Abstract
Congenital disorders of glycosylation (CDG) are a group of genetic, mostly multisystem disorders, which often involve the central nervous system. ALG3-CDG is one the some 130 known CDG. Here we report two siblings with a severe phenotype and intrauterine death. Whole-exome sequencing revealed two novel variants in ALG3: NM_005787.6:c.512G>T (p.Arg171Leu) inherited from the mother and NM_005787.6:c.511C>T (p.Arg171Trp) inherited from the father.
Subject terms: Genetics, Diseases
Introduction
Congenital disorders of glycosylation (CDG) are a group of inherited disorders characterized by deficient glycosylation [1]. They are mostly multisystem disorders often involving the central nervous system [2–5]. ALG3-CDG is a rare disorder, with only 23 patients reported so far [2–13]. ALG3 adds the 6th mannose to the growing dolichol-linked oligosaccharide in the ER [2, 14]. Here we report two siblings with a severe malformation syndrome and intrauterine death.
Materials and methods
Genetic analysis
Genomic DNA was extracted from the muscle tissue of the fetuses and from peripheral blood of their parents. Whole-exome sequencing (WES) and Sanger sequencing were performed according to standard procedures.
Western blotting
Muscle tissues from the patients and a control were washed with phosphate-buffered saline and western blot analysis was performed according to standard procedures.
Results
Clinical report
We report two siblings with severe multisystem dysmorphism who were born to healthy parents. The mother stated that she was never exposed to alcohol, warfarin, or other drugs. The present study was approved by the hospital’s Institutional Review Board, and written informed consent was obtained from the parents. The control tissue was obtained from a healthy fetus who was born with induced labor. The tissue sample was voluntarily donated to our hospital, which is in accordance with the ethical guidelines.
Patient 1
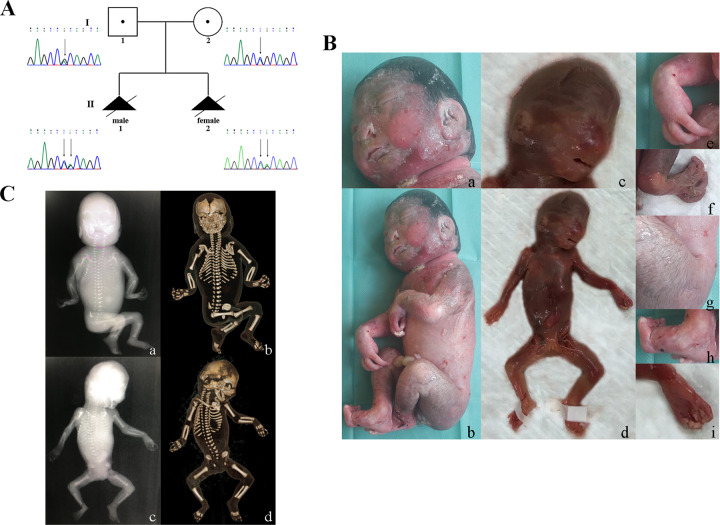
Patient 1 was a male fetus. Multiple congenital abnormalities were detected on prenatal ultrasound scan (USS) at 26 weeks of gestation. The parents decided to terminate the pregnancy at 28 weeks of gestation. The following multiple anomalies were detected: intrauterine growth restriction with short limbs, micrognathia, separation of bilateral renal collecting system, hydramnios, the hands postural fixation, increased cardiothoracic proportion, and fetal edema especially of the scalp tissue. Facial dysmorphism included eyelid ptosis, hypertelorism, short nose, flat nasal bridge, anteverted nares, thin lips, low-set, large and thick ears with malformed pinnae and micrognathia (Fig. 1b (a)). In addition, the patient had a short neck, short limbs, inverted widely spaced nipples; joint contractures, long fingers and toes, ulnar deviation of fingers, adducted thumbs, toes valgus, abnormal subcutaneous fat distribution at neck and buttock, and hirsutism (Fig. 1b (b, e–h)). Radiographic examination showed short long bones with wide metaphyses, short vertebral bodies, short ribs, a narrow thorax, paddle-shaped iliac wings, and bilateral small scapulae (Fig. 1c (a, b)). Fetal karyotype was normal.
Fig. 1.
Pedigree, photographs, and radiographic examination results of the two patients. a II 1: patient 1 (the first pregnancy of the family); II 2: patient 2 (the second pregnancy of the family). b a, b, e, g, h Pictures of patient 1. c, d, f, i Pictures of patient 2. c a, b Radiographic examination result of patient 1. c, d Radiographic examination result of patient 2
Patient 2
This patient was the sister of patient 1 and the mother’s second pregnancy. USS at 18 weeks of gestation showed scalp tissue edema and mildly short limbs. After genetic counseling, the parents decided to terminate the pregnancy at 22 weeks of gestation. Dysmorphism was similar to that in patient 1. Contractures of wrists, knees, and left elbow were milder. Hirsutism and short neck were not observed (Fig. 1b (c, d)). Radiographic examination revealed short limbs, short ribs, a narrow thorax, vertebral hypoplasia, and scoliosis (Fig. 1c (c, d)).
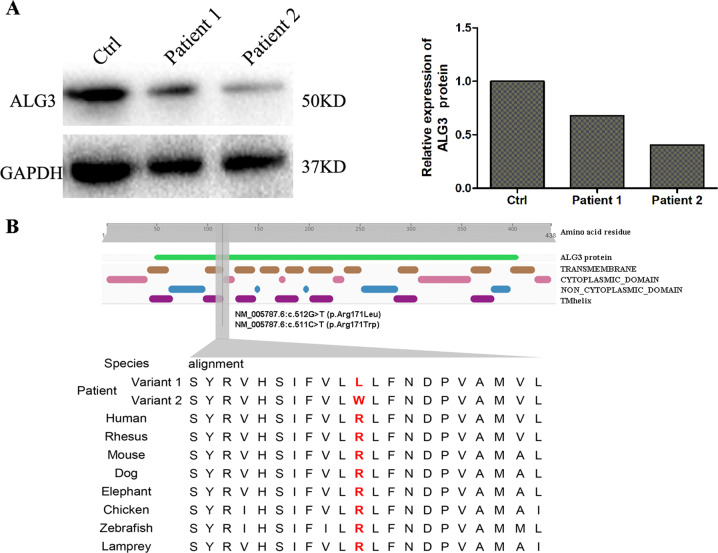
Whole-exome sequencing and Sanger sequencing results
Whole-exome sequencing showed two novel variants in the ALG3 gene: NM_005787.6:c.512G>T (p.Arg171Leu) inherited from the mother and NM_005787.6:c.511C>T (p.Arg171Trp) inherited from the father. The second patient showed the same variants. (Fig. 1a). The effect of NM_005787.6:c.512G>T (p.Arg171Leu) was predicted using the computational tools Sorting Intolerant from Tolerant (SIFT), PolyPhen‑2, and MutationTaster, M-CAP, and the results indicated that the protein variant is “damaging,” “damaging,” “disease causing,” and “damaging,” respectively. The CADD_phred score of the variant is 35. SIFT, PolyPhen‑2, MutationTaster and M-CAP predicted NM_005787.6:c.511C>T (p.Arg171Trp) to be a “damaging,” “damaging,” “disease causing,” and “damaging” variant, respectively. The CADD_phred score of this variant is 33. According to the ACMG criteria, both variants were classified as uncertain significance (PM2, PM5 and PP3).
ALG3 protein expression in the two patients
Western blot analysis of ALG3 in muscle tissues showed a clearly decreased expression in the two patients compared to that in the control (Fig. 2a).
Fig. 2.
The effects of the variants on ALG3 protein. a Relative protein expression of ALG3 in the two patients. GAPDH was used as an internal reference protein. b The location of the variants and conservation of ALG3 residues. The variants were located in ALG3 protein domain, and the amino acid residue was highly conserved
Discussion
Twenty-three ALG3-CDG patients have been reported so far. These patients showed a broad phenotypical spectrum that mainly includes dysmorphism and neurological, cardiac, skeletal, gastrointestinal, and urogenital abnormalities (summary of reported patients in Table 1). The phenotypes of our patients were already extremely severe in utero and resembled those of the patients reported by Lepais et al. [3] and Sun et al. [10]. The patient described by Sun et al. died at 19 days and showed multiple dysmorphisms with prominent cerebral, cerebellar, skeletal, cardiac, pulmonary, urogenital, hepatic, and pancreatic involvement. Lepais et al. [3] reported similarly affected siblings. In one, the abnormalities were detected at 23 weeks of gestation, which was terminated at 25 weeks. In the other, intrauterine growth retardation and short long bones were noted at 13 weeks. The parents refused to terminate the pregnancy, and the child died at 12 days due to heart failure. This severe fetal phenotype resembles that of a patient reported with ALG9-CDG (OMIM: 608776) and patients with Schneckenbecken dysplasia, also known as SLC35D1-CDG (OMIM: 269250).
Table 1.
ALG3 genetic defects and clinical features of present and reported patients
| Current study | Körner et al. Stibler et al. | Denecke et al. | Schollen et al. | Sun et al. | Kranz et al. | Rimel-la‐Le‐Huu et al. | Riess et al. | Lepais et al. | Fiumara et al. | Alsubhi et al. | Himmelreich et al. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 2 | 1 | 1 | 1 | 2 | 3 | 4 |
| Gene mutation | c.368G>T/ c.367C>T | c.368G>T/ c.367C>T | c.353G>A | c.160_1–96del | c.796C>T | c.512G>A | c.470T>A | c.116-C>T/c.512G>A | c.206T>C/c.626T>C | c.286G>A | c.564_566del/c.1125G>A plus c.1127del | c.512G>A | c.160_1–96del | c.1263G>A | c.350G>C/c.286G>A | c.296+4-A>G(c.197_2–96del)/c.1037-A>G | |||
| Protein change | p.R123L/ p.R123W | p.R123L/ p.R123W | p.G118D | p.V54Fs-X66* | p.R266C | p.R171Q | p.M157K | p.P39L /p.R171Q | p.I69T/p.M209T | p.G96R | p.l189del/p.M375I + p.P376Lf-s*92 | p.R171Q | See report | p.W421* | p.R117P/p.G96R | p.A65Fs-X42*/p.N346S | |||
| Gender | M | F | M | M | F | F | M | F | M | F | M | M | F | F | 3 F, 4 M | M | F | F | M |
| Pregnancy | Abnormal | Abnormal | Normal | Normal | Normal | Abnormal | n.d. | n.d. | Normal | Normal | Normal | Abnormal | Abnormal | n.d. | n.d. | Normal | Normal | Normal | Normal |
| Consanguinity | − | − | − | n.d. | n.d. | − | n.d. | n.d. | − | − | − | − | − | n.d. | - | + | + | - | - |
| Amniotic fluid | Hydramnios | n.d. | n.d. | n.d. | Oligohydramnios | n.d. | n.d. | n.d. | − | − | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | |
| Intrauterine growth restriction (IUGR) | + | + | − | n.d. | − | + | n.d. | n.d. | − | − | − | + | n.d. | n.d. | - | - | - | - | |
| Birth weight | n.d. | n.d. | 4150 g | 4700 g (>97th centile) | 3440 g (85th centile) | 3250 g (25th–50th centile) | n.d. | n.d. | 3790 g (>90th centile) | 2760 g | 2920 g (10th centile) | 755 g (−0.5 SD) | 2870 g (50th percentile) | 2550 g (50th centile) | n.d. | Normal | >97th centile | n.d. | Normal |
| Birth length | n.d. | n.d. | 54 cm | 48 cm (75th centile) | 52 cm (90th centile) | 50 cm (50th centile) | n.d. | n.d. | 50 cm (50th–90th centile) | n.d. | 47 cm (10th centile) | n.d. | n.d. | n.d. | n.d. | Normal | >97th centile | n.d. | Normal |
| Hc | n.d. | n.d. | 36 cm | 36 cm (75th centile) | 31.5 cm (5th centile) | 31 cm (<3rd centile) | n.d. | n.d. | 34 cm (50th centile) | Normal | 33 cm (10th centile) | n.d. | n.d. | n.d. | n.d. | Normal | Normal | n.d. | 34.5 cm −2sd |
| Microcephaly | n.d. | n.d. | Present at 4 months | <3rd centile by 5 years | <3rd centile by 4 years | <3rd centile at birth | + (at birth) | + (at birth) | <3rd centile by 5 years | <3rd centile by 10 months | <3rd centile by 4 months | + | + | + | +(4),-(1),n.d.(2) | + | + | - | n.d. |
| Micrognathia | + | + | n.d. | n.d. | + | + | n.d. | n.d. | + | n.d. | n.d. | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Ocular ptosis | + | + | n.d. | n.d. | + | n.d. | n.d. | n.d. | − | + | + | n.d. | n.d. | n.d. | n.d. | + | n.d. | n.d. | n.d. |
| Hypertelorism | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | − | + | + | + | + | n.d. | n.d. | n.d. | n.d. | + | n.d. |
| Short nose | + | + | n.d. | n.d. | n.d. | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Flat nose bridge | + | + | n.d. | n.d. | n.d. | + | n.d. | n.d. | + | + | + | − | − | n.d. | n.d. | + | n.d. | n.d. | n.d. |
| Anteverted nares | + | + | n.d. | n.d. | n.d. | + | n.d. | n.d. | − | − | − | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Thin lip | + | + | n.d. | n.d. | + | + | n.d. | n.d. | + | − | + | + | + | + | n.d. | n.d. | n.d. | n.d. | n.d. |
| Abnormality of the ear | + | + | + | n.d. | n.d. | + | + | + | + | + | + | + | + | + | n.d. | + | + | n.d. | n.d. |
| Short neck | + | - | n.d. | n.d. | n.d. | + | n.d. | n.d. | n.d. | n.d. | n.d. | + | n.d. | + | n.d. | n.d. | n.d. | n.d. | n.d. |
| Short limbs | + | + | − | n.d. | n.d. | + | − | − | − | n.d. | n.d. | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Inverted wide-spaced nipples | + | + | − | n.d. | n.d. | + | + | + | − | n.d. | − | + | + | n.d. | −(7) | − | − | − | n.d. |
| Flexed joint | + | + | n.d. | n.d. | n.d. | + | + | + | n.d. | n.d. | n.d. | + | + | n.d. | n.d. | n.d. | n.d. | + | n.d. |
| Long fingers and toes | + | + | n.d. | n.d. | n.d. | + | n.d. | n.d. | + | n.d. | n.d. | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Ulnar deviation of fingers | + | + | n.d. | n.d. | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | + | + | n.d. | n.d. | n.d. | n.d. | n.d. |
| Adducted thumbs | + | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | + | n.d. |
| Lateral deviation of toes | + | + | n.d. | n.d. | n.d. | + | n.d. | n.d. | n.d. | n.d. | n.d. | + | + | + | n.d. | n.d. | n.d. | n.d. | n.d. |
| Abnormal subcutaneous fatty distribution | + | n.d. | − | n.d. | n.d. | + | n.d. | n.d. | − | − | − | + | + | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Hirsutism | + | − | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. | − | − | − | − | n.d. | n.d. | n.d. | n.d. | n.d. | n.d. |
| Status | Induced labor | Induced labor | Alive at 12 months | Alive at 6 years | Alive at 4 years | Died at 19 days of sepsis | Alive at 9 years | Alive at 7 years | Alive at 5 years | Alive at 21 years | Alive at 15 years | n.d. | n.d. | Died at age 22 months | Neonatal death | Alive at 2 years and 7 months | Alive at 14 months | Died at age 3.5 years | Alive at 6 years |
| Other phenotypic features | separation of bilateral renal collecting system | Limb normal | Limb normal | Limb normal | Pregnancy history was unremarkable | Pregnancy history was unremarkable | Skeletal dysplasia | Limb abnormalities | Limb abnormalities | Limb abnormalities | Limb abnormalities | ||||||||
| Glycosylation pattern | Accumulation of the LLO intermediate; abnormal of N-glycosylation | Accumulation of the LLO intermediate; hypoglycosylated glycoproteins | Accumulation of the truncated LLO species | Accumulate glycans the size of Man5 GlcNAc2 | Accumulation of truncated Man5-GlcNAc2 oligosaccharide in addition to the mature Glc3Man9GlcNAc2 oligosaccharide | Serum transferrin IEF showed a type 1 pattern | Accumulation of the truncated Man5GlcNAc2 oligosaccharide | Serum Tf IEF showed a type 1 pattern | IEF of Patient Tf revealed a type I pattern. Accumulation of Man5GlcNAc2-PP-dolichol | ||||||||||
F Female, M Male, n.d. Non-detected, LLO lipid-linked oligosaccharide, Tf serum transferrin, IEF isoelectric focusing.
In conclusion, our cases expand the gene variant database of ALG3-CDG. In addition, we provide a new prenatal genotype-phenotype correlation of ALG3-CDG, which may be beneficial for the future prenatal diagnosis of other CDG cases.
Acknowledgements
We are grateful to the patients and their family for providing samples and clinical histories.
Funding
This research was supported in part by the 345 Talent Project to YL and National Natural Science Foundation of China (81701462 to YL) and National Key R&D Program of China (2018YFC1002900 to YL).
Author contributions
YB and SGZ performed the research and analyzed and interpreted the data. YB and HQ drafted the manuscript. HL, ZTZ, and YSW helped in sample collection. CXL performed phenotyping of patients. YL and CQ helped in analysis and interpretation of ES data. HKJ provided technical support. YB, HL, ZTZ, YSW, YL, JLL, and CQ were involved in scientific discussion and offered suggestions. CQ and YL conceived and designed the study, revised the manuscript, and provided final approval of the manuscript.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chang IJ, He M, Lam CT. Congenital disorders of glycosylation. Ann Transl Med. 2018;6:477. doi: 10.21037/atm.2018.10.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rimella-Le-Huu A, Henry H, Kern I, Hanquinet S, Roulet-Perez E, Newman CJ, et al. Congenital disorder of glycosylation type Id (CDG Id): phenotypic, biochemical and molecular characterization of a new patient. J Inherit Metab Dis. 2008;31:S381–S6. doi: 10.1007/s10545-008-0959-x. [DOI] [PubMed] [Google Scholar]
- 3.Lepais L, Cheillan D, Frachon SC, Hays S, Matthijs G, Panagiotakaki E, et al. ALG3-CDG: report of two siblings with antenatal features carrying homozygous p.Gly96Arg mutation. Am J Med Genet A. 2015;167A:2748–54. doi: 10.1002/ajmg.a.37232. [DOI] [PubMed] [Google Scholar]
- 4.Kranz C, Sun L, Eklund EA, Krasnewich D, Casey JR, Freeze HH. CDG-Id in two siblings with partially different phenotypes. Am J Med Genet A. 2007;143A:1414–20. doi: 10.1002/ajmg.a.31796. [DOI] [PubMed] [Google Scholar]
- 5.Alsubhi S, Alhashem A, Faqeih E, Alfadhel M, Alfaifi A, Altuwaijri W, et al. Congenital disorders of glycosylation: the Saudi experience. Am J Med Genet A. 2017;173:2614–21. doi: 10.1002/ajmg.a.38358. [DOI] [PubMed] [Google Scholar]
- 6.Denecke J, Kranz C, von Kleist-Retzow JC, Bosse K, Herkenrath P, Debus O, et al. Congenital disorder of glycosylation type Id: clinical phenotype, molecular analysis, prenatal diagnosis, and glycosylation of fetal proteins. Pediatr Res. 2005;58:248–53. doi: 10.1203/01.PDR.0000169963.94378.B6. [DOI] [PubMed] [Google Scholar]
- 7.Körner C, Knauer R, Stephani U, Marquardt T, Lehle L, von Figura K. Carbohydrate deficient glycoprotein syndrome type IV: deficiency of dolichyl-P-Man:Man(5)GlcNAc(2)-PP-dolichyl mannosyltransferase. EMBO J. 1999;18:6816–22. doi: 10.1093/emboj/18.23.6816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riess S, Reddihough DS, Howell KB, Dagia C, Jaeken J, Matthijs G, et al. ALG3-CDG (CDG-Id): clinical, biochemical and molecular findings in two siblings. Mol Genet Metab. 2013;110:170–5. doi: 10.1016/j.ymgme.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 9.Stibler H, Stephani U, Kutsch U. Carbohydrate-deficient glycoprotein syndrome–a fourth subtype. Neuropediatrics. 1995;26:235–7. doi: 10.1055/s-2007-979762. [DOI] [PubMed] [Google Scholar]
- 10.Sun L, Eklund EA, Chung WK, Wang C, Cohen J, Freeze HH. Congenital disorder of glycosylation id presenting with hyperinsulinemic hypoglycemia and islet cell hyperplasia. J Clin Endocrinol Metab. 2005;90:4371–5. doi: 10.1210/jc.2005-0250. [DOI] [PubMed] [Google Scholar]
- 11.Fiumara A, Barone R, Del Campo G, Striano P, Jaeken J. Electroclinical features of early-onset epileptic encephalopathies in congenital disorders of glycosylation (CDGs) JIMD Rep. 2016;27:93–9. doi: 10.1007/8904_2015_497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Himmelreich N, Dimitrov B, Geiger V, Zielonka M, Hutter A-M, Beedgen L, et al. Novel variants and clinical symptoms in four new ALG3-CDG patients, review of the literature, and identification of AAGRP-ALG3 as a novel ALG3 variant with alanine and glycine-rich N-terminus. Hum Mutat. 2019;40:938–51.. doi: 10.1002/humu.23764. [DOI] [PubMed] [Google Scholar]
- 13.Schollen E, Grünewald S, Keldermans L, Albrecht B, Körner C, Matthijs G. CDG-Id caused by homozygosity for an ALG3 mutation due to segmental maternal isodisomy UPD3(q21.3-qter) Eur J Med Genet. 2005;48:153–8. doi: 10.1016/j.ejmg.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 14.Denecke J, Kranz C, Kemming D, Koch H-G, Marquardt T. An activated 5’ cryptic splice site in the human ALG3 gene generates a premature termination codon insensitive to nonsense-mediated mRNA decay in a new case of congenital disorder of glycosylation type Id (CDG-Id) Hum Mutat. 2004;23:477–86. doi: 10.1002/humu.20026. [DOI] [PubMed] [Google Scholar]