Abstract
Introduction
It is known that viral infections are epidemiologically prevalent and some of them are harmful to the central nervous system (CNS) due to the development of neuropsychiatric syndromes which affect the cognitive, affective, behavioral and perceptual domains.
Objective
To carry out a comprehensive analysis of the psychiatric and neuropsychiatric repercussions of COVID-19 based on epidemiological, pathophysiological and clinical foundations observed in previous and recent pandemic events, and also to make a proposition about effective therapeutic interventions to help tackle this serious public health problem, more specifically in its neuropsychiatric developments.
Method
This current literature review has utilized literature reserves and scientific search engines MEDLINE, EMBASE and Web of Science. The search terms included, “SARS-CoV-2”, “etiology,” “psychiatric and neuropsychiatric repercussions”, “severe infections” “COVID-19”. Specific choices of unique papers from each of the searches were identified. The inclusion criteria were relevance and availability of full-text. Papers were excluded on the basis of relevance and non-availability of full-text. Papers were identified in the general literature reserve as pertinent to the search terms.
Results
The main psychiatric and neuropsychiatric repercussions analyzed were depression, anxiety, post-traumatic stress disorder, psychosis, nonspecific neurological symptoms, delirium, cerebrovascular complications, encephalopathies, neuromuscular disorders, anosmia and ageusia.
Conclusion
The psychiatric and neuropsychiatric symptoms of acute respiratory syndromes can appear during or after the infectious stage. Among the risk factors pointed out for such effects are the female gender, health professionals, presence of avascular necrosis and distressing pain.
Keywords: SARS-CoV-2, Etiology, Psychiatric and neuropsychiatric repercussions, Severe infections, COVID-19
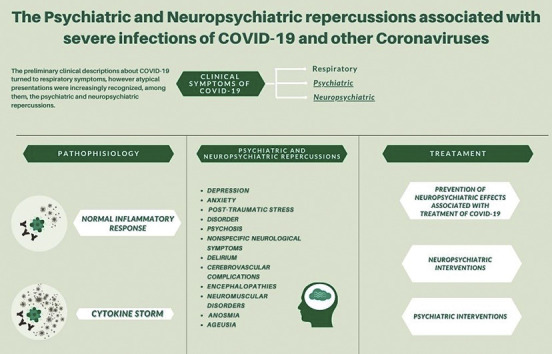
Graphical abstract
Highlights
-
•
Coping with the pandemic situation regarding COVID-19 is a significant psychiatric stressor.
-
•
The direct effects of the virus itself and the subsequent immune response of the host on the human central nervous system (CNS) are still poorly known.
-
•
Viral infections are epidemiologically prevalent and some of them are harmful to the central nervous system (CNS).
1. Introduction
Given that a very large number of individuals will be infected with SARS-CoV-2, the immediate impact on mental health could be considerable. Clinicians must be aware of the possibility of depression, anxiety, fatigue, post-traumatic stress disorder, and rarer neuropsychiatric syndromes in the aftermath (Rogers et al., 2020).
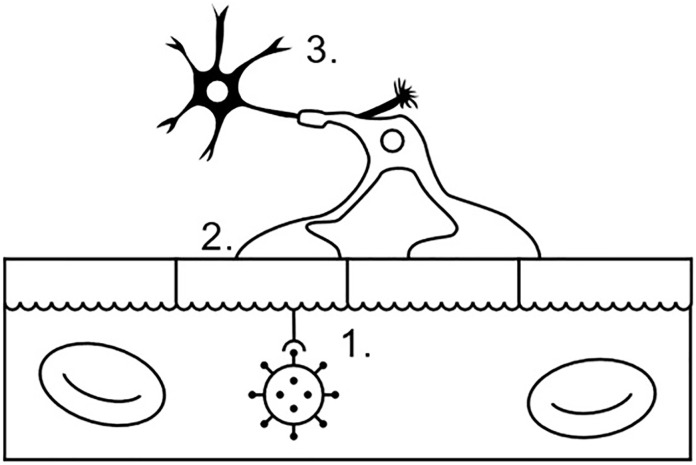
Coronaviruses (CoVs) are pleomorphic RNA viruses whose crown-shaped peplomers are 80 to 160 nM in size, with positive polarity of 27 to 32 kb, belonging to the Coronaviridae family and to the order Nidovirales. The model of the molecular structure of the coronavirus can be seen in Fig. 1 . CoVs spread pathologically in the respiratory, intestinal, hepatic and nervous systems and are considered harmful to humans since their association with acute respiratory syndromes (Sahin, 2020; Yin, 2020; Correia et al., 2020). Historically, coronaviruses have been responsible for two notable outbreaks: Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS) respectively in 2002 and 2012. Suddenly, cases of atypical pneumonia were reported in Wuhan, China, which were associated with the new coronavirus responsible for Acute Respiratory Syndrome 2 (SARS-CoV-2), later called COVID-19 (Rogers et al., 2020). The initial clinical descriptions of this infectious pathology consisted mainly of respiratory symptoms. Although COVID-19 is largely responsible for the clinical worsening of the infectious condition, atypical presentations are being increasingly recognized (Beach et al., 2020).
Fig. 1.
Entry of SARS-CoV-2 into the Nervous System.
(1. The virus is recognized by the ACE2, invades a blood-brain barrier reaches the 2. oligodendrocyte that leads to the 3. neurons.
Source: Authors (2020).
With regard to atypical presentations, coping with the pandemic situation regarding COVID-19 is a significant psychiatric stressor, due to the substantial impact on all facets of life and organizations of individuals in the social and economic sectors (Troyer et al., 2020). Evidence about the symptoms indicate that deliriums are common to acute stages of SARS, MERS and COVID-19. Psychiatric disorders such as depression, anxiety disorders, fatigue and post-traumatic stress disorder were evidenced after the acute stages in epidemics previous to coronaviruses, but the data for COVID-19 are still scarce (Rogers et al., 2020). However, in addition to the psychological distress associated with the pandemic, the direct effects of the virus itself and the subsequent immune response of the host on the human central nervous system (CNS) and the results are still poorly known (Troyer et al., 2020). In converging perspectives, it is known that viral infections are epidemiologically prevalent and some of them are harmful to the central nervous system (CNS) due to the development of neuropsychiatric syndromes which affect the cognitive, affective, behavioral and perceptual domains (Rogers et al., 2020).
Previous pandemic events suggest that neuropsychiatric symptoms manifest themselves in acute viral infection or after varying periods of time after infection. (Jasti et al., 2020). Neuropsychiatric symptoms such as insomnia, anxiety, depression, mania, psychosis, suicide and delirium marked the pandemic flu of the 18th and 19th centuries (Troyer et al., 2020; Honigsbaum, 2013; Menninger, 1926). The CNS inflammatory disorder called Encephalitis lethargica (EL) characterized by hypersomnolence, psychosis, catatonia and parkinsonism had an increase in its rates during the Spanish Flu pandemic in the 20th century. More recently, neuropsychiatric sequelae have been reported, such as narcolepsy, seizures, encephalitis, encephalopathy, Guillain-Barré syndrome (GBS) and other neuromuscular and demyelinating processes related to SARS-CoV-1, MERS and H1N1 (Troyer et al., 2020). On the other hand, the SARS-Cov-2 enters the human host cells through the agiotensin-converting enzyme 2 receptor, which has low levels of expression in the brain; however, there are preliminary evidences in vitro of the ability to replicate in neuronal cells, which differs from other previous coronaviruses (Rogers et al., 2020).
The simultaneity between the progressive expansion of new cases of COVID-19 and serious psychiatric implications is notorious. This is mainly due to the broad social impact of the pandemic situation and the government responses to social distancing and quarantines (Troyer et al., 2020). Infected and uninfected populations may be susceptible to generalized anxiety and stress in response to certain experiences. Other experiences may be specific to individuals infected by the virus, among them, the concern with the prognosis of their illness, stigma or traumatic memories of serious illnesses (Rogers et al., 2020). Fears of illness, death and uncertainty about the future are significant psychological stressors for the population, and the social isolation resulting from the loss of structured educational and work activities also threatens to worsen public mental health. This pandemic is a potential source of direct and indirect trauma for everyone, which is only further emphasized by disturbing case reports of suicide deaths related to fear of contracting or spreading COVID-19 (Troyer et al., 2020).
It is estimated that more than a third of patients with COVID-19 develop neuropsychiatric symptoms, including headache, paresthesia and disturbed consciousness, and those symptoms appear to be associated with more serious illnesses (Beach et al., 2020). Even though some authors suggest that serious neuropsychiatric implications are rare, a considerable number of individuals worldwide could be affected. Pandemics prior to influenza have been associated with long-term neuropsychiatric repercussions and, therefore, it is possible that other large-scale viral infections may cause sustained mental morbidity (Rogers et al., 2020). Therefore, we aim to carry out a comprehensive analysis of the psychiatric and neuropsychiatric repercussions of COVID-19 based on epidemiological, pathophysiological and clinical foundations observed in previous and recent pandemic events, and also to make a proposition about effective therapeutic interventions to help tackle this serious public health problem, more specifically in its neuropsychiatric developments.
2. Method
This current literature review has utilized literature reserves and scientific search engines MEDLINE, EMBASE and Web of Science. The search terms included, “SARS-CoV-2”, “etiology,” “psychiatric and neuropsychiatric repercussions”, “severe infections” “COVID-19”. Specific choices of unique papers from each of the searches were identified. The inclusion criteria were relevance and availability of full-text. Papers were excluded on the basis of relevance and non-availability of full-text. Papers were identified in the general literature reserve as pertinent to the search terms.
3. Disorders and epidemiological profiles
By the end of 2019, SARS-CoV-2 quickly spread from China to the rest of the continents (Jasti et al., 2020), corresponding to more than 4,170,000 cases and 287,399 deaths, according to the statement World Health Organization (WHO) carried out on May 13, 2020 (Zhou et al., 2020). The COVID-19 takes, thereby, a pandemic feature, whose landmark is its effects on the respiratory system and its more serious manifestation: the Severe Acute Respiratory Syndrome (Troyer et al., 2020.). Due to the ability to generate multiple infections to systemic organs (Jasti et al., 2020), the referred virus can cause damage to the kidneys, heart, liver and brain, for example (Dinakaran et al., 2020). From a neurological perspective, individuals affected by the virus have reported headache, dizziness, hypogeusia and hyposmia during the course of the disease, with intensive care patients being more likely to complain of dizziness (Zhou et al., 2020).
Along with the reported neurological impairments, neuropsychiatric sequelae are also imminent in view of the diversity of stress elements during the pandemic, such as fear of the disease, uncertainty of the future, in addition to the frequent exposure and the shortage of private protective equipment suffered by health professionals in the frontline. Thus, symptoms may appear after the infectious period: insomnia, depression, anxiety, psychosis, among other manifestations (Troyer et al., 2020). According to studies reviewed by Rogers et al., 2020, patients admitted to hospital due to SARS or MERS during the acute phase of the disease had psychiatric impairment factors: depressed mood (32.6%), anxiety (35.7%), impaired memory (34.1%) and insomnia (42%). Moreover, researches also addressed by the aforementioned meta-analysis points out the neuropsychiatric repercussion in the post-infectious period, demonstrating the persistence of depressed mood and anxiety, in addition to the development of euphoria (10.8%), irritability (12.8%), fatigue (19.3%), emotional lability (23.5%) and traumatic memories (30.4%).
As an important finding, confusion during the acute phase of SARS and MERS occurred in 27.9% of patients, suggesting that delirium is a common neurological episode among this group. Under the careful analysis of Rogers et al., 2020, the etiology and epidemiology of psychiatric factors associated with Covid-19 are multifactorial, as they result from a possibly associated brain infection or from cerebrovascular diseases, along with sentimental aspects also reported by qualitative studies, such as loneliness, boredom, frustration through isolation and concern for family health. Finally, in this same manuscript, there is a significant relationship between post-traumatic stress and population and risk factors, such as female gender, health occupation and presence of avascular necrosis and distressing pain after SARS.
The research by Guo et al., 2020 resumes the topic of the highest rates of depression and anxiety among infected patients in relation to the control group. In this light, psychiatric disorders can become more intense, since apathy and anxiety are increasing in individuals with mild cognitive impairment, while agitation and aberrant motor behavior are aggravated in Alzheimer's disease patients (Beatriz Lara et al., 2020). Other comorbidities were also found in these individuals, often with older age (on average 77.4 years), being more frequent among women (60%): hypertension (60%), dyslipidemia (52.5%) and diabetes (30%). It is also seen that the involvement of SARS-CoV-2 with neurological aspects can affect different levels of the Central and Peripheral Nervous System, in addition to causing skeletal-muscular injury, representing 36.4% of the cases considered, including impairment of consciousness, ataxia, acute cerebrovascular disease, seizure and neuropathic pain, for example (Bilbul et al., 2020). In an epidemiologically deeper approach, Dinakaran et al. (2020) reinforces a percentage value close to the one reported by Bilbul et al. (2020) regarding the neurological complaints of COVID-19 patients: 36%.
4. Physiopathology
4.1. Neuroinvasion and neurotropism
Associated with multiple impairments on the individual's mental and physical health, both in their psychiatric and neurological consequences, the action of SARS-CoV-2 and the immune response of the human Central Nervous System have been the focus of pathophysiological investigation (Troyer et al., 2020). In this light, the neuroinvasive character of the virus in question and the manifestations at central and peripheral levels suffered by the referred system are raised: headache, dizziness - most common-, reduced level of consciousness, ataxia, impaired perception of taste and smell and neuropathic pain, possibly including also injury of skeletal muscle tissue (Bilbul et al., 2020; Zhou et al., 2020). According to research by Beach et al. (2020) the emergence of this panorama, including acute encephalopathy, can reach more than a third of patients with COVID-19, in addition to delirium as a common phenomenon of the most serious infections. Moreover, a reading of the neuropsychiatric spectrum allows the association of post-infectious states with disorders, such as post-traumatic stress, depressed mood, anxiety and insomnia (Rogers et al., 2020).
Although the main clinical signs are related to respiratory function, SARS-CoV-2 is also capable of infecting cells of the Nervous System, intestinal mucosa, kidneys and lymphoid system, for example, culminating in nausea, diarrhea, vomiting, among other symptoms whose severity depends on tissue sensibility (Serrano-Castro et al., 2020; Li et al., 2020). For possible associations between SARS-CoV-2 tropism and neurological symptoms, it is necessary to understand its characteristics and its similarity to SARS-CoV. SARS-CoV-2 corresponds to a enveloped single-stranded RNA betacoronavirus, containing 29,891 nucleotides for the encoding of 9860 amino acids (Li et al., 2020). In view of this panorama, the studies by Li et al. (2020) and Zhou et al. (2020) roughly agree on the degree of similarity between pathogens: 79.5% and 89.1%, respectively, what allowed the discovery about the viral structure of these pathogens and their similarity in the infectious mechanism: interaction with Angiotensin-2 receptors (ACE-2) - abundant on the cell surface of various human organs (Li et al., 2020; Zhou et al., 2020).
Thus, also present in the cells of the Central Nervous System, it is possible that the ACE-2 receptor allows the action of SARS-CoV-2 in neuronal cells, that then activate the TMPRSS2 serine protease, allowing protein peak and, consequently, the virus entry. Such infectious mechanism can be potentiated by the infection of endothelial cells, which could cause damage to the blood-brain barrier and increase its permeability and vulnerability to SARS-CoV-2, with slow blood flow in capillaries being a possible aggravating factor for the interaction between the virus and the endothelial cells of CNS vessels, whose consequences of this interaction are cerebral edema and intracranial hypertension, for example (Li et al., 2020; Serrano-Castro et al., 2020). Furthermore, among the possibilities raised as neurological behaviors for the virus discussed, it is possible to elicit the action of SARS-COV-1 in animal experimentations, whose trajectory of the virus occurred through the respiratory tract, using peripheral nerves, such as the olfactory, to reach the SNC (Zhou et al., 2020; Troyer et al., 2020).
4.2. Neuropsychiatric pathophysiology
As discussed earlier, the spectrum of probable neurological and neuropsychiatric damage to COVID-19 patients is wide. From this perspective, the pathophysiology, although there is still a need for further studies, allows us to assume the relationship between SARS-CoV-2 mechanisms and different manifestations (Troyer et al., 2020).
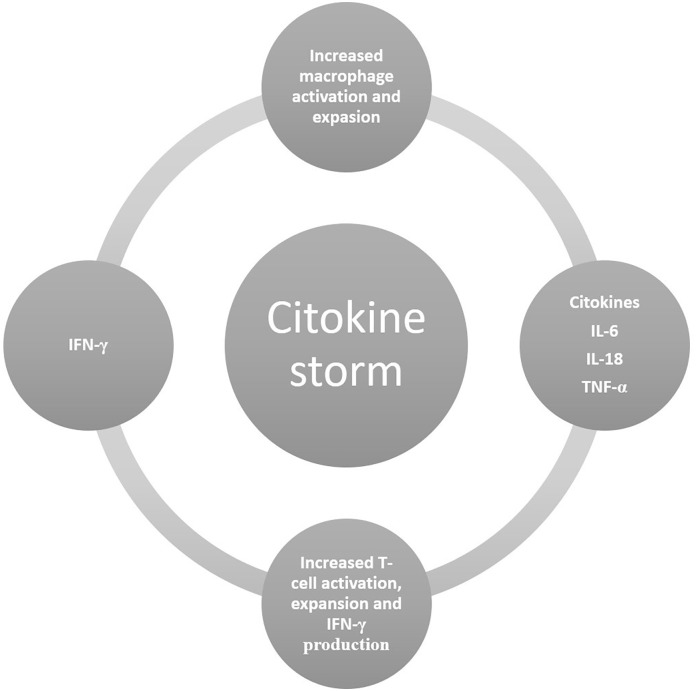
Regarding Acute Neuropsychiatric Symptoms, researches contemplated by Troyer et al. (2020), out of 217 hospitalized patients, almost half had cerebrovascular complications, encephalopathies and myalgia - commonly combine with a reduced total number of lymphocytes and high reactive C protein. Furthermore, findings in children with COVID-19 also demonstrated a drop in lymphocytes. The high signalization of granulocyte-macrophage colony-stimulating factor (GM-CSF) is also linked to the invasion of the CNS by cells derived from monocytes, which allows us to raise the research of Serrano-Castro et al. (2020) regarding inflammatory persistence and invasion of hematopoietic cells, such as lymphocytes, dendritic cells and macrophages. In relation to encephalopathy, researches considered by Troyer et al. (2020) evaluated patients with COVID-19, in Wuhan (China), with considerable presence of encephalopathy and alterations in consciousness among these. Continuing these considerations, blood tests detected increased levels of proinflammatory cytokines, such as interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α), characterizing Cytokine Storm Syndrome (CSS), in fatal COVID-19 patients. This condition, also noted by Serrano-Castro et al. (2020) reinforces these inflammatory disorders with reduced lymphocytes and increased cytokines, a condition also observed during SARS-VOC-1 infections. In addition, it is possible to raise delirium as a primary encephalopathy and harbinger of invasion of the CNS by SARS-COV-2 (Beach et al., 2020).
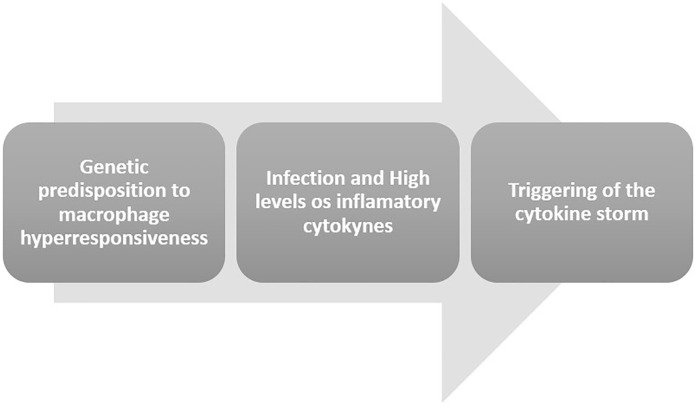
The triggering of the cytokine storm has been described in studies by Grom et al. (2016) in a multiple model of pathogenic events in rheumatic diseases. In this approach, the genetic factors and the inflammatory environment created by the underlying rheumatic disease act synergistically to reach the threshold of macrophage activation syndrome (MAS) in the presence of an infectious trigger, according to Fig. 2, Fig. 3 .
Fig. 2.
The triggering of the cytokine strom.
(Source: Authors)
Fig. 3.
Molecular components of the cytokine strom.
(Source: Authors)
Regarding anosmia and ageusia, although greater formal publications on the subject are still needed, Troyer et al. (2020) considers, according to researches included in the manuscript, that the impairment of olfactory and gustatory perception occurs through the virus-receptor interaction and use by the pathogen of these sensory pathways to reach the CNS. In turn, the transition from the subacute phase to chronic sequelae caused by SARS-COV-2 should be analyzed. Depression and anxiety are common consequences of COVID-19 outbreaks. Although these psychiatric symptoms are often attributed to proximity to infected individuals and the atypical context of quarantine, the development of stress due to difficulty in breathing due to infection can trigger the release of corticotropic hormones, hypothalamic stimulation and the production of glucocorticoids with interference on brain metabolism (Li et al., 2020; Troyer et al., 2020). Other psychiatric complications can be raised from reported episodes of detection of HCoV antibodies in patients affected by recent psychotic episodes (Troyer et al., 2020). In this light, Acute Inflammatory Demyelinating Polyneuropathy/Guillain-Barré Syndrome has been observed in individuals infected with SARS-COV-2, with case reports in China, Italy and Spain, whose presumed underlying pathophysiology is the inflammatory trigger of cytokines generated by the infection, which can also be associated with Acute Necrotizing Encephalopathy (Jasti et al., 2020).
Another pathophysiological mechanism is associated with the dysregulation of the cytokine network. Research evaluated by Troyer et al. (2020) and Serrano-Castro et al. (2020) demonstrate the upregulation of pro-inflammatory cytokines: IL-10, TNF-α, IL-6, IL-2R and CCL2, for example. In this way, organs damaged by severe states of infection can remain producing endogenous substances capable of generating chronic and systemic inflammation. In addition, the “cytokine storm” raises important questions about the degenerative chronicity in relation to the CNS specifically, given that other neurodegenerative pathologies originate from a similar mechanism, such as Parkinson's, Alzheimer's, Huntington's disease and Amyotrophic lateral sclerosis (Serrano-Castro et al., 2020). Troyer et al. (2020) highlight the exacerbated inflammatory reaction and its link with autoimmune mechanisms by COVID-19, since SARS-COV-1 and MERS-CoV present descriptions associated with autoimmune neurodegenerative syndromes.
Injuries of skeletal muscle tissue occurs by breakage and weakening of muscular skeletal system - observable by high levels of creatine kinase and lactate dehydrogenase - added to the muscle damage caused by inflammatory hyperreactivity (Jasti et al., 2020). Regarding to strokes when not associated with D-dimer (signaling particle of clot formation), a hypothesized relationship between the development of vasculitis secondary to cytokine reactions in the intracranial setting, similarly to what occurs in the triggered pathophysiology by SARS-CoV-2, is raised (Jasti et al., 2020). In regard to headaches, researches considered by Jasti et al. (2020) also highlight the relationship between inflammatory hyperreactivity as a responsible mechanism, in addition to the influence of hypoxia and changes in blood flow caused by the infection. As for seizures, they may also be secondary to the innate immune response of cytokines.
5. Main repercussions
Much has been discussed about the respiratory impacts of COVID-19. However, the disease is not limited to the respiratory system, but also affects the nervous system, with psychiatric and neuropsychiatric repercussions.
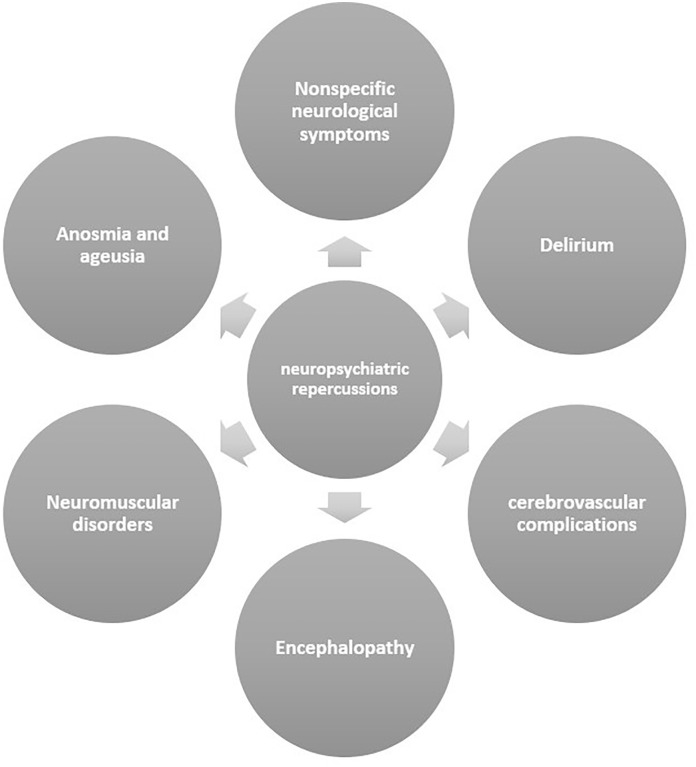
5.1. Neuropsychiatric repercussions
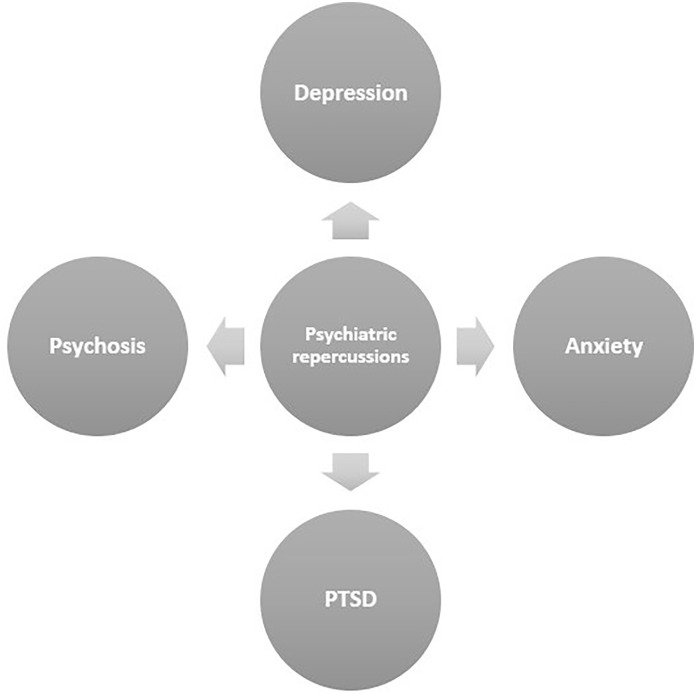
SARS-CoV-2 has been increasingly associated with neurological manifestations (for example, febrile seizures, seizures, changes in mental status and encephalitis). The neurotropic and neuroinvasive capabilities of coronaviruses in humans have been described previously, such as entry into the CNS via the olfactory bulb, causing inflammation and demyelination (Asadi-Pooya and Simani, 2020). Neuropsychiatric repercussions refer to mental disorders caused by sequelae of brain damage or disease, which can arise from direct effects of CNS infection or indirect by an immune response or medical therapy (Rogers et al., 2020). Despite limited data and studies on neuropsychiatric presentations as a result of COVID-19, it is known that some symptoms are present in the course of the disease, either by direct spread of the virus or indirectly by physiological hyperinflammation (Jasti et al., 2020). It is estimated that more than a third of patients with COVID-19 develop neuropsychiatric symptoms (Beach et al., 2020). The neurpsychiatric repercussions are summarized in Fig. 4 .
Fig. 4.
Main neuropsychiatric repercussions.
(Source: Authors)
5.2. Nonspecific neurological symptoms
Specific neurological symptoms such as seizures and cerebrovascular disorders are manifested in certain patients affected by COVID-19, in which SARS-CoV-2 neuroinvasion would partially explain respiratory failure in some cases. In contrast, nonspecific neurological symptoms can arise in patients affected by COVID-19, such as confusion and headache (Asadi-Pooya and Simani, 2020). The most described nonspecific symptoms are headache, myalgia, dizziness and fatigue (Carod Artal, 2020). In a study by Mao et al. (2020) with 214 hospitalized patients diagnosed with COVID-19 at the Hospital of Huazhong University of Science and Technology in Wuhan, China, 36.4% had neurological manifestations. The most common symptoms of CNS manifestations were dizziness (36 cases) and headache (28 cases).
5.2.1. Delirium
Delirium is a the most common neuropsychiatric presentation in patients with COVID-19, with symptomatic manifestation in 65% of patients in the intensive care unit, along with agitation and altered consciousness (Rogers et al., 2020). Beach et al. (2020) exposed a series of four cases in which patients experienced delirium as a result of infection with coronavirus. It is worth noting that three of the four cases did not have significant respiratory symptoms, but had a change in mental status as a presentation of the disease. With this rise in delirium rates as a symptom of COVID-19, it becomes necessary to assess whether changes in mental status should be incorporated into the test criteria. The pathophysiology of this mechanism remains unclear, and may be a primary manifestation, with the virus invading the nervous system, or secondary, through encephalopathy caused by inflammation or other systemic effects of the virus.
5.2.2. Cerebrovascular complications
SARS-CoV-2 infection has been reported to cause an event called cytokine storm, involving molecules that participate in the inflammatory process, produced by cells of the immune system. It is likely that this mechanism can cause cerebrovascular diseases. Furthermore, patients with severe COVID-19 have high levels of D-dimer and reduced platelets, which can lead to acute cerebrovascular events (Serrano-Castro et al., 2020; Wu et al., 2020).
5.2.3. Encephalopathy
Encephalopathy is a transient syndrome of cerebral dysfunction, with impaired level of consciousness. It is known that patients with COVID-19 can suffer from cerebral hypoxia, which is a risk factor for encephalopathy. In addition, the cytokine storm resulting from the immune inflammatory process may cause this neuropsychiatric manifestation (Carod Artal, 2020; Troyer et al., 2020). Retrospective analyzes indicate the presence of encephalopathies in one fifth of individuals affected by COVID-19 in Wuhan, China. Remarkably, plasma levels of proinflammatory cytokines were significantly higher among fatal COVID-19. This converges with the report of the cytokine storm syndrome in SARS-CoV-1, which may be associated with encephalopathy. In addition to immunological manifestations, neurocognitive deficits and mild cognitive impairment have been reported in patients affected by COVID-19 (Troyer et al., 2020).
5.2.4. Neuromuscular disorders
Muscle damage and myalgia were observed in patients with COVID-19, being manifested with elevated creatine kinase and lactate dehydrogenase levels higher than patients without muscular symptoms. Another reason for this symptom may be the cytokine storm, which can contribute to the manifestation of ataxia (Jasti et al., 2020).
5.2.5. Anosmia and ageusia
Smell and taste disorders are related to a wide variety of viral infections, including COVID-19. Out of the 59 patients with COVID-19 hospitalized in a hospital in Milan, Italy, 33.9% reported at least one taste or smell disorder, and 18.6% had both. Alterations in taste perception were more frequent before hospitalization, demonstrating that these symptoms are reasonably frequent and may precede the complete clinical appearance of the disease, requiring a careful look at these symptoms, which can represent a useful screening tool (Giacomelli et al., 2020). Formal studies have not yet been published for CoV-2-related anosmia despite an increasing number of clinical cases (Vaira et al., 2020); however, it has emerged as a screening criterion for COVID-19 in an increasing number of clinics. Experimental studies prior to those related to coronaviruses suggested that the alpha-coronavirus interrupts the ciliary nasal epithelium, a possible mechanism of olfactory dysfunction. Indeed, there is expression of the angiotensin receptors through which COVID-19 enters cells; in contrast, the specific cellular receptor subtype mediating anosmia remains uncertain (Troyer et al., 2020).
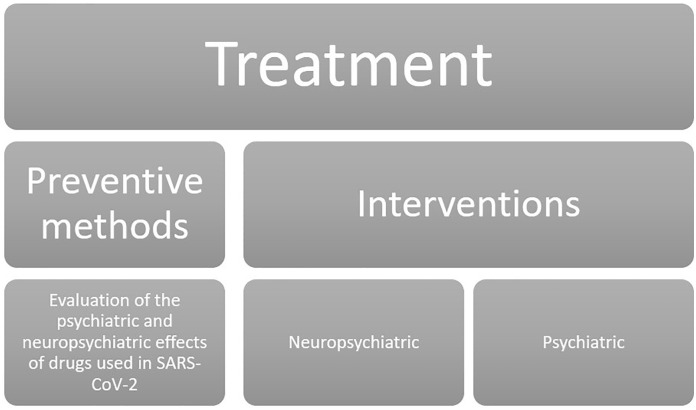
5.3. Psychiatric repercussions
It is known that during a pandemic state, the environmental stress, coupled with fear, quarantine and symptom complaints can lead to different psychiatric disorders, such as depression, anxiety, psychiatric symptoms or post-traumatic stress (Li et al., 2020). Psychiatric symptoms associated with trauma were related to coronavirus outbreaks; however, there is need for confirmation if the risks are attributable to viral infections o immune responses. Therefore, it is essential to continuously monitor such clinical signs and their repercussions associated with SARS-CoV-2 (Troyer et al., 2020). The psychiatric repercussions are summarized in Fig. 5 .
Fig. 5.
Main psychiatric repercussions.
(Source: Authors)
5.3.1. Depression
The response to infection for COVID-19 is a hyperinflammatory state in which there is an increase in the concentration of C-reactive protein, ferritin and interleukin-6, which, despite being a brief state, is likely to have a link with psychiatric problems (Rogers et al., 2020). The levels of C-reactive protein, a peripheral inflammatory indicator, correlated positively with patients who showed symptoms of depression. Thus, it is noticed that psychological suffering is something experienced by patients with COVID-19, and that inflammatory markers are related to the levels of depressive characteristics in these patients (Guo et al., 2020).
5.3.2. Anxiety
Studies suggest that the social levels of symptoms associated with anxiety increase when a serious infectious disease spreads, such as the psychological burden caused by SARS-CoV1-, in which a considerable part of the sample presented anxiety disorders. A possible cause may be related to hypochondriac concerns and fear (Furer et al., 1997; Huang and Zhao, 2020). Among the various impacts of COVID-19, fear and uncertainty about the disease can precipitate disorders, such as anxiety. It is noticed that the pandemic affects more significantly patients who have already had psychiatric disorders, which may be related to pro-inflammatory cytokines in these patients (Hao et al., 2020).
5.3.3. Post-traumatic stress disorder (PTSD)
In the post-disease stage, with SARS and MERS infections as a parameter, patients may develop traumatic memories, with manifestations of post-traumatic stress disorder. It is necessary that health professionals are aware of the possibility of psychiatric repercussions, both during the course of the disease and in the long term (Rogers et al., 2020). In addition, these symptoms can go beyond infected patients, impacting the general population. A study in Wuhan, China, one month after the outbreak of COVID-19 showed that the prevalence of PTSD in the most affected areas in China was 7%. Health services must be designed to promote the psychological well-being of the population (Liu et al., 2020).
5.3.4. Psychosis
The presence of antibodies against coronavirus strains has been reported in individuals with psychosis, although most studies focus on the history of influenza infections and their relationship to the risk of psychosis. However, an increased prevalence of antibodies against four strains of HCoV in patients with a recent episode psychosis compared with non-psychiatric controls was found, suggesting a possible relationship between infections and psychosis, which may also occur with the SARS-CoV-2 (Troyer et al., 2020). Evidences suggest that 0.9 to 4% of individuals infected with SARS-CoV-2 develop psychotic spectrum disorders (Dinakaran et al., 2020).
6. Therapeutic interventions
The challenges surrounding the treatment of COVID-19 become even more complex when referring to the involvement of the Nervous System. The dense parenchyma and the impermeability of brain tissues not only protect the brain from infectious processes, but also hinder its elimination in cases of brain involvement (Jasti et al., 2020). Therapeutic interventions are divided into areas of activity in Fig. 6 .
Fig. 6.
Summary table for therapeutic interventions.
(Source: Authors)
6.1. Preventive methods for neuropsychiatric effects associated with the treatment of patients with COVID-19
As the pandemic spreads in the population, the medical psychiatrists are being called upon to treat psychiatric conditions of the individuals with COVID-19 and are finding challenging clinical scenarios of multiple comorbidities and unknown drugs. In this sense, in view of the use of drugs with effects that are still little known, a rigorous assessment of the possible interactions between these drugs in vivo is necessary. Thus, the physician must be aware of the possibility of making adjustments to the medication arrangements, including avoiding the use of certain agents that can raise safety concerns (Bilbul et al., 2020).
6.1.1. Chloroquine and Hydroxychloroquine
These drugs have been reported to produce neuropsychiatric side effects such as agitation, personality change, depression and sleep disorders (Good and Shader, 1977; Juurlink, 2020). The responsible professional must recognize the presence of risk factors that induce such effects, which may be the simultaneous use of CYP3A4 inhibitors or low doses of glucocorticoids, in addition to the presence of family history of pre-existing psychiatric diseases, being female, low body weight and therapeutic overdose (Bilbul et al., 2020).
6.1.2. Remdesivir
There is not enough information available on the neuropsychiatric repercussions of this drug, but its administration has been associated with hypotension, diaphoresis and tremor reactions, which can be mistaken as a panic attack (Bilbul et al., 2020). Thus, physicians must be aware of possible adverse effects, weighing the risks and benefits in making clinical decisions.
1.3 Psychotropic drugs.
Several psychotropics have recently been named on a list of FDA-approved drugs with effective in vitro action against SARS-CoV-2 (Gordon et al., 2020). Among them, haloperidol, valproic acid and fluvoxamine are being tested for their ability to reduce hyperinflammation, for having antioxidant action and anti-inflammatory properties (Bilbul et al., 2020). In this way, psychiatrists can preferentially consider the use of these agents whenever appropriate.
6.2. Neuropsychiatric interventions
6.2.1. Unspecific neurological complications
The treatment of patients with neurological complications resulting from Sars-Cov- 2 requires greater caution, since certain drugs used as a therapeutic resource in normal conditions can aggravate the acute respiratory syndrome related to COVID-19. Out of these, immunosuppressive drugs for autoimmune neurological diseases and corticosteroid drugs stand out. In regard to typical second-line treatments for neuroinflammatory conditions, intravenous immunoglobulins (IVIg) or plasma (PLEX) are less likely to delay viral clearance in COVID-19. However, this therapy should be well evaluated, since IVIg is associated with an increased risk of thromboembolism. Finally, third-line medications, such as cyclophosphamide or rituximab, represent a high risk regarding COVID-19 infection, and should be used as the last treatment choice (Needham et al., 2020).
6.2.2. Delirium
The cases of delirium triggered by the COVID-19 infection have been related mainly to hyperactive or mixed varieties, with high degrees of anxiety, a fact that increases the challenge regarding treatment. In such cases, preference should be given to low-potency antipsychotic agents, including second-generation ones such as olanzapine and quetiapine, but also chlorpromazine (Beach et al., 2020). In addition, although there is limited evidence to support the use of any interventions in hyperactive delirium associated with COVID-19, most psychiatrists consider haloperidol as the best agent for controlling agitation in delusional patients (Bilbul et al., 2020).
Studies have also revealed that the administration of melatonin or melatonin receptor agonists (ARM) has been strongly associated with a reduction in the prevalence of delirium. In this sense, given its safety, melatonin should be considered a first-line agent to treat disorders of sleep-wake rhythm and consciousness, in addition to minimizing the administration of molecules that can cause central respiratory depression, such as benzodiazepines (Zambrelli et al., 2020). It is worth mentioning that the prescription of benzodiazepines, opioids and drugs with strong cholinergic properties (tertiary amine, tricyclic antidepressants, low-potency antipsychotics, benztropine and diphenhydramine) can potentially cause or exacerbate confusion, sedation and/or falls in patients with COVID- 19 (Bilbul et al., 2020). Thus, health professionals must follow local guidelines and policies related to the monitoring and management of delirium, being necessary to implement easy screening methods for delirium especially in light of the heavy workload during the COVID-19 crisis (Kotfis et al., 2020).
6.2.3. Cerebrovascular complications
The neurological clinical manifestations associated with the cytokine storm triggered by COVID-19 have been shown in three different ways: transient ischemic attack, ischemic stroke and hemorrhagic stroke. The most recent indicators suggest that the cerebrovascular disease in COVID-19 may be due to coagulopathy. In these patients, which damage is likely to be caused by the host's response to viral infection, establishing causality is even more challenging. Therefore, immediate anticoagulation with low-molecular-weight heparin was recommended in order to reduce the risk of thrombotic disease. For patients with cerebrovascular accident (CVA), cerebral angiography, intracranial imaging of the vessel wall and, if necessary, brain biopsy, in searches for vasculitis should also be considered (Ellul et al., 2020).
6.2.4. Encephalopathies
So far, no specific treatment for SARS-CoV-2 encephalitis has been observed. However, some recommendations include the use of anticonvulsants, antiviral drugs and antibiotics. The diagnosis of viral encephalitis should be based on clinical evidence of brain inflammation, such as cerebrospinal fluid (CSF) pleocytosis, imaging alterations, focal seizures or histological alterations. It is worth mentioning that, even if the virus is detected in the CSF, encephalitis should not be diagnosed, unless there is evidence of brain inflammation (Ellul et al., 2020).
6.2.5. Neuromuscular disorders
When investigating patients with limb weakness and sensory changes, it is essential to distinguish between peripheral nerve disease, such as GBS, and inflammation of the spinal cord, which can present flaccid paralysis if the cells of the anterior horn are involved. For this purpose, CSF examination, neurophysiological studies and imaging of the spine are essential (Ellul et al., 2020). The use of neuromuscular non-depolarizing blocking agent is reported as a risk factor for the development of myopathy due to critical illness. However, this was not observed in patients with other coronaviruses who received short cycles of these drugs (Guidon and Amato, 2020).
6.2.6. Anosmia and ageusia
The prior recognition of sensory symptoms possibly related to COVID-19 becomes extremely important because it would avoid the risk of inadequate treatment (such as anti-inflammatory predominant therapy, especially nasal and systemic corticosteroids and immunomodulators), which are contraindicated in case of SARS-CoV-2. In addition, psychiatrists, neurologists and doctors in general should be aware of this presentation of symptoms to avoid mistreatment, given that persistent olfactory dysfunction can increase the risk of nutritional deficit and lead to the development of other disorders (Pallanti, 2020).
6.3. Psychiatric interventions
6.3.1. Depression
Many of the experimental treatments for COVID-19, such as chloroquine and hydroxychloroquine, have high potential for neuropsychiatric effects related to the development of depression. It has also been shown that tocilizumab may have some positive effects on depressive symptoms in rheumatoid arthritis. In addition to these, azithromycin, vitamin C and corticosteroids have also been shown to induce depression depending on the dose and the therapeutic cycle (Bilbul et al., 2020). Therefore, the clinical management of these drugs should always be cautious. Finally, for the treatment of depression triggered by a state of hyperinflammation resulting from the infection, immune modulation therapies, such as interleukin-6 inhibitors and melatonin, are under investigation, and other therapies such as cytokine blocking drugs and Janus kinase inhibitors (JAK) have also been suggested (Ferrando et al., 2020).
6.3.2. Anxiety
The psychiatrist may be asked to evaluate and manage COVID-19 patients with anxiety or panic symptoms, in addition to breathing difficulties. Although there may be situations in which the use of small doses of benzodiazepines is appropriate, it is important to highlight its potential for respiratory depression. Therefore, physicians need to consider the risks and benefits of using benzodiazepines in patients with prominent respiratory symptoms. Depending on the circumstances and symptoms of each patient, alternative medications such as gabapentin, buspirone, hydroxyzine or a low dose of selective serotonin reuptake inhibitors (SSRIs) can be used. In addition, non-pharmacological and psychological interventions, such as psychotherapy, should also be prioritized (Bilbul et al., 2020).
6.3.3. Post-traumatic stress disorder (PTSD)
Studies conducted in Wuhan province with people with acute PTSD during the COVID-19 outbreak reported the need for a broader, more comprehensive psychological intervention. According to the data obtained, women, people with a recent history of exposure to the virus and people at high risk of infection or poor sleep quality deserve special attention, as these indicators were defined as strong precursors for the development of disorders typical of post-traumatic stress. In this perspective, the health professional is responsible for the early detection and intervention for PTSD, with a in-depth assessment of the risk factors that can lead to psychological problems, including previous mental health problems, grief, personal or family injuries, circumstances with life risk, panic, separation from the family and low family income (Sun et al., 2020; Duan and Zhu, 2020.). To this end, the development of teams with specialists qualified to deal with emotional stress, in addition to the training of community health workers regards basic aspects of mental health care, is essential (Rajkumar, 2020).
6.3.4. Psychosis
The relationship between the development of psychosis in patients with COVID-19 and the previous existence of psychiatric vulnerability was observed. In order to diagnose this condition, delirium should be considered in these patients and, in case of psychosis caused by COVID-19, the treatment of psychotic symptoms should be done with antipsychotic medication, although the possible complications triggered by these drugs due to the underlying infection by COVID-19 must be highlighted. (Ferrando et al., 2020).
6.4. Concluding remarks
The clinical worsening of the COVID-19 infection is mainly due to the Severe Acute Respiratory Syndrome; however, analyzing the atypical repercussions, including psychiatric and neuropsychiatric ones, is fundamental to mitigate the direct and indirect damages of this pandemic event. The main psychiatric and neuropsychiatric repercussions were depression, anxiety, post-traumatic stress disorder, psychosis, nonspecific neurological symptoms, delirium, cerebrovascular complications, encephalopathies, neuromuscular disorders, anosmia and ageusia. The psychiatric and neuropsychiatric symptoms of acute respiratory syndromes can appear during or after the infectious stage. Among the risk factors pointed out for such effects are the female gender, health professionals, presence of avascular necrosis and distressing pain. Therefore, it is necessary to intervene therapeutically through pharmacological and non-pharmacological means regarding such disorders; however, it is still important to observe the psychiatric effects of the drugs that are being used to treat COVID-19.
SARS-CoV-2 infection has a broad pathophysiological spectrum due to the availability of tissues with ACE-2 receptors. Through a first contact of the human organism with the aforementioned virus, the innate immunity acts in an increased way, generating exacerbated pro-inflammatory reactions, whose landmark is the “cytokine storm”, a key point for alterations in the neuronal tissue and the endothelial tissue attached to it. From this mechanism, studies point it as a trigger for encephalopathies, CNS autoimmune diseases, psychiatric and peripheral changes in the system in question, among other disorders which the studies about are still inconclusive. Our analytical limitations are essentially due to the scarce original articles and reviews on psychiatric and neuropsychiatric symptoms, which have their therapeutic interventions based on relatively small groups or case reports. More specifically, although certain mechanisms of pathophysiology of neuropsychiatric disorders are more consistent, others are assumed based on the interactions between the central nervous system and MERS or SARS-CoV-1.
6.5. Core messages
The preliminary clinical descriptions about COVID-19 turned to respiratory symptoms, however atypical presentations were increasingly recognized, among them, the psychiatric and neuropsychiatric repercussions.
Under the pathophysiological perspective, complex mechanisms are being proposed about neurotropism and neuroinvasion, as well as inflammatory mechanisms, such as the cytokine storm.
The main psychiatric and neuropsychiatric repercussions analyzed in this chapter were depression, anxiety, post-traumatic stress disorder, psychosis, nonspecific neurological symptoms, delirium, cerebrovascular complications, encephalopathies, neuromuscular disorders, anosmia and ageusia.
We believe that it is essential to analyze not only psychiatric and neuropsychiatric disorders, but also therapeutic interventions in a pharmacological and non-pharmacological way, in addition to observing the psychiatric effects of the drugs that are being used to treat COVID-19.
Authors' contributions
MLRN Conceptualization; Data curation; Formal analysis; Funding acquisition; Methodology.
CGLS and ISC Project administration; Resources; Software; Supervision.
JLSM, SMBB, JGV, NCBC, EBGF, PWGF and MLRN Validation; Visualization; Writing - original draft; Writing - review & editing.
Ethical approval
The study is a systematic review, and approval by the Ethics Committee is not required.
Funding
The Suicidology Research Group from Universidade Federal do Ceará (UFC) and Brazilian National Council for Scientific and Technological Development (CNPq) – institution linked to the Brazilian Department of Science, Technology and Innovation to encourage research in Brazil.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgements
The Brazilian National Council for Scientific and Technological Development (CNPq) – institution linked to the Brazilian Department of Science, Technology and School of Medicine/Universidade Federal do Cariri –UFCA.
References
- Asadi-Pooya A., Simani L. Central nervous system manifestations of COVID-19: a systematic review. J. Neurol. Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach S., Praschan N., Hogan C., Dotson S., Merideth F., Kontos N. Delirium in COVID-19: a case series and exploration of potential mechanisms for central nervous system involvement. Gen. Hosp. Psychiatry. 2020;65:47–53. doi: 10.1016/j.genhosppsych.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beatriz Lara B., Carnes A., Dakterzada F., Benitez I., Piñol-Ripoll G. Neuropsychiatric symptoms and quality of life in Spanish Alzheimer’s disease patients during COVID-19 lockdown. Eur. J. Neurol. 2020 doi: 10.1111/ene.14339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilbul M., Paparone P., Kim A., Mutalik S., Ernst C. Psychopharmacology of COVID-19. Psychosomatics. 2020 doi: 10.1016/j.psym.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carod Artal F. Complicaciones neurológicas por coronavirus y COVID-19. Revista De Neurología. 2020;70(09):311. doi: 10.33588/rn.7009.2020179. [DOI] [PubMed] [Google Scholar]
- Correia A., Feitosa P., Moreira J., Nogueira S., Fonseca R., Nobre M. Neurological manifestations of COVID-19 and other coronaviruses: a systematic review. Neurol. Psychiatry Brain Res. 2020;37:27–32. doi: 10.1016/j.npbr.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinakaran D., Manjunatha N., Naveen Kumar C., Suresh B. Neuropsychiatric aspects of COVID-19 pandemic: a selective review. Asian J. Psychiatr. 2020;53:102188. doi: 10.1016/j.ajp.2020.102188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):300–302. doi: 10.1016/s2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellul M., Benjamin L., Singh B., Lant S., Michael B., Kneen R. Neurological associations of COVID-19. SSRN Electron. J. 2020 doi: 10.2139/ssrn.3589350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrando S., Klepacz L., Lynch S., Tavakkoli M., Dornbush R., Baharani R. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? Psychosomatics. 2020 doi: 10.1016/j.psym.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furer P., Walker J., Chartier M., Stein M. Hypochondriacal concerns and somatization in panic disorder. Depress. Anxiety. 1997;6(2):78–85. doi: 10.1002/(sici)1520-6394(1997)6:2<78::aid-da4>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Giacomelli A., Pezzati L., Conti F., Bernacchia D., Siano M., Oreni L. Self-reported olfactory and taste disorders in patients with severe acute respiratory coronavirus 2 infection: a cross-sectional study. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good M., Shader R. Behavioral toxicity and equivocal suicide associated with chloroquine and its derivatives. Am. J. Psychiatr. 1977;134(7):798–801. doi: 10.1176/ajp.134.7.798. [DOI] [PubMed] [Google Scholar]
- Gordon D., Jang G., Bouhaddou M., Xu J., Obernier K., White K. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature. 2020 doi: 10.1038/s41586-020-2286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grom A.A., Horne A., De Benedetti F. Macrophage activation syndrome in the era of biologic therapy. Nat. Rev. Rheumatol. 2016;12(5):259–268. doi: 10.1038/nrrheum.2015.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidon A., Amato A. COVID-19 and neuromuscular disorders. Neurology. 2020;94(22):959–969. doi: 10.1212/wnl.0000000000009566. [DOI] [PubMed] [Google Scholar]
- Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020:1–11. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honigsbaum M. The art of medicine: “an inexpressible dread”: psychoses of influenza at fin-de-siècle. Lancet. 2013;381:988–989. doi: 10.1016/S0140-6736(13)60701-1. [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasti M., Nalleballe K., Dandu V., Onteddu S. A review of pathophysiology and neuropsychiatric manifestations of COVID-19. J. Neurol. 2020:1–6. doi: 10.1007/s00415-020-09950-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juurlink D. Safety considerations with chloroquine, hydroxychloroquine and azithromycin in the management of SARS-CoV-2 infection. Can. Med. Assoc. J. 2020;192(17):E450–E453. doi: 10.1503/cmaj.200528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotfis K., Williams Roberson S., Wilson J.E. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit. Care. 2020;24:176. doi: 10.1186/s13054-020-02882-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Xue Q., Xu X. Involvement of the nervous system in SARS-CoV-2 infection. Neurotox. Res. 2020;38(1):1–7. doi: 10.1007/s12640-020-00219-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L., Jin H., Wang M., Hu Y., Chen S., He Q. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77(6):683. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menninger K.A. Influenza and schizophrenia. Am. J. Psychiatry. 1926;82:469–529. doi: 10.1176/ajp.82.4.469. [DOI] [PubMed] [Google Scholar]
- Needham E., Chou S., Coles A., Menon D. Neurological implications of COVID-19 infections. Neurocrit. Care. 2020;32(3):667–671. doi: 10.1007/s12028-020-00978-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallanti S. Importance of SARs-Cov-2 anosmia: from phenomenology to neurobiology. Compr. Psychiatry. 2020;100:1–3. doi: 10.1016/j.comppsych.2020.152184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J., Chesney E., Oliver D., Pollak T., McGuire P., Fusar-Poli P. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020:1–17. doi: 10.1016/s2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin A. 2019 novel coronavirus (COVID-19) outbreak: a review of the current literature. Euras. J. Med. Oncol. 2020;4(1):1–7. doi: 10.14744/ejmo.2020.12220. [DOI] [Google Scholar]
- Serrano-Castro P., Estivill-Torrús G., Cabezudo-García P., Reyes-Bueno J., Ciano Petersen N., Aguilar-Castillo M. Influencia de la infección SARS-CoV-2 sobre enfermedades neurodegenerativas y neuropsiquiátricas: ¿una pandemia demorada? Neurología. 2020;35(4):245–251. doi: 10.1016/j.nrl.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun L., Sun Z., Wu L., Zhu Z., Zhang F., Shang Z. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. Medrxiv. 2020:1–17. doi: 10.1101/2020.03.06.20032425. [DOI] [Google Scholar]
- Troyer E., Kohn J., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020:1–6. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaira L.A., Salzano G., Deiana G., De Riu G. Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope. 2020:1–4. doi: 10.1002/lary.28692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020:1–5. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin C. Genotyping coronavirus SARS-CoV-2: methods and implications. Genomics. 2020:1–9. doi: 10.1016/j.ygeno.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambrelli E., Canevini M., Gambini O., D’Agostino A. Delirium and sleep disturbances in COVID–19: a possible role for melatonin in hospitalized patients? Sleep Med. 2020;70:111. doi: 10.1016/j.sleep.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z., Kang H., Li S., Zhao X. Understanding the neurotropic characteristics of SARS-CoV-2: from neurological manifestations of COVID-19 to potential neurotropic mechanisms. J. Neurol. 2020:1–6. doi: 10.1007/s00415-020-09929-7. [DOI] [PMC free article] [PubMed] [Google Scholar]