Abstract
Background:
In genetics research, it has become common practice for researchers to consider returning genetic information to participants who wish to receive it. Research participants in lower resource settings may have barriers or competing interests that reduce the benefit or relevance of such information. Thus, the decision to return genetic information in these settings may involve special considerations of participants’ interests and preferences. In this project, our goal was to assess Bangladeshi research participants’ attitudes towards receiving information regarding genetic susceptibility to the effects of arsenic in drinking water, a serious environmental health concern in Bangladesh and other countries.
Methods:
We administered a short questionnaire to 200 individuals participating in the Health Effects of Arsenic Longitudinal Study. Associations between survey responses and participant characteristics were estimated using logistic regression.
Results:
100% of our participants were interested in receiving information regarding their genetic susceptibility to arsenic toxicities, and 91% indicated that being at increased genetic risk would motivate them to make efforts to reduce their exposure. Lower levels of education showed evidence of association with less concern regarding the health effects of arsenic and lower levels of motivation to reduce exposure in response to genetic information.
Conclusions:
Research participants in this low resource setting appeared interested in receiving information on their genetic susceptibility to arsenic toxicity and motivated to reduce exposure in response to such information. Additional research is needed to understand how best to communicate genetic information in this population and assess the impact of such information individuals’ behaviors and health.
Keywords: Arsenic, Environmental risk factors, ethics of genetic research, return of genetic results
Introduction
Returning genetic results to research participants has become a topic of debate in recent years [1–3] due in part to increasing availability of whole-genome genotyping and sequencing data and an improved understanding of genetic causes of disease. Whole-genome sequencing data can contain information relevant to the health care of a research participant, although not necessarily relevant to the research questions; this has been termed “incidental findings”. There is a growing consensus that researchers should offer to return such “incidental findings” to research participants, [4]. Groups such as the American College of Medical Genetics (ACMG) have provided recommendations regarding which genes and variants should be considered “medically relevant” and offered to participants as a part of incidental findings [5].
In addition, there is a trend among researchers and funders to make research participants’ genetic data freely available to them should they want access to it [1–5]. These types of data could be specific research results (i.e., the specific genetic variant(s) under study in meeting a research project’s aims) [6] or genome-wide measures of genetic variation (potentially communicated as polygenic estimates of risk for specific diseases or as an interpretation of participants’ genetic ancestry). It has been suggested that providing participants their genetic results is one way researchers can demonstrate respect for participants and enhance participants’ engagement in research [3]. However, returning results could be harmful if participants misinterpret the significance of the information received. Returning results may also overburden researchers with limited resources [3,7–9].
The debate surrounding returning genetic information has primarily occurred among research communities in North America, Europe, and high-income countries, as the majority of human genetics research occurs in these settings. However, there are emerging initiatives to facilitate genomics research in lower resource settings, including the NIH-funded H3Africa (Human Heredity and Health in Africa) program [10]. Research participants in lower resource settings may have additional threats, barriers, and/or competing interests that may reduce the benefit or relevance of returning genomic results [11] (e.g., less formal education, poverty, malnourishment, contaminated water, violence). Thus, the decision to return (or not return) genetic information to participants in these settings may involve special considerations not relevant in high resource settings. Additional research is needed in lower-resource settings to better understand participants’ attitudes towards receiving genetic results and how best to return them in order to best serve participants’ interests and avert potential harms.
In this study, surveyed participants’ attitudes towards returning of genetic results in Bangladesh. More specifically, we collected data on attitudes towards receiving information regarding genetic susceptibility to arsenic toxicity, as these participants reside in a rural area where a substantial fraction of drinking wells are naturally contaminated with arsenic, a known human carcinogen and toxicant[12]. Thus, these participants are unique both in terms of the research setting and their environmental exposures [13]. Collecting this data is timely, as we now know of inherited genetic variation that impacts arsenic metabolism efficiency, as well as risk of arsenic toxicity [13] and arsenic-associated diseases [14–20]. Thus, researchers studying arsenic-exposed populations (several of which would be considered “low resource”) have the opportunity to consider returning genetic data to participants that is highly relevant to their susceptibility to the effects of exposure.
Methods
We administered a questionnaire to 200 individuals participating in The Health Effects of Arsenic Longitudinal Study (HEALS) [21] in Araihazar, Bangladesh, a rural area with high exposure to arsenic through naturally-contaminated groundwater [13]. HEALS was initiated in 2000–2002 with the recruitment of ~12,000 healthy individuals (ages 18–75 years), with additional recruitment in 2006–2014 resulting in cohort of >20,000 individuals. At recruitment, participants were residents of Araihazar for >5 years and primarily consumed water from a local well. A multifaceted arsenic mitigation program was implemented after baseline (2000–2002) [22]. Interventions included person-to-person reporting of well arsenic levels and health education, labeling of wells to indicate arsenic concentration, village-level health education, and installation of deep, low-arsenic wells in villages with high exposure. Currently, the participants’ communities label wells to reflect arsenic concentration, enabling avoidance of high arsenic wells, the most effective method of reducing exposure in this community [23].
A questionnaire to assess attitudes towards receiving information on genetic susceptibly to arsenic toxicity was developed by Drs. Pierce, Ahsan, and Eunus (Supplementary File 1), consisting of seven questions designed to gauge concern about the arsenic, interest in receiving information on genetic susceptibility to arsenic toxicity, and expected behavioral responses to receiving such information. All questions were translated into Bengali by Dr. Eunus (Supplementary File 2). The questionnaire included text intended to orient the respondent to the idea that inherited genetic variation can impact susceptibility to arsenic. This was done to attempt to increase participants’ understanding of genetic susceptibility, as this community has low levels of formal education (Table 1). The questionnaire was administered by Dr. Eunus and his staff to 200 participants visiting the HEALS health clinic in Araihazar (July-October 2014). 67 of the 200 joined HEALS at the original baseline visit (2000–2002), while 129 were recruited during expansion efforts (2006–2014).
Table 1.
Descriptive Characteristics of Survey Participants (n=200, Araihazar, Bangladesh)
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 43 (21.5%) |
| Female | 157 (78.5%) |
| Age at interview, mean (years) | 44.3 |
| Age at Categories | |
| 20–29 years | 20 (10%) |
| 30–39 years | 54 (27%) |
| 40–49 years | 53 (26.5) |
| 50–59 years | 54 (27%) |
| 60–69 years | 17 (8.5%) |
| 70–79 years | 2 (1%) |
| Education | |
| 0 years | 103 (51.5%) |
| > 0 years | 97 (48.5%) |
| Urine Arsenic (μg/g creatinine) | |
| Mean | 100.3 |
| 25th percentile | 41.5 |
| Median | 70.5 |
| 75th percentile | 139.0 |
Urine samples were collected at recruitment and follow-ups visits. Arsenic concentrations were measured using graphite furnace atomic absorption [Perkin-Elmer Analyst 600 graphite furnace system] (limit of detection =5 μg/L) at the Columbia University Trace Metal Core Laboratory [24,25]. For some newly-recruited participants, follow-up arsenic measurements are not yet available. For this work, we used individuals’ most recent urine arsenic measurement as a measure of exposure (n=196).
Associations between survey responses and participant characteristics were estimated using logistic regression, adjusting for sex, age, and education status (categorized as 0 versus >0 years of formal education). Analyses were conducted using R (version 3.5.2).
Results
Characteristics of our 200 respondents are shown in Table 1. The majority of participants were female (79%) and over half (52%) had no formal education. Responses to our survey are described in Table 2. Most notably, 100% of our participants reported being interested in receiving genetic information regarding their susceptibility to arsenic toxicities (Q5). Furthermore, 91% of respondents indicated that they would be motivated to change their family’s water source in order to reduce their family’s exposure if their genes indicated they (or family members) were at elevated risk for arsenic toxicities (Q8). All but one respondent indicated that they would be comfortable disclosing to family members that they were at elevated risk (Q9), while 30% indicated they would keep this information confidential from non-family members (Q10).
Table 2.
Survey Question Descriptions
| Survey Questions | Yes | No | Don’t know |
|---|---|---|---|
| Q4. Are you concerned about the health effects of arsenic-contaminated drinking water? | 173 (86.5%) | 27 (13.5%) | NA |
| Q5. If your genes could provide you information on your susceptibility to arsenic toxicities, would you be interested to receive this information? | 200 (100%) | 0 (0%) | NA |
| Q6. Is your primary water source believed to be “arsenic free”? | 117 (58.5%) | 66 (33%) | 17 (8.5%) |
| Q7. At this point in time, is it possible for you to take steps to further reduce you and/or your family’s exposure to arsenic in water used for drinking and cooking? | 98 (49%) | 102 (51%) | NA |
| Q8. If your genes indicated you (or your family members) were at elevated risk for arsenic toxicities, would this information motivate you to alter your family’s water sources to reduce your family’s arsenic exposure? | 182 (91%) | 18 (9%) | NA |
| Q9. If your genes indicated that you were at elevated risk for arsenic toxicity, would you be comfortable disclosing this information with others in your family? | 199 (99.5%) | 1 (0.5%) | NA |
| Q10. If your genes indicated that you were at elevated risk for arsenic toxicity, would you want to keep this information confidential from non-family members? | 59 (29.5%) | 141 (70.5%) | NA |
To validate our respondent’s knowledge regarding levels of arsenic in their drinking water, we stratified participants by median urine arsenic concentration. Using logistic regression, we observed that individuals who reported an “arsenic-free” primary water source were more likely to have lower arsenic concentrations in urine (P<0.001, Table 3), as expected.
Table 3.
Stratified analysis of Survey Questions by Creatinine adjusted Urine Arsenic
| Creatinine-adjusted arsenic in urine (n=196) | P-Value | ||
|---|---|---|---|
| Survey Questions | ≤ 143 μg/g | > 143 μg/g | |
| Q6. Is your primary water source believed to be “arsenic free”? | |||
| Yes | 75 (75.8) | 41 (42.3) | < 0.001 |
| No | 18 (18.2) | 45 (46.4) | |
| Don’t Know | 6 (6.1) | 11 (11.3) | |
We then sought to determine if concern regarding aresenic (Q4) was related to the perceived impact of genetic information on motivation to reduce exposure (Q8). Concern regarding arsenic toxicities did not show a clear association with individuals’ motivation to act on genetic information (OR=1.14; CI:0.24–3.98; P=0.84); however our power to estimate this association was limited due to the small number of individuals answering “no” to Q4 and Q8. However, it remains possible that particpants’ self-reported concern regarding arsenic may be unrelated to their reported intention to act on genetic information.
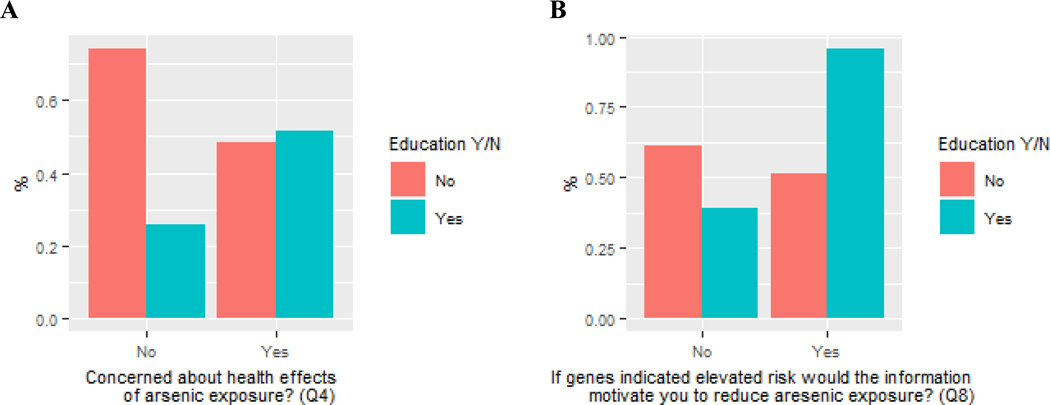
To determine if motivation to change behavior based on genetic information was related to education, we tested the association of education status with 1) concern regarding the health effects arsenic (Q4) and 2) the perceived impact of genetic information on motivation to reduce exposure (Q8). Individuals with lower education were less likely to be concerned about the effects of arsenic (Q4) (Figure 1; OR=1.12; CI: 1.02–1.23; P=0.025). Education status showed a similar association with the perceived impact of genetic information on motivation to reduce expsoure (Q8), but statistical power was limited due to the few people who answered “no” to Q8 (Figure 1; OR=1.29; CI: 0.46–3.82; P=0.62)
Figure 1. Attitudes towards arsenic-related risks and genetic susceptibility stratified by education status.
Panel A shows the percent of participants concern about the health effects of arsenic exposure (Q4), stratified by education status. Panel B shows the percent of individuals motivated to reduce the exposure to arsenic in response to learning they are genetically susceptibility, stratified by education status.
Discussion
In this survey of Bangladeshi research participants, we assessed attitudes towards receiving information regarding individuals’ genetic susceptibility to the effects of arsenic, an exposure of concern in their community. Our most striking observation is that 100% of respondents were interested in receiving such information, demonstrating a clear interest in access to personal genetic information in this community.
A substantial fraction of participants (13.5%) were not concerned about the health effects of arsenic (Q4). However, these same participants reported being interested in receiving information on genetic susceptibility to arsenic toxicities (Q5), and the response to Q5 was not associated with the response to concern regarding arsenic (Q4). This finding suggests that concern regarding arsenic and interest in receiving information regarding their genetic susceptibility are perceived somewhat differently. This finding also speaks to the possibility that returning genetic information could modify individuals’ concern regarding arsenic exposure, with a “return of results” intervention among highly susceptible individuals potentially increasing their motivation to reduce exposure.
Participants with higher levels of formal education were more likely to be concerned about arsenic (Q4) and appeared more motivated to reduce exposure based on increased genetic risk (Q8). This suggests that education may impact the effectiveness of interventions aimed at reducing exposure (including those invovling returning genetic results) and should be considered when designing such intervention studies.
Within HEALS, we have the opportunity to study the impact of returning information on genetic susceptibility to arsenic toxicity. Using genetic variation in the AS3MT (arsenic methyltransferase ) and FTCD (formiminotransferase cyclodeaminase) regions known to impact arsenic metabolism efficiency and arsenic-induced skin lesions risk [13,26,27], we can identify participants at high risk for arsenic toxicities. In the context of an exposure reduction intervention (i.e., Chen et al [22] and Huhmann et al [28]), informing high-risk individuals of their increased genetic risk may provide additional motivation to change behavior and reduce exposure, potentially increasing the effectiveness of an intervention among those most susceptible to the effects of exposure.
There are potential risks when returning genetic results to participants (such as misinterpretation of results, stigmatization, or psychosocial stress), and additional research is needed to understand how best to communicate genetic information in this population, in order to minimize the risk of potential harms. Despite these concerns, the practice of returning results is becoming more widely accepted, including plans within the National Institutes of Health’s (NIH) All of Us cohort to have genetic results responsibly returned to participants who are interested in receiving them.
There are two primary arguments motivating the return of genetic results to research participants, both of which are potentially relevant to our participants. The first is that participants have a right to genetic data (should they want it), and the second is that researchers have an obligation to return results that are important to participants’ health and potentially actionable. In the context of genetic susceptibility to the effects of environmental exposures, returning genetic information could be viewed as a component of precision public health, a term defined as “providing the right intervention at the right time to the right population” [29]. In this way, we could target high-risk individuals using genetic information, and provide this information to participants as a piece of a larger public health effort in this population.
HEALS participants surveyed in this study are individuals who visited the HEALS clinic, a sample which may not be representative of the larger cohort. Regarding participants’ understanding of genetic concepts, research staff attempted to convey these concepts with the help of the explanatory text on the survey, but we did not assess their understanding.
Conclusion
In conclusion, our results indicate that research participants in this rural, low resource setting are interested in receiving information on their genetic susceptibility to the effects of arsenic exposure. The vast majority of participants report being motivated to reduce their exposure if they learned they were at elevated genetic risk for arsenic toxicities. Similarly, past studies conducted in higher-resource settings have demonstrated that the public’s attitude toward receiving genetic information is generally positive, across a range of different diseases [30–33]. Additional research is needed to understand how best to communicate genetic information in this population and assess the impact of such information individuals’ behaviors, arsenic exposure status, and psychosocial health. The questions of if and how genetic information should be returned in low-resource settings are likely to require research to understand population-specific needs, preferences, and barriers related to receiving, understanding, and using such information.
Supplementary Material
Acknowledgement
The authors would like to thank all study participants and staff who have contributed to HEALS.
Statement of Ethics
This research was approved by the Institutional Review Board of the University of Chicago (IRB16-1236). Verbal informed consent was obtained from all participants.
Funding Sources
This work was supported by National Institutes of Health grants R01 ES023834 (to B.L.P.), R35 ES028379 (to B.L.P.), R01 ES020506 (to B.L.P.), P42ES010349 (to J.H.G.), R01 CA107431 (to H.A.), P30 ES027792 (to H.A. and Gail Prins), R24 ES028532 (to H.A.) and R24 TW009555 (to H.A.). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Disclosure Statement
The authors declare that no conflict of interest, financial or other, exists.
References
- [1].Alessi SA. The Return of Results in Genetic Testing: Who Owes What to Whom, When, and Why? vol. 64 2013. [Google Scholar]
- [2].Jarvik GP, Amendola LM, Berg JS, Brothers K, Clayton EW, Chung W, et al. Return of Genomic Results to Research Participants: The Floor, the Ceiling, and the Choices In Between 2014;12:14. doi: 10.1016/j.ajhg.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Heaney C, Tindall G, Lucas J, Haga SB. Researcher Practices on Returning Genetic Research Results n.d. doi: 10.1089/gtmb.2010.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sullivan HK, Berkman BE. Incidental Findings in Low-Resource Settings. Hastings Cent Rep 2018;48:20–8. doi: 10.1002/hast.851. [DOI] [PubMed] [Google Scholar]
- [5].Knoppers BM, Zawati MH, Sénécal K. Return of genetic testing results in the era of whole-genome sequencing. Nat Rev Genet 2015;16:553–9. doi: 10.1038/nrg3960. [DOI] [PubMed] [Google Scholar]
- [6].Wolf SM. Return of Individual Research Results and Incidental Findings: Facing the Challenges of Translational Science 2013. doi: 10.1146/annurev-genom-091212-153506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].MacNeil SD, Fernandez C V. Offering results to research participants. BMJ 2006;332:188–9. doi: 10.1136/bmj.332.7535.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Bunin GR, Kazak AE, Mitelman O. Informing subjects of epidemiologic study results. Children’s Cancer Group. Pediatrics 1996;97:486–91. [PubMed] [Google Scholar]
- [9].Shalowitz DI, Miller FG. Disclosing Individual Results of Clinical Research: Implications of Respect for Participants. JAMA 2005;294:737. doi: 10.1001/jama.294.6.737. [DOI] [PubMed] [Google Scholar]
- [10].Friedrich MJ. Ethical Guidelines for Genomic Research in AfricaEthical Guidelines for Genomic Research in AfricaGlobal Health. JAMA 2018;319:2371. doi: 10.1001/jama.2018.7241. [DOI] [PubMed] [Google Scholar]
- [11].Mackay D. Returning Incidental Findings in Low-Resource Settings: A Case of Rescue? Hastings Cent Rep 2018;48:28–30. doi: 10.1002/hast.852. [DOI] [PubMed] [Google Scholar]
- [12].Smith AH, Lingas EO, Rahman M. Contamination of drinking-water by arsenic in Bangladesh: a public health emergency. n.d. [PMC free article] [PubMed] [Google Scholar]
- [13].Pierce BL, Kibriya MG, Tong L, Argos JF. Genome-Wide Association Study Identifies Chromosome 10q24.32 Variants Associated with Arsenic Metabolism and Toxicity Phenotypes in Bangladesh. PLoS Genet 2012;8:1002522. doi: 10.1371/journal.pgen.1002522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Agusa T, Fujihara J, Takeshita H, Iwata H. Individual variations in inorganic arsenic metabolism associated with AS3MT genetic polymorphisms. Int J Mol Sci 2011;12:2351–82. doi: 10.3390/ijms12042351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hsieh R-L, Su C-T, Shiue H-S, Chen W-J, Huang S-R, Lin Y-C, et al. Relation of polymorphism of arsenic metabolism genes to arsenic methylation capacity and developmental delay in preschool children in Taiwan. Toxicol Appl Pharmacol 2017;321:37–47. doi: 10.1016/J.TAAP.2017.02.016. [DOI] [PubMed] [Google Scholar]
- [16].de la Rosa R, Steinmaus C, Akers NK, Conde L, Ferreccio C, Kalman D, et al. Associations between arsenic (+3 oxidation state) methyltransferase ( AS3MT ) and N-6 adenine-specific DNA methyltransferase 1 ( N6AMT1 ) polymorphisms, arsenic metabolism, and cancer risk in a chilean population. Environ Mol Mutagen 2017;58:411–22. doi: 10.1002/em.22104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].McClintock TR, Chen Y, Bundschuh J, Oliver JT, Navoni J, Olmos V, et al. Arsenic exposure in Latin America: Biomarkers, risk assessments and related health effects. Sci Total Environ 2012;429:76–91. doi: 10.1016/J.SCITOTENV.2011.08.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Antonelli R, Shao K, Thomas DJ, Sams R, Cowden J. AS3MT, GSTO, and PNP polymorphisms: Impact on arsenic methylation and implications for disease susceptibility. Environ Res 2014;132:156–67. doi: 10.1016/j.envres.2014.03.012. [DOI] [PubMed] [Google Scholar]
- [19].Gong G, O’Bryant SE. Low-level arsenic exposure, AS3MT gene polymorphism and cardiovascular diseases in rural Texas counties. Environ Res 2012;113:52–7. doi: 10.1016/J.ENVRES.2012.01.003. [DOI] [PubMed] [Google Scholar]
- [20].Chen X, Guo X, He P, Nie J, Yan X, Zhu J, et al. Interactive Influence of N6AMT1 and As3MT Genetic Variations on Arsenic Metabolism in the Population of Inner Mongolia, China. Toxicol Sci 2017;155:124–34. doi: 10.1093/toxsci/kfw181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ahsan H, Chen Y, Parvez F, Argos M, Hussain AI, Momotaj H, et al. Health Effects of Arsenic Longitudinal Study (HEALS): Description of a multidisciplinary epidemiologic investigation. J Expo Sci Environ Epidemiol 2006;16:191–205. doi: 10.1038/sj.jea.7500449. [DOI] [PubMed] [Google Scholar]
- [22].Chen Y, van Geen A, Graziano JH, Pfaff A, Madajewicz M, Parvez F, et al. Reduction in urinary arsenic levels in response to arsenic mitigation efforts in Araihazar, Bangladesh. Environ Health Perspect 2007;115:917–23. doi: 10.1289/ehp.9833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Jamil NB, Feng H, Ahmed KM, Choudhury I, Barnwal P, van Geen A. Effectiveness of Different Approaches to Arsenic Mitigation over 18 Years in Araihazar, Bangladesh: Implications for National Policy. Environ Sci Technol 2019:acs.est.9b01375. doi: 10.1021/acs.est.9b01375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jansen RJ, Argos M, Tong L, Li J, Rakibuz-Zaman M, Islam T, et al. Determinants and consequences of arsenic metabolism efficiency among 4,794 individuals: demographics, lifestyle, genetics, and toxicity n.d. doi: 10.1158/1055-9965.EPI-15-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nixon DE, Mussmann G V, Eckdahl SJ, Moyer’ TP. Total Arsenicin Urine: Palladium-Persulfatevs Nickel as a Matrix Modifierfor Graphite FurnaceAtomicAbsorptionSpectrophotometry. vol. 37 1991. [Google Scholar]
- [26].Pierce BL, Tong L, Dean S, Argos M, Jasmine F, Rakibuz-Zaman M, et al. A missense variant in FTCD is associated with arsenic metabolism and toxicity phenotypes in Bangladesh. PLOS Genet 2019;15:e1007984. doi: 10.1371/journal.pgen.1007984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Pierce BL, Tong L, Argos M, Gao J, Jasmine F, Roy S, et al. Arsenic metabolism efficiency has a causal role in arsenic toxicity: Mendelian randomization and gene-environment interaction. Int J Epidemiol 2013;42:1862–72. doi: 10.1093/ije/dyt182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Huhmann BL, Harvey CF, Navas-Acien A, Graziano J, Parvez F, Chen Y, et al. Changes in arsenic exposure in Araihazar, Bangladesh from 2001 through 2015 following a blanket well testing and education campaign. Environ Int 2019;125:82–9. doi: 10.1016/J.ENVINT.2019.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Khoury MJ, Iademarco MF, Riley WT. Precision Public Health for the Era of Precision Medicine. Am J Prev Med 2016;50:398–401. doi: 10.1016/J.AMEPRE.2015.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Haga SB, Barry WT, Mills R, Ginsburg GS, Svetkey L, Sullivan J, et al. Public Knowledge of and Attitudes Toward Genetics and Genetic Testing n.d. doi: 10.1089/gtmb.2012.0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Morren M, Rijken M, Baanders AN, Bensing J. Perceived genetic knowledge, attitudes towards genetic testing, and the relationship between these among patients with a chronic disease. Patient Educ Couns 2007;65:197–204. doi: 10.1016/j.pec.2006.07.005. [DOI] [PubMed] [Google Scholar]
- [32].Middleton A, Morley KI, Bragin E, Firth H V, Hurles ME, Wright CF, et al. Attitudes of nearly 7000 health professionals, genomic researchers and publics toward the return of incidental results from sequencing research. Eur J Hum Genet 2016;24:21–9. doi: 10.1038/ejhg.2015.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Yu J-H, Crouch J, Jamal SM, Tabor HK, Bamshad MJ. Attitudes of African Americans Toward Return of Results From Exome and Whole Genome Sequencing. Am J Med Genet Part A 2013;161:1064–72. doi: 10.1002/ajmg.a.35914. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.