Abstract
Leiomyomas are the most common benign gynecologic tumors and the most common surgical indication for hysterectomy or myomectomy. Recurrent pelvic leiomyomas or vaginal leiomyomas are rare. We report the case of a 60-year-old woman with a history of a cesarean total hysterectomy 25 years before presenting to us, who developed a pelvic leiomyoma arising from the vaginal cuff. The patient underwent single-port laparoscopic tumor excision and recovered uneventfully.
KEYWORDS: Cuff, Hysterectomy, Laparoscopy, Myoma, Recurrence
INTRODUCTION
Uterine leiomyomas are the most common benign gynecologic tumors and the most common surgical indication for hysterectomy or myomectomy. However, recurrent pelvic myomas after morcellation during laparoscopy have been reported at rates of 0.12%-0.95% [1]. Furthermore, low-incidence leiomyosarcomas can occur under this setting [2]. Thus, in-bag manual morcellations have been recommended [3].
Recurrent myomas after a total hysterectomy are rare with <110 cases reported until now [4]. Here, we report the case of a woman with a pelvic recurrent myoma arising from the vaginal cuff after total hysterectomy during a cesarean section that had taken place 25 years before.
CASE REPORT
A 60-year-old woman, gravida 3, para 3, presented with an asymptomatic pelvic mass. She had undergone cesarean total hysterectomy with bilateral adnexa preservation 25 years before due to the presence of a uterine myoma. After that, she experienced surgical menopause. Her medical history included coronary artery disease, type 2 diabetes mellitus, dyslipidemia, and hyperparathyroidism. She had no history of hormone replacement therapy after menopause.
She was referred to our hospital with a pelvic mass found incidentally during a routine health examination. A whole-body magnetic resonance (MR) image showed a well-circumscribed mass of 7.2 × 6.4 cm in the pelvis [Figure 1a and b]. Vaginal examination revealed an upward deviation of her vaginal cuff. Transvaginal ultrasound images demonstrated a 6.25 × 5.03 × 6.94 cm pelvic tumor [Figure 1c and d]. Tumor markers (CA 125, CA 19-9, and CEA) were all within normal ranges.
Figure 1.
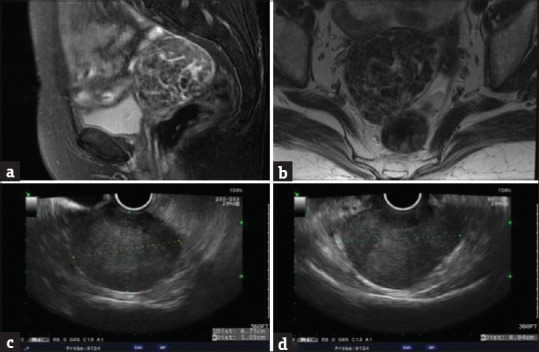
Image study of the pelvic myoma. Pelvic magnetic resonance image showing sagittal (a) and coronary (b) views of the myoma. Pelvic ultrasound showing sagittal (c) and coronary (d) views of the myoma
We scheduled the patient for surgery to rule out the possibility of malignancy. She underwent a single-port laparoscopic tumor excision. During the surgery, we found the tumor to be pedunculated and originating from the vaginal cuff [Figure 2a]. The tumor was round, firm, and sharply circumscribed resembling a uterine leiomyoma [Figure 2b]. A frozen section revealed a leiomyoma [Figure 3a and b]. The immunohistochemistry was positive for vimentin [Figure 3c] and smooth muscle actin (SMA) [Figure 3d], which are typical of myomas. We discharged the patient 2 days after the operation. Her condition was good when she came back to our outpatient department for a follow-up 1 month after surgery.
Figure 2.
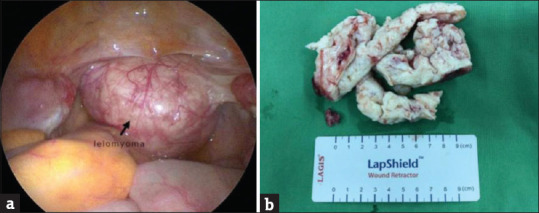
Laparoendoscopic surgery for pelvic myoma. (a) Pelvic myoma along the vaginal cuff region. (b) Myoma retrieval by in-bag manual morcellation
Figure 3.
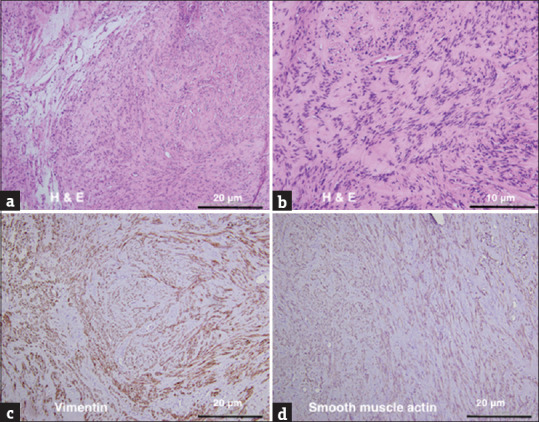
Pathology of pelvic myoma. (a and b) Histology of the myoma showed by H and E staining. Smooth muscle cells were elongated with eosinophilic cytoplasm. Smooth muscle bundle showed fascicular pattern. The immunohistochemistry was positive for vimentin (c) and smooth muscle actin (d) which are typical of myoma. Scale bar = 10 μm (b) and = 20 μm (a, c, and d)
DISCUSSION
Uterine leiomyomas are the most common pelvic tumors in women. They are benign and monoclonal tumors originating from uterine smooth muscle cells. Interestingly, they can behave like malignancies and metastasize to various sites outside the uterus, such as the pelvis, lungs, retroperitoneum, heart, vessels, spine, and lymph nodes [5]. Vaginal leiomyomas are rare with about 300 reported cases [6]. A vaginal vault leiomyoma developing after a hysterectomy is even more uncommon, and only six cases have been reported [7,8,9,10,11,12]. The recurrence intervals have ranged from 1 to 25 years [Table 1]. In our case, the myoma recurred 25 years after the hysterectomy.
Table 1.
Summary of cases with vaginal cuff leiomyomas after hysterectomy
| Author (years) | Patient age (years) | Time to diagnosis (years) | Hysterectomy indication/procedure | Recurrence site | Tumor size (cm) | Pathology | Treatment |
|---|---|---|---|---|---|---|---|
| Yogesh et al., 2005 [7] | 42 | 5 | Leiomyoma/TAH | Anterior vaginal wall | 19×11×9 | Leiomyoma | Surgical excision with BSO (laparotomy) |
| Yanamandra et al., 2007 [8] | 47 | 8 | Leiomyoma/TAH | Vaginal vault | 15×10 | Leiomyoma | Surgical excision with BSO (laparotomy) |
| Ismail and Adams 2009 [9] | 47 | 1 | Leiomyoma/TAH | Vaginal vault | 3×3 | Leiomyoma | Surgical excision (vaginal) |
| Yarci et al., 2010 [10] | 70 | 25 | Leiomyoma/TAH + BSO | Vaginal vault | 7×3 | Leiomyoma | Surgical excision (vaginal) |
| P et al., 2014 [11] | 48 | 6 | Leiomyoma/TAH | Vaginal stump near right broad ligament | 4×4 | Leiomyoma | Surgical excision (laparotomy) |
| Bhuyar 2015 [12] | 65 | 4 | Leiomyoma/TAH + BSO | Vaginal vault | 10×10 | Atypical leiomyoma | Surgical excision (vaginal) |
| Present case | 65 | 25 | Leiomyoma/cesarean hysterectomy | Vaginal vault | 7×6 | Leiomyoma | Surgical excision (laparoscopic) |
TAH: Total abdominal hysterectomy; BSO: Bilateral salpingo-oophorectomy
Vaginal leiomyomas are pathologically similar to uterine leiomyomas. They are thought to arise from the vascular smooth muscle of the vagina, the submucosal smooth muscle, the smooth muscle of the round ligament, or from mesenchymal stem cell differentiation into smooth muscle cells [13]. Peritoneal seeding after myomectomy or hysterectomy during laparotomy or laparoscopic morcellation for uterine leiomyomas is another possible cause of these tumors. In theory, the residual morcellation fragments may be introduced to the peritoneum or adjacent tissues, where they later develop into pelvic or vaginal leiomyomas [5]. The growth of vaginal leiomyomas may depend on the association between hormones and locally active growth factors. They show strong positivity for SMA. In the study by Zhao et al., 38.5% and 34.6% of vaginal leiomyomas expressed estrogen receptor and epidermal growth factor receptor, respectively, suggesting a role for estrogen in the pathogenesis of the tumor. However, recurrent leiomyomas can occur in women with poor estrogenic statuses even after a total hysterectomy and bilateral salpingo-oophorectomy without hormone replacement therapy [10].
Vaginal leiomyomas may be asymptomatic. However, symptoms may be present depending on the site of occurrence and include lower abdominal pain, low back pain, vaginal bleeding, dyspareunia, urinary frequency dysuria, and urinary obstruction [6].
The diagnosis of vaginal leiomyomas through ultrasonography may be difficult, and MR imaging is a superior tool for diagnosing them. In MR imaging, these tumors can appear as single, smooth tumors with homogeneous low-signal intensity on both T1- and T2-weighted images, as is typical in uterine leiomyomas. However, the cellular and vascular-type leiomyomas may show hyperintensity on T2-weighted images and marked contrast enhancement [14]. Malignant changes of primary leiomyomas or malignancies have also been reported [7]. Histopathological confirmation is the gold standard of diagnosis to rule out the possibility of malignancy.
Surgical resection of the tumor can be performed vaginally, laparoscopically, or abdominally depending on the tumor size, location, and accessibility. In our case, the leiomyoma originated from the vaginal cuff and protruded into the pelvic cavity. We resected it successfully through a laparoscopic approach. Vaginal myomectomy and transvaginal natural orifice transluminal endoscopic surgery myomectomy are feasible alternatives. Oophorectomy may be performed concurrently with the removal of the fibroids, ensuring an estrogen-poor environment and reducing the risk of recurrence. Complete and in-bag removal of the tumors with undetermined pathology is recommended during the operation to prevent inadvertent dissemination or spillage of occult malignancies.
CONCLUSION
Although rare, vaginal cuff leiomyomas can develop even in hysterectomized women. The outcome is favorable after complete excision of the tumor.
Declaration of patient consent
We, the authors, certify that we have obtained all appropriate patient consent forms. In the forms, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her names and initials will not be published and due efforts will be made to conceal her identity, but that anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Van der Meulen JF, Pijnenborg JM, Boomsma CM, Verberg MF, Geomini PM, Bongers MY. Parasitic myoma after laparoscopic morcellation: A systematic review of the literature. BJOG. 2016;123:69–75. doi: 10.1111/1471-0528.13541. [DOI] [PubMed] [Google Scholar]
- 2.Wright JD, Tergas AI, Cui R, Burke WM, Hou JY, Ananth CV, et al. Use of electric power morcellation and prevalence of underlying cancer in women who undergo myomectomy. JAMA Oncol. 2015;1:69–77. doi: 10.1001/jamaoncol.2014.206. [DOI] [PubMed] [Google Scholar]
- 3.Ding DC, Hong MK, Chu TY, Chang YH, Liu HW. Robotic single-site supracervical hysterectomy with manual morcellation: Preliminary experience. World J Clin Cases. 2017;5:172–7. doi: 10.12998/wjcc.v5.i5.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kyriakopoulos K, Domali E, Stavrou S, Rodolakis A, Loutradis D, Drakakis P. Recurrent benign leiomyomas after total abdominal hysterectomy? Rich or poor estrogenic environment may lead to their recurrence. Int J Surg Case Rep. 2018;44:191–3. doi: 10.1016/j.ijscr.2018.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnaś E, Książek M, Raś R, Skręt A, Skręt-Magierło J, Dmoch-Gajzlerska E. Benign metastasizing leiomyoma: A review of current literature in respect to the time and type of previous gynecological surgery. PLoS One. 2017;12:e0175875. doi: 10.1371/journal.pone.0175875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chakrabarti I, De A, Pati S. Vaginal leiomyoma. J Midlife Health. 2011;2:42–3. doi: 10.4103/0976-7800.83274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yogesh K, Amita M, Rajendra K, Raju A, Rekha W, Hemant T. Vaginal leiomyoma developing after hysterectomy - Case report and literature review. Aust N Z J Obstet Gynaecol. 2005;45:96–7. doi: 10.1111/j.1479-828X.2005.00354.x. [DOI] [PubMed] [Google Scholar]
- 8.Yanamandra SR, Redman CW, Coomarasamy A, Varma R. Leiomyoma appearing in the vaginal vault following hysterectomy. J Obstet Gynaecol. 2007;27:91–2. doi: 10.1080/01443610601076176. [DOI] [PubMed] [Google Scholar]
- 9.Ismail SM, Adams SA. Vaginal vault leiomyoma. J Obstet Gynaecol. 2009;29:160–1. doi: 10.1080/01443610802643972. [DOI] [PubMed] [Google Scholar]
- 10.Yarci A, Bayramov V, Sükür YE, Yüce T, Berker B. Vaginal vault leiomyoma: 25 years after total abdominal hysterectomy. J Minim Invasive Gynecol. 2010;17:116–7. doi: 10.1016/j.jmig.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 11.Pallavee P, Ghose S, Samal S, Begum J, Zabeen M. Fibroid after hysterectomy: A diagnostic dilemma. J Clin Diagn Res. 2014;8:OD01–2. doi: 10.7860/JCDR/2014/8195.4532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhuyar S. Recurrent atypical leiomyoma arising from vaginal cuff after hysterectomy-A rare case report. IOSR-J Dental Med Sci. 2015;14:69–72. [Google Scholar]
- 13.Zhao Y, Li Y, Xu Y. Clinico-pathologic analysis of 26 cases of leiomyoma of the vagina. Beijing Da Xue Xue Bao Yi Xue Ban. 2003;35:37–40. [PubMed] [Google Scholar]
- 14.Shimada K, Ohashi I, Shibuya H, Tanabe F, Akashi T. MR imaging of an atypical vaginal leiomyoma. AJR Am J Roentgenol. 2002;178:752–4. doi: 10.2214/ajr.178.3.1780752. [DOI] [PubMed] [Google Scholar]


