Due to the nationwide pandemic, the Ontario government has recommended guidelines in regard to social distancing and self-quarantining for vulnerable individuals, as well as any infected patients or those awaiting test results. As a community pharmacist practising in the rural community of Chapleau, Ontario, these recommendations pose unique challenges to the provision of my pharmacy services. Chapleau and surrounding communities include large elderly and Indigenous populations with a high prevalence of comorbidities, putting them at increased risk of developing severe coronavirus disease 2019 (COVID-19). Offering a delivery service would limit exposure and protect patients, but this was not feasible due to limited pharmacy staffing and the broad geographical region serviced.
To address this barrier, I collaborated with the local paramedic service and family health team to provide a delivery service to patients at high risk of severe COVID-19. A protocol was developed in which the pharmacy team scheduled deliveries for the patients and the paramedics executed these deliveries. This new service was advertised to the local physician offices as well as at the pharmacy. Since its initiation, the demand for delivery has been high, particularly for elderly patients who lack the social supports to assist with medication pickup. As a pharmacist, I am proud knowing that I am able to provide a valuable service to my community in a time of crisis. Not only will this provide safe access for patients, but it will also assist in preventing the spread of COVID-19 by reducing traffic within the pharmacy.

—Mathew Eidt, PharmD, RPh
Pharmacy Manager, Model Guardian Drug Store
Chapleau, Ontario
A few weeks ago, Alex Munter, the CEO of the Children’s Hospital of Eastern Ontario (CHEO), reached out to all staff asking for volunteers to help out in Ottawa’s nursing homes, as they have become extremely short-staffed. A number of pharmacists and technicians at CHEO who volunteered have already been deployed to the Madonna Long-Term Care Residence.
The volunteers are working 12-hour shifts, with tasks including cleaning high touch points, delivering meals, feeding residents, cleaning up after the meals, helping the nurses and personal support workers to provide care such as bathing and changing and keeping residents company as they are confined to their rooms during the pandemic.
One of our pharmacists is working in a unit that has about 25 residents, with all but one testing positive for COVID-19. Everyone is wearing the appropriate personal protective equipment, but ensuring that everything is always done with proper infection prevention and control techniques is challenging. One of the pharmacists, Stephanie Dean, says, “I think the hardest part for me has been trying to comfort those residents who are palliative or not doing well. They are suffering without having their families around them and are so lonely. On my 3 shifts alone, I have lost about 3 residents whom I was involved with. It is incredibly emotional work.” Another pharmacist, Bradley Murphy, says, “It just breaks my heart to see their posted pictures and what they look like now. I have spoken to one of the residents’ daughters and she has seen such a decline, not really because he is COVID positive but because of the isolation for the past weeks. . . . As I am sitting with a resident and assisting them with their meal, all I can think about is if this were my grandmother or grandfather, I would hope someone else would volunteer and step up to help out. They really need our help and it’s an experience I’ll never forget.”
—Heather Hammond
Senior Administrative Assistant
Pharmacy Department, CHEO
J’ai compris dès le début de la crise que je devais agir rapidement. En jetant un coup d’œil à ma salle d’attente, l’ampleur du risque de contamination et les conséquences potentielles sur la santé de mes patients les plus vulnérables m’apparaissaient graves et évidentes. J’ai dès lors choisi de fermer mes portes au public afin de contrôler l’accès à la pharmacie.
Plus d’un mois après le début de cette crise, cela peut sembler un choix évident puisque plusieurs pharmacies fonctionnent maintenant de cette façon, mais nous étions alors le 13 mars et personne ne saisissait encore les proportions que prendrait cette pandémie. En rétrospective, la décision était facile à prendre, mais c’était de la prendre avant tout le monde qui était le plus difficile.
Rapidement, la taille de notre laboratoire s’est avérée un défi. Puisque nous disposons d’un laboratoire étroit, il était inconcevable d’y regrouper l’équipe sans mettre les employés à risque. J’ai donc formé deux équipes qui se relaient tous les jours à 14 h. Jamais ces deux équipes ne se croisent. L’équipe qui termine son quart de travail désinfecte les espaces pendant que l’autre attend à l’entrée de la pharmacie. Lorsque cette dernière arrive au laboratoire, elle désinfecte à nouveau les lieux afin de prendre toutes les précautions nécessaires.
Comme pharmacienne et comme propriétaire, je suis responsable à la fois de la sécurité de mes patients et de mes employés, ce qui occasionne son lot de stress dans une situation aussi nouvelle et extraordinaire que celle que nous vivons. Malgré tout, leur reconnaissance envers les efforts déployés pour leur santé me permet de faire le plein d’énergie et de continuer à faire mon travail du mieux que je le peux.
—Mélissa Béland
Pharmacienne propriétaire
Lévis, Québec
I currently work part-time as a pharmacist at the Burlington Family Health Team and have long believed that pharmacists, regardless of where we work, need to work together. I continue to support collaborative efforts with hospital and community pharmacists in Burlington and I have them all listed in a database, including address, phone, fax and email for the pharmacy manager. So when issues arise in Burlington relevant to them, I can easily contact them.
I recently contacted all those in my database to determine their current hours with the COVID-19 situation, whether they offer delivery and dispense methadone and/or Suboxone. I shared the updated list (without email addresses) with all those in the database, as well as with about 200 Burlington physicians. When a community pharmacist asked why Joseph Brant Hospital was still giving hardcopy prescriptions for discharged patients, I suggested to my CEO that she share the list with the hospital as well.
Since we received such positive feedback, I recently prepared a similar list for about 360 community pharmacies in the Hamilton area. I was pleasantly surprised that most are providing delivery and/or curbside pickup and some have special hours for seniors. A large percentage dispenses methadone and/or Suboxone and they planned to be open for Good Friday and/or Easter Sunday to support those patients. I shared the list with Hamilton Health Sciences, St. Joseph’s Health Care, Hamilton Academy of Medicine, Hamilton Family Health Team and the Hamilton District Pharmacists Associations, who put it on their website.
Since I already have email addresses for the Burlington pharmacies, I have continued to forward relevant COVID-related resources that they might not otherwise be aware of, because we are all in this together.
—Mary Nelson, BScPhm, RPh
Clinical Pharmacist
Burlington Family Health Team
From one town to another, my job as pharmacist coach has taken me all over Ontario. The COVID-19 pandemic was a turning point for all of us to reorganize our priorities to the most important goal of providing Canadians with their regular medication supply.
I changed my role quickly to offer my services as a pharmacist in one of our stores, an hour and a half away from where I live. It is the only pharmacy in town with a drive-through, around-the-clock deliveries and hundreds of patients on compliance packs.
The pandemic has forced many physicians’ offices in town to close and patients found that pharmacies were their only sanctuary for their health needs. More patients started to call us—many were elderly, fearful and confused, seeking reassurance and answers to their questions. The staff was fearful too, rubbing alcohol was getting scarcer, protective gear was always on back order. The news about people in neighbouring businesses getting infected left everyone concerned. Reassuring staff and regularly reminding them to wash hands and keep their 6-foot distance among each other was a continuous challenge.
The store was very busy and pharmacy workstations needed to be reorganized. Staff were asked not to share phones, pens or computers as much as possible, and every station was cleaned on an hourly basis. Every box or bag was sprayed before it was brought into the pharmacy. Gloves were available to everyone, a Plexiglass shield was installed around the front counter of the pharmacy and finally face shields arrived to make our staff feel a little safer. Drive-through was now a deciding factor for patients in using our pharmacy. The regular delivery cycle was essential to make patients feel that they could have their medications without disturbing their quarantine rules or imposing on neighbours.
Pharmacists and pharmacy staff have often gone unrecognized—it is times like this that show that pharmacists are truly the most accessible health care professionals.
—Anas Bahnassi, PhD, RPh
Foundational Reset Ambassador
Rexall Pharmacy Group Ltd.
As the pharmacist running the Geriatric Clinic for Parkinson’s with a Parkinson’s specialist at the North York General, I often receive calls relating to patients’ progressive Parkinson’s disease (PD) symptoms. However, during COVID-19, physicians have not been as easily accessible, and I began to receive calls for any urgent medical conditions. One late evening, I received a call from a patient’s son. He was not able to reach their family physician. The patient’s blood pressure had been consistently over 170/90 for the last few days. This patient was known to our clinic with a history of stroke and PD for several years. The son called me while waiting to be seen at the emergency department (ED). He reported hundreds of patients were ahead of them. I quickly reviewed his current medications and contacted our clinic physician to prescribe an antihypertensive medication. Just before the patient’s pharmacy closed for the day, I was able to pass the verbal prescription to his pharmacist, who kindly offered to deliver the medication that evening. The patient’s son was so relieved that they didn’t need to stay in the hospital any longer during the COVID pandemic! He was thankful for the patient-centred care that our clinic and the patient’s community pharmacist collaboratively provided.
Since elderly patients are the most vulnerable, it’s critical to prevent them from any unnecessary ED visit. Due to social distancing, many patients’ adult children were instructed not to visit them. Our clinic strived to continue our service by using virtual meetings. Although most patients/caregivers have mobile phones, they are not computer savvy enough to download the required app. Coaching them to navigate the system takes a lot of patience, but they are so amazed when we finally see each other on the screen. By visually assessing a patient’s tremor and mobility, we are able to prevent falls or other PD-related complications.
—Greta Mah, BScPhm, RPh, BCGP
Clinical Pharmacist, Geriatric Clinic for Parkinson’s
North York General Hospital, Toronto, Ontario
My frontline is a bit atypical from that of many of my pharmacist colleagues. I work as the study manager for a not-for-profit cardiac research foundation in a small Canadian city. Our research team conducts local investigator-initiated research, participates in national registries and has been a site for many international research studies such as DECLARE, COMPLETE and THEMIS.
My favourite job perk is interacting with study participants, but this was halted on March 15, when the research team made the decision to stop all in-person study-related activities. This was reinforced by our Research Ethics Board directive on March 17 to all research teams in our health region. The embargo on in-person meetings means that we have suspended all recruitment into current studies, and all protocol-directed follow-up encounters are to be held via telephone/virtually only until the time that pandemic distancing mandates have been lifted.
Another issue is that many of our study participants require investigational product (IP) dispenses over the next few months. Our current IP (including apixaban/placebo, colchicine/placebo, spironolactone/placebo) is housed in a secured study office in a critical care area of one of our hospitals. As a nonessential health care professional who is a contract employee of the not-for-profit research team and not an employee of our health region, it was anticipated that I might be denied access to the area that normally houses our office and the IP (which is directly under my supervision rather than dispensed out of the hospital pharmacy). Health Canada directs that IP must be securely held and storage conditions must protect from loss and temperature excursion. The decision was thus made that I would bring the IP home with me, where I can be assured it is safe from loss and where I can monitor for temperature excursions on a daily basis.
Delivery of the IP to the patient presented another problem—how to get the investigational product from the research staff to the participant, which in most studies must be done in person with hand-to-hand transfer? Our team decided that we would personally deliver to participants’ homes or other prearranged location so that the transfer could occur safely and the study team could watch the study participant retrieve the medication. Luckily, our current study participants live in or very close to our city, which has not always been the norm.
These days, I am madly putting together ethics board applications for a flurry of COVID-19-related cardiac studies. It has been remarkable to see researchers from across North America coming together in effective and efficient manners to address COVID-19 management questions, often with limited or no funding options. Collaboration, cooperation and dedication have allowed this to happen and will likely be the common themes in many pharmacy and health care–related frontline stories throughout this pandemic. Let us hope these themes continue long after the pandemic is over.
—Kendra Townsend, BSP, CDE
Prairie Vascular Research Network
Regina, Saskatchewan
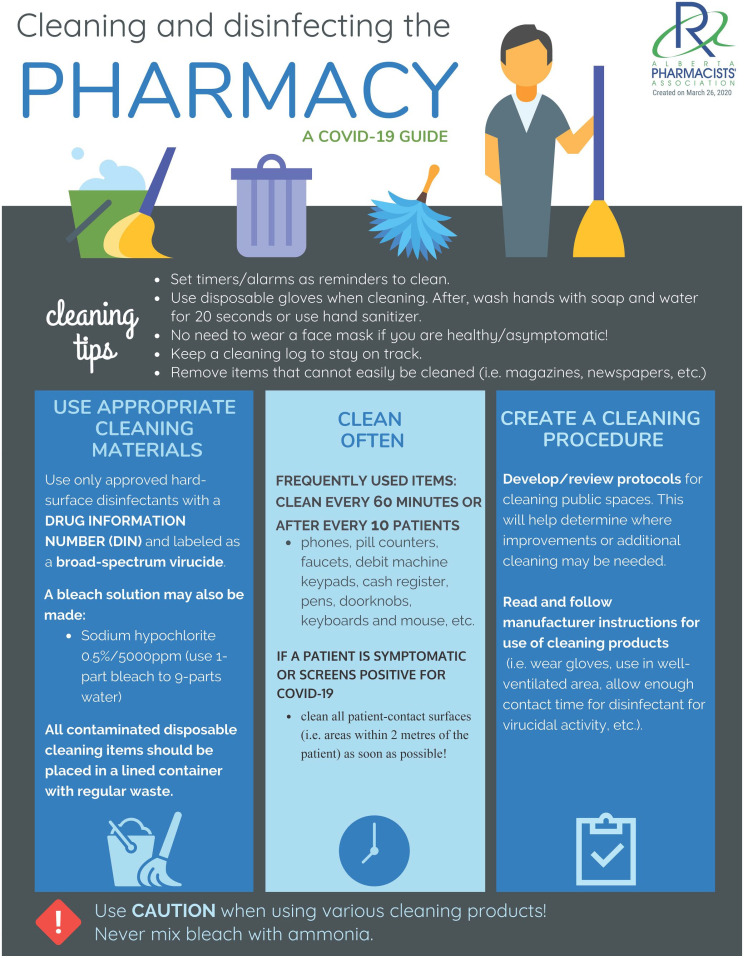
As COVID-19 began its insidious journey throughout the world, the Alberta Pharmacists’ Association (RxA) began receiving questions from community pharmacists such as, “How do I stay safe?” “How do I manage the drug supply?” “How do I clean my pharmacy?” and comments like, “I am really stressed.” Like other health care professionals, pharmacists wanted us to hear, protect, prepare, support and care for them. This is how we responded:
To ensure pharmacists’ concerns were heard, we
Ensured RxA staff were available to listen to member concerns
Were active on social media
Gathered our Leadership Cohort to support communication efforts
Actively monitored COVID-19-related publications and developed a resource webpage
Worked with CPhA to gain a national perspective
Developed a Member2Member webpage to enable members to share with each other
To protect pharmacists, we actively lobbied government for and delivered on
Personal protective equipment for pharmacists and their team
Payment for COVID-19 telephone screening of patients
Thirty-day dispensing with fiscal support for seniors
To prepare pharmacists with credible and current information, we
Switched to daily information updates sent to Alberta pharmacies
Developed posters and infographics
Shared information on social media
To ensure pharmacists were supported, we
Reminded members about the RxA Member Wellness Program
Provided information on mental health supports
Developed an infographic
Distributed information about daycare access
To show we cared about pharmacists, we
Developed a list of available government supports
In response to RxA’s efforts, we have received abundant positive feedback. Providing tangible results in a timely fashion is challenging, but we worked hard to get results. We have been proud to represent and support our pharmacists.
—Margaret Wing, BScPharm, RPh, ICDD
Chief Executive Officer
—Heather Scarlett-Ferguson, BSP, RPh, MEd, EdD
Director, Professional Development
Alberta Pharmacists’ Association
Nova Scotia Health Authority (NSHA) is an integrated and diverse (urban and rural) health care system, providing services across the province. Prior to the COVID-19 pandemic, a provincial clinical pharmacy leadership structure to support frontline health care providers did not exist. Varying resources, practices, priorities and geographic challenges impact clinical support for frontline health care providers across NSHA. The COVID-19 pandemic magnified the urgent need for clearly defined, unified and agile clinical pharmacy leadership.
Six clinical pharmacy coordinators from across NSHA, with clinical expertise in critical care, infectious diseases and antimicrobial stewardship, rapidly formed the NSHA COVID-19 Clinical Pharmacy Working Group to provide clinical support for frontline staff across NSHA. This support includes advising on and creating evidence-based COVID-19 clinical resources such as guidance documents, tools, orders sets, educational sessions and materials. Resources created by the working group are used by health care providers across the province. The mission of this working group is to support safe and effective patient care across all transitions of care, including disposition back to the community.
NSHA pharmacy management states they are “extremely fortunate in NSHA to have the pharmacy experts in our organization come together as a highly functioning and organized group to support all of our patients and staff. Their work and guidance has rapidly provided extremely valuable and practical resources for clinicians across the province. They have also developed clinical networks which can be leveraged post-COVID.”
As members of the working group, we feel we are part of a collaborative team effort and feel united with frontline pharmacy team members across the province. Working with passionate individuals towards similar goals makes us feel impactful and in a position to help the residents of Nova Scotia through this pandemic.
—Kim Abbass, RPh, BSc(Pharm), PharmD; Sarah Burgess, RPh, BSc(Pharm), ACPR, PharmD; Lauren Hutton, RPh, BSc(Pharm), ACPR, PharmD; Andrea Kent, RPh, BSc(Pharm), PharmD; Meghan MacKenzie, RPh, BSc(Pharm), ACPR, PharmD; on behalf of the COVID-19 Clinical Pharmacy Working Group
Pharmacy Department, Nova Scotia Health Authority