Abstract
Summary and background data
Recent coronavirus outbreak and “stay at home” policies have accelerated the implementation of virtual healthcare. Many surgery departments are implementing telemedicine to enhance remote perioperative care. However, concern still arises regarding the safety of this modality in postoperative follow-up after gastrointestinal surgery. The aim of the present prospective study is to compare the use of telemedicine clinics to in-person follow-up for postoperative care after gastrointestinal surgery during COVID-19 outbreak.
Methods
Prospective study that included all abdominal surgery patients operated since the COVID-19 outbreak. On discharge, patients were given the option to perform their postoperative follow-up appointment by telemedicine or by in-person clinics. Demographic, perioperative, and follow-up variables were analyzed.
Results
Among 219 patients who underwent abdominal surgery, 106 (48%) had their postoperative follow-up using telemedicine. There were no differences in age, gender, ASA score, and COVID-19 positive rate between groups. Patients who preferred telemedicine over in-person follow-up were more likely to have undergone laparoscopic surgery (71% vs. 51%, P = 0.037) and emergency surgery (55% vs. 41%; P = 0.038). Morbidity rate for telemedicine and in-person group was 5.7% and 8%, (P = 0.50). Only 2.8% of patients needed an in-person visit following the telemedicine consult, and 1.9% visited the emergency department.
Conclusions
In the current pandemic, telemedicine follow-up can be safely and effectively performed in selected surgical patients. Patients who underwent laparoscopic and emergency procedures opted more for telemedicine than in-person follow-up.
Keywords: Telemedicine, Postoperative care, COVID-19 pandemic
Telemedicine is the use of electronic information and video communication technologies to provide and support healthcare when distance separates participants [1]. Due to the widespread adoption of technology in all fields, telemedicine is increasingly being used and becoming a promising tool in healthcare [2]. Among its benefits, excellent clinical outcomes, enhanced patient satisfaction, increased accessibility, reduced cost and reduced waiting times have been described [1].
Recent coronavirus outbreak [3] has accelerated the implementation of virtual health platforms and pushed its limits to the edge. “Stay at home” policies such as lockdowns, curfews and social distancing protocols have forced patients to stay away from hospitals and postpone surgical consultations [2, 4]. Telemedicine has been reported useful in preoperative and postoperative surgical consultations and has even been used for intraoperative mentoring with successful outcomes for patients [5]. Despite the reported benefits, most surgeons do not rely on telemedicine advantages and fear to misdiagnose postoperative complications. Patients undergoing emergency surgery during COVID outbreak are of particular interest since they are a high-risk population with increased surgical complications [6]. Most of reported postoperative telemedicine studies were performed from the surgeon’s office to another medical facility (clinics, hospitals, etc.) with the nurse’s presence to aid the patient. To our knowledge, no reports have been made regarding results of the use of telemedicine for postoperative care for patients at home during the COVID-19 pandemic [7].
Due to the current context and the urgent need to maintain social distance, reorganize human resources and keep patients away from clinical areas; our gastrointestinal surgery team implemented a contingency strategy based on telemedicine for postoperative patient care. This study aims to report our results using telemedicine consults for postoperative care and compare them to in-person follow-up after gastrointestinal surgery during COVID-19 outbreak.
Patient and methods
COVID cases increased in our country since mid-March, so patients operated since March 15th who had undergone follow-up before July 19th were included in this prospective study. All patients were offered either a telemedicine follow-up or an in-person visit for postoperative care. Appointments were scheduled online or by telephone. Patients were educated and encouraged to use telemedicine to avoid visits to clinical areas. They were always able to contact a surgical nurse to request an in-person visit with the on-call surgeon anytime during the first postoperative month and as many times as needed. When needed, vitals and weight were reported by patients using commercial devices. Patients with tubes or drains in place at the time of discharge and prolonged hospital stay (> 14 days) were excluded.
A telemedicine platform for video conference was developed by the innovation team of our institution (Red de Salud UC-Christus). The platform allowed access to patient medical records and the possibility to write prescriptions online. Patient information was protected by security passwords following local ethical and legal protocols.
Patients and the attending surgeon connected on a face to face video-call via the online platform, which they accessed from their homes or office. Examination of the surgical site was performed using the camera or pictures sent to the attending surgeon. If the surgeon decided that a physical examination was needed, an immediate in-person visit was scheduled.
A prospective database of all cases operated during COVID-19 pandemic was performed. Demographic, perioperative and follow-up variables were registered. Continuous variables were reported as mean ± standard deviation and categorical variables as percentages. Mann–Whitney, Chi-square and ANOVA tests were used as needed in SPSS and a P value < 0.05 was considered significant.
The study was approved by the Institutional Review Board and informed consent was obtained from all individual participants involved in this work.
Results
A total of 219 patients underwent abdominal surgery during the study period and were included for analysis, 47% had an emergency procedure and 22% had an oncological diagnosis.
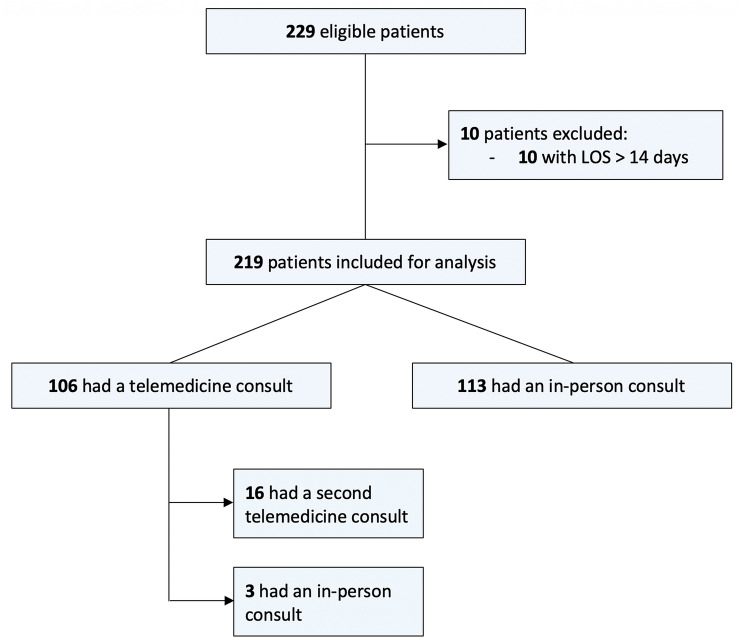
Telemedicine follow-up was preferred by 106 (48%) patients and 113 (52%) preferred an in-person postoperative consult (Fig. 1). The mean interval between surgery and first consult was 15.4 (± 8.5) days for the telemedicine group and 17.4 (± 10.4) days for the in-person follow-up group.
Fig. 1.
Eligible patients for analysis. A total of 219 patients were included for analysis: 106 had a telemedicine postoperative visit and 113 an in-person consult
Patient demographics and perioperative variables are summarized in Table 1. There were no differences in age, gender, ASA score, oncologic surgery, and length of stay between patients followed by telemedicine or by in-person visits.
Table 1.
Demographic, perioperative and follow-up variables
| Telemedicine; n (%) | In-person; n (%) | P value | |
|---|---|---|---|
| Patients | 106 (48%) | 113 (52%) | |
| Male | 48 (45%) | 54 (48%) | 0.710 |
| Age; y mean (SD) | 49 (± 20) | 53 (± 16) | 0.089 |
| Oncological diagnosis | 19 (17.9%) | 29 (25.7%) | 0.167 |
| ASA classification | 0.675 | ||
| I–II | 100 (94%) | 108 (96%) | |
| III or more | 6 (6%) | 5 (4%) | |
| Length of stay; d mean (SD) | 2.3 (± 1.8) | 3.3 (± 3.3) | 0.388 |
| Surgical approach | 0.037 | ||
| Open | 20 (19%) | 44 (39%) | |
| Laparoscopic | 76 (71%) | 58 (51%) | |
| Endoscopic | 5 (5%) | 4 (4%) | |
| Hybrid | 5 (5%) | 7 (6%) | |
| Surgery type | 0.038 | ||
| Elective | 48 (45%) | 67 (59%) | |
| Urgent/emergency | 58 (55%) | 46 (41%) | |
| Morbidity | 6 (5.7%) | 9 (8%) | 0.499 |
| Elective | 2 (1.9%) | 6 (5.3%) | 0.319 |
| Urgency/emergency | 4 (3.8%) | 3 (2.7%) | 0.939 |
| COVID (+) | 9 (8.5%) | 6 (5.3%) | 0.351 |
| Days to visit 1; d mean (SD) | 15.4 (± 7.5) | 17.4 (± 10.4) | 0.083 |
ASA American Society of Anesthesiologists, SD standard deviation, y years, d days
Overall postoperative morbidity rate for telemedicine group was 5.7% and 8% for the in-person group (5.7% vs 8%; P = 0.50) (Table 1). No mortality was reported. In the morbidity subgroup analysis, there were no differences when comparing elective (1.9% vs 5.3%; P = 0.32) and urgent/emergency (3.8% vs 2.7%; P = 0.94) surgery between both groups (Table 1). Minor and major complications rates showed no differences between telemedicine and in-person groups (6% vs 8%; P = 0.79 and 0% vs 0.9%; P > 0.99, respectively). Perioperative COVID-19 infection was reported in 9 (8.5%) of patients followed by telemedicine and 6 (5.3%) patients followed by in-person postoperative visit (P = 0.35).
Only 3 (2.8%) patients followed by telemedicine required a subsequent in-person visit to the attending surgeon. The reasons for this visit were acute diarrhea (resolved at the time of visit), removal of skin staples and patient’s preference. Two (1.9%) patients visited the emergency department (ED) following telemedicine consults within 30 days after surgery, one for COVID-19 symptoms (tested positive) and the other due to a colonic perforation secondary to peritoneal carcinomatosis. Sixteen (14.9%) patients had a second telemedicine follow-up within 30 days after surgery with no reported complications.
Four patients (3.5%) in the in-person follow-up group had a second in-person visit to the surgeon (2.8% vs 3.5%; P = 0.09), and 7 (6.2%) had a subsequent telemedicine consult. Seven patients (6.2%) visited the ED in the in-person follow-up group. The reasons for ED consult were fever, postoperative pain, respiratory symptoms, skin infection in a patient receiving chemotherapy and nephrolithiasis.
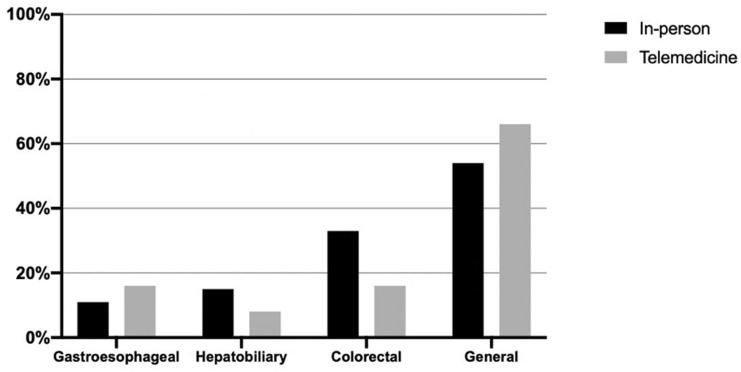
Patients who opted for telemedicine over in-person follow-up were most likely to have undergone laparoscopic surgery (71% vs 51%, P = 0.037) and emergency surgery (55% vs 41% P = 0.038). In the subgroup analysis of minimally invasive procedures (laparoscopic and endoscopic), there were no differences in age, gender, length of stay, morbidity and surgical procedures between telemedicine and in-person group (Table 2). Also, there was no difference between both groups when comparing the rate of patients who underwent gastroesophageal, hepatobiliary, colorectal and general surgical procedures (15% vs 10%, 7% vs 13%, 15% vs 29% and 62% vs 48%, respectively; P = 0.18) (Fig. 2).
Table 2.
Telemedicine versus in-person follow-up for patients who underwent laparoscopic and/or endoscopic procedures
| Telemedicine; N (%) | In-person; N (%) | P value | |
|---|---|---|---|
| Patients | 86 (58%) | 63 (42%) | |
| Age; y mean (SD) | 48.6 (± 20) | 52.3 (± 14.1) | 0.103 |
| Male | 37 (43%) | 30 (48%) | 0.578 |
| LOS; d mean (SD) | 2.3 (± 1.8) | 2.7 (± 3.1) | 0.458 |
| Morbidity | 5 (5.8%) | 5 (7.9%) | 0.609 |
| Surgical procedure | 0.201 | ||
| Appendicectomy | 26 (30%) | 12 (19%) | |
| Cholecystectomy | 26 (30%) | 20 (32%) | |
| Hernia repair | 3 (4%) | 5 (8%) | |
| Bariatric surgery | 6 (7%) | 4 (6%) | |
| Gastroesophageal | 6 (7%) | 5 (8%) | |
| Hepatobiliary | 2 (2%) | 4 (6%) | |
| Small and large bowel | 8 (9%) | 10 (14%) | |
| Exploratory laparoscopy | 2 (2%) | 0 (0%) | |
| Adhesiolysis | 1 (1%) | 3 (5%) | |
| ERCP | 6 (7%) | 1 (2%) | |
| Others | 1 (1%) | 0 (0%) | |
| Type of surgery | 0.047 | ||
| Elective | 35 (41%) | 36 (57%) | |
| Urgent/emergency | 51 (59%) | 27 (43%) |
LOS length of stay, ERCP endoscopic retrograde cholangiopancreatography, SD standard deviation, y years, d days
Fig. 2.
Type of surgical procedures. There was no difference between telemedicine and in-person groups when comparing the rate of patients who underwent gastroesophageal, hepatobiliary, colorectal and general surgery procedures (15% vs 10%, 7% vs 13%, 15% vs 29% and 62% vs 48%, respectively; P = 0.18)
Discussion
After widespread advisories for social distancing and shelter-in-place mandates, telemedicine has become an essential tool for medical attention during the COVID-19 pandemic. After years of being slowly implemented, the pandemic forced its rapid expansion to deliver remote patient care [8]. In the surgical field, recent evidence suggests high enthusiasm for telemedicine from both patients and providers. However, concerns arise in respect to the quality of care delivered and the safety of this practice for postoperative care clinics [9].
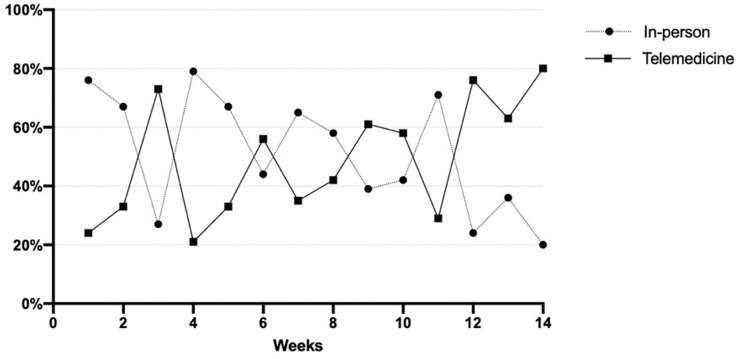
Previous experiences with telemedicine in postoperative care have demonstrated safe and effective wound care, postoperative patient education and even ileostomy output management [10, 11]. However, most patients and providers prefer in-person postoperative visits during normal times [9]. COVID-19 social distancing protocols have encouraged many patients to seek remote medical attention even after major surgery. To understand more about patient preferences and safety of telemedicine in this setting, we conducted this prospective study giving patients the option to have either a telemedicine or an in-person postoperative follow-up. To minimize the need for wound care, our surgical team was encouraged to use absorbable sutures, avoid skin staples and to attempt drain or tube removal before discharge, when possible. At the time of discharge, patients were informed and instructed on telemedicine and on the possibility to schedule an immediate surgical appointment without additional costs whenever they deemed necessary. On the first month of COVID era 70% of the patients preferred in-person follow-up but this decreased to 40% in the last month of this study, with most patients favoring telemedicine postoperative care (Fig. 3).
Fig. 3.
Evolution in time of telemedicine and in-person visits. During week 1, 25% of patients had telemedicine consults; and during week 14, 80% of patients. There were two waves of COVID-19 in our country, the first one during week 1 and the second during week 6 of our study
In the reported telemedicine series, complication rates range from 0 to 12.5% [7]. This wide range is due to heterogeneous groups of patients included in the different studies. In our series, six patients (5.7%) had postoperative complications in the telemedicine group, all classified as minor morbidity (Clavien–Dindo I or II). One patient had an abdominal infection treated with antibiotics; one had an adynamic ileus treated conservatively, which was diagnosed at the time of the telemedicine consult. One needed an analgesic catheter due to increased postoperative pain, and the last one presented fever due to a respiratory infection. Only 2.8% of patients needed an in-person consultation with an attending surgeon, and only 1.9% visited the ED following a telemedicine appointment. The reasons for a consult in the ED were COVID-19 symptoms in a patient who underwent an anorectal fistula repair and abdominal pain in an oncological patient who was operated for an incarcerated incisional hernia and presented with an abdominal infection. No patients had a misdiagnosed complication in this group. On the other hand, in the in-person follow-up group, nine patients (8%) had postoperative complications. One patient presented an episode of upper gastrointestinal bleeding needing endoscopic therapy, and the other eight were classified as minor complications (Clavien–Dindo I and II).
Even though many studies have demonstrated telemedicine safety in surgical care, it was only after COVID pandemic that it achieved worldwide acceptance with many centers implementing it in postoperative care. However, guidelines for selecting eligible patients are currently lacking. In this study, our patients decided on the follow-up modality choosing between telemedicine and in-person visit. We think this was a positive selection criterion after appropriate patient education and with no differences in postoperative outcomes [1, 6, 7]. Previously published telemedicine experiences for postoperative follow-up often include carefully selected patients who underwent elective surgeries [12–17]. In this study, 18% of the telemedicine group patients had an oncological diagnosis, and 55% underwent emergency/urgent surgery.
Additionally, in most reported series, consults were performed from the surgeon’s office to another medical facility (clinics, hospitals, etc.) with a nurse’s presence to aid the patient [14, 15, 18]. In our study, both patients and surgeons were at home or office at the time of the consult, reducing the traveling times, infrastructure needs and, especially in this period, the contagion risk.
For the integration of telemedicine in healthcare technological and legal aspects are necessary [4]. Our institutional platform provided the technological aspects with videoconference support, electronic medical record, online prescribing options, laboratory results, imaging, and pathology reports. In our country the Ministry of Health authorized telemedicine care on mid-March and implemented coverage by insurance companies. Globally, governments are still making decisions about temporary/emergent policies for the delivery of telemedicine clinics. Future efforts will need to explore country-specific insurance status and out-of-pocket costs.
Our study has several limitations. First, this is a single-institution study; therefore, these results may not be generalizable to other settings. Second, it is limited only to gastrointestinal surgery, and other surgical subspecialties may have different results in implementing telemedicine for postoperative follow-up. And finally, patients could choose between in-person or telemedicine consult after surgery; so, the telemedicine group included patients who were comfortable with this modality for different reasons, contributing to the selection bias. Despite the above, findings indicate that telemedicine postoperative follow-up can be safely and effectively performed in a selected group of surgical patients in the current pandemic context. Our experience included elective and emergency procedures reporting overall low morbidity and a low proportion of patients requiring a subsequentially in-person visit.
While further prospective studies are needed to support the safety of telemedicine in postoperative care, we found that a telemedicine protocol could be safely implemented for gastrointestinal surgery follow-up during the COVID-19 pandemic. This helped to reallocate resources and minimize patient and provider exposure to infection.
Author contributions
MJI contributed to the acquisition, analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. MI contributed to the acquisition of data, critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. RM contributed to the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. NQ contributed to the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. AB contributed to the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. MG contributed to the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. PS contributed to the interpretation of data, critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. MD contributed to the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. GU contributed to the interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. JV contributed to the interpretation of data, critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. SV contributed to the interpretation of data, critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. FC contributed to the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work. PA contributed to conception and design of the work, the analysis and interpretation of data, drafting and critical revision of the manuscript, approved the final version to be published and agree to be accountable for all aspects of the work.
Funding
No funding was received for this work.
Compliance with ethical standards
Disclosures
Drs. María J. Irarrázaval, Martin Inzunza, Rodrigo Muñoz, Nicolás Quezada, Alejandro Brañes, Mauricio Gabrielli, Pedro Soto, Martin Dib, Gonzalo Urrejola, Julian Varas, Sebastián Valderrama, Fernando Crovari and Pablo Achurra have no conflicts of interest or financial ties to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Williams AM, Bhatti UF, Alam HB, Nikolian VC. The role of telemedicine in postoperative care. Mhealth. 2018;4:11. doi: 10.21037/mhealth.2018.04.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong Z, Li N, Li D, Li J, Li B, Xiong W, et al. Telemedicine during the COVID-19 pandemic: experiences from Western China. J Med Internet Res. 2020;22(5):e19577. doi: 10.2196/19577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J Am Coll Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palomba G, Dinuzzi VP, De Palma GD, Aprea G. Management strategies and role of telemedicine in a surgery unit during COVID-19 outbreak. Int J Surg. 2020;79:189–190. doi: 10.1016/j.ijsu.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nikolian VC, Williams AM, Jacobs BN, Kemp MT, Wilson JK, Mulholland MW, et al. Pilot study to evaluate the safety, feasibility, and financial implications of a postoperative telemedicine program. Ann Surg. 2018;268(4):700–707. doi: 10.1097/SLA.0000000000002931. [DOI] [PubMed] [Google Scholar]
- 7.Gunter RL, Chouinard S, Fernandes-Taylor S, Wiseman JT, Clarkson S, Bennett K, et al. Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg. 2016;222(5):915–927. doi: 10.1016/j.jamcollsurg.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robbins T, Hudson S, Ray P, Sankar S, Patel K, Randeva H, et al. COVID-19: a new digital dawn? Digit Health. 2020;6:2055207620920083. doi: 10.1177/2055207620920083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sorensen MJ, Bessen S, Danford J, Fleischer C, Wong SL. Telemedicine for surgical consultations—pandemic response or here to stay?: A report of public perceptions. Ann Surg. 2020 doi: 10.1097/SLA.0000000000004125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Segura-Sampedro JJ, Rivero-Belenchón I, Pino-Díaz V, Rodríguez Sánchez MC, Pareja-Ciuró F, Padillo-Ruiz J, et al. Feasibility and safety of surgical wound remote follow-up by smart phone in appendectomy: a pilot study. Ann Med Surg (Lond) 2017;21:58–62. doi: 10.1016/j.amsu.2017.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bednarski BK, Slack RS, Katz M, You YN, Papadopolous J, Rodriguez-Bigas MA, et al. Assessment of ileostomy output using telemedicine: a feasibility trial. Dis Colon Rectum. 2018;61(1):77–83. doi: 10.1097/DCR.0000000000000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hwa K, Wren SM. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148(9):823–827. doi: 10.1001/jamasurg.2013.2672. [DOI] [PubMed] [Google Scholar]
- 13.Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68(4):729–735. doi: 10.1016/j.eururo.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Urquhart AC, Antoniotti NM, Berg RL. Telemedicine—an efficient and cost-effective approach in parathyroid surgery. Laryngoscope. 2011;121(7):1422–1425. doi: 10.1002/lary.21812. [DOI] [PubMed] [Google Scholar]
- 15.Costa MA, Yao CA, Gillenwater TJ, Taghva GH, Abrishami S, Green TA, et al. Telemedicine in cleft care: reliability and predictability in regional and international practice settings. J Craniofac Surg. 2015;26(4):1116–1120. doi: 10.1097/SCS.0000000000001560. [DOI] [PubMed] [Google Scholar]
- 16.Cremades M, Ferret G, Parés D, Navinés J, Espin F, Pardo F, et al. Telemedicine to follow patients in a general surgery department. A randomized controlled trial. Am J Surg. 2020;219(6):882–7. doi: 10.1016/j.amjsurg.2020.03.023. [DOI] [PubMed] [Google Scholar]
- 17.Kummerow Broman K, Roumie CL, Stewart MK, Castellanos JA, Tarpley JL, Dittus RS, et al. Implementation of a telephone postoperative clinic in an integrated health system. J Am Coll Surg. 2016;223(4):644–651. doi: 10.1016/j.jamcollsurg.2016.07.010. [DOI] [PubMed] [Google Scholar]
- 18.Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL, et al. A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare. 2014;20(8):427–430. doi: 10.1177/1357633X14555610. [DOI] [PubMed] [Google Scholar]