Abstract
The purpose of this study was to determine (i) if failing to achieve a patient-reported outcome (PRO) threshold at 1 year was associated with secondary operations at minimum 2-year follow-up and (ii)what outcome measure and threshold has the highest association with future surgeries. Inclusion criteria for this study were cases of primary hip arthroscopy between July 2014 and April 2017. Included patients had recorded pre-operative and 1-year post-operative modified Harris Hip Score (mHHS) and 12-item international Hip Outcome Tool (iHOT-12) scores. Patients were classified based on their ability to achieve minimal clinical important difference (MCID), substantial clinical benefit (SCB) and patient acceptable symptom state (PASS) for each PRO and the status of secondary operations at minimum 2-year follow-up. The sensitivity, specificity, accuracy, positive likelihood ratio and negative likelihood ratio for these thresholds were calculated. Of 425 eligible cases, 369 (86.8%) had minimum 2-year follow-up. Of the included patients, 28 underwent secondary operations (7.59%), with 14 undergoing secondary arthroscopies (3.79%) and 14 converting to total hip arthroplasty (3.79%). For mHHS, 267 (72.4%), 173 (46.9%) and 277 (75.1%) hips met MCID, SCB and PASS, respectively. For iHOT-12, 234 (63.4%), 218 (59.1%) and 280 (75.9%) hips met the respective thresholds. The highest specificity, sensitivity and accuracy were identified as for iHOT-12 MCID (0.79), iHOT-12 PASS (0.79) and iHOT-12 MCID (0.77), respectively. Patients not attaining MCID and PASS for mHHS and iHOT-12 at 1-year post-operatively are at increased risk of secondary operation. The most accurate threshold associated with secondary operation (0.77) is not achieving iHOT-12 MCID. Level of evidence: retrospective case series: level IV.
INTRODUCTION
Patient management of intra-articular hip pathologies has improved drastically over the past two decades and today hip arthroscopy plays an important role in hip preservation surgery. Successful outcomes have been shown in large clinical studies [1, 2] and randomized control studies [3, 4]. Hip arthroscopy has been especially beneficial among athletes with a recent systematic review showing a 93% return-to-play [5].
Despite these positive outcomes, a subset of patients will continue to suffer from pain and functional limitations, subsequently requiring secondary procedures on the hip. A recent systematic review and meta-analysis of patients who underwent primary hip arthroscopy reported a 5.5% secondary operation rate among 1981 hips, with an undefined time-frame [6]. In a registry-based study of nearly 4000 hip preservation patients, the secondary operation rate was 9.6% at a minimum 2-year follow-up [7]. Davies et al. and Degan et al. [8, 9] evaluated potential risk factors influencing the need for secondary operations following hip arthroscopy and included older age, dysplastic features or osteoarthritis on pre-operative radiographs, and intraoperative findings of arthritis.
Defining a surgical success in hip arthroscopy is multifaceted. In one respect, it may be defined as improvement in pain and function, as measured by patient-reported outcomes (PROs); however, another aspect would be remaining free from secondary operations [10, 11]. As part of the shift toward a patient-centered approach for treatment assessment, PROs have increasingly gained recognition as an essential component of surgical outcome evaluation. In the realm of hip arthroscopy, several PROs have been constructed and validated. The most common PRO is the modified Harris Hip Score (mHHS) [12, 13]. The short version of the 12-item international Hip Outcome Tool (iHOT-12) [14], a newer PRO, has recently gained attention. It has been notable for its use in younger patients and has been recommended for evaluation of femoroacetabular impingement (FAI) treatment in the Warwick Agreement [15].
A major utility of PROs is the ability to evaluate post-operative functional status based on attainment of predefined thresholds [16]. The patient acceptable state score (PASS) is defined as the minimal score above which patients are satisfied with the state of their condition. The substantial clinical benefit (SCB) is the difference between pre-operative and post-operative condition which the patient deems as substantially better, while the minimal clinical important difference (MCID) is defined as the smallest perceptible change patients recognize as beneficial [17, 18].
These thresholds have been defined for PROs commonly used in the hip preservation literature. For the mHHS, MCID was defined to be 8 by Kemp et al. [19], SCB was defined to be 19.8 by Nwachukwu et al. [20] and the PASS score was defined to be 74 by Chahal et al. [21]. For iHOT-12, MCID and SCB were determined to be 13 and 28, respectively by Martin et al. [22] and the PASS was determined to be 63 by Nwachukwu et al. [23].
The purpose of this study was to determine (i) if failing to achieve a PRO threshold at 1 year was associated with secondary operations at minimum 2-year follow-up and (ii) to determine which outcome measure and threshold have the highest association with future surgeries. First, we hypothesized that failure to achieve PRO threshold values for mHHS and iHOT-12 would be associated with secondary operations at minimum 2-year follow-up. Second, we hypothesized that achieving the defined thresholds of the iHOT-12 would be more strongly associated with secondary operations than the mHHS.
MATERIALS AND METHODS
Patient participation in blinded registry
While the present study presents novel findings, data on some patients may have been reported in other studies performed at our institution. All data collection received Institutional Review Board approval.
Patient selection criteria
Data on all primary hip arthroscopy for treatment of FAI performed by a single, high-volume, fellowship-trained hip surgeon (B.G.D.) between July 2014 and April 2017 was prospectively collected and retrospectively reviewed. All patients had to have pre-operative and post-operative mHHS and iHOT-12 scores at their 1-year follow-up. Patients were excluded if they underwent prior ipsilateral hip surgeries, were Tonnis grade >1, had previous hip conditions, such as Legg–Calve–Perthes, slipped capital femoral epiphysis, hip dysplasia (lateral center edge angle < 18) or avascular necrosis. Patients who were unwilling to participate or of worker’s compensation status were also excluded. Endpoints, defined as either secondary hip arthroscopy or conversion to total hip arthroplasty (THA), were recorded at each of the post-operative encounters.
Defining outcome thresholds and patient categories
Based on previous literature [19–23], this study set the values for MCID, SCB and PASS for mHHS at 8, 19.8 and 74, respectively; and for iHOT-12 at 13, 28 and 63, respectively. Since the studies that established these thresholds did so using 1-year post-operative outcomes, this study used the 1-year outcomes as well.
Patients were categorized based on their achievement of the PRO thresholds and whether they underwent a secondary operation. ‘True positives’ were patients who did not achieve the PRO threshold and required a secondary operation, while ‘false positives’ were patients who did not meet the PRO threshold yet remained operation free. ‘True negatives’ were patients who met the threshold and remained free of secondary operations, while ‘false negatives’ were patients who met the threshold but still underwent a secondary operation (Table I).
Table I.
Contingency table layout
| Secondary operation required | Free of secondary operation | |
|---|---|---|
| Threshold unmet | True positive | False positive |
| Threshold met | False negative | True negative |
Statistical analysis
Continuous variables (age, body mass index, follow-up and PROs) were reported as means and standard deviations, whereas categorical variables (gender and laterality) were reported as counts and percentages. Sensitivity, specificity and accuracy were calculated accompanied by 95% confidence intervals (CIs) for each PRO and each threshold. The positive likelihood ratio (LR+) and negative likelihood ratio (LR−) were calculated as well. For this study, LR+ were calculated by dividing true positives by false positives and the LR− were calculated by dividing false negatives by true negatives. In general, an LR of 0.1 decreases likelihood by 45%, while an LR of 0.5 decreases likelihood by 15%. Similarly, an LR of 2.0 increases the likelihood by 15%, while an LR of 10 increases the likelihood by 45% [24, 25].
The equations used to calculate sensitivity, specificity, accuracy, LR+ and LR− are presented in Table II. All statistical analyses were carried out using Python (Version 3.7.1; Python Software Foundation).
Table II.
Equations for sensitivity, specificity, accuracy and relative risk
| Sensitivity | TP/(TP + FN) |
| Specificity | TN/(TN + FP) |
| Accuracy | (TP + TN)/(TP + TN + FP + FN) |
| LR+ | (Sensitivity)/(1 − specificity) |
| LR− | (1 − sensitivity)/(specificity) |
TP: true positive; TN: true negative; FP: false positive; FN: false negative; LR+: positive likelihood ratio; LR−: negative likelihood ratio.
RESULTS
Patient population
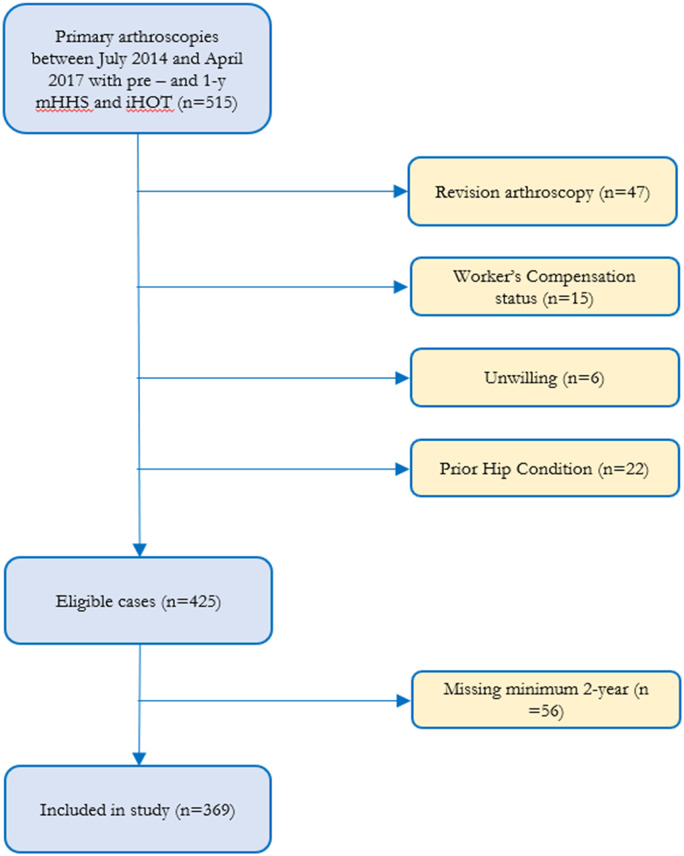
A total of 515 hips (498 patients) that underwent hip arthroscopy had baseline and 1-year post-operative mHHS and iHOT-12 scores. After applying exclusion criteria, 425 hips (398 patients) were eligible for inclusion in the study, of which follow-up was available for 369 patients (86.8%). The flowchart for patient inclusion and exclusion is shown in Fig. 1.
Fig. 1.
Flowchart of patient inclusion and exclusion in the study. mHHS: modified Harris Hip Score; iHOT-12: 12-item international Hip Outcome Tool.
Patient demographics and outcomes are shown in Table III. The mean follow-up time was 32.08 ± 8.40 months. Of the included patients, 28 underwent secondary operations (7.59%), with 14 undergoing secondary arthroscopies (3.79%) and 14 converting to THA (3.79%).
Table III.
Summary of cohort characteristics
| Measure | Entire cohort |
|---|---|
| Age (years), mean ± SD | 40.22 ± 15.07 |
| Body mass index (kg/m2), mean ± SD | 26.46 ± 4.96 |
| Follow-up (months), mean ± SD | 32.08 ± 8.40 |
| Pre-mHHS (mean ± SD) | 62.76 ± 14.63 |
| Latest mHHS (mean ± SD) | 85.72 ± 17.23 |
| Pre-IHOT (mean ± SD) | 35.65 ± 20.15 |
| Latest IHOT (mean ± SD) | 75.93 ± 25.62 |
| Gender (male:female), % male | (250:119), 67.75% |
| Side (right:left), % right | (183:186) 49.59% |
mHHS: modified Harris Hip Score; iHOT-12: 12-item international Hip Outcome Tool.
Attainment of patient-reported outcome thresholds
For mHHS, the number of hips that met MCID, SCB and PASS were 267 (72.4%), 173 (46.9%) and 277 (75.1%), respectively. For iHOT-12, 234 (63.4%), 218 (59.1%) and 280 (75.9%) hips met the respective thresholds (Fig. 2).
Fig. 2.
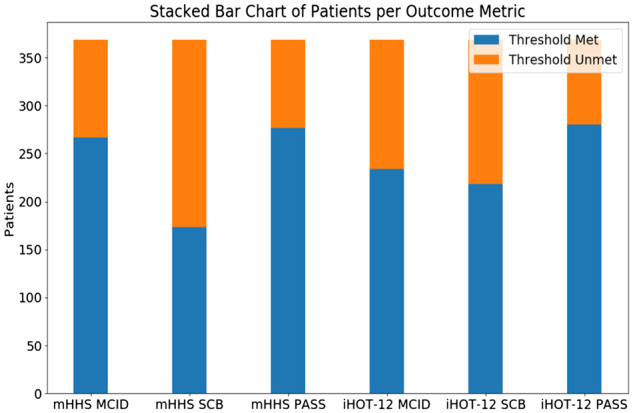
Stacked bar chart of patients attaining the score thresholds. mHHS: modified Harris Hip Score; iHOT-12: 12-item international Hip Outcome Tool; MCID: minimal clinical important difference; SCB: substantial clinical benefit; PASS: patient acceptable symptom state.
The highest specificity, sensitivity and accuracy for secondary operations were identified as iHOT-12 MCID (0.79; CI 0.74–0.83), iHOT-12 PASS (0.79; CI 0.63–0.94) and iHOT-12 MCID (0.77; CI 0.73–0.81), respectively. All data regarding sensitivity, specificity and accuracy are presented in Table IV. All LR+ were >1, while all LR− were between 0 and 1. Contingency tables associating future surgery and achievement of thresholds are shown in Tables V and VI.
Table IV.
Statistical measures for all future surgeries
| Outcome measure | Metric | Specificity (CI) | Sensitivity (CI) | Accuracy (CI) | LR+ (CI) | LR− (CI) |
|---|---|---|---|---|---|---|
| mHHS | MCID | 0.77 (0.72–0.81) | 0.46 (0.28–0.64) | 0.74 (0.70–0.79) | 2.00 (1.28–3.12) | 0.70 (0.49–0.99) |
| SCB | 0.49 (0.44–0.54) | 0.79 (0.63–0.94) | 0.51 (0.46–0.56) | 1.54 (1.24–1.92) | 0.43 (0.21–0.89) | |
| PASS | 0.75 (0.70–0.80) | 0.64 (0.46–0.82) | 0.74 (0.70–0.79) | 2.61 (1.87–3.64) | 0.47 (0.29–0.78) | |
| iHOT-12 | MCID | 0.79 (0.74–0.83) | 0.57 (0.39–0.75) | 0.77 (0.73–0.81) | 2.67 (1.83–3.90) | 0.54 (0.35–0.84) |
| SCB | 0.62 (0.57–0.67) | 0.75 (0.59–0.91) | 0.63 (0.58–0.68) | 1.97 (1.53–2.53) | 0.40 (0.21–0.77) | |
| PASS | 0.67 (0.62–0.72) | 0.79 (0.63–0.94) | 0.68 (0.63–0.72) | 2.37 (1.86–3.03) | 0.32 (0.16–0.65) |
Highest values in each category are marked in bold.
CI: confidence interval; LR+: positive likelihood ratio; LR−: negative likelihood ratio; mHHS: modified Harris Hip Score; iHOT-12: 12-item international Hip Outcome Tool; MCID: minimal clinical important difference; SCB: substantial clinical benefit; PASS: patient acceptable symptom state.
Table V.
Contingency table for mHHS
| MCID |
SCB |
PASS |
||||
|---|---|---|---|---|---|---|
| Secondary operation required | Free of secondary operation | Secondary operation required | Free of secondary operation | Secondary operation required | Free of secondary operation | |
| Threshold unmet | 13 | 79 | 22 | 174 | 18 | 84 |
| Threshold met | 15 | 262 | 6 | 167 | 10 | 257 |
mHHS: modified Harris Hip Score; MCID: minimal clinical important difference; SCB: substantial clinical benefit; PASS: patient acceptable symptom state.
Table VI.
Contingency table for iHOT-12
| MCID |
SCB |
PASS |
||||
|---|---|---|---|---|---|---|
| Secondary operation required | Free of secondary operation | Secondary operation required | Free of secondary operation | Secondary operation required | Free of secondary operation | |
| Threshold unmet | 16 | 73 | 21 | 130 | 22 | 113 |
| Threshold met | 12 | 268 | 7 | 211 | 6 | 228 |
mHHS: modified Harris Hip Score; MCID: minimal clinical important difference; SCB: substantial clinical benefit; PASS: patient acceptable symptom state.
The analyses were performed separately for each type of surgery (i.e. secondary arthroscopy and THA). For secondary hip arthroscopy, the highest specificity was found to be for iHOT-12 MCID (0.77; CI 0.72–0.81), the highest sensitivity was found to be for mHHS SCB (0.79; CI 0.57–1.00) and the highest accuracy was found to be for iHOT-12 MCID (0.75; CI 0.71–0.80) (Table VII).
Table VII.
Statistical measures for future hip preservation surgery
| Outcome measure | Metric | Specificity (CI) | Sensitivity (CI) | Accuracy (CI) | LR+ (CI) | LR− (CI) |
|---|---|---|---|---|---|---|
| mHHS | MCID | 0.76 (0.71–0.80) | 0.43 (0.17–0.69) | 0.74 (0.70–0.79) | 1.77 (0.94–3.33) | 0.75 (0.48–1.19) |
| SCB | 0.48 (0.48–0.53) | 0.79 (0.57–1.00) | 0.49 (0.44–0.54) | 1.51 (1.13–2.02) | 0.45 (0.16–1.23) | |
| PASS | 0.73 (0.69–0.78) | 0.57 (0.31–0.83) | 0.73 (0.68–0.77) | 2.16 (1.33–3.51) | 0.58 (0.32–1.07) | |
| iHOT-12 | MCID | 0.77 (0.72–0.81) | 0.43 (0.17–0.69) | 0.75 (0.71–0.80) | 1.83 (0.97–3.45) | 0.75 (0.47–1.18) |
| SCB | 0.60 (0.55–0.65) | 0.64 (0.39–0.89) | 0.60 (0.55–0.65) | 1.61 (1.07–2.42) | 0.60 (0.29–1.21) | |
| PASS | 0.65 (0.60–0.70) | 0.71 (0.48–0.95) | 0.65 (0.60–0.70) | 2.03 (1.42–2.91) | 0.44 (0.19–1.01) |
Highest values in each category are marked in bold.
CI: confidence interval; LR+: positive likelihood ratio; LR−: negative likelihood ratio; mHHS: modified Harris Hip Score; iHOT-12: 12-item international Hip Outcome Tool; MCID: minimal clinical important difference; SCB: substantial clinical benefit; PASS: patient acceptable symptom state.
For conversion to THA, the highest specificity was found to be for iHOT-12 MCID (0.78; CI 0.73–0.82), the highest sensitivity was found to be for iHOT-12 PASS and iHOT-12 SCB (0.86; CI 0.67–1.00) and the highest accuracy was found to be for iHOT-12 MCID (0.77; CI 0.73–0.82) (Table VIII).
Table VIII.
Statistical measures for conversion to total hip arthroplasty
| Outcome measure | Metric | Specificity (CI) | Sensitivity (CI) | Accuracy (CI) | LR+ (CI) | LR− (CI) |
|---|---|---|---|---|---|---|
| mHHS | MCID | 0.76 (0.72–0.80) | 0.50 (0.24–0.76) | 0.75 (0.71–0.79) | 2.09 (1.20–3.64) | 0.66 (0.39–1.11) |
| SCB | 0.48 (0.43–0.53) | 0.79 (0.57–1.00) | 0.49 (0.44–0.54) | 1.51 (1.13–2.02) | 0.45 (0.16–1.23) | |
| PASS | 0.74 (0.69–0.79) | 0.71 (0.48–0.95) | 0.74 (0.69–0.78) | 2.76 (1.89–4.01) | 0.39 (0.17–0.88) | |
| iHOT-12 | MCID | 0.78 (0.73–0.82) | 0.71 (0.48–0.95) | 0.77 (0.73–0.82) | 3.21 (2.19–4.71) | 0.37 (0.16–0.84) |
| SCB | 0.61 (0.56–0.66) | 0.86 (0.67–1.00) | 0.62 (0.57–0.67) | 2.19 (1.70–2.81) | 0.23 (0.06–0.85) | |
| PASS | 0.65 (0.60–0.70) | 0.86 (0.67–1.00) | 0.66 (0.61–0.71) | 2.47 (1.91–3.20) | 0.22 (0.06–0.79) |
Highest values in each category are marked in bold.
CI: confidence interval; LR+: positive likelihood ratio; LR−: negative likelihood ratio; mHHS: modified Harris Hip Score; iHOT-12: 12-item international Hip Outcome Tool; MCID: minimal clinical important difference; SCB: substantial clinical benefit; PASS: patient acceptable symptom state.
Ten patients were found to have met the MCID threshold for both mHHS and iHOT-12 but still required a secondary operation. Of these 10, three subsequently developed osteoarthritis and required a THA while seven re-tore their labrum and required a secondary arthroscopy.
DISCUSSION
This study on 369 hips found that for mHHS using MCID, SCB or PASS as thresholds was associated with secondary operations with accuracies of 74%, 51% and 74%, respectively; and for iHOT-12, MCID, SCB and PASS was associated with secondary operations with accuracies of 77%, 63% and 68%, respectively. Of all thresholds, specificity was highest for iHOT-12 MCID (0.79), while sensitivity was highest for both mHHS SCB and iHOT-12 PASS (0.79). The iHOT-12 MCID demonstrated the highest accuracy and LR+ (0.77 and 2.67, respectively).
The study found that failure to achieve SCB for mHHS and PASS for iHOT-12 had the highest sensitivity for secondary operations. This was true for secondary operations in general as well as for either secondary arthroscopy or THA independently. This finding is reasonable, as patients who failed to demonstrate even the minimal detectable clinical improvement will naturally seek further treatment options. A surgeon’s tendency to suggest future surgery as well as proclivity to operate on these patients increases the likelihood of secondary operation rate as well.
For all scores assessed, LR+ was >1 as would be expected, indicating that those patients who did not meet the PRO threshold had a higher likelihood of undergoing surgery that those patients that did meet the threshold. Of the scores, the MCID of iHOT-12 was most indicative of secondary operation (LR+ = 2.67). Similarly, all LR− were <1 (0.32–0.70), indicating that those patients that did achieve the scores did not undergo future surgery. Of these, the PASS of iHOT-12 was most indicative of not undergoing future surgery with an LR− of 0.32. These results may be explained by higher applicability of iHOT-12 to the younger population undergoing hip arthroscopy.
In hip arthroscopy, several studies have determined that pre-operative PROs can serve as predictors for outcomes of surgical intervention [26–28]. Pre-operative PROs have consistently been found to correlate to post-operative scores [11]. Redmond et al. [27] identified the pre-operative mHHS as a predictor for 2-year conversion to THA. Likewise, Griffin et al. [28] performed a systematic review identifying low pre-operative PROs as predictors of conversion to THA in older adults. To our knowledge, using the achievement of post-operative PRO thresholds for prediction of treatment failure in hip arthroscopy is a novel concept. This concept has, however, been explored in hip arthroplasty. Registry-based studies from Sweden and New Zealand found that inferior PROs at 6 months and 1 year were strong predictors of future ipsilateral hip secondary operations, and concluded that these patients should, therefore, be closely monitored [29–31].
Levy et al. [18] conducted a comprehensive systematic review of the hip arthroscopic literature to evaluate the proportion of studies that satisfied the MCID and PASS for mHHS and the Hip Outcome Score. While they report high rates of meeting the MCID and PASS for mHHS (97% and 88%, respectively), these values referred to the overall study averages and not to the individual patient. In contrast, there is a paucity of studies reporting on the proportion of patients attaining MCID and PASS.
The threshold scores for iHOT-12 have only recently been published, and therefore, to our knowledge studies have yet to report findings based on these thresholds. Conversely, proportions of patients attaining MCID and PASS for mHHS have been reported in a few studies. In the study by Chahal et al. [21], in which the PASS for mHHS was determined, the proportion of patients achieving PASS was 69%. Basques et al. [32] reported on 624 patients undergoing surgery for FAI and found that 67% of their patients achieved mHHS PASS. Cvetanovich et al. [33] reported a 74% achievement of MCID and a 68% achievement of PASS for the mHHS. Nwachukwu et al. [34] reported that 77.2% of 364 patients undergoing surgery for FAI achieved MCID. In our study, the proportion of patients achieving MCID, SCB and PASS for the mHHS are 72.3%, 46.9% and 75.1%, respectively. For iHOT-12, the proportion of patients achieving MCID, SCB and PASS are 63.4%, 59.1% and 75.9%, accordingly. Thus, the percentage of patients attaining MCID for mHHS in our study is in line with previous reports, although the percentage attaining PASS is slightly higher than other reports.
In the opinion of the authors, it is important to not only report the average PRO for the population but also to specifically emphasize the proportion of patients achieving these thresholds. This type of analysis can, in turn, allow clinicians to more accurately estimate success of a given procedure for an individual patient, which can therefore make the results more generalizable and help improve shared decision-making.
Strengths and limitations
The primary strength of our study lies in the large cohort of patients for which data on pre- and post-operative PROs were collected. Additionally, there was a high follow-up regarding secondary operation status at minimum of 2 years for those patients eligible for inclusion based on PROs at 1 year (86.8%). Lastly, the use of two validated PRO tools in the same cohort of patients enabled comparison between scores and thresholds.
This study is not without limitations. First, 13 patients had secondary operations prior to the 1-year follow-up period and thus were not included due to lack of 1-year PROs. Therefore, the true rate of secondary operation is higher than what was found in this study. Second, this is a single-center study based on registry data from a single high-volume surgeon, thus the generalizability of this study may be limited. Third, the decision for secondary operations are subjective and made by both patient and surgeon through a shared decision-making process. Furthermore, secondary operation itself is not a disease endpoint, but rather is a decision. These factors may diminish replicability of these results. Fourth, only patients with 1-year post-operative PROs were included in this study, which may introduce selection and transfer bias. Fifth, the specific factors that influenced the decision for secondary operation were not investigated as this is beyond the scope of the present study. Future studies may focus on the possible reasons to delay surgery of patients with unsuccessful outcomes. Lastly, this study only identified an association of achievements of PRO metrics and secondary operations. This study refrained from using terms such as ‘predictors’ regarding our findings since these do not imply causation, but correlation.
CONCLUSIONS
Patients not attaining MCID and PASS for mHHS and iHOT-12 at 1-year post-operatively are at increased risk of secondary operations. The most accurate threshold associated with secondary operation (0.77) is not achieving iHOT-12 MCID.
ETHICAL STATEMENT
This study was performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. This study was carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA). Details that might disclose the identity of the subjects under study have been omitted. This study was approved by the IRB (IRB ID: 5276). This study was performed at the American Hip Institute.
CONFLICT OF INTEREST STATEMENT
Dr. Rosinsky reports food/beverage and travel/lodging support from Arthrex, Stryker, and Smith & Nephew. Dr. Lall reports educational support from Medwest and Smith & Nephew; research support from Arthrex, Stryker, and Medacta; food and beverage from Smith & Nephew, Stryker, Zimmer Biomet, Arthrex; travel and lodging from Stryker and Arthrex; and consulting fees from Arthrex and Graymont Medical. Dr. Lall is the Medical Director of Hip Preservation at St. Alexius Medical Center. Dr. Maldonado reports food/beverage and travel/lodging support from Arthrex, Stryker, and Smith & Nephew. Dr Maldonado is also a board member of the Journal of Arthroscopy. Dr. Meghpara reports educational support, food/beverage, and travel/lodging from Arthrex, Stryker, and Smith & Nephew. Dr. Shapira reports food/beverage and travel/lodging support from Arthrex, Stryker, and Smith & Nephew. Dr. Domb has HAD ownership interests in Hinsdale Orthopaedics, the American Hip Institute, SCD#3, North Shore Surgical Suites, and Munster Specialty Surgery Center; has received research support from Arthrex, ATI, the Kauffman Foundation, Stryker, and Pacira Pharmaceuticals; has received consulting fees from Adventist Hinsdale Hospital, Arthrex, MAKO Surgical, Medacta, Pacira Pharmaceuticals, and Stryker; has received educational support from Arthrex, Breg, and Medwest; has received speaking fees from Arthrex and Pacira Pharmaceuticals; and receives royalties from Arthrex, DJO Global, MAKO Surgical, Stryker, and Orthomerica. Dr. Domb is the Medical Director of Hip Preservation at St. Alexius Medical Center, a board member for the American Hip Institute Research Foundation, AANA Learning Center Committee, the Journal of Hip Preservation Surgery, and the Journal of Arthroscopy. The American Hip Institute Research Foundation fund research and is where our study was performed.
Contributor Information
Philip J Rosinsky, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA.
Jeffery W Chen, Vanderbilt University School of Medicine, 1161 21st Ave, Nashville, TN 37232, USA.
Mitchell J Yelton, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA.
Ajay C Lall, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA; American Hip Institute, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA.
David R Maldonado, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA.
Mitchell B Meghpara, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA; Orthopaedic Department, AMITA Health St. Alexius Medical Center, 1555 Barrington Rd, Hoffman Estates, IL 60169, USA.
Jacob Shapira, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA.
Benjamin G Domb, American Hip Institute Research Foundation, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA; American Hip Institute, 999 E Touhy Ave, Suite 450, Des Plaines, IL 60018, USA.
REFERENCES
- 1. Domb BG, Gui C, Hutchinson MR et al. Clinical outcomes of hip arthroscopic surgery: a prospective survival analysis of primary and revision surgeries in a large mixed cohort. Am J Sports Med 2016; 44: 2505–17. [DOI] [PubMed] [Google Scholar]
- 2. Lund B, Mygind-Klavsen B, Grønbech Nielsen T et al. Danish Hip Arthroscopy Registry (DHAR): the outcome of patients with femoroacetabular impingement (FAI). J Hip Preserv Surg 2017; 4: 170–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Griffin DR, Dickenson EJ, Wall PDH et al. ; FASHIoN Study Group. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet 2018; 391: 2225–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Palmer AJR, Gupta VA, Fernquest S et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ 2019; 364: l185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Memon M, Kay J, Hache P et al. Athletes experience a high rate of return to sport following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc 2018; 10: 3066–104. [DOI] [PubMed] [Google Scholar]
- 6. Minkara AA, Westermann RW, Rosneck J, Lynch TS. Systematic review and meta-analysis of outcomes after hip arthroscopy in femoroacetabular impingement. Am J Sports Med 2019; 47: 488–500. [DOI] [PubMed] [Google Scholar]
- 7. Kester BS, Capogna B, Mahure SA et al. Independent risk factors for revision surgery or conversion to total hip arthroplasty after hip arthroscopy: a review of a large statewide database from 2011 to 2012. Arthroscopy 2018; 34: 464–70. [DOI] [PubMed] [Google Scholar]
- 8. Davies O, Grammatopoulos G, Pollard TCB et al. Factors increasing risk of failure following hip arthroscopy: a case control study. J Hip Preserv Surg 2018; 5: 240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Degen RM, Pan TJ, Chang B et al. Risk of failure of primary hip arthroscopy—a population-based study. J Hip Preserv Surg 2017; 4: 214–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Poehling-Monaghan KL, Krych AJ, Levy BA et al. Female sex is a risk factor for failure of hip arthroscopy performed for acetabular retroversion. Orthop J Sports Med 2017; 5: 232596711773747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saadat E, Martin SD, Thornhill TS et al. Factors associated with the failure of surgical treatment for femoroacetabular impingement: review of the literature. Am J Sports Med 2014; 42: 1487–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beckmann JT, Havrilak EE, Millis MB et al. Functional outcome assessment in hip preservation surgery. JBJS Rev 2018; 6: e6. [DOI] [PubMed] [Google Scholar]
- 13. Reiman MP, Peters S, Sylvain J et al. Prevalence and consistency in surgical outcome reporting for femoroacetabular impingement syndrome: a scoping review. Arthroscopy 2018; 34: 1319–28.e9. [DOI] [PubMed] [Google Scholar]
- 14. Griffin DR, Parsons N, Mohtadi NGH et al. ; Multicenter Arthroscopy of the Hip Outcomes Research Network. A short version of the international Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy 2012; 28:611–6; quiz 616–8. [DOI] [PubMed] [Google Scholar]
- 15. Griffin DR, Dickenson EJ, O'Donnell J et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016; 50: 1169–76. [DOI] [PubMed] [Google Scholar]
- 16. Harris JD, Brand JC, Cote MP et al. Research pearls: the significance of statistics and perils of pooling. Part 1: clinical versus statistical significance. Arthroscopy 2017; 33: 1102–12. [DOI] [PubMed] [Google Scholar]
- 17. Cvetanovich GL, Weber AE, Kuhns BD et al. Clinically meaningful improvements after hip arthroscopy for femoroacetabular impingement in adolescent and young adult patients regardless of gender. J Pediatr Orthop 2018; 38: 465–70. [DOI] [PubMed] [Google Scholar]
- 18. Levy DM, Kuhns BD, Chahal J et al. Hip arthroscopy outcomes with respect to patient acceptable symptomatic state and minimal clinically important difference. Arthroscopy 2016; 32: 1877–86. [DOI] [PubMed] [Google Scholar]
- 19. Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med 2013; 41: 2065–73. [DOI] [PubMed] [Google Scholar]
- 20. Nwachukwu BU, Chang B, Fields K et al. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med 2017; 45: 1297–303. [DOI] [PubMed] [Google Scholar]
- 21. Chahal J, Van Thiel GS, Mather RC et al. The patient acceptable symptomatic state for the modified Harris Hip Score and hip outcome score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med 2015; 43: 1844–9. [DOI] [PubMed] [Google Scholar]
- 22. Martin RL, Kivlan BR, Christoforetti JJ et al. Minimal clinically important difference and substantial clinical benefit values for the 12-item international Hip Outcome Tool. Arthroscopy 2019; 35: 411–6. [DOI] [PubMed] [Google Scholar]
- 23. Nwachukwu BU, Chang B, Beck EC et al. How Should We Define Clinically Significant Outcome Improvement on the iHOT-12? HSS J 2018. Available at: 10.1007/s11420-018-9646-0. Accessed: 25 March 2019. [DOI] [PMC free article] [PubMed]
- 24. McGee S. Simplifying likelihood ratios. J Gen Intern Med 2002; 17: 647–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sloane PD. Essentials of Family Medicine. Lippincott Williams & Wilkins, 2008. [Google Scholar]
- 26. Domb BG, Martin TJ, Gui C et al. Predictors of clinical outcomes after hip arthroscopy: a prospective analysis of 1038 patients with 2-year follow-up. Am J Sports Med 2018; 46: 1324–30. [DOI] [PubMed] [Google Scholar]
- 27. Redmond JM, Gupta A, Dunne K et al. What factors predict conversion to THA after arthroscopy? Clin Orthop Relat Res 2017; 475: 2538–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Griffin DW, Kinnard MJ, Formby PM et al. Outcomes of hip arthroscopy in the older adult: a systematic review of the literature. Am J Sports Med 2016; 45: 1928–36. [DOI] [PubMed] [Google Scholar]
- 29. Devane P, Horne G, Gehling DJ. Oxford hip scores at 6 months and 5 years are associated with total hip revision within the subsequent 2 years. Clin Orthop Relat Res 2013; 471: 3870–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Eneqvist T, Nemes S, Bülow E et al. Can patient-reported outcomes predict re-operations after total hip replacement? Int Orthop 2018; 42: 273–9. [DOI] [PubMed] [Google Scholar]
- 31. Rothwell AG, Hooper GJ, Hobbs A et al. An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg Br 2010; 92: 413–8. [DOI] [PubMed] [Google Scholar]
- 32. Basques BA, Waterman BR, Ukwuani G et al. Preoperative symptom duration is associated with outcomes after hip arthroscopy. Am J Sports Med 2019; 47: 131–7. [DOI] [PubMed] [Google Scholar]
- 33. Cvetanovich GL, Weber AE, Kuhns BD et al. Hip arthroscopic surgery for femoroacetabular impingement with capsular management: factors associated with achieving clinically significant outcomes. Am J Sports Med 2018; 46: 288–96. [DOI] [PubMed] [Google Scholar]
- 34. Nwachukwu BU, Fields K, Chang B et al. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med 2017; 45: 612–9. [DOI] [PubMed] [Google Scholar]