseini M, Yekaninejad MS, Shahi F. The effect of aromatherapy with peppermint essential oil on nausea and vomiting in the acute phase of chemotherapy in patients with breast cancer. Babol Univ Med Sci. 2018;20:66-71. [Google Scholar]
- 23. Zorba P, Ozdemir L. The preliminary effects of massage and inhalation aromatherapy on chemotherapy-induced acute nausea and vomiting: a quasi-randomized controlled pilot trial. Cancer Nurs. 2018;41:359-366. [DOI] [PubMed] [Google Scholar]
- 24. Fearrington MA, Qualls BW, Carey MG. Essential oils to reduce postoperative nausea and vomiting. J Perianesth Nurs. 2019; 34:1047-1053. [DOI] [PubMed] [Google Scholar]
- 25. Sahhinfar J, Zeraati H, Imani Hesary S, Masrorniya M, Shojaei S. The effect of mint extract on the incidence and severity of nausea and vomiting after cesarean section under spinal anesthesia: a Randomized Clinical Trial. Patient Saf Qual Improve J 2017;5:482-487. [Google Scholar]
- 26. Briggs P, Hawrylack H, Mooney R. Inhaled peppermint oil for postop nausea in patients undergoing cardiac surgery. Nursing. 2016;46:61-67. [DOI] [PubMed] [Google Scholar]
- 27. Ferruggiari L, Ragione B, Rich ER, Lock K. The effect of aromatherapy on postoperative nausea in women undergoing surgical procedures. J Perianesth Nurs. 2012;27:246-251. [DOI] [PubMed] [Google Scholar]
- 28. Najafi B, Ghahrisarabi A, Esmaeili R, Alavi Majd H, Mojab F. A survey on inhalation effect of essence of peppermint on nausea and vomiting after abdominal surgery in patients who have been admitted to Besaat and Tohid hospitals in Sanandaj. Adv Nurs Midwifery. 2014;24:27-32. [Google Scholar]
- 29. Joulaeerad N, Ozgoli G, Hajimehdipoor H, Ghasemi E, Salehimoghaddam F. Effect of aromatherapy with peppermint oil on the severity of nausea and vomiting in pregnancy: a single-blind, randomized, placebo-controlled trial. J Reprod Infertil. 2018;19:32. [PMC free article] [PubMed] [Google Scholar]
- 30. Ghani RMA, Ibrahim ATA. The effect of aromatherapy inhalation on nausea and vomiting in early pregnancy: a pilot randomized controlled trial. J Nat Sci Res. 2013;3:10-22. [Google Scholar]
- 31. Pasha H, Behmanesh F, Mohsenzadeh F, Hajahmadi M, Moghadamnia AA. Study of the effect of mint oil on nausea and vomiting during pregnancy. Iran Red Crescent Med J. 2012;14:727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jung ES, Lee BS. Effects of aroma oil inhalation on nausea vomiting and anorexia in cancer patients receiving chemotherapy. J Korean Acad Adult Nurs. 2004;16:135. [Google Scholar]
- 33. Delavar MA, Ebrahimi S, Esmaeilzadeh S, Khamse A. Effect of peppermint oil on premenstrual syndrome: a randomized, double-blind placebo-controlled study. Iran Red Crescent Med J. 2019;21: e84657. [Google Scholar]
- 34. Cash BD, Epstein MS, Shah SM. A novel delivery system of peppermint oil is an effective therapy for irritable bowel syndrome symptoms. Dig Dis Sci. 2016;61:560-571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Loolaie M, Moasefi N, Rasouli H, Adibi H. Peppermint and its functionality: a review. Arch Clin Microbiol. 2017;8:54. [Google Scholar]
- 36. Nimrouzi M, Zarshenas MM. Anorexia: highlights in traditional Persian medicine and conventional medicine. Avicenna J Phytomed. 2018;8:1. [PMC free article] [PubMed] [Google Scholar]
- 37. Mizuno S, Kato K, Ono Y, et al. Oral peppermint oil is a useful antispasmodic for double-contrast barium meal examination. J Gastroenterol Hepatol. 2006;21:1297-1301. [DOI] [PubMed] [Google Scholar]
- 38. Sinno MH, Coquerel Q, Boukhettala N, et al. Chemotherapy-induced anorexia is accompanied by activation of brain pathways signaling dehydration. Physiol. Behav. 2010;101:639-648. [DOI] [PubMed] [Google Scholar]