Using national linked birth and infant death records, we find county-level socioeconomic disadvantage, and not health care, best explains higher infant mortality rates in rural counties.
Abstract
BACKGROUND AND OBJECTIVES:
Rural counties have the highest infant mortality rates across the United States when compared with rates in more urban counties. We use a social-ecological framework to explain infant mortality disparities across the rural-urban continuum.
METHODS:
We created a cohort of all births in the United States linked to infant death records for 2014 to 2016. Records were linked to county-level data from the Area Health Resources File and the American Community Survey and classified using the National Center for Health Statistics Urban-Rural Classification Scheme. Using multilevel generalized linear models, we investigated the association of infant mortality with county urban-rural classification, considering county health system resources and measures of socioeconomic advantage, net of individual-level characteristics, and controlling for US region and county centroid.
RESULTS:
Infant mortality rates were highest in noncore (odds ratio [OR] = 1.32, 95% confidence interval [CI]: 1.26–1.39) and micropolitan counties (OR = 1.26, 95% CI: 1.20–1.32) when compared with large metropolitan fringe counties, controlling for geospatial measures. Inclusion of county health system characteristics did little to attenuate the greater odds of infant mortality in rural counties. Instead, a composite measure of county-level socioeconomic advantage was highly protective (adjusted OR = 0.84; 95% CI: 0.82–0.86) and eliminated any difference between the micropolitan and noncore counties and the large metropolitan fringe counties.
CONCLUSIONS:
Higher infant mortality rates in rural counties are best explained by their greater socioeconomic disadvantage than more-limited access to health care or the greater prevalence of mothers’ individual health risks.
What’s Known on This Subject:
Infant mortality rates in the United States increase as counties become more rural. This mirrors the “rural mortality penalty” among adults, where those living in rural areas have higher mortality rates at every age than those in more urban settings.
What This Study Adds:
Higher infant mortality rates in rural counties are best explained by their greater socioeconomic disadvantage than more-limited access to health care or the greater prevalence of mothers’ individual health behaviors such as tobacco use.
Infant mortality rates in the United States increase as counties become more rural,1,2 mirroring the “rural mortality penalty” found among adults.3–5 The growing understanding of the importance of “place” as a strong influence on health and mortality is a new dimension in the broad literature on the social determinants of health. In the United States, there is a growing mortality disadvantage among adults living in rural areas that differs by race and type of rural setting.4,6,7 Current research suggests the association of place with health is in part a reflection of high-level structural factors, including access to health care, socioeconomic factors, and racial segregation, rather than due to individual-level characteristics such as health behaviors.7–15 A social-ecological approach provides a framework for considering differences in health of populations that go beyond individual health behaviors and can guide analytic strategies to disentangle these multiple effects.16–19 However, few contemporary studies have considered the importance of these factors on infant mortality across the rural-urban continuum.3,16
In this study, we seek to better explain differences in infant mortality across the rural-urban continuum by moving beyond analyses focused on individual-level characteristics and health behaviors and employing instead the social-ecological framework. Multilevel analyses have proved a robust strategy to examine the relationship between neighborhood factors and health.19 Using national linked birth and infant death records, we conduct a series of multilevel regression models, including geospatial measures, nesting individuals within their resident county, state, and region. With this approach, we provide a detailed examination of the rural infant mortality penalty, focusing on the influence of structural factors, especially county-level health care resources, of relevance to maternal and infant health, as well as socioeconomic advantage, net of individual characteristics.
Methods
Data Sources and Creation of a Cohort File
We conducted a cohort study of all live US births from 2014 to 2016 using 3 sources of data, linked to individual records using federal information processing codes for the mother’s resident county. We used 2014 to 2017 geocoded Period Linked Birth/Infant Death Data Sets (henceforth “birth and death records”) containing county of residence, 2010 to 2014 American Community Survey county-level 5-year samples, and 2010 to 2014 data included in the 2016 to 2017 Area Health Resource File publicly available from the Health Services Resources and Services Administration.20
The birth and death records were provided with permission from the National Association for Public Health Statistics and Information Systems as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. These records link birth and death certificates of each infant dying within the first year after birth. The recent rate of record linkage between birth records and infant death records is excellent. In the 2014 linked file, only 161 of 23 247 infant deaths were unlinked; similarly, in the 2015 linked file, 143 of 23 490 infant deaths were unlinked, and in 2016, only 113 of 23 079 were unlinked.21–23 Each birth record includes the federal information processing code of the mother’s county of residence, which we use to link the birth and death records to the socioeconomic, demographic, and health care access data from the American Community Survey and Area Health Resource File.
We constructed cohort files from the 2014 to 2017 period files for use in this analysis, the most current available at the start of this study, because the last cohort file produced by the National Center for Health Statistics (NCHS) was for 2013 births. We used the DUPLICATE command in Stata to identify infant deaths that occurred in the period file of the subsequent year. Using this process, we identified and replaced all but 3 birth records with the linked birth–infant death files for 2014, 2015, and 2016, thus creating cohort files from the period files.
Study Population
From a total population of 11 912 448 US resident births, we excluded all births occurring before 20 weeks, births occurring after 44 weeks, and births in which the gestational age–specific birth weight is >4 SD from the mean (n = 30 137 cases). Records missing information on resident county (n = 5 counties and n = 497 live births) were also excluded, leaving 11 881 814 observations, 99.7% of the national cohort of US resident births.
The records for 2014 to 2016 reflect a transition to the 2003 Revised Certificate of Live Birth and thus include data from both the revised and the unrevised 1989 versions.24 For the descriptive analysis and the model that included individual-level data, we excluded Connecticut, Rhode Island, and New Jersey (n = 449 739 births) because they had not yet adopted the 2003 Revised Certificate of Live Birth; also Georgia, Virginia, and Hawaii (n = 756 484), which had a substantial fraction of missing data for key covariates, were excluded in some analyses. Cases with missing data (n = 622 939 births) were also excluded from the analyses. After exclusions, 10 109 644 births, or 84.9% of total US live births, were included in the analyses that included individual-level characteristics.
Independent and Dependent Variables
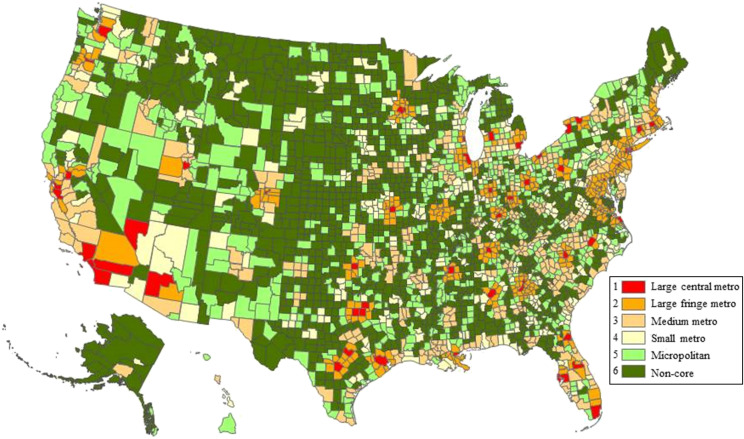
The primary outcome was infant death, within the first year of life overall and during the neonatal (birth to <28 days) and postneonatal periods (28 days to 1 year), the latter assessed among those infants who had survived the neonatal period, as identified in the linked birth and death records. The primary exposure was a county-level measure of rurality and urbanicity of the mother’s resident county by using the NCHS urban-rural classification scheme, which categorizes areas by metropolitan or micropolitan classification, population size, and whether the county is part of the metropolitan core.25 Figure 1 shows a map of the 6 NCHS categories: large central metropolitan, large fringe metropolitan, median metropolitan, small metropolitan, micropolitan, and noncore (rural). In some classification analyses, micropolitan and noncore counties are combined into a single rural category. In these analyses, we chose to consider them as separate groups. To account for regional effects and spatial autocorrelation, we used the 10 US Department of Health and Human Services Regions and also the longitude and latitude of the county geometric centroid from the ArcGIS shapefiles.
FIGURE 1.
NCHS urban-rural classification scheme for counties. Reprinted with permission from Ingram DD, Franco SJ. 2013 National Center for Health Statistics (NCHS) urban-rural classification scheme for counties. Vital Health Stat 2. 2014;(166):4.
We used 2 county-level measures reflecting access to perinatal care: dichotomous variables indicating counties with a hospital that offers obstetrical care and counties with a hospital with a NICU. In addition, we included more general factors related to health care by using dichotomous variables indicating whether a county has been designated as a Health Professional Shortage Area (HPSA) for primary care or had a Federally Qualified Health Center (FQHC) or Rural Health Clinic (RHC) in the county. These measures are included to reflect access to health care before pregnancy and infant and pediatric care.
We estimated county-level socioeconomic status using the “advantage index” developed by Diez Roux et al.26 This index includes 5 components: logged median household income; logged median value of owner-occupied housing units; the percentage of households with interest, dividend, or net rental income; the percentage of workers in management, science, and arts occupations; and the percentage of residents >25 with at least a high school diploma. We calculated this index by summing the z scores for each component as previously described.26 Positive values on the scale indicate socioeconomic advantage, whereas negative values indicate disadvantage.
We also included several county-level measures of population characteristics: fraction of county-level population by race using non-Hispanic (NH) white, NH Black, Hispanic, or NH other. Furthermore, because the birth cohort reflects the characteristics of the population, including local norms of family size, which are known to differ by geography, we included county-level total fertility rate (TFR).27
Last, we examined available individual-level factors known to be associated with infant mortality, including mother’s demographic characteristics, tobacco use, diagnosis of gestational diabetes, diabetes mellitus, chronic hypertension, gestational hypertension and preeclampsia, prepregnancy BMI, method of delivery and whether at a hospital, and whether delivery was performed by a physician. Finally, we also included infant sex and plurality.
Statistical Analysis
We calculated infant mortality rates across the 6 NCHS categories for the 3 years of pooled births as deaths per 1000 live births, considering overall infant mortality as well as neonatal and postneonatal mortality. We conducted a descriptive analysis comparing the county and individual-level characteristics of women across the 6 NCHS categories. Analysis of variance and χ2 tests were used to test the significance of differences across geographic classification, with P < .05 considered to be significant. We also examined associations of each component of the advantage index with the outcome and in the full structural models to determine if one or more components were driving the observed associations.
We used generalized linear models to specify multilevel analyses using county fixed effects while allowing individual-level factors to vary. Because of the substantial regional variation in the distribution of rural and urban counties across the United States, we control both for region of the United States and for location using latitude–longitude coordinates for county centroids. Because the Index of Dissimilarity was not independently associated with the outcome after controlling for county-level population characteristics, it was not included in the models.
Model 1 = NCHS category plus county centroids and regional controls.
Model 2 = model 1 plus county-level health care factors (HPSA, obstetric hospital, NICU, FQHC/RHC).
Model 3 = model 1 plus county-level socioeconomic status (advantage index).
Model 4 (full structural model) = model 1 plus county-level socioeconomic status (advantage index) plus county population characteristics (fraction white, Black, Hispanic, other; TFR).
Model 5 (complete model) = model 4 plus individual-level variables.
We used the Bayesian information criterion (BIC) measure to compare model fit. Sensitivity analyses was conducted to ensure excluding cases with missing data in model 5 did not change our findings. Sensitivity analyses included modeling of 2016 alone, the year in which all states had adopted the new birth certificate. Because we were unable to identify siblings of multiple gestation pregnancies in the data, we also ran separate models that included only singleton births to account for the potential effects of nonindependence.
All analyses were conducted by using Stata SE V16.0 (Stata Corp, College Station, TX).28
Results
The Infant Mortality Gradient by County Rural-Urban Classification
The sample included 11 881 814 live births in 2014 to 2016 and 64 478 infant deaths distributed across 3134 counties (Table 1). The infant mortality rate was lowest among infants born to mothers living in large fringe metropolitan counties. There were significant differences in the odds of infant death when comparing with fringe metropolitan counties, controlling for year, county location, and region. As counties become more rural, the odds increased and were greatest for infants of women living in noncore counties, with an odds ratio (OR) of 1.32 (95% confidence interval [CI]: 1.26–1.39) when compared with large fringe metropolitan counties. Rural-urban mortality gradients varied by period of infant death, with odds of neonatal death lowest in large fringe metropolitan counties and an inconsistent trend with increasing rurality. This contrasts with postneonatal mortality, in which the odds were progressively higher as counties became more rural, with an OR of 1.57 (95% CI: 1.46–1.69) for noncore counties when compared with large fringe metropolitan counties.
TABLE 1.
Distribution of Live Births and Infant Deaths Across Rural-Urban Classification of Resident County in the United States, 2014–2016
| Urban-Rural Classification | All Births | Infant Death | Neonatal Death | Postneonatal Death | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Ratea | ORb (95%CI) | n (%) | Ratea | ORb (95%CI) | n (%) | Ratea | ORb (95%CI) | ||
| Metropolitan | ||||||||||
| Large central metropolitan | 3 927 480 | 20 214 (31.4) | 5.15 | 1.08 (1.01–1.16)* | 13 406 (32.3) | 3.41 | 1.11 (1.04–1.19)*** | 6808 (29.7) | 1.74 | 1.06 (0.97–1.17) |
| Large fringe metropolitan | 2 784 786 | 13 301 (20.6) | 4.78 | 1.00 | 8866 (21.3) | 3.18 | 1.00 | 4435 (19.3) | 1.60 | 1.00 |
| Medium metropolitan | 2 492 999 | 14 395 (22.3) | 5.77 | 1.19 (1.13–1.25)**** | 9263 (22.3) | 3.72 | 1.18 (1.12–1.24)**** | 5132 (22.4) | 2.07 | 1.23 (1.14–1.32)**** |
| Small metropolitan | 1 068 628 | 6414 (9.9) | 6.00 | 1.22 (1.16–1.29)**** | 3915 (9.4) | 3.66 | 1.16 (1.09–1.22)**** | 2499 (10.9) | 2.35 | 1.38 (1.28–1.49)**** |
| Rural | ||||||||||
| Micropolitan | 969 396 | 6000 (9.3) | 6.19 | 1.26 (1.20–1.32)**** | 3649 (8.8) | 3.76 | 1.19 (1.13–1.26)**** | 2351 (10.2) | 2.43 | 1.42 (1.32–1.52)**** |
| Noncore (most rural) | 638 525 | 4154 (6.4) | 6.51 | 1.32 (1.26–1.39)**** | 2430 (5.9) | 3.81 | 1.20 (1.14–1.27)**** | 1724 (7.5) | 2.71 | 1.57 (1.46–1.69)**** |
| Total | 11 881 814 | 64 478 (99.9) | 5.43 | — | 41 529 (100) | 3.50 | — | 22 949 (100) | 1.94 | — |
—, not applicable.
Mortality rate is calculated as deaths per 1000 live births.
OR adjusted for county centroid, region, and year.
P < .05.
P < .01.
P < .005.
P < .001.
County and Individual Characteristics by Rural-Urban Classification
County-level characteristics (Table 2) varied by rural-urban classification (all P < .001) in measures that reflect access to health care resources, including the presence of an obstetric hospital, a facility with a NICU, a FQHC/RHC, or whether the county is identified as a HPSA. For example, whereas 100% of large central metropolitan counties had ≥1 obstetric hospital in that county, 68.2% of micropolitan and only 25.7% noncore counties had any obstetric hospital. Differences were even greater in the percentages of counties with ≥1 hospital with an NICU. Although 97.1% of large central metropolitan counties had an NICU, only 6.1% of micropolitan and 1.4% noncore counties had an NICU. There were also differences in socioeconomic status as measured by using the advantage index, as well as characteristics of the population. All individual-level characteristics (Table 3), with the exception of infant sex, also differed across the rural-urban continuum including age at delivery, completed education, BMI, and tobacco use (P < .001).
TABLE 2.
County-Level Descriptive Statistics for All United States Counties by NCHS Rural-Urban Classification, 2014–2016
| Variables | Total | Large Central Metropolitan | Large Fringe Metropolitan | Medium Metropolitan | Small Metropolitan | Micropolitan | Noncore |
|---|---|---|---|---|---|---|---|
| N = 3134 | n = 68 (2.2%) | n = 368 (11.7%) | n = 372 (11.9%) | n = 357 (11.4%) | n = 641 (20.5%) | n = 1328 (42.4%) | |
| HHS regions, n (%) | |||||||
| I | 67 (2.1) | 3 (4.4) | 13 (3.5) | 11 (3.0) | 7 (2.0) | 16 (2.5) | 17 (1.3) |
| II | 83 (2.6) | 10 (14.7) | 26 (7.1) | 13 (3.5) | 10 (2.8) | 14 (2.2) | 10 (0.8) |
| III | 282 (9.0) | 9 (13.2) | 68 (18.5) | 38 (10.2) | 46 (12.9) | 34 (5.3) | 87 (6.6) |
| IV | 736 (23.5) | 12 (17.6) | 91 (24.7) | 120 (32.3) | 90 (25.2) | 153 (23.9) | 270 (20.3) |
| V | 524 (16.7) | 10 (14.7) | 81 (22.0) | 48 (12.9) | 62 (17.4) | 138 (21.5) | 185 (13.9) |
| VI | 502 (16.0) | 8 (11.8) | 43 (11.7) | 67 (18.0) | 44 (12.3) | 104 (16.2) | 236 (17.8) |
| VII | 412 (13.1) | 2 (2.9) | 19 (5.2) | 30 (8.1) | 36 (10.1) | 74 (11.5) | 251 (18.9) |
| VIII | 291 (9.3) | 2 (2.9) | 10 (2.7) | 11 (3.0) | 25 (7.0) | 48 (7.5) | 195 (14.7) |
| IX | 94 (3.0) | 10 (14.7) | 9 (2.4) | 17 (4.6) | 15 (4.2) | 21 (3.3) | 22 (1.7) |
| X | 143 (4.6) | 2 (2.9) | 8 (2.2) | 17 (4.6) | 22 (6.2) | 39 (6.1) | 55 (4.1) |
| Health care characteristics, n (%) | |||||||
| Obstetric hospital | 1481 (47.3) | 68 (100.0) | 217 (59.0) | 206 (55.4) | 212 (59.4) | 437 (68.2) | 341 (25.7) |
| NICU | 445 (14.2) | 66 (97.1) | 89 (24.2) | 132 (35.5) | 101 (28.3) | 39 (6.1) | 18 (1.4) |
| HPSA | 1332 (42.5) | 36 (52.9) | 116 (31.5) | 154 (41.4) | 142 (39.8) | 208 (32.4) | 676 (50.9) |
| FQHC/RHC | 2605 (83.1) | 68 (100.0) | 275 (74.7) | 323 (86.8) | 292 (81.8) | 511 (79.7) | 1136 (85.5) |
| County characteristics, mean (SD) | |||||||
| Advantage index | −0.49 (0.01) | 0.19 (0.09) | 0.14 (0.05) | −0.29 (0.04) | −0.39 (0.04) | −0.63 (0.03) | −0.71 (0.02) |
| TFR | 2.14 (0.01) | 1.83 (0.02) | 1.91 (0.02) | 1.96 (0.02) | 1.98 (0.02) | 2.08 (0.02) | 2.35 (0.02) |
| Population, white | 77.65 (0.35) | 50.10 (1.91) | 76.26 (0.90) | 74.59 (0.97) | 78.49 (0.87) | 77.89 (0.79) | 79.95 (0.56) |
| Population, Black | 8.87 (0.26) | 20.68 (1.79) | 10.39 (0.68) | 10.89 (0.71) | 9.25 (0.66) | 8.04 (0.56) | 7.58 (0.42) |
| Population, Hispanic | 8.66 (0.24) | 19.03 (1.77) | 8.47 (0.50) | 9.77 (0.75) | 7.83 (0.59) | 9.78 (0.61) | 7.55 (0.36) |
| Population, other | 4.83 (0.15) | 10.18 (0.90) | 4.87 (0.21) | 4.75 (0.27) | 4.43 (0.33) | 4.30 (0.28) | 4.92 (0.31) |
HHS Regions: I: Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont; II: New Jersey, New York, Virgin Islands (Puerto Rico excluded); III: District of Columbia, Delaware, Maryland, Pennsylvania, Virginia, West Virginia; IV: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, Tennessee; V: Illinois, Indiana, Michigan, Minnesota, Ohio, Wisconsin; VI: Arkansas, Louisiana, New Mexico, Oklahoma, Texas; VII: Iowa, Kansas, Missouri, Nebraska; VIII: Colorado, Montana, North Dakota, South Dakota, Utah, Wyoming; IX: Arizona, California, Hawaii, Nevada; X: Alaska, Idaho, Oregon, Washington (American Samoa, Federated States of Micronesia, Guam, Marshall Islands, Northern Mariana Islands, Palau excluded). This includes only counties with a live birth during the study period and also excludes 5 counties in Alaska without health services indicators. All differences across region were significant to P < .001. HHS, US Department of Health and Human Services.
TABLE 3.
Individual-Level Demographic, Health, and Health Care Characteristics of Mothers and Their Infants by NCHS Rural-Urban Classification, 2014–2016
| Variables | Total | Large Central Metropolitan | Large Fringe Metropolitan | Medium Metropolitan | Small Metropolitan | Micropolitan | Noncore |
|---|---|---|---|---|---|---|---|
| N = 10 109 644 | n = 3 459 247 (34.2%) | n = 2 091 176 (20.7%) | n = 2 179 916 (21.6%) | n = 932 211 (9.2%) | n = 877 981 (8.7%) | n = 569 113 (5.63%) | |
| Mother’s characteristics | |||||||
| Age, y, mean (SD) | 28.43 (0.002) | 29.12 (0.003) | 29.34 (0.004) | 27.91 (0.004) | 27.47 (0.006) | 26.96 (0.006) | 26.72 (0.007) |
| Race and ethnicity, n (%) | |||||||
| NH white | 5 526 992 (54.7) | 1 269 739 (36.7) | 1 275 582 (61.0) | 1 257 203 (57.7) | 642 791 (69.0) | 642 868 (73.2) | 438 809 (77.1) |
| NH Black | 1 399 685 (13.8) | 636 384 (18.4) | 261 362 (12.5) | 280 460 (12.9) | 103 038 (11.1) | 73 171 (8.3) | 45 270 (8.0) |
| Hispanic | 2 394 589 (23.7) | 1 141 826 (33.0) | 397 773 (19.0) | 533 928 (24.5) | 143 715 (15.4) | 123 807 (14.1) | 53 540 (9.4) |
| AI, AN | 101 577 (1.0) | 12 811 (0.4) | 7478 (0.4) | 18 078 (0.8) | 14 106 (1.5) | 23 328 (2.7) | 25 776 (4.5) |
| API | 649 714 (6.4) | 379 472 (11.0) | 141 309 (6.8) | 85 920 (3.9) | 25 875 (2.8) | 12 914 (1.5) | 4224 (0.7) |
| Others | 37 087 (0.4) | 19 015 (0.5) | 7672 (0.4) | 4327 (0.2) | 2686 (0.3) | 1893 (0.2) | 1494 (0.3) |
| Foreign born | 2 170 197 (21.5) | 1 139 893 (33.0) | 453 607 (21.7) | 358 984 (16.5) | 106 401 (11.4) | 77 987 (8.9) | 33 325 (5.9) |
| Married | 6 064 932 (60.0) | 2 036 461 (58.9) | 1 386 459 (66.3) | 1 273 705 (58.4) | 549 340 (58.9) | 495 284 (56.4) | 323 683 (56.9) |
| Mother’s education, n (%) | |||||||
| Not HS graduate | 1 458 024 (14.4) | 543 663 (15.7) | 222 547 (10.6) | 328 700 (15.1) | 127 748 (13.7) | 140 825 (16.0) | 94 541 (16.6) |
| HS graduate | 2 527 744 (25.0) | 827 718 (23.9) | 440 641 (21.1) | 561 384 (25.8) | 256 275 (27.5) | 261 193 (29.7) | 180 533 (31.7) |
| Some college or AA | 3 014 619 (29.8) | 907 743 (26.2) | 613 581 (29.3) | 693 774 (31.8) | 310 092 (33.3) | 294 937 (33.6) | 194 492 (34.2) |
| BA and more | 3 109 257 (30.8) | 1 180 123 (34.1) | 814 407 (38.9) | 596 058 (27.3) | 238 096 (25.5) | 181 026 (20.6) | 99 547 (17.5) |
| Private insurance | 4 927 237 (48.7) | 1 636 023 (47.3) | 1 255 300 (60.0) | 997 633 (45.8) | 436 608 (46.8) | 371 282 (42.3) | 230 391 (40.5) |
| Paternal information | 9 026 645 (89.3) | 3 067 880 (88.7) | 1 925 896 (92.1) | 1 936 562 (88.8) | 824 590 (88.5) | 773 050 (88.0) | 498 667 (87.6) |
| Mother’s health, n (%) | |||||||
| Prepregnancy BMI | |||||||
| Underweight: <18.5 | 366 304 (3.6) | 136 246 (3.9) | 69 834 (3.3) | 75 802 (3.5) | 32 499 (3.5) | 31 861 (3.6) | 20 062 (3.5) |
| Ideal weight: 18.5–2 | 4 561 856 (45.1) | 1 653 070 (47.8) | 974 243 (46.6) | 948 606 (43.5) | 398 282 (42.7) | 361 738 (41.2) | 225 917 (39.7) |
| Overweight: 25–29.99 | 2 605 055 (25.8) | 881 039 (25.5) | 546 640 (26.1) | 569 629 (26.1) | 238 695 (25.6) | 223 458 (25.5) | 145 594 (25.6) |
| Obese I: 30–34.99 | 1 413 670 (14.0) | 450 680 (13.0) | 280 966 (13.4) | 317 437 (14.6) | 138 867 (14.9) | 134 893 (15.4) | 90 827 (16.0) |
| Obese II: 35–39.99 | 684 440 (6.8) | 203 336 (5.9) | 131 658 (6.3) | 156 949 (7.2) | 71 465 (7.7) | 72 036 (8.2) | 48 996 (8.6) |
| Obese III: 40+ | 478 319 (4.7) | 134 876 (3.9) | 87 835 (4.2) | 111 493 (5.1) | 52 403 (5.6) | 53 995 (6.1) | 37 717 (6.6) |
| Prenatal tobacco | 807 193 (8.0) | 120 044 (3.5) | 140 668 (6.7) | 189 164 (8.7) | 114 741 (12.3) | 139 743 (15.9) | 102 833 (18.1) |
| Diabetes | 81 164 (0.8) | 25 952 (0.8) | 15 149 (0.7) | 18 390 (0.8) | 8105 (0.9) | 8135 (0.9) | 5433 (1.0) |
| GDM | 582 035 (5.8) | 194 076 (5.6) | 125 841 (6.0) | 130 515 (6.0) | 51 393 (5.5) | 48 208 (5.5) | 32 002 (5.6) |
| Chronic hypertension | 165 751 (1.6) | 50 434 (1.5) | 33 761 (1.6) | 38 104 (1.7) | 16 060 (1.7) | 16 027 (1.8) | 11 365 (2.0) |
| Hypertension, preeclampsia | 592 722 (5.9) | 186 576 (5.4) | 123 671 (5.9) | 133 652 (6.1) | 55 936 (6.0) | 55 276 (6.3) | 37 611 (6.6) |
| Health care | |||||||
| Hospital delivery | 9 956 550 (98.5) | 3 418 125 (98.8) | 2 063 055 (98.7) | 2 143 407 (98.3) | 916 590 (98.3) | 860 603 (98.0) | 554 770 (97.5) |
| Doctor attendant | 9 104 761 (90.1) | 3 151 124 (91.1) | 1 890 329 (90.4) | 1 944 117 (89.2) | 823 187 (88.3) | 784 394 (89.3) | 511 610 (89.9) |
| Cesarean delivery | 3 214 950 (31.8) | 1 106 773 (32.0) | 686 954 (32.9) | 684 858 (31.4) | 277 747 (29.8) | 275 639 (31.4) | 182 979 (32.2) |
| Infant characteristics, n (%) | |||||||
| Female sex | 4 937 600 (48.8) | 1 689 853 (48.9) | 1 021 083 (48.8) | 1 064 476 (48.8) | 455 193 (48.8) | 429 198 (48.9) | 277 797 (48.8) |
| Singleton | 9 767 042 (96.6) | 3 340 300 (96.6) | 2 013 987 (96.3) | 2 108 124 (96.7) | 902 188 (96.8) | 850 655 (96.9) | 551 788 (97.0) |
| First born | 3 900 385 (38.6) | 1 402 584 (40.5) | 813 890 (38.9) | 814 487 (37.4) | 349 231 (37.5) | 320 155 (36.5) | 200 038 (35.1) |
All differences across region were significant to P < .001. AA, associate’s degree; AI, American Indian; AN, Alaskan native; API, Asian American and Pacific Islander; BA, bachelor’s degree; GDM, gestational diabetes mellitus; HS, high school.
Multilevel Models
The results of the multilevel models for overall mortality, neonatal mortality, and postneonatal mortality are presented in Table 4. Regional controls did little to change to the varying odds across rural-urban classification (model 1). The presence of an obstetric hospital and an NICU was significantly associated with higher odds of infant mortality overall and for both neonatal and postneonatal mortality (model 2), whereas county designation as HPSA or with an FQHC/RHC was not. Including health system characteristics in the model did little to attenuate the differences in odds of infant mortality across rural and urban classification groups.
TABLE 4.
Multilevel Models of Infant Mortality by Rural-Urban Classification of Resident County, 2014–2016
| Urban-Rural Classification | Model 1a | Model 2a | Model 3a | Model 4a | Model 5b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
| Total infant deaths | |||||||||||||||
| Metropolitan | |||||||||||||||
| Large metropolitan central | 1.12 | 1.05–1.21 | **** | 1.10 | 1.02–1.18 | *** | 1.09 | 1.02–1.16 | *** | 1.02 | 0.97–1.07 | NS | 1.00 | 0.95–1.05 | NS |
| Large metropolitan fringe | 1.00 | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | |
| Medium metropolitan | 1.17 | 1.11–1.24 | **** | 1.16 | 1.10–1.22 | **** | 1.09 | 1.04–1.14 | **** | 1.09 | 1.04–1.13 | **** | 1.06 | 1.02–1.10 | *** |
| Small metropolitan | 1.20 | 1.13–1.27 | **** | 1.19 | 1.12–1.26 | **** | 1.08 | 1.02–1.13 | *** | 1.06 | 1.02–1.11 | *** | 1.06 | 1.01–1.11 | * |
| Rural | |||||||||||||||
| Micropolitan | 1.23 | 1.16–1.30 | **** | 1.22 | 1.15–1.29 | **** | 1.04 | 0.99–1.10 | NS | 1.04 | 0.99–1.09 | NS | 1.01 | 0.97–1.06 | NS |
| Noncore (most rural) | 1.28 | 1.20–1.36 | **** | 1.26 | 1.18–1.34 | **** | 1.04 | 0.98–1.10 | NS | 1.03 | 0.97–1.08 | NS | 1.00 | 0.95–1.06 | NS |
| Health care | |||||||||||||||
| HPSA | — | — | — | 1.01 | 0.97–1.05 | NS | — | — | — | 1.03 | 1.00–1.07 | NS | — | — | — |
| FQHC/RHC | — | — | — | 0.99 | 0.95–1.03 | NS | — | — | — | 1.03 | 0.99–1.06 | NS | — | — | — |
| Obstetric hospital | — | — | — | 1.05 | 1.02–1.09 | *** | — | — | — | 1.00 | 0.97–1.02 | NS | — | — | — |
| NICU | — | — | — | 1.09 | 1.04–1.14 | **** | — | — | — | 1.04 | 0.99–1.08 | NS | — | — | — |
| Advantage index | — | — | — | — | — | — | 0.84 | 0.83–0.86 | **** | 0.82 | 0.81–0.84 | **** | — | — | — |
| BIC statistic | 798 137.5 | 798 174.7 | 797 933.6 | 797 658.6 | 618 383.2 | ||||||||||
| Neonatal deaths | |||||||||||||||
| Metropolitan | |||||||||||||||
| Large metropolitan central | 1.14 | 1.05–1.22 | **** | 1.10 | 1.02–1.18 | ** | 1.10 | 1.03–1.18 | *** | 1.01 | 0.96–1.07 | NS | 0.98 | 0.91–1.05 | NS |
| Large metropolitan fringe | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — |
| Medium metropolitan | 1.17 | 1.10–1.24 | **** | 1.15 | 1.09–1.22 | **** | 1.10 | 1.04–1.16 | **** | 1.10 | 1.04–1.15 | **** | 1.08 | 1.03–1.14 | *** |
| Small metropolitan | 1.14 | 1.07–1.21 | **** | 1.13 | 1.06–1.20 | **** | 1.04 | 0.99–1.11 | NS | 1.04 | 0.98–1.10 | NS | 1.04 | 0.98–1.11 | NS |
| Rural | |||||||||||||||
| Micropolitan | 1.17 | 1.10–1.24 | **** | 1.17 | 1.10–1.25 | **** | 1.03 | 0.97–1.09 | NS | 1.04 | 0.98–1.10 | NS | 1.03 | 0.96–1.09 | NS |
| Noncore (most rural) | 1.17 | 1.10–1.26 | **** | 1.18 | 1.10–1.26 | **** | 1.00 | 0.94–1.07 | NS | 1.02 | 0.96–1.09 | NS | 1.00 | 0.93–1.08 | NS |
| Health care | |||||||||||||||
| HPSA | — | — | — | 1.03 | 0.99–1.08 | NS | — | — | — | 1.05 | 1.00–1.09 | * | — | — | — |
| FQHC/RHC | — | — | — | 1.01 | 0.97–1.06 | NS | — | — | — | 1.03 | 0.98–1.07 | NS | — | — | — |
| OB hospital | — | — | — | 1.05 | 1.02–1.10 | *** | — | — | — | 1.00 | 0.97–1.04 | NS | — | — | — |
| NICU | — | — | — | 1.07 | 1.01–1.13 | ** | — | — | — | 1.03 | 0.98–1.08 | NS | — | — | — |
| Advantage index | — | — | — | — | — | — | 0.88 | 0.86–0.90 | **** | 0.87 | 0.85–0.89 | **** | — | — | — |
| BIC statistic | 551 437.2 | 551 481.2 | 551 359.5 | 551 284.8 | 415 463.5 | ||||||||||
| Postneonatal Deaths | |||||||||||||||
| Metropolitan | |||||||||||||||
| Large metropolitan central | 1.13 | 1.02–1.24 | ** | 1.13 | 1.02–1.25 | ** | 1.07 | 0.99–1.17 | NS | 1.03 | 0.96–1.10 | NS | 1.03 | 0.97–1.09 | NS |
| Large metropolitan fringe | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — | 1.00 | — | — |
| Medium metropolitan | 1.20 | 1.11–1.30 | **** | 1.19 | 1.10–1.29 | **** | 1.08 | 1.01–1.16 | * | 1.08 | 1.01–1.14 | ** | 1.02 | 0.97–1.08 | NS |
| Small metropolitan | 1.35 | 1.22–1.48 | **** | 1.34 | 1.22–1.47 | **** | 1.15 | 1.06–1.24 | **** | 1.12 | 1.04–1.20 | *** | 1.08 | 1.02–1.15 | * |
| Rural | |||||||||||||||
| Micropolitan | 1.36 | 1.24–1.49 | **** | 1.34 | 1.22–1.47 | **** | 1.07 | 0.99–1.16 | NS | 1.05 | 0.98–1.12 | NS | 1.00 | 0.93–1.07 | NS |
| Noncore (most rural) | 1.48 | 1.33–1.65 | **** | 1.41 | 1.27–1.58 | **** | 1.10 | 1.01–1.21 | * | 1.03 | 0.95–1.12 | NS | 1.01 | 0.93–1.09 | NS |
| Health care | |||||||||||||||
| HPSA | — | — | — | 0.97 | 0.92–1.03 | NS | — | — | — | 1.01 | 0.96–1.07 | NS | — | — | — |
| FQHC/RHC | — | — | — | 0.96 | 0.91–1.01 | NS | — | — | — | 1.03 | 0.98–1.08 | NS | — | — | — |
| OB hospital | — | — | — | 1.06 | 1.01–1.11 | ** | — | — | — | 1.00 | 0.96–1.04 | NS | — | — | — |
| NICU | — | — | — | 1.12 | 1.04–1.20 | *** | — | — | — | 1.04 | 0.98–1.11 | NS | — | — | — |
| Advantage index | — | — | — | — | — | — | 0.78 | 0.76–0.80 | *** | 0.75 | 0.73–0.77 | *** | — | — | — |
| BIC statistic | 330 663.3 | 330 705.9 | 330 467.8 | 330 266.9 | 266 771.3 | ||||||||||
Model 1 = NCHS category plus county centroids and regional controls. Model 2 = model 1 plus county-level health care factors (HPSA, obstetric hospital, NICU, FQHC/RHC). Model 3 = model 1 plus county-level socioeconomic status (advantage index). Model 4 (full structural model) = model 1+ county-level socioeconomic status (advantage index) plus county population characteristics (fraction white, Black, Hispanic, other; TFR). Model 5 (complete model) = model 4 plus individual-level variables. NS, not significant; —, not applicable.
P < .05.
P < .01.
P < .005.
P < .001.
a All models control for county centroid.
b This model excludes Connecticut, Rhode Island, New Jersey, Georgia, Virginia, and Hiawaii and includes all individual level covariates.
In contrast, the advantage index was positively associated with infant mortality (model 3), overall as well as neonatal and postneonatal, and when included in the model eliminated any significant difference in the odds of infant mortality between the micropolitan and noncore counties and the large metropolitan fringe classification groups for both overall and neonatal mortality outcomes. For postneonatal mortality, including the advantage index eliminated the differences between micropolitan counties, and only a small difference remained for noncore counties. In addition, this also eliminated any association between the health care characteristics of the county with infant mortality. Analyses of the individual components of the advantage index reveal these associations were largely driven by household income and median value of owner-occupied housing units, each inversely related to the odds of an infant death (Supplemental Table 5).
County population-level characteristics were included in the full structural model (Table 4, model 4). County race and ethnicity were associated with the outcome (P < .0001 for each) but had little effect on the overall differences across the rural-urban classification groups. The TFR was not independently associated with the odds of infant mortality. When structural factors and individual-level characteristics were included in the full model (Table 4, model 5), differences by county-level rural-urban geographic classification were small and significant only for medium and small metropolitan counties. There were no differences by region, and the population level race and ethnic composition and advantage index were each significantly associated with the outcome (all P < .001). Including individual-level characteristics, such as type of medical insurance and health behaviors such as tobacco use, did little to change the county-level odds. Results from each model, including all individual-level covariates, are included in the Supplemental Tables 6 through 8.
Separate sensitivity analyses using data for 2016 only, and for singleton births, revealed no meaningful differences in the associations found for the entire cohort.
Using the BIC to assess model fit, we found the addition of health care factors (model 2) led to a poorer fit, whereas fit improved for the other models. The advantage index improved the postneonatal model more than the neonatal model. The model predicting postneonatal mortality had a substantially better fit, based on the BIC, than those predicting overall and neonatal mortality.
Discussion
In this national study of all 2014 to 2016 US resident births, rates of infant mortality were higher as counties became more rural and driven by higher rates of mortality in the postneonatal period. Although individuals living in rural counties were less likely to have access to an obstetric hospital or an NICU in their county, with our multilevel analysis we found no evidence that this factor explains the greater odds of infant mortality in rural counties. The more prevalent use of tobacco, presence of other health risks, and lower rates of private insurance also did not account for the differences. Instead, we find the higher infant mortality rates in rural counties are best explained by the greater socioeconomic disadvantage of their county of residence.
The association of socioeconomic factors with mortality is consistent with United States and international studies of mortality.5,15,29–32 Although access to health care may be of unique relevance to maternal and infant health, our analysis finds little independent contribution of local health care resources to the higher rates of infant mortality in rural counties in the United States, net of socioeconomic and individual factors. The resources of hospitals with higher levels of care, including NICUs, are critically important to improved survival of infants born at early gestational ages. However, our results are consistent with a growing literature showing infant mortality rates due to congenital malformations, sudden unexpected infant death as well as higher rates of unintentional injuries are higher in more rural counties, and not low birth weight or maternal complications.2,33
As in previous literature, we found that individuals living in rural counties are less likely to live in a county with an obstetric hospital or an NICU. However, these resources were not independently associated with odds of infant mortality. This may be due to the success of formal and informal systems of regionalized perinatal care supporting maternal and infant health, connecting more rural communities with larger urban centers offering higher levels of obstetrical and neonatal intensive care services.34,35 Alternatively, it may reflect the more limited impact of these systems on this important outcome.32 This is especially likely when considering their limited impact on postneonatal deaths because their cause of death is unlikely to be related to NICU care. Also consistent with previous research, many individual-level health risk factors, including lack of private insurance, tobacco use, and obesity, were more common as counties became more rural. However, their greater prevalence did not explain the higher infant mortality rates in micropolitan and noncore counties.
Limitations of this study are important to consider. The NCHS rural-urban classification of counties is a crude assessment of rurality and does not fully account for within-county variation or resources in nearby metropolitan areas. Similarly, the county-level data used to estimate socioeconomic resources may not reflect the spatial variability across neighborhoods and communities, but small-area data are difficult to examine on the national scale and for rare outcomes such as infant death. As in any study of this magnitude, missing data are inevitable. Some states were dropped from our final model; however, sensitivity analyses suggest their exclusion made little difference in the results. In addition, the results do not address the potential association of these factors with stillbirth or perinatal mortality, an important area for future research.
Conclusions
Differences in infant mortality may be better understood within a multilevel framework informed by the socio-ecological perspective and considering the importance of socioeconomic factors. Despite increasing levels of urbanization, 13.5% of 2014 to 2016 live births in the US occurred to residents of micropolitan and noncore (rural) counties. Given national goals to reduce infant mortality and achieve health equity in birth outcomes, health policymakers should also pay attention to the differing outcomes and socioeconomic milieux along the rural-urban continuum. These findings suggest that investment beyond medical care may be needed if we are to continue to see improvements in infant mortality at the national level and equity in rural areas.
Acknowledgments
We thank Dr Emily Shrider for her valuable contributions to early versions of this article. This research uses data from the NCHS with permission from the National Association for Public Health Statistics and Information Systems as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. All other data are from publicly available sources.
Glossary
- BIC
Bayesian information criterion
- CI
confidence interval
- FQHC
Federally Qualified Health Center
- HPSA
Health Professional Shortage Area
- NCHS
National Center for Health Statistics
- NH
non-Hispanic
- OR
odds ratio
- RHC
Rural Health Clinic
- TFR
total fertility rate
Footnotes
Dr Ehrenthal conceptualized and designed the study, obtained the data, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Kuo conducted the data linkages and data cleaning, contributed to the study design, conducted the data analysis, and reviewed and revised the manuscript. Dr Kirby contributed to the study design and critically reviewed and revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Support was provided in part by grants awarded to the Center for Demography and Ecology at the University of Wisconsin–Madison by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2C HD047873). The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the National Institutes of Health or any other institutions listed above. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Ely DM, Driscoll AK, Matthews TJ. Infant Mortality Rates in Rural and Urban Areas in the United States, 2014. Hyattsville, MD: National Center for Health Statistics; 2017 [PubMed] [Google Scholar]
- 2.Womack LS, Rossen LM, Hirai AH. Urban-rural infant mortality disparities by race and ethnicity and cause of death. Am J Prev Med. 2020;58(2):254–260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James WL. All rural places are not created equal: revisiting the rural mortality penalty in the United States. Am J Public Health. 2014;104(11):2122–2129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. J Urban Health. 2014;91(2):272–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cosby AG, McDoom-Echebiri MM, James W, Khandekar H, Brown W, Hanna HL. Growth and persistence of place-based mortality in the United States: the rural mortality penalty. Am J Public Health. 2019;109(1):155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callaghan WM. Geographic variation of reproductive health indicators and outcomes in the United States: place matters. Am J Obstet Gynecol. 2014;211(3):278–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim D, Saada A. The social determinants of infant mortality and birth outcomes in Western developed nations: a cross-country systematic review. Int J Environ Res Public Health. 2013;10(6):2296–2335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463 [DOI] [PubMed] [Google Scholar]
- 9.Huynh M, Spasojevic J, Li W, et al. Spatial social polarization and birth outcomes: preterm birth and infant mortality - New York City, 2010-14. Scand J Public Health. 2018;46(1):157–166 [DOI] [PubMed] [Google Scholar]
- 10.Kramer MR, Cooper HL, Drews-Botsch CD, Waller LA, Hogue CR. Metropolitan isolation segregation and Black-White disparities in very preterm birth: a test of mediating pathways and variance explained. Soc Sci Med. 2010;71(12):2108–2116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh GK, Kogan MD. Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the United States, 1969-2001. Pediatrics. 2007;119(4). Available at: www.pediatrics.org/cgi/content/full/119/4/e928 [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Ten great public health achievements–United States, 1900-1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241–243 [PubMed] [Google Scholar]
- 13.Hung P, Henning-Smith CE, Casey MM, Kozhimannil KB. Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004-14. Health Aff (Millwood). 2017;36(9):1663–1671 [DOI] [PubMed] [Google Scholar]
- 14.Brantley MD, Davis NL, Goodman DA, Callaghan WM, Barfield WD. Perinatal regionalization: a geospatial view of perinatal critical care, United States, 2010–2013. Am J Obstet Gynecol. 2017;216(2):185.e1-185.e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sparks PJ, McLaughlin DK, Stokes CS. Differential neonatal and postneonatal infant mortality rates across US counties: the role of socioeconomic conditions and rurality. J Rural Health. 2009;25(4):332–341 [DOI] [PubMed] [Google Scholar]
- 16.Matteson DW, Burr JA, Marshall JR. Infant mortality: a multi-level analysis of individual and community risk factors. Soc Sci Med. 1998;47(11):1841–1854 [DOI] [PubMed] [Google Scholar]
- 17.Krieger N. Epidemiology and social sciences: towards a critical reengagement in the 21st century. Epidemiol Rev. 2000;22(1):155–163 [DOI] [PubMed] [Google Scholar]
- 18.McMichael AJ. Prisoners of the proximate: loosening the constraints on epidemiology in an age of change. Am J Epidemiol. 1999;149(10):887–897 [DOI] [PubMed] [Google Scholar]
- 19.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Health Resources and Services Administration. Area Health Resources Files. 2019. Available at: https://data.hrsa.gov/topics/health-workforce/ahrf. Accessed November 10, 2019
- 21.Department of Health and Human Services. User guide to the 2014 period linked birth/infant death public use file. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/periodlinked/LinkPE14Guide.pdf. Accessed January 29, 2020
- 22.Department of Health and Human Services. User guide to the 2015 period linked birth/infant death public use file. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/periodlinked/LinkPE15Guide.pdf. Accessed January 29, 2020
- 23.Department of Health and Human Services. User guide to the 2016 period linked birth/infant death public use file. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/DVS/periodlinked/LinkPE16Guide.pdf. Accessed June 5, 2020
- 24.Kirby RS, Salihu HM. Back to the future? A critical commentary on the 2003 U.S. National standard certificate of live birth. Birth. 2006;33(3):238–244 [DOI] [PubMed] [Google Scholar]
- 25.Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Hyattsville, MD: National Center for Health Statistics; 2014 [PubMed] [Google Scholar]
- 26.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106 [DOI] [PubMed] [Google Scholar]
- 27.Ely DM, Hamilton BE. Trends in Fertility and Mother’s Age at First Birth Among Rural and Metropolitan Counties: United States, 2007-2017. Hyattsville, MD: National Center for Health Statistics; 2018 [PubMed] [Google Scholar]
- 28.Stata Statistical Software: Release 16 [computer program]. College Station; TX: StataCorp LLC; 2019 [Google Scholar]
- 29.Chen A, Oster E, Williams H. Why is infant mortality higher in the United States than in Europe? Am Econ J Econ Policy. 2016;8(2):89–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoynes H, Miller D, Simon D. Income, the earned income tax credit, and infant health. Am Econ J Econ Policy. 2015;7(1):172–211 [Google Scholar]
- 31.Komro KA, Livingston MD, Markowitz S, Wagenaar AC. The effect of an increased minimum wage on infant mortality and birth weight. Am J Public Health. 2016;106(8):1514–1516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mohamoud YA, Kirby RS, Ehrenthal DB. Poverty, urban-rural classification and term infant mortality: a population-based multilevel analysis. BMC Pregnancy Childbirth. 2019;19(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ely DM, Hoyert DL. Differences Between Rural and Urban Areas in Mortality Rates for the Leading Causes of Infant Death: United States, 2013–2015. Hyattsville, MD: National Center for Health Statistics; 2018 [PubMed] [Google Scholar]
- 34.Handley SC, Srinivas SK, Lorch SA. Regionalization of care and the maternal-infant dyad disconnect. JAMA. 2019;322(6):503–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Otterloo LR, Connelly CD. Risk-appropriate care to improve practice and birth outcomes. J Obstet Gynecol Neonatal Nurs. 2018;47(5):661–672 [DOI] [PubMed] [Google Scholar]