Abstract
Background:
A reduced forced vital capacity without obstruction (low FVC) is the predominant spirometric abnormality reported in workers and volunteers exposed to dust, gases, and fumes at the World Trade Center (WTC) disaster site in 2001–2002. While low FVC has been associated with obesity and metabolic syndrome, its association with WTC occupational exposures has not been demonstrated. We estimated the prevalence of this abnormality and examined its association with WTC exposure level.
Methods:
Longitudinal study of the relation between arrival at the WTC site within 48 hours and FVC below the lower limit of normal (FVC<LLN, with normal FEV1/FVC ratio) at any time in 10,284 workers with at least two spirometries between 2002 and 2018. Logistic regression and linear mixed models were used for the multivariable analyses.
Results:
The prevalence of low FVC increased from 17.0% (95% CI 15.4%, 18.5%) in June 2003, to 26.4% (95% CI 24.8%, 28.1%) in June 2018, and exceeded at both times that of obstruction. The rate of FVC decline was −43.7 ml/year during the study period. In a multivariable analysis adjusting for obesity, metabolic syndrome indicators, and other factors, early arrival at the WTC disaster site was significantly associated with low FVC, but only among men (ORadj =1.29, 95% CI 1.17, 1.43). Longitudinal FVC rate of decline did not differ by WTC site arrival time.
Conclusions:
Among WTC workers, the prevalence of low FVC increased over a 16-year period. Early arrival to the WTC disaster site was significantly associated with low FVC in males.
Keywords: Occupational lung disease; smoke inhalation injury; World Trade Center Attack, 2001; longitudinal changes in lung function; Spirometry
Introduction
Occupational exposures at the World Trade Center (WTC) disaster site in 2001–2002 have been associated with a variety of adverse health effects[1], including a heterogeneous, often not easily classifiable group of chronic lower airway diseases[1, 2]. In all cohorts with lung function data, the most consistent and frequently reported spirometric ventilatory impairment pattern has been that of reduced forced vital capacity (low FVC), with obstruction being considerably less frequent[1, 3–7].
In 2009, a report of longitudinal expiratory flow trajectories in the largest and most diverse occupational WTC cohort, was based on only two spirometries per subject[8]. In that study, the decline rate in lung function was normal or what was expected with aging: the mean decline in prebronchodilator FVC and first second forced expiratory flow (FEV1) were −13 and −2 mL/year, respectively. Moreover, the only identified predictors of more rapid decline in FEV1 and FVC were lack of bronchodilator responsiveness at the baseline examination, and weight gain between examinations, with these two factors accounting, however, for no more than 10% of the variance in lung function decline. A more recent report of a sub-cohort of WTC responders[7], identified a larger average FEV1 decline (−35.7 ml/year), more widely divergent longitudinal FEV1 trajectories, and quantitative chest CT measured wall area percent, age at baseline, presence of bronchodilator response, and lack of significant pre-WTC occupational exposures as significant predictors. Importantly, neither study identified WTC occupational exposure indicators as significant predictors.
On the basis of previous findings, we conducted an updated analysis of decline in FVC in the WTC cohort, 18 years after the disaster, using also an updated definition of low FVC that requires absence of obstruction (i.e., FEV1/FVC above lower limit of normal)[9]. Low FVC thus defined is emerging as a phenotype of chronic airway disease[9, 10]. Low FVC can, however, also result from a variety of factors, including obesity[11] (more prevalent in the WTC occupational cohorts[6, 8, 12, 13] than in the general U.S. population[14]), short exhalatory time, and true lung restriction (i.e., reduced total lung capacity)[15]. We hypothesized that two previously proposed[1] WTC exposure level indicators, namely early arrival (within 48 hours) to the disaster site and WTC exposure duration, would be associated with a reduced FVC, after adjusting for other risk factors in this and other WTC occupational cohorts[7, 16, 17], as well as in the general population[18].
Methods
Subjects and clinical data acquisition:
All subjects participated in the screening, surveillance, and clinical programs of the WTC Clinical Center of Excellence at Mount Sinai Medical Center, in New York City[4, 5]. The New York University School of Medicine IRB (i16–01412), and the Mount Sinai Program for the Protection of Human Subjects (HS 17–01098) approved the study. Details on subject recruitment, eligibility criteria, and screening and surveillance protocols have been previously reported[4]. In brief, participants were all workers and volunteers who performed rescue, recovery, and service restoration duties at the WTC disaster site from September 11, 2001 to June 2002. This open cohort includes all occupational groups that worked at the disaster site[19]. Beginning in July 2002, all subjects underwent a baseline screening evaluation, which included questionnaires on respiratory symptoms, pre-WTC- and WTC-related occupational exposures, physical examination, laboratory testing, spirometry, and chest radiograph (repeated on alternate visits). Subsequent (“monitoring”) health surveillance visits included a similar evaluation at 12- to 18-month intervals, and clinical services were offered (often contiguously to the screening) for individualized diagnostic and treatment services[1, 20]. Inclusion into this study required that the WTC workers had at least two screening and surveillance spirometries of adequate quality.
Spirometry:
Spirometry was performed using the EasyOne® portable flow device (ndd, Zurich, Switzerland). Bronchodilator response (BDR) was assessed at least once (and most often at the baseline visit) by repeating spirometry 15 minutes after administration of 180 mcg of albuterol via metered dose inhaler and a disposable spacer. Predicted values for spirometric measurements were calculated for all subjects’ acceptable tests, based on reference equations from the third National Health and Nutrition Examination Survey (NHANES III)[21], and all testing, quality assurance, ventilatory impairment pattern definitions, bronchodilator response presence, and interpretative approaches followed American Thoracic Society recommendations[22–24]. Spirometries in this study were selected if performance had been acceptable, and they had a good quality, based on computer quality grade (a measure of reproducibility)[24] A or B, or C if at least 5 trials had been obtained, and a forced exhalatory time of at least 6 seconds[9].
Statistical analysis:
Presentation of descriptive data included means and standard deviations (SD), medians and interquartile ranges (IQR), or counts and proportions, as appropriate. We employed simple logistic regression for unadjusted analyses, and standardized differences (StD)[25] to compare subjects included and excluded from the study. For the latter, we considered a standardized difference≥0.2 as indicating a significant effect size of a covariate. Cross-sectional prevalence of low FVC was determined by the occurrence of that pattern among all subjects tested within the year preceding June 30, 2003, and June 30, 2018, respectively.
Our outcome of interest was having low FVC, defined as both a measured pre-bronchodilator FVC below each individual’s predicted lower limit of predicted normal value (LLN), and a normal ratio of first-second forced expiratory volume to FVC (FVC<LLN and FEV1/FVC>LLN, low FVC). Our dichotomous predictor of interest was self-reported arrival at the WTC disaster site within 48 hours at the WTC site. We employed multivariable logistic regression, using generalized estimating equations with an exchangeable correlation structure to account for repeated measures. For descriptive purposes, we estimated the prevalence of obstruction, defined as pre-bronchodilator evidence of FEV1/FVC<LLN.
The following covariates were included in the multivariable analyses: (1) cumulative WTC exposure duration, assessed at baseline, and categorized with more than 60 days as the cutpoint; (2) social and demographic variables, all assessed at baseline: age on September 11, 2001, gender, height, race/ethnicity (Latino of any race, and non-Latino White, Black, and other race), and occupation before 9/11/2001 (categorized into protective services, construction, building cleaning and maintenance and electrical, telecommunications, and other installation and repair group [BCM&IRG], and all other); (3) body mass index (BMI) at each evaluation, categorized into normal (>18 and <25 kg/m2), overweight (≥25 and <30 kg/m2), and obese (≥30 kg/m2); (4) entry into the cohort, categorized into calendar years 2002–2005, 2006–2008, and 2009 and later; (5) evidence of bronchodilator response (dichotomous) at any visit; (6) smoking status at each visit, categorized into never, former and current smokers. A subject was considered a never smoker if (s)he had smoked less than 20 packs of cigarettes (or 12 oz. of tobacco) in a lifetime, or less than 1 cigarette/day (or 1 cigar/week) for one year. A minimum of 12 months without tobacco use was required to deem a subject a former smoker[26]; (7) highest recorded heart rate (cutpoint 90 beats per minute), diastolic blood pressure (cutpoint 90 mm Hg); (8) highest recorded serum glucose level (whether fasting or not, cutpoint 200 mg/dl), triglyceride level (whether fasting or not, cutpoint 300 mg/dl), eosinophil (cutpoint 351/mcl), and neutrophil (cutpoint 6,000/mcl) counts, and lowest recorded high-density lipoprotein (HDL, cutpoints 40 and 50 mg/dl for men and women, respectively). We used HDL, glucose, triglycerides, and diastolic blood pressure as surrogate indicators of probable metabolic syndrome (Metsyn), categorized as 0–1 and 2–4 indicators.
Collinearity among variables was excluded by the variance inflation factor. The dependent variable was the dichotomous outcome of whether a subject’s FVC was below the lower limit of predicted normal, without obstruction (low FVC), at any time , and the main predictor, arrival within 48 hours at the WTC disaster site. Interaction terms were examined, and stratified results were presented if found. We used multiple imputation with fully conditional specification to address missing responses among the independent variables, and performed sensitivity analysis without multiple imputation as a comparison. The results with the complete and imputed data sets were essentially identical, and we therefore present only the latter.
We also used linear mixed model with a random intercept to estimate the longitudinal rate of FVC decline for the cohort. In this multivariable model, the covariates were the same as in our main model, and all were estimated as fixed effects, with age on 9/11/2001 and height centered at the mean, and in 5-year, and 5-cm units, respectively.
A two-sided p value below 0.05 defined statistical significance. The SAS program, version 9.4 (SAS Institute, Cary, NC) was used for all analyses.
Results
We had 33,093 spirometries on 10,284 subjects (mean 3.2, SD 1.4), followed for a mean of 7.2 (SD 4.1) years, until 30-June-2018. The cohort demonstrated the predominance of male sex (85.4%) and overweight and obesity (85.6%) typical of the WTC occupational cohorts. Figure 1 shows the study flow chart. Compared to subjects excluded from this analysis, those included were slightly older, and more likely to be early entrants into the cohort, to meet at least 2 of the metabolic syndrome indicators, and to have higher neutrophil and eosinophil counts (Table OS1).
Figure 1.
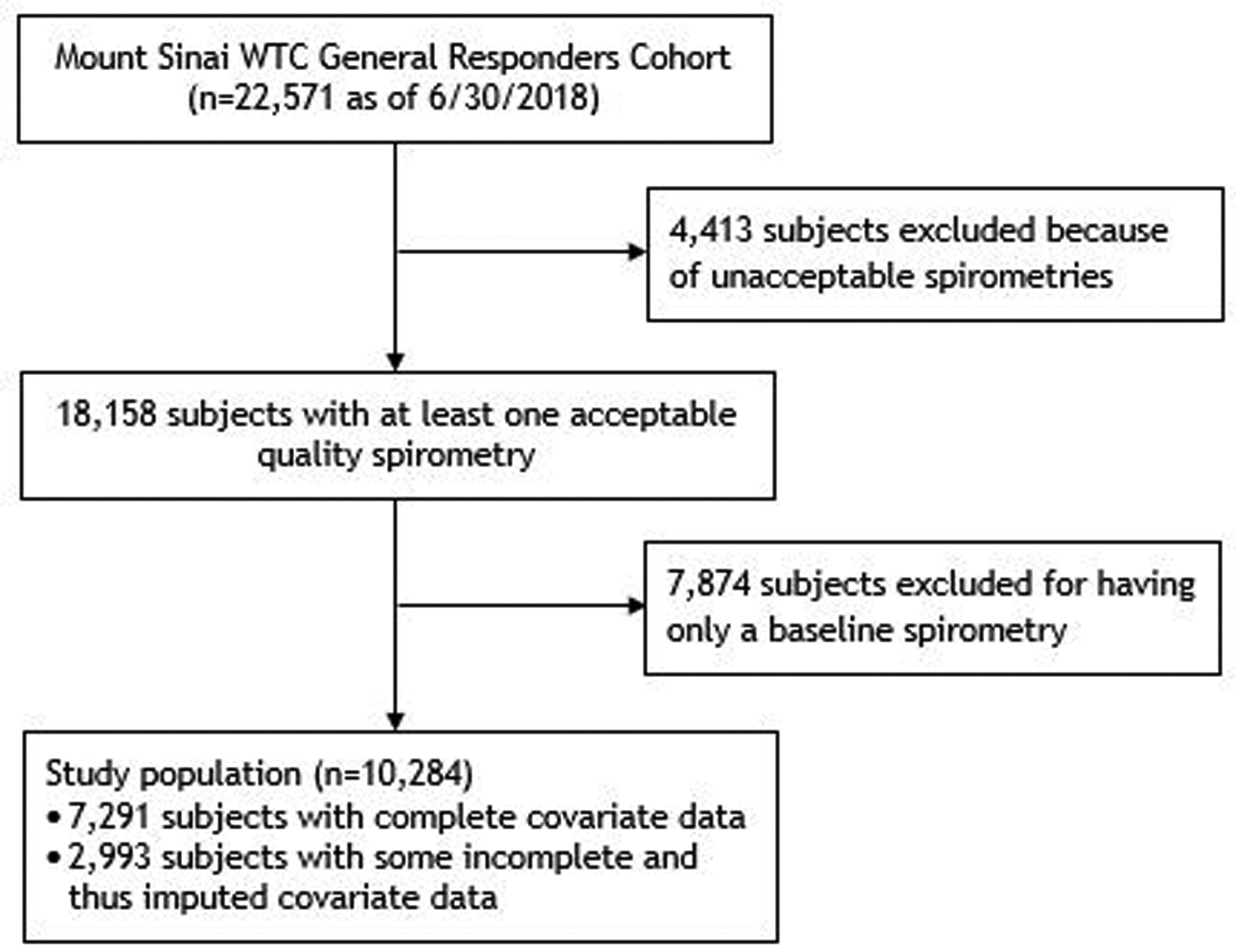
Study flowchart.
Table 1 shows the main characteristics of study participants. The mean age was 39.7 (SD 8.7) years on September 11, 2001, with the typical male predominance (85.4%), and overweight/obesity prevalence (85.6%) of the WTC occupational cohorts. The overall cross-sectional prevalence of low FVC in June 2003 was 17.0% (95% CI 15.4%, 18.5%), and was higher among those who arrived at the WTC within 48 hours (18.5%, 95% CI 16.5%, 20.6%) vs. those who did not (14.5%, 95% CI 12.2%, 16.9%). That overall prevalence increased by June 2018 to 26.4% (95% CI 24.8%, 28.1%), being even more clearly higher among those who arrived at the WTC within 48 hours (29.2%, 95% CI 27.0%, 31.4%) vs. those who did not (22.0%, 95% CI 19.4%, 24.6%). In contrast, the prevalence of obstruction was 10.5% and 5.9% in June 2003 and June 2018, respectively, and was not significantly associated with WTC arrival within 48 hours in either unadjusted or adjusted analyses (data not presented). The rate of longitudinal decline in FVC for the cohort was −43.7 (95% CI −42.9, −44.5) ml/year, and did not differ by WTC arrival time.
Table 1.
Characteristics of 10,284 WTC responders, with stratification by the main predictor of interest, arrival at the WTC disaster site within 48 hours of the terrorist attack on September 11, 2001.
| Arrival at the WTC disaster site | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Entire group | ≤ 48 hr | > 48 hr | Missing | ||||||
| Characteristic | value | n or mean | % or SD | n or mean | % or SD | n or mean | % or SD | n or mean | % or SD |
| Arrival at WTC disaster site | ≤ 48 hours | 6,338 | 61.6 | 6,338 | 61.6 | - | - | ||
| > 48 hours | 3,868 | 37.6 | - | - | 3,868 | 37.6 | - | - | |
| Missing | 78 | 0.8 | - | - | - | - | 78 | 0.8 | |
| Age on 9/11 | Years | 39.7 | 8.7 | 39.4 | 8.2 | 40.4 | 9.3 | 39.6 | 10.1 |
| Sex | Female | 1,505 | 14.6 | 721 | 11.38 | 771 | 19.93 | 13 | 16.67 |
| Male | 8,779 | 85.4 | 5,617 | 88.62 | 3097 | 80.07 | 65 | 83.33 | |
| Ethnicity/race | Non-Latino/Black | 1.289 | 12.5 | 854 | 13.47 | 425 | 10.99 | 10 | 12.82 |
| Non-Latino/White | 5,612 | 54.6 | 3,724 | 58.76 | 1850 | 47.83 | 38 | 48.72 | |
| Latino/any race | 3,086 | 30.0 | 1,552 | 24.49 | 1507 | 38.96 | 27 | 34.62 | |
| Non-Latino/Other | 230 | 2.2 | 163 | 2.57 | 64 | 1.65 | 3 | 3.85 | |
| Missing | 67 | 0.7 | 45 | 0.71 | 22 | 0.57 | - | - | |
| Height | cm | 173.7 | 9.4 | 175.2 | 8.6 | 171.4 | 10.1 | 172.6 | 10.3 |
| BMI category | Normal | 1,484 | 14.4 | 818 | 12.91 | 654 | 16.91 | 12 | 15.38 |
| Overweight | 4,625 | 45.0 | 2,765 | 43.63 | 1826 | 47.21 | 34 | 0.33 | |
| Obese | 4,175 | 40.6 | 2,755 | 43.47 | 1388 | 35.88 | 32 | 41.03 | |
| Cohort entry period | 2002–2005 | 6,218 | 60.5 | 3,708 | 58.50 | 2473 | 63.93 | 37 | 47.44 |
| 2006–2008 | 2,708 | 26.3 | 1,704 | 26.89 | 978 | 25.28 | 26 | 33.33 | |
| 2009+ | 1,358 | 13.2 | 926 | 14.61 | 417 | 10.78 | 15 | 19.23 | |
| Smoking status | Never smoker | 6,075 | 59.1 | 3,857 | 60.86 | 2172 | 56.15 | 46 | 58.97 |
| Former smoker | 2,580 | 25.1 | 1,560 | 24.61 | 1001 | 25.88 | 19 | 24.36 | |
| Current smoker | 1,434 | 13.9 | 816 | 7.93 | 606 | 5.89 | 12 | 0.12 | |
| Missing | 195 | 1.9 | 105 | 1.66 | 89 | 2.30 | 1 | 1.28 | |
| Pre-WTC occupation group | Construction | 2,716 | 26.4 | 1,186 | 18.71 | 1524 | 39.40 | 6 | 7.69 |
| BCM&IRG† | 1,061 | 10.3 | 517 | 8.16 | 539 | 13.93 | 5 | 6.41 | |
| Other | 2,193 | 21.3 | 1,181 | 18.63 | 950 | 24.56 | 62 | 79.49 | |
| Protective | 4,314 | 42.0 | 3,454 | 54.50 | 855 | 22.10 | 5 | 6.41 | |
| WTC exposure duration | <60 days | 4,897 | 47.6 | 3,225 | 50.88 | 1665 | 43.05 | 7 | 8.97 |
| >60 days | 5,321 | 51.7 | 3,113 | 49.12 | 2202 | 56.93 | 6 | 7.69 | |
| Missing | 66 | 0.6 | - | - | 1 | 0.03 | 65 | 83.33 | |
| Bronchodilator response | Absent | 8,121 | 79.0 | 4,991 | 78.75 | 3071 | 79.40 | 59 | 75.64 |
| Present | 1,537 | 15.0 | 939 | 14.82 | 583 | 15.07 | 15 | 19.23 | |
| Missing | 626 | 6.1 | 408 | 3.97 | 214 | 2.08 | 4 | 0.04 | |
| Probable Metsyn‡ | 0–1 criteria | 8,377 | 81.5 | 5,188 | 81.86 | 3130 | 80.92 | 59 | 75.64 |
| 2–4 criteria | 1,888 | 18.4 | 1,143 | 18.03 | 727 | 18.80 | 18 | 23.08 | |
| Missing | 19 | 0.2 | 7 | 0.11 | 11 | 0.28 | 1 | 1.28 | |
| Heart rate | ≤ 90 bpm | 10,002 | 97.3 | 6,166 | 97.29 | 3763 | 97.29 | 73 | 93.59 |
| > 90 bpm | 254 | 2.5 | 156 | 2.46 | 95 | 2.46 | 3 | 3.85 | |
| Missing | 28 | 0.3 | 16 | 0.25 | 10 | 0.26 | 2 | 2.56 | |
| Eosinophil count | ≤ 300/mcl | 8,221 | 79.9 | 5,151 | 81.27 | 3009 | 77.79 | 61 | 78.21 |
| > 300/mcl | 2,042 | 19.9 | 1,179 | 18.60 | 847 | 21.90 | 16 | 20.51 | |
| Missing | 21 | 0.2 | 8 | 0.13 | 12 | 0.31 | 1 | 1.28 | |
| Neutrophil count | ≤ 6000/mcl | 7,573 | 73.6 | 4,649 | 73.35 | 2873 | 74.28 | 51 | 65.38 |
| > 6000/mcl | 2,690 | 26.2 | 1,681 | 26.52 | 983 | 25.41 | 26 | 33.33 | |
| Missing | 21 | 0.2 | 8 | 0.13 | 12 | 0.31 | 1 | 1.28 | |
BCM&IRG: buildings and grounds cleaning and maintenance, and electrical, telecommunications and other installation and repair groups
Probable Metsyn: probable metabolic syndrome
Unadjusted comparisons (Table OS2) showed that low FVC was associated with our main WTC occupational exposure indicator, arrival within 48 hours at the disaster site, but sex modified the effect, so that the effect was restricted to men (OR 1.43, 95% CI 1.30, 1.58). All the covariates were also associated, except for cumulative WTC exposure duration, smoking status at each visit, and eosinophil count. The association of early arrival at the WTC site for men was confirmed after adjustment for covariates (ORadj 1.29, 95% CI 1.17, 1.43, see Table OS2). The multivariable analysis confirmed all the unadjusted associations, except for cohort entry period. There were no significant interactions between WTC early arrival and occupational exposure duration, age, probable MetSyn, or smoking status at each visit on its effect on low FVC.
Discussion
In this 16-year longitudinal study, we estimated the prevalence of low FVC, the most frequently reported ventilatory impairment pattern seen in this diverse occupational WTC cohort, and its increase over time. We demonstrate for the first time an association between more intense occupational WTC dust, as suggested by early arrival (within 48 hours) at the WTC disaster site[1] and low FVC. This association is independent from risk factors for adverse respiratory outcomes in this[7] and other cohorts[27], such as overweight and obesity, current smoking, bronchodilator response[7], having a pre-WTC occupational category other than construction, high peripheral blood neutrophil counts, meeting at least 2 indicators suggestive of the metabolic syndrome[18], and having a higher heart rate[28]. We confirmed a previous observation[1] of the relative lack of significance of the association of adverse respiratory health effects with WTC exposure duration in this cohort.
This is the first study to focus on the predominant spirometric abnormality of the WTC responders and, accordingly, to restrict the analyses to spirometries with a minimum of 6 seconds of forced exhalatory time, besides acceptable reproducibility criteria (quality grades). The low FVC prevalence in this WTC cohort substantially exceeds the 8.2% and 7.1% estimates among participants aged 40–59 in NHANES III in 1988–1994, and 2007–2010, respectively[29], and that of obstruction. Low FVC (when not explained by true restriction) is emerging as a phenotype of chronic airway disease[30–32] and has been associated with significant morbidity[33–41] and mortality[38, 42]. Quantitative chest computed tomography data from other studies[39], and our own[43], demonstrated evidence suggestive of proximal airway inflammation in individuals with low FVC. Those results do not exclude distal airway disease[44] and, indeed, other lines of evidence have suggested that low FVC impairment by spirometry[45] or in response to bronchial challenge testing[46] may result from loss of lung units in parallel distally to obstructed bronchioles. Additionally, unadjusted impulse oscillometric data in a WTC-exposed community resident and worker case series reported evidence of increased distal airway resistance[47]. Although low FVC is often a stable disease state, it has also been shown to be sometimes a transitional state to and from both normal lung function and COPD, respectively[48]. Low FVC can also result from true restriction. While no evidence of an increased incidence of interstitial lung disease has been documented in the WTC occupational cohorts, in subsets with chest CT scans[6], there is evidence of mostly mild interstitial lung abnormalities in a small proportion of these workers, which warrant continued longitudinal observation, but are unlikely to explain the observed prevalence of low FVC. The observation of the effect restricted to men, the majority (85.4%) of our cohort, may be explained by the relative small number of women, or residual confounding by another variable.
Low FVC (unrelated to true restriction) is not generally recognized as associated with occupational exposures[9], although previous occupational studies (e.g., among grain elevator workers[49]) had already demonstrated it. Our study provides additional support for that association, but also finds a relatively normal age-related mean rate of longitudinal expiratory flow decline, which is consistent with a single “hit and shift” trajectory, as reported in WTC occupational cohorts[7, 8, 50]. That seemingly normal mean age-related longitudinal expiratory flow decline is not surprising in a population who was not heavily smoking at baseline[1, 43] and whose smoking prevalence seems to have declined over time[43], but it also hides significantly divergent trajectories with accelerated decline and unexpected gain in subsets of the cohort[7].
Our study had the added advantage of examining one of the largest, and most sociodemographically diverse occupational WTC cohorts[19]. This cohort has the richest spirometry data set and is unique in that more than 80% of the subjects had bronchodilator responsiveness testing since 2002, usually at their baseline examination, and irrespective of clinical status. The spirometry quality requirements for our study sought to exclude suboptimal performance, reproducibility, expiratory effort, and (uniquely in the occupational WTC studies to date) short (< 6 sec) forced exhalatory time. We also adjusted longitudinally for substantial and highly prevalent potential confounders (notably, obesity and smoking), and for many metabolic and cardiovascular risk factors that have been reported in association with low FVC[9, 33–36]. Selection bias due to differential loss to follow-up is a possible but unlikely explanation for our findings, given the observed differences between subjects who were and were not included in this analysis.
Study limitations include the lack of pre-WTC lung function data in the vast majority of subjects, as well as a suitable unexposed comparison population. We also lacked total lung capacity measurements to exclude true restriction in all subjects with low FVC, as plethysmography is not part of the surveillance program. CT imaging is similarly not part of the surveillance program, but available data suggests only mild interstitial lung abnormalities in about 10% of a subset of that subcohort[6]. We lacked detailed pre-WTC occupational exposure data. In a previous study with a subset of this cohort, we demonstrated that those pre-WTC occupational exposures (e.g., to asbestos) are indeed potentially relevant, and can be associated with CT scan abnormalities such as pleural thickening[6], but not lung nodules[51]. Similar to essentially all WTC-related studies, we lack direct toxicant exposure data, as the exposure hazards were grossly underestimated[52], and detailed exposure studies were extremely limited in size[53]. The latter and clinical data[1], in turn, support the empirically derived occupational exposure indicators based on early arrival at the disaster site. A clinical study in a small subset of this cohort[1] had already reported unadjusted association of WTC-related lower airway disease with arrival at the WTC disaster site within 48 hours (before the first rain, that in all likelihood helped settle dust), and the lack of association of WTC exposure duration with this adverse respiratory outcome. Finally, although there are still some differences in the definition of low FVC impairment across studies[9], the best designed amongst them generally share requirements for both reduction in FVC and exclusion of obstruction in their definition (whether using a fixed percentage or statistical lower limit of normal to define them), while they may or may not require a concomitant FEV1 reduction[9, 32]. Our results did not vary with the inclusion of the latter criterion (data not presented), and we focused our efforts on the more important[9], and unprecedented requirement (among large occupational WTC studies)[54] of >6 sec forced exhalatory times for all spirometries.
In conclusion, we demonstrated that occupational WTC exposure intensity, as indicated by arrival at the disaster site within the first 48 hours, was associated with low FVC, by far the most prevalent spirometric abnormality in this diverse cohort of WTC workers and volunteers, and the high prevalence of that abnormality is not only persisting but increasing after 16 years of follow up, independently from obesity, smoking, and other potential risk factors.
Supplementary Material
Highlights.
A reduced FVC without obstruction (low FVC) is a highly prevalent chronic airway phenotype
Low FVC is the most common spirometric abnormality in former WTC workers
Suboptimal effort, short exhalatory time, and obesity can cause low FVC
Low FVC was independently associated with early arrival at the WTC disaster site among men in this cohort
Acknowledgements
The authors would like to thank all participants in this study, and the staff of the Mount Sinai WTC Health Program Clinical Center of Excellence, and the WTC General Responders Cohort Data Center. We also acknowledge the able support of Horacio Romero as clinical research coordinator.
Footnotes
Conflict of interest disclosures:
This work was supported by cooperative agreements No. U01 OH011300 (AN, PI), U01 OH010401 and U01 OH011697 (RED, PI), and contract 200-2017-93325 (WTC General Responders Cohort Data Center, RGL, PI) from the Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health (CDCP/NIOSH). The authors had no other relevant financial conflict of interest. The contents of this article are the sole responsibility of the authors and do not necessarily represent the official views of the CDCP/NIOSH.
References
- [1].de la Hoz RE, Shohet MR, Chasan R, Bienenfeld LA, Afilaka AA, Levin SM, Herbert R, Occupational toxicant inhalation injury: the World Trade Center (WTC) experience, Int Arch Occup Environ Health 81 (2008) 479–485. 10.11007/s00420-007-0240-x. [DOI] [PubMed] [Google Scholar]
- [2].de la Hoz RE, Occupational lower airway disease in relation to World Trade Center inhalation exposure, Curr Opin Allergy Clin Immunol 11 (2011) 97–102. 10.11097/ACI.0b013e3283449063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Prezant DJ, Weiden M, Banauch GI, McGuinness G, Rom WN, Aldrich TK, Kelly KJ, Cough and bronchial responsiveness in firefighters at the World Trade Center site, N Engl J Med 347 (2002) 806–815. 10.11056/NEJMoa021300. [DOI] [PubMed] [Google Scholar]
- [4].Herbert R, Moline J, Skloot G, Metzger K, Barron S, Luft B, Markowitz S, Udasin I, Harrison D, Stein D, Todd AC, Enright P, Stellman JM, Landrigan PJ, Levin SM, The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program, Environ Health Perspect 114 (2006) 1853–1858. 10.11289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wisnivesky JP, Teitelbaum S, Todd AC, Boffeta P, Crane M, Crowley L, de la Hoz RE, Dellenbaugh C, Harrison D, Herbert R, Kim H, Jeon Y, Kaplan J, Katz C, Levin S, Luft B, Markowitz S, Moline JM, Ozbay F, Pietrzak RH, Shapiro M, Sharma V, Skloot G, Southwick S, Stevenson L, Udasin I, Wallenstein S, Landrigan PJ, Persistence of multiple illnesses in September 11 rescue workers, Lancet 378 (2011) 888–897. 10.11016/S0140-6736(11)61180-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].de la Hoz RE, Weber J, Xu D, Doucette JT, Liu X, Carson DA, Celedón JC, Chest CT scan findings in World Trade Center workers, Arch Environ Occup Health 74 (2018) 263–270. 10.11080/19338244.2018.1452712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].de la Hoz RE, Liu X, Doucette JT, Reeves AP, Bienenfeld LA, Wisnivesky JP, Celedón JC, Lynch DA, San José Estépar R, Increased airway wall thickness is associated with adverse longitudinal first-second forced expiratory volume trajectories of former World Trade Center workers, Lung 196 (2018) 481–489. 10.11007/s00408-018-0125-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Skloot GS, Schechter CB, Herbert R, Moline JM, Levin SM, Crowley LE, Luft BJ, Udasin IG, Enright PL, Longitudinal assessment of spirometry in the World Trade Center Medical Monitoring Program, Chest 135 (2009) 492–498. Erratum in Chest 2009; 135(4):1114, 10.1016/S0012-3692(09)60282-8. . [DOI] [PubMed] [Google Scholar]
- [9].Godfrey MS, Jankowich MD, The vital capacity is vital: epidemiology and clinical significance of the restrictive spirometry pattern, Chest 149 (2016) 238–251. 10.11378/chest.15-1045. [DOI] [PubMed] [Google Scholar]
- [10].Wan ES, Fortis S, Regan EA, Hokanson J, Han MK, Casaburi R, Make BJ, Crapo JD, DeMeo DL, Silverman EK, Longitudinal phenotypes and mortality in preserved ratio impaired spirometry in the COPDGene study, Am J Respir Crit Care Med 198 (2018) 1397–1405. 10.11164/rccm.201804-0663OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jones RL, Nzekwu MM, The effects of body mass index on lung volumes, Chest 130 (2006) 827–833. 10.11378/chest.130.3.827. [DOI] [PubMed] [Google Scholar]
- [12].Webber MP, Lee R, Soo J, Gustave J, Hall CB, Kelly K, Prezant D, Prevalence and incidence of high risk for obstructive sleep apnea in World Trade Center-exposed rescue/recovery workers, Sleep Breath 15 (2011) 283–294. 10.11007/s11325-010-0379-7. [DOI] [PubMed] [Google Scholar]
- [13].Flegal KM, Carroll MD, Ogden CL, Curtin LR, Prevalence and trends in obesity among US adults, 1999–2008, JAMA 303 (2010) 235–241. 10.11001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- [14].Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM, Prevalence of overweight and obesity in the United States, 1999–2004, JAMA 295 (2006) 1549–1555. [DOI] [PubMed] [Google Scholar]
- [15].Venkateshiah SB, Ioachimescu OC, McCarthy K, Stoller JK, The utility of spirometry in diagnosing pulmonary restriction, Lung 186 (2008) 19–25. 10.11007/s00408-007-9052-8. [DOI] [PubMed] [Google Scholar]
- [16].Weiden MD, Naveed B, Kwon S, Cho SJ, Comfort AL, Prezant DJ, Rom WN, Nolan A, Cardiovascular biomarkers predict susceptibility to lung injury in World Trade Center dust-exposed firefighters, Eur Respir J 41 (2013) 1023–1030. 10.11183/09031936.00077012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zeig-Owens R, Singh A, Aldrich TK, Hall CB, Schwartz T, Webber MP, Cohen HW, Kelly KJ, Nolan A, Prezant DJ, Weiden MD, Blood leukocyte concentrations, FEV1 decline, and airflow limitation - a 15-year longitudinal study of World Trade Center-exposed firefighters, Ann Am Thorac Soc 15 (2018) 173–183. 10.11513/AnnalsATS.201703-276OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Chen WL, Chung-Ching W, Wu LW, Kao TW, Chan JYH, Chen YJ, Yang YH, Chang YW, Peng TC, Relationship between lung function and metabolic syndrome, PLoS One 9 (2014) e108989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Woskie SR, Kim H, Freund A, Stevenson L, Park BY, Baron S, Herbert R, Siegel de Hernandez M, Teitelbaum S, de la Hoz RE, Wisnivesky JP, Landrigan P, World Trade Center disaster: assessment of responder occupations, work locations, and job tasks, Am J Ind Med 54 (2011) 681–695. 10.11002/ajim.20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].de la Hoz RE, Occupational asthma and lower airway disease in former World Trade Center workers and volunteers, Curr Allergy Asthma Rep 10 (2010) 287–294. 10.11007/s11882-010-0120-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hankinson JL, Odencratz JR, Fedan KB, Spirometric reference values from a sample of the general U.S. population, Am J Respir Crit Care Med 159 (1999) 179–187. 10.11164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- [22].American Thoracic Society, Standardization of spirometry, 1994 update, Am J Respir Crit Care Med 152 (1995) 1107–1136. 10.11164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- [23].Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CPM, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J, Standardisation of spirometry, Eur Respir J 26 (2005) 319–338. 10.11183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- [24].Enright PL, Skloot GS, Cox-Ganser JM, Udasin IG, Herbert R, Quality of spirometry performed by 13,599 participants in the World Trade Center Worker and Volunteer Medical Screening Program, Respir Care 55 (2010) 303–309. [PubMed] [Google Scholar]
- [25].Austin PC, Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research, Communications in Statistics - Simulation and Computation 38 (2009) 1228–1234. 10.11080/03610910902859574. [DOI] [Google Scholar]
- [26].Zwirevich CV, ller NLM, Conventional and high-resolution computed tomography of chronic infiltrative lung disease, in: Simmons DH, Tierney DF (Eds.), Current Pulmonology, Mosby-Year Book, Inc., St. Louis, 1992, pp. 193–220. [Google Scholar]
- [27].Schenck EJ, Echevarria GC, Girvin FG, Kwon S, Comfort AL, Rom WN, Prezant DJ, Weiden MD, Nolan A, Enlarged pulmonary artery is predicted by vascular injury biomarkers and is associated with WTC-lung injury in exposed fire fighters: a case–control study, BMJ Open 4 (2014) e005575 10.11136/bmjopen-2014-005575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Naveed B, Weiden MD, Kwon S, Gracely EJ, Comfort AL, Ferrier N, Kasturiarachchi KJ, Cohen HW, Aldrich TK, Rom WN, Kelly K, Prezant DJ, Nolan A, Metabolic syndrome biomarkers predict lung function impairment: a nested case-control study, Am J Respir Crit Care Med 185 (2011) 392–399. 10.11164/rccm.201109-1672OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB, Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination surveys from 1988–1994 to 2007–2010, Chest 143 (2013) 1395–1406. 10.11378/chest.12-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Prime FJ, Scadding JG, Blood-gas and spirometric findings in chronic bronchitis and asthma, Lancet 291 (1968) 1372 10.11016/S0140-6736(68)92069-2. [DOI] [Google Scholar]
- [31].Bouhuys A, van de Woestijne KP, Restrictive versus obstructive ventilatory impairment, Lancet 292 (1968) 352 10.11016/s0140-6736(68)90561-8. [DOI] [PubMed] [Google Scholar]
- [32].Adibi A, Sadatsafavi M, Looking at the COPD spectrum through “PRISm”, Eur Respir J 55 (2020) 1902217 10.11183/13993003.02217-2019. [DOI] [PubMed] [Google Scholar]
- [33].Engstrom G, Lind P, Hedblad B, Wollmer P, Stavenow L, Janzon L, Lindgarde F, Lung function and cardiovascular risk: relationship with inflammation-sensitive plasma proteins, Circulation 106 (2002) 2555–2560. [DOI] [PubMed] [Google Scholar]
- [34].Engstrom G, Hedblad B, Nilsson P, Wollmer P, Berglund G, Janzon L, Lung function, insulin resistance and incidence of cardiovascular disease: a longitudinal cohort study, J Intern Med 253 (2003) 574–581. [DOI] [PubMed] [Google Scholar]
- [35].Johnston AK, Mannino DM, Hagan GW, Davis KJ, Kiri VA, Relationship between lung function impairment and incidence or recurrence of cardiovascular events in a middle-aged cohort, Thorax 63 (2008) 599–605. 10.11136/thx.2007.088112. [DOI] [PubMed] [Google Scholar]
- [36].Hickson DA, Burchfiel CM, Liu J, Petrini MF, Harrison K, White WB, Sarpong DF, Diabetes, impaired glucose tolerance, and metabolic biomarkers in individuals with normal glucose tolerance are inversely associated with lung function: the Jackson Heart Study, Lung 189 (2011) 311–321. 10.11007/s00408-011-9296-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Mannino DM, McBurnie MA, Tan W, Kocabas A, Anto J, Vollmer WM, Buist AS, Restricted spirometry in the Burden of Lung Disease Study, Int J Tuberc Lung Dis 16 (2012) 1405–1411. 10.15588/ijtld.12.0054. [DOI] [PubMed] [Google Scholar]
- [38].Guerra S, Sherrill DL, Venker C, Ceccato CM, Halonen M, Martinez FD, Morbidity and mortality associated with the restrictive spirometric pattern: a longitudinal study, Thorax 65 (2010) 499–504. 10.11136/thx.2009.126052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Wan ES, Hokanson JE, Murphy JR, Regan EA, Make BJ, Lynch DA, Crapo JD, Silverman EK, Clinical and radiographic predictors of GOLD-unclassified smokers in the COPDGene study, Am J Respir Crit Care Med 184 (2011) 57–63. 10.11164/rccm.201101-0021OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Jankowich M, Elston B, Liu Q, Abbasi S, Wu WC, Blackshear C, Godfrey M, Choudhary G, Restrictive spirometry pattern, cardiac structure and function, and incident heart failure in African Americans - the Jackson Heart Study, Ann Am Thorac Soc 15 (2018) 1186–1196. 10.11513/AnnalsATS.201803-184OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Leone N, Courbon D, Thomas F, Bean K, Jego B, Leynaert B, Guize L, Zureik M, Lung function impairment and metabolic syndrome: the critical role of abdominal obesity, Am J Respir Crit Care Med 179 (2009) 509–516. 10.11164/rccm.200807-1195OC. [DOI] [PubMed] [Google Scholar]
- [42].Lee HM, Le H, Lee BT, Lopez VA, Wong ND, Forced vital capacity paired with Framingham Risk Score for prediction of all-cause mortality, Eur Respir J 36 (2010) 1002–1006. 10.11183/09031936.00042410. [DOI] [PubMed] [Google Scholar]
- [43].Weber J, Reeves AP, Doucette JT, Jeon Y, Sood A, San José Estépar R, Celedón JC, de la Hoz RE, Quantitative CT evidence of airway inflammation in World Trade Center workers and volunteers with low FVC spirometric pattern Lung 198 (2020) 555–563. 10.11007/s00408-020-00350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Nakano Y, Wong JC, de Jong PA, Buzatu L, Nagao T, Coxson HO, Elliott WM, Hogg JC, Pare PD, The prediction of small airway dimensions using computed tomography, Am J Respir Crit Care Med 171 (2005) 142–146. 10.11164/rccm.200407-874OC. [DOI] [PubMed] [Google Scholar]
- [45].Guerry-Force ML, Müller NL, Wright JL, Wiggs B, Coppin C, Paré PD, Hogg JC, A comparison of bronchiolitis obliterans with organizing pneumonia, usual interstitial pneumonia, and small airways disease, Am Rev Respir Dis 135 (1987) 705–712. 10.11164/arrd.1987.135.3.705. [DOI] [PubMed] [Google Scholar]
- [46].Gibbons WJ, Sharma A, Lougheed D, Macklem PT, Detection of excessive bronchoconstriction in asthma, Am J Respir Crit Care Med 153 (1996) 582–589. 10.11164/ajrccm.153.2.8564102. [DOI] [PubMed] [Google Scholar]
- [47].Berger KI, Reibman J, Oppenheimer BW, Vlahos I, Harrison D, Goldring RM, Lessons from the World Trade Center disaster: airway disease presenting as restrictive dysfunction, Chest 144 (2013) 249–257. 10.11378/chest.12-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Sood A, Petersen H, Qualls C, Meek PM, Vazquez-Guillamet R, Celli BR, Tesfaigzi Y, Spirometric variability in smokers: transitions in COPD diagnosis in a five-year longitudinal study, Respir Res 17 (2016) 147 10.11186/s12931-016-0468-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Chan-Yeung M, Dimich-Ward H, Enarson DA, Kennedy SM, Five cross-sectional studies of grain elevator workers, Am J Epidemiol 136 (1992) 1269–1279. 10.11093/oxfordjournals.aje.a116435. [DOI] [PubMed] [Google Scholar]
- [50].Aldrich TK, Gustave J, Hall CB, Cohen HW, Webber MP, Zeig-Owens R, Cosenza K, Christodoulou V, Glass L, Al Othman F, Weiden MD, Kelly KJ, Prezant DJ, Lung function in rescue workers at the World Trade Center after 7 years, N Engl J Med 362 (2010) 1263–1272. 10.11056/NEJMoa0910087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Sigel KM, Xu D, Weber J, Wisnivesky JP, Celedón JC, de la Hoz RE, The prevalence of pulmonary nodules on computed tomography in World Trade Center rescue and recovery workers, Ann Am Thorac Soc 17 (2020) 125–128. 10.11513/AnnalsATS.201907-517RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Wallingford KM, Snyder EM, Occupational exposures during the World Trade Center disaster response, Toxicol Ind Health 17 (2001) 247–253. 10.11191/0748233701th112oa. [DOI] [PubMed] [Google Scholar]
- [53].Geyh AS, Chillrud S, Williams DL, Herbstman JB, Symons JM, Rees K, Ross J, Kim SR, Lim HJ, Turpin B, Breysse P, Assessing truck driver exposure at the World Trade Center disaster site: personal and area monitoring for particulate matter and volatile organic compounds during October 2001 and April 2002, J Occup Environ Hyg 2 (2005) 179–193. 10.11080/15459620590923154. [DOI] [PubMed] [Google Scholar]
- [54].Aldrich TK, Vossbrinck M, Zeig-Owens R, Hall CB, Schwartz TM, Moir W, Webber MP, Cohen HW, Nolan A, Weiden MD, Christodoulou V, Kelly KJ, Prezant DJ, Lung function trajectories in World Trade Center-exposed New York City firefighters over 13 years: the roles of smoking and smoking cessation, Chest 149 (2016) 1419–1427. 10.11016/j.chest.2015.10.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


