Abstract
PURPOSE
Infection prevention among children with cancer is a major challenge at Children Hospital Lahore (CHL), a public health care facility in Pakistan with 1,000 new pediatric cancer admissions annually. The objective has been to reduce infections through collaboration between CHL and the St Jude Children’s Hospital Global Infectious Disease program via a grant by the Sanofi Espoir foundation through the My Child Matters program. The aim of the current study was to describe the effect of the collaborative improvement strategy on existing infection prevention and control (IPC) standards at CHL.
MATERIALS AND METHODS
Our work was a prospective before-and-after study to improve IPC standards. We compared the WHO Hand Hygiene Self-Assessment Framework and four modules of the St Jude modified Infection Control Assessment Tool (ICAT) scores over a 3-year period. Our strategy included creating a multidisciplinary team of pediatric oncologists, infectious disease physicians, nurses, a microbiologist, and a data manager; engaging in monthly online IPC mentoring sessions with St Jude Children’s Hospital Global Infectious Disease program and My Child Matters mentors; performing daily inpatient health care–associated infection surveillance rounds; and performing regular hand hygiene training and compliance audits.
RESULTS
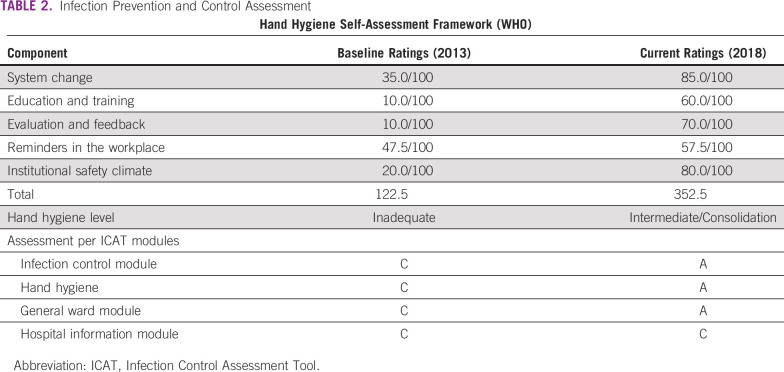
Baseline needs assessment showed health care–associated infections identified by positive blood cultures as 8.7 infections per 1,000 patient-days. Deficient hand hygiene supplies, health education measures, and bed sharing of neutropenic patients were identified as major challenges. Our hand hygiene facility level, per WHO scores, increased from Inadequate to Intermediate/Consolidation by the end of the 3-year implementation (122 v 352 WHO Hand Hygiene Self-Assessment Framework scores). The sink:bed and hand sanitizer:bed ratios improved to 1:6 and 1:1, respectively. The ICAT general infection control module increased by 40% (45 v 78 ICAT scores) and hygiene compliance improved by 20%.
CONCLUSION
Implementing a collaborative improvement strategy improved IPC standards in our center, which can be easily replicated in other pediatric oncology centers in lower- and middle-income countries.
INTRODUCTION
Pediatric patients with cancer are immunosuppressed, putting them at a higher risk of life-threating infections. The situation is worse in lower- and middle-income countries, with higher infection rates and antibiotic-resistant, gram-negative bacteria associated with increased morbidity and mortality. Infection control is an under-recognized practice in lower- and middle-income countries like Pakistan.
CONTEXT
Key Objective
There is an urgent need to improve and monitor existing infection prevention and control standards in pediatric oncology units, particularly in lower- and middle-income countries using low-cost interventions and standards tools.
Knowledge Generated
We used the St Jude oncology-adapted Infection Control and Assessment Tool (ICAT) and WHO hand hygiene modules for baseline needs evaluation as well as for ongoing progress measurement at the Children Hospital Lahore, Lahore, Pakistan, through collaboration with St Jude Global Pediatric Medicine team and Sanofi Espoir foundation via the My Child Matters project. Our hand hygiene facility level, per WHO scores, increased from “Inadequate” during the baseline assessment to “Intermediate/Consolidation” (122 v 352 Hand Hygiene Self-Assessment Framework scores). The ICAT general infection control module increased by 40% (45 v 78 ICAT score) and hygiene compliance improved by 20%.
Relevance
This is a successful model of public-private collaboration and can be easily replicated in other lower- and middle-income countries to improve their infection prevention and control standards.
The Children’s Hospital and Institute of Child Health, Lahore, is the largest, solely pediatric, government-run tertiary hospital in Pakistan. Limited infection prevention and control (IPC) measures and inadequate knowledge and monitoring, along with insufficient operational funds for IPC for the care of immune-deficient patients were identified as major risk factors for health care–associated infections (HAIs). To overcome these challenges between January 2013 till 2018, we received two 3-year grants from the Sanofi Espoir Foundation through its My Child Matters program for implementing systematic improvements to the existing IPC practices for our patients. Through the My Child Matters program, St Jude Global Infectious Disease experts helped us implement this ambitious program. Additional improvement in infrastructure was achieved through government funding, which the My Child Matters program helped us obtain through highlighting need. The study objective was to describe the effect of a collaborative improvement strategy on IPC standards in a pediatric oncology unit in a resource-limited setting.
MATERIALS AND METHODS
Methods
We used the oncology-adapted St Jude Infection Control and Assessment Tool (ICAT),1 which has four modules: hospital information, infection control, general ward, and hand hygiene. It offers a practical approach to baseline assessment, intervention, and monitoring of IPC measures.
The mandatory preliminary step was to identify a committed on-the-ground team, which consisted of pediatric hemato-oncologists (M.F., S.A., and A.H.), infection control physicians (R.K. and A.H.), an infection control officer (R.S.), and microbiology experts (H.J. and A.Z.), with local hospital administrative support (A.W.R. and M.S.). An infection control coordinator was hired solely for IPC through this project.
Formal orientation and training of this team by the St Jude Global Pediatric Medicine (SJ-GPM) team (M.A.C., M.G., M.H., and A.Z.) and mentors (M.T. and M.A.C.) was done through monthly online sessions. Training involved the completion of online educational modules, as well as training and guidance about data collection with the creation of a monthly report for discussion/evaluation during monthly live online meetings with the SJ-GPM team using Cure4Kids Web conferencing, which is St Jude’s free Web site for health professionals.
Monitoring involved the collection of patient HAI data, teaching and training sessions, hand hygiene audits, and sharing results with the St Jude team in monthly sessions using Cure4Kids. Direct observations of hand hygiene practices and ward environmental cleaning practices were performed on a weekly basis and hand hygiene audits were done on a monthly basis.
Baseline needs assessment of the unit was performed and areas that lacked good IPC measures were identified using ICAT modules and WHO Hand Hygiene Self-Assessment Framework guidelines.2 Ward infrastructure changes were made to support IPC services for patients. Workplace reminders for hand hygiene and infection control were increased.
Teaching and training sessions for the local team, patients, and parents were started with collaboration between the Global Infectious Disease program at St Jude and CHL. Training of provincial pediatricians through workshops—two per year—and seminars were also done to help improve early detection and management of infections even though this was not the primary aim of the project.
Operational Definitions
-
HAIs:
○ HAIs are infections that patients acquire during the course of receiving treatment for other conditions in a health care setting.
-
Patient days:
○ The total number of days for all patients who were admitted for an episode of care.
-
Number of infections:
○ The number of cases identified by surveillance activities during a defined timeframe in a defined population.
-
Number of infected patients:
○ The number of patients identified with infection by surveillance activities during a defined timeframe in a defined population.
-
Number of infections per 1,000 patient-days:
○ Total number of infections/Total patient days × 1,000
-
Number of infections per 100 discharges:
○ Total number of infections/Total number of discharges × 100
-
Number of infected patients per 100 discharges:
○ Total number of infected patients/Total number of discharges × 100
RESULTS
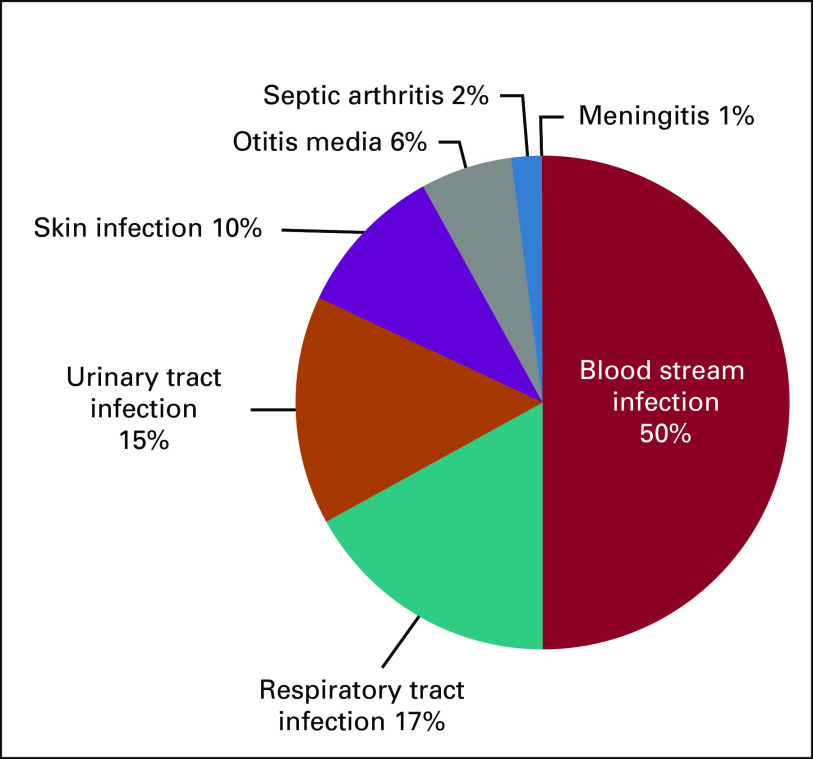
Baseline needs assessment over 6 months of culture-proven HAIs collected showed 101 HAIs in 83 patients. The number of infections per 100 discharges was 11.24, whereas the number of infected patients per 100 discharges was 9.24. Total number of infections per 1,000 patient-days was 6.66. The most common culture-proven HAI was bloodstream infection (49.5%; n = 50) and the most common organism was Klebsiella species (19%; n = 19; Fig 1 and Table 1). Of those patients with proven HAI, 40% died of the infection. There were deficient hand hygiene supplies and the sink:bed ratio was greater than 1:10. There was no dedicated/available budget for the continuous procurement of hand hygiene products—for example, alcohol-based hand rubs. There was no formal system of training of health care workers regarding hand hygiene in our facility. We did monthly audits of hand hygiene and consumption of alcohol-based hand rub was monitored every 3 months. Health care worker knowledge of IPC topics was assessed 3 monthly after education sessions. Direct observation of hand hygiene compliance was performed using the WHO Hand Hygiene Observation tool and immediate feedback was given to health care workers at the end of each hand hygiene compliance observation session. Improvements after our interventions are shown in Table 2.
FIG 1.
Percentages of infections according to the site of infection.
TABLE 1.
Percentage of Various Types of Organisms Isolated
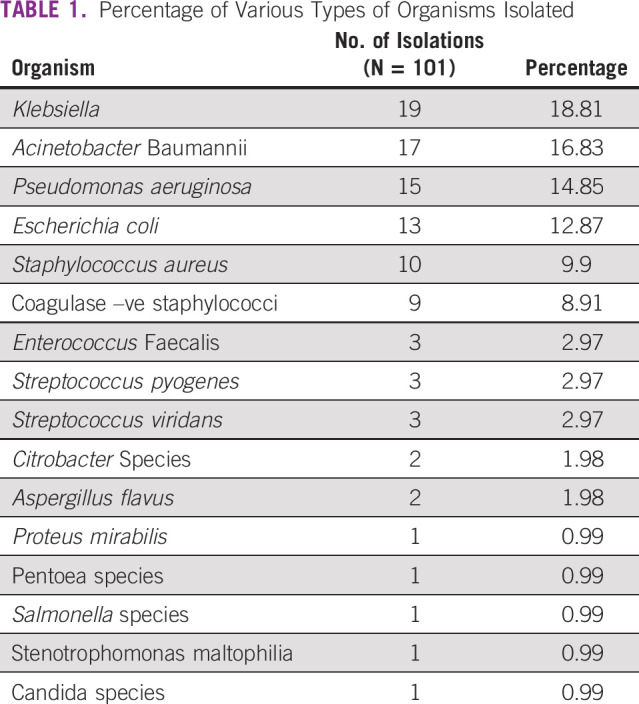
TABLE 2.
Infection Prevention and Control Assessment
Focused interventions were performed, keeping infection control a priority. Renovation of our unit was completed in 2017 with government funding, which increased the number of beds, sinks, and wash rooms, and included an allocation of a separate bay in ward for neutropenic patients as well as a chemotherapy bay. Previously, our unit consisted of a 60-bed hematology-oncology indoor block, and there was no segregation of neutropenic patients. After renovation, our unit is divided into two separate bays: a 40-bed bay (bay 1) with one patient-one bed, reserved for neutropenic patients and those receiving high-dose chemotherapy, and bay 2, which has 20 beds where mostly new patients are managed. A separate 60-bed outpatient chemotherapy bay and transfusion unit was setup, which caters to patients requiring outpatient chemotherapy as well as the delivery of intravenous antibiotics for patients with febrile neutropenia and blood and platelet transfusions. Six washrooms were added to our unit. The total number of wash basins—hand-washing stations—was increased and bed-to-bed alcohol hand rubs were fixed.
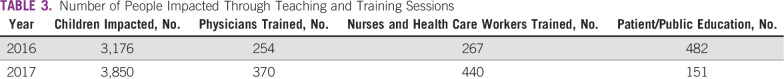
Hand hygiene supplies increased and hand hygiene audits showed progressive improvement from September 2016 to September 2018, from 40% to 90% for senior doctors, 40% to 76% for resident doctors, 35% to 75% for nurses, 25% to 64% for patient attendants, and to 71% for paramedical staff. The one patient-one bed policy was strictly followed in bay 1. The patient:alcohol hand rub ratio increased to 1:1 in bay 1. The estimated total amount of alcohol hand rub used per month increased from 72 L per month in 2016 to 160 L per month in 2018. The sink:bed ratio increased to 1:6. Hand Hygiene Self-Assessment Framework from WHO showed “inadequate hand hygiene level (score 122.5)” in 2017, which improved to “intermediate/consolidation” level (score 352.5) in March 2018. Formal assessment tools were used to document results that showed significant improvement in infection control, hand hygiene, and general ward hygiene (Table 2). Training of other local team members was done by the on-site team through mandatory IPC training for new postgraduate residents and teaching sessions for patients, families, doctors, and paramedical staff after being trained by SJ-GPM team (Table 3).
TABLE 3.
Number of People Impacted Through Teaching and Training Sessions
DISCUSSION
Pediatric cancer is a major health problem in lower- and middle-income countries, where 90% of the world’s childhood population resides.3 After infections and accidents, cancer is a major health burden. Whereas childhood cancer survival in high-income countries has dramatically improved, the prognosis is still poor in lower- and middle-income countries, where overall prognosis varies from 20% to 80% for different malignancies. High infection-related mortality further reduces survival. The magnitude of HAIs and subsequent mortality remains underestimated, primarily because HAI diagnosis is complex and surveillance activities to guide intervention require expertise and resources that are not often available in lower- and middle-income countries. As in our patients, HAIs have been shown to be a major cause of morbidity and mortality in different studies from Pakistan4 and other lower- and middle-income countries.5,6 This can be explained by deficient supportive care services, limited funds, and patient overload, resulting in bed sharing of neutropenic patients. There is a lack of availability of diagnostic and treatment facilities at other district-level medical centers/hospitals, along with malnutrition and poor socioeconomic status of our patients, which make infection control even more difficult.
Infection control strategies have now become an integral part of modern oncologic care and comprise a multilevel approach, including patient, health care environment, community, and health care worker.7 Interventions require training, funding, and education on IPC measures.8
Over the past decade, there has been a remarkable demonstration of progress and examples of good practice, where a holistic approach to managing childhood cancer—medical, social, and economic—with collaboration and partnership has had a tremendous influence on outcomes in lower- and middle-income countries.9 Many centers in other resource-constrained countries have formed long-term twinning partnerships with high-income countries to improve existing local standards10 and showed significant improvements. Twinning partnerships provide advice, expertise, support, and technology transfer from established pediatric oncology centers to developing ones to help them overcome the challenges they face.11 Hand hygiene practices constitute a cornerstone of any infection control program. There was significant improvement in hand hygiene supplies, reminders, and practices, which were frequently monitored and their success documented over time (Table 2) using the WHO Hand Hygiene Self-Assessment Framework2 and WHO’s My Five Steps of Hand Washing: before touching a patient, before cleaning/aseptic procedures, after body fluid exposure/risk of such exposure, after touching a patient, and after touching a patient’s surroundings.12 These practices must continuously be revaluated and require a multidisciplinary team, including infection control practitioners, physicians, nurses, and administrators, as well as local government involvement, particularly in public hospitals like ours. This has been successfully demonstrated in our project. Infrastructural changes would not have been possible without local administration and government support, which has proved to be invaluable.
Since this collaboration was established, there has been significant improvement in the understanding of the magnitude of the problem and concrete steps have been taken for IPC. These collaborative improvement strategies have significantly improved current IPC practices in our unit via improved surveillance, education, infrastructural changes, and, most importantly, better hand-washing practices. The St Jude oncology-adapted ICAT tool and the WHO Hand Hygiene Self-Assessment framework are useful tools with which to monitor progress as demonstrated by our study in Pakistan and in other lower- and middle-income countries.13,14
Significant challenges still exist, the majority being high patient turnover, as CHL is the only public hospital providing free treatment and diagnostic facilities to all of its patients. There is a need for shared care and regular surveillance, teaching and training of patients and families, and mobilization of government agencies and media to spread the message of the importance of IPC in improving pediatric cancer prognoses. This is an ongoing struggle and targets can be effectively achieved through continuous collaborative efforts.
In conclusion, active surveillance and good infection control practices are of critical importance in a good pediatric oncology unit. The St Jude oncology-adapted ICAT tool and WHO hand hygiene modules are effective objective tools for baseline needs evaluation as well as for ongoing progress measurement. Our project demonstrates the positive effects of simple and relatively low-cost interventions, like hand hygiene compliance, clinical surveillance, and training and education, on improving current IPC practices at CHL. This model can be easily replicated in other lower- and middle-income countries to improve IPC. On the basis of our above experience, additional targeted interventions are being developed to decrease HAI rates and infection-related morbidity and mortality in our population.
ACKNOWLEDGMENT
The authors thank Anne Gagnepain-Lacheteau, MD, leader of the My Child Matters program, not only for the financial support from the Sanofi Espoir Foundation, but also for facilitating intellectual guidance and mentorship through experts at the St Jude Children’s Research Hospital, and the Royal Marsden Hospital through the My Child Matters program.
PRIOR PRESENTATION
Presented at the 2018 World Cancer Congress, Kuala Lumpur, Malaysia, October 1-4, 2018.
SUPPORT
Funded by the Sanofi Espoir Foundation.
AUTHOR CONTRIBUTIONS
Conception and design: Mahwish Faizan, Miguela A. Caniza, Humera Javed, Aizza Zafar, Mary Munaza Taj, Maysam Homsi, Ahsan Waheed Rathore, Masood Sadiq, Miriam Gonzalez, Alia Zaidi
Administrative support: Mahwish Faizan, Miguela A. Caniza, Aizza Zafar, Masood Sadiq, Miriam Gonzalez
Provision of study materials or patients: Mahwish Faizan, Saadia Anwar, Rahat-ul-Ain Kashif, Humera Javed, Aizza Zafar
Collection and assembly of data: Mahwish Faizan, Saadia Anwar, Rahat-ul-Ain Kashif, Rabia Saleem, Aizza Zafar, Ambreen Hameed, Maysam Homsi, Ahsan Waheed Rathore, Masood Sadiq, Miriam Gonzalez
Data analysis and interpretation: Mahwish Faizan, Humera Javed, Aizza Zafar, Ambreen Hameed, Ahsan Waheed Rathore, Miriam Gonzalez
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1.Rational Pharmaceutical Management Plus . Improving Hospital Infection Control Practices—A Standardized Approach Using the Infection Control Assessment Tool and Rapid Cycle Quality Improvement: Introduction to the Infection Control CD-ROM. Arlington, VA: US Agency for International Development by the Rational Pharmaceutical Management Plus Program; 2006. [Google Scholar]
- 2.World Health Organization Hand Hygiene, Self-Assessment Framework: Introduction and User Instructions. https://www.who.int/gpsc/country_work/hhsa_framework_October_2010.pdf?ua=1
- 3.Magrath I, Steliarova-Foucher E, Epelman S, et al. Paediatric cancer in low-income and middle-income countries. Lancet Oncol. 2013;14:e104–e116. doi: 10.1016/S1470-2045(13)70008-1. [DOI] [PubMed] [Google Scholar]
- 4.Siddiqui N-u-R, Wali R, Haque A-u, et al. Healthcare-associated infections among pediatric oncology patients in Pakistan: Risk factors and outcome. J Infect Dev Ctries. 2012;6:416–421. doi: 10.3855/jidc.1705. [DOI] [PubMed] [Google Scholar]
- 5.Kafazi A, Stylianou C, Zwmas A, et al. Surveillance of healthcare-associated infections rates in hematology-oncology patients. J Integr Oncol. 2017;6:1000200. [Google Scholar]
- 6.Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet. 2011;377:228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 7.Ariza-Heredia EJ, Chemaly RF. Update on infection control practices in cancer hospitals. CA Cancer J Clin. 2018;68:340–355. doi: 10.3322/caac.21462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Galindo C, Friedrich P, Morrissey L, et al. Global Challenges in pediatric oncology. Curr Opin Pediatr. 2013;25:3–15. doi: 10.1097/MOP.0b013e32835c1cbe. [DOI] [PubMed] [Google Scholar]
- 9.Israels T, Challinor J, Howard S, et al. Treating children with cancer worldwide: Challenges and interventions. Pediatrics. 2015;136:607–610. doi: 10.1542/peds.2015-0300. [DOI] [PubMed] [Google Scholar]
- 10.Ribeiro RC, Antillon F, Pedrosa F, et al. Global pediatric oncology: Lessons from partnerships between high-income countries and low- to mid-income countries. J Clin Oncol. 2016;34:53–61. doi: 10.1200/JCO.2015.61.9148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hopkins J, Burns E, Eden T. International twinning partnerships: An effective method of improving diagnosis, treatment and care for children with cancer in low-middle income countries. J Can Pol. 2013;1:e8–e19. [Google Scholar]
- 12.World Health Organization . SAVE LIVES: Clean Your Hands—WHO’s global annual call to action for health workers. Geneva, Switzerland: World Health Organization; 2017. who.int/gpsc/5may/ [Google Scholar]
- 13.Kilpatrck C, Tartari E, Gayet-Ageron A, et al. Global hand hygiene improvement progress: Two surveys using the WHO Hand Hygiene Self-Assessment Framework. J Hosp Infect. 2018;100:202–206. doi: 10.1016/j.jhin.2018.07.036. [DOI] [PubMed] [Google Scholar]
- 14.Sharma R, Sharma M, Koushal V. Compliance to hand hygiene world health organization guidelines in hospital care. Int J Prev Med. 2014;5:127–128. [PMC free article] [PubMed] [Google Scholar]