Abstract
The lockdown response to COVID-19 has resulted in an unprecedented reduction in global economic activity and associated air pollutant levels, especially from a decline in land transportation. We utilized a network of >10,000 air quality stations distributed over 34 countries during lockdown dates up until 15 May 2020 to obtain lockdown related anomalies for nitrogen dioxide, ozone and particulate matter smaller than 2.5 μm in diameter (PM2.5). Pollutant anomalies were related to short-term health outcomes using empirical exposure-response functions. We estimate that there were a net total of 49,900 (11,000 to 90,000; 95% confidence interval) excess deaths and 89,000 (64,700 to 107,000) pediatric asthma emergency room visits avoided during lockdowns. In China and India alone, the PM2.5-related avoided excess mortality was 19,600 (15,300 to 24,000) and 30,500 (5700 to 68,000), respectively. While the state of COVID-19 imposed lockdown is not sustainable, these findings illustrate the potential health benefits gained by reducing “business as usual” air pollutant emissions from economic activities primarily through finding alternative transportation solutions.
Keywords: Particulate matter, Pediatric asthma, Public health, Mortality, Nitrogen dioxide
1. Introduction
Long-term exposure to air pollution including fine particulate matter with a diameter less than 2.5 μm (PM2.5) and ozone (O3) are estimated to be associated with ~8.8 million excess deaths from acute respiratory infections and non-communicable diseases annually (Burnett et al., 2018; Chowdhury et al., 2020; Lelieveld et al., 2020), while exposure to nitrogen dioxide (NO2) results in 4 million new pediatric asthma cases annually (Achakulwisut et al., 2019). Despite the apparent global air pollution “pandemic”, anthropogenic emissions continue to increase in most low- and middle-income and some high-income nations (Crippa et al., 2018; Hoesly et al., 2018; Li et al., 2017). With the rapid emergence of the recent coronavirus (COVID-19), and the associated government enforced lockdown measures aimed at containment, economic activity, particularly in the transportation sector, has dramatically reduced in many countries (Cohen and Kupferschmidt, 2020; Venter et al., 2020). Lockdown measures have included partial or complete closure of international borders, schools, small business and even restricted citizen mobility in some countries.
The reductions in traffic and industry were associated with decreases in surface concentrations of air pollutants worldwide (Bao and Zhang, 2020; Dantas et al., 2020; Muhammad et al., 2020; Nakada and Urban, 2020; Venter et al., 2020). These changes offer an unprecedented opportunity to estimate the short-term effects of the enforced lockdown on global human health burden attributable to air pollution. We utilized ground-level measurements from >10,000 air quality stations in 34 countries after accounting for meteorological variations to make explicit links between air pollutant changes and the associated public health burden. The detailed methodology on estimating the air pollutant anomalies due to enforced lockdowns is described elsewhere (Venter et al., 2020), which we will refer to frequently in this article. In this short communication we use established exposure-response functions to estimate mortality and pediatric asthma emergency room visits (ERVs) that have potentially been avoided due to air pollution declines during lockdown.
2. Methods
2.1. Estimating the air pollutant anomalies
We obtained the data for NO2, O3 and PM2.5 from >10,000 in-situ air quality monitoring stations across the 34 countries considered in this study. The countries were chosen based on the availability of air quality data and represent mostly industrialized nations. Data were obtained from January 2017 until 15 May 2020. These data were accessed from the OpenAQ Platform (www.openaq.org) and originate from government- and research-grade sources. Commencement dates of enforced lockdown were obtained for each country to isolate the effect of COVID-19 mitigation measures by calculating lockdown pollutant levels for each country separately. For countries with variable internal lockdown dates (e.g. variation between states in the USA), we used the average starting date over the country. As air pollution anomalies measured during lockdowns are not necessarily attributable to localized reduction of economic activity, but may also be influenced by meteorological variability during the lockdown periods, we built a weather-benchmark model to separate the impact of prevailing meteorological conditions. We defined lockdown air pollution anomalies as the difference between population weighted observed pollutant concentrations and the population-weighted weather-benchmark concentrations for lockdown dates up until 15 May 2020. These anomalies were utilized to estimate the resultant changes in air pollution related health burden associated with the COVID19 imposed lockdowns. For details on the methodology to estimate the air pollution anomalies and meteorological control please refer to Venter et al. (2020).
2.2. Linking air pollution anomalies to public health burden
To relate COVID-19 lockdown air pollution anomalies to all-cause (based on historical data and therefore excluding COVID-19 as a cause) mortality and pediatric asthma exacerbation we applied short-term (daily) exposure-response relationships reported in the recent literature. We obtained relative risks from recent studies on the relationship between daily mortality and O3 (Vicedo-Cabrera et al., 2020) and PM2.5 (Liu et al., 2019) resulting from the Multi-City Multi-Country (MCC) Collaborative Research Network (Gasparrini et al., 2015). For NO2-mortality responses, we used relative risks reported in a meta-analysis which accounted for the effect of particulate matter to extract excess mortality solely attributable to NO2 (Mills et al., 2016). Pediatric (<18 years) short-term relative risks for asthma-related emergency room visits (ERVs) in response to NO2, O3 and PM2.5 were derived from a global meta-analysis of 87 studies (Zheng et al., 2015). These data are not country-specific and we therefore applied the same relative risk rate to all countries in our study.
The daily health burden (mortality and asthma ERVs) for each country was derived with the formula:where Mo is the baseline mortality rate or asthma ERV incidence rate (/100,000 population per year) and Pop is the total population. Mo for mortality or asthma were obtained from the Institute for Health Metrics and Evaluation (IHME) for the 34 countries in our study (Roth et al., 2018), downloadable at the GDBx platform (http://ghdx.healthdata.org/). We used country-specific fractions of asthmatics visiting emergency rooms reported in Anenberg et al. (2018) to calculate Mo for asthma exacerbation. Population estimates for 2020 were calculated using the Gridded Population of the World (GPWv14) dataset (“Gridded Population of the World, Version 4 (GPWv4): Population Count, Revision 11,” 2018). RR is the relative risk derived from the literature after log-linear transformation. We used log-linear transformation as adopted by many others to prevent assumptions of linearity in the relationship between pollutant concentrations and health outcome (Achakulwisut et al., 2019; Anenberg et al., 2018; Chowdhury et al., 2020). We derive the transformed RR using:
where α is the pollutant concentration and γ is the low concentration threshold below which there is no risk of mortality or asthma incidence. Low concentration thresholds were derived from the associated literature for O3 (Vicedo-Cabrera et al., 2020) at 70 μg m−3; PM2.5 (Liu et al., 2019) at 4.1 μg m−3 and NO2 (Achakulwisut et al., 2019) at 2 ppb. Here β is defined by the function:where λ is the relative risk reported in the literature and ẟ is the concentration increment used. All three studies reported results relative to increments of 10 μg m−3.
The air pollution health burden anomaly coincident with COVID-19 lockdown was defined as:
where observed health burden was calculated based on actual pollutant concentrations and the benchmark values were those predicted from the weather benchmark model. We used 95% confidence intervals reported in the literature to derive uncertainty margins around our change estimates.
3. Results
As of 15 May 2020, of the 34 countries considered in this study, China (113 days) and Italy (84 days) enforced the longest lockdowns while Sweden (40 days) imposed the shortest. During lockdown dates, population-weighted global ground-level NO2 concentrations were on average 60% (population-weighted mean with 95% confidence interval 48%–72%) lower than those expected provided the prevailing meteorological conditions and time of year (weather-corrected benchmark). Similarly, global population-weighted PM2.5 declined by 31% (17%–45%), whereas O3 increased by 4% (−2%–10%). We refer the readers to Venter et al. (2020) for elaborated and country-specific results on air pollution anomalies during the lockdown.
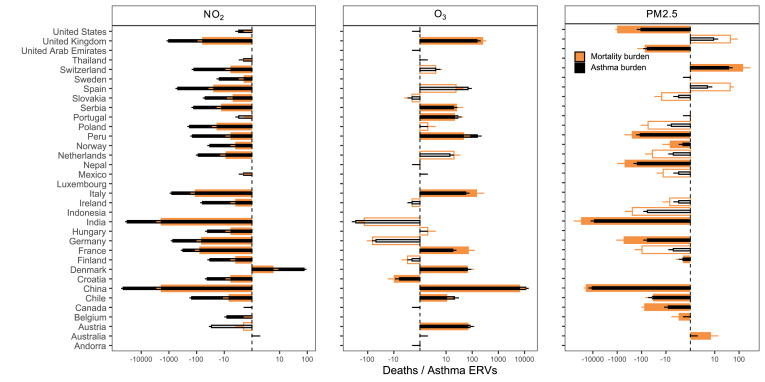
Using the weather-corrected ground-level air pollution anomalies during lockdown in combination with published exposure-response functions for NO2, O3 and PM2.5, we estimated changes in daily all-cause mortality and pediatric asthma emergency room visits (ERVs). We estimate a total of 49,900 (11,000 to 90,000) excess deaths and 89,000 (64,700 to 107,000) pediatric asthma ERVs avoided across 34 countries with recorded COVID-19 mitigation measures (Fig. 1 ; Table S1). The number of PM2.5-related excess deaths avoided (52,000; 103,00 to 94,600) exceeded those related to NO2 (4300; 2400 to 6300). The increase in O3 concentrations means that an additional 7300 (1100 to 13,000) excess deaths have likely occurred. NO2 reductions contributed to more avoided pediatric asthma ERVs (80800; 64500 to 96400) compared to PM2.5 (19500; 7300 to 24600). In China and India alone, the PM2.5-related reductions in excess mortality burden were 19,600 (15,300 to 24,000) and 30,500 (5700 to 68,000), respectively (Fig. 1; Table S1). These are countries with both the highest baseline pollution levels and population densities, and therefore have the most to gain from pollutant declines. The corresponding numbers for all the 34 countries are presented in SI Table 1.
Fig. 1.
Post-lockdown health burden changes attributable to air pollution. Air pollution anomalies during lockdown are converted to changes in mortality and asthma exacerbation (n = 34 countries). Total health burden avoided (-ve) and incurred (+ve) values are presented with bars along a log-transformed x-axis. 95% uncertainty intervals are marked with error bars. Hollow bars represent estimates where the change in pollutant concentrations were not significant (p > 0.05) after accounting for weather variations.
4. Discussion
We estimate that during the 2-3-month lockdown periods these pollution anomalies have significantly reduced the global burden of disease. We by no means imply that global pandemics such as the COVID-19, nor lockdown actions, are beneficial for public health. However, we suggest the current situation is a useful lens through which we can view the global air pollution “pandemic”. Time will tell how significant the overall change in health burden has actually been. Nevertheless, the early evidence presented here suggests it is likely significant. Reduced excess mortality from air pollution thus appears to be a co-benefit to the reduced number of COVID-19 deaths from the lockdown measures, although more accurate, quantitative assessments must await termination of the crisis.
Making explicit links between ambient air pollution and human health burden relies on several assumptions that are difficult to verify a priori. First, using relative risk rates from select meta-analyses and multi-city (n > 406) short-term time-series association studies (Liu et al., 2019; Mills et al., 2016; Vicedo-Cabrera et al., 2020; Zheng et al., 2015) to make inferences over entire countries rests on the assumption that city- or cohort-specific response rates are generalizable to broader populations. Similarly, generalizing point-based air pollution measurements to larger regions and countries may not be accurate given that air quality can be spatially variable. While this is likely to introduce uncertainty, the dearth of representative data necessities these generalizations, and this approach has been used by numerous studies at the global scale (Achakulwisut et al., 2019; Chowdhury et al., 2020; Lelieveld et al., 2020). Further, we acknowledge that our results may be affected by harvesting effects (Schwartz, 2001), where deaths attributed to air pollution might have otherwise occurred in the immediate future. Note that this also applies to death counts attributed to COVID-19. We also acknowledge that altered mobility patterns have changed the time people spent indoors and we do not account for indoor sources of PM2.5 pollution which are unlikely to be reduced by lockdown measures (Aunan et al., 2018; Shen et al., 2020). As smoke from household stoves adds substantially to population exposure for those who depend on solid fuels, accounting for ambient air pollution only could imply a misclassification of exposure and biased health burden estimates (Shen et al., 2020). The additional health burden observed due to increases in ozone may be partially explained by ozone's seasonality, with summer time peaks in the northern hemisphere. Finally, the baseline mortality rates available to us are from 2017 and therefore may be prone to ignoring before and after COVID-19 onset differences in baseline mortality incidence.
Despite these assumptions and the associated uncertainty, the analysis and results presented here can provide useful insights to raise awareness and orientate interventions regarding the global effects of air pollution on human health. They should be interpreted as preliminary lessons from the Corona crisis. As the science evolves, and the COVID-19 pandemic plays out, empirical data will emerge to fill in the knowledge gaps and uncertainties associated with air pollution health burden attribution. More data will be needed to fully account for lockdown-induced changes to cofactors like hospital capacity, alcohol use and mental health, which have been significantly altered by declines in economic activity. Further, we were not able to calculate the extent to which air pollution reductions have mitigated COVID-19 deaths. For instance, positive associations have been reported between air pollution and SARS case fatalities in China during 2003 (Cui et al., 2003) and preliminary analysis has revealed similar patterns for COVID-19 (Conticini et al., 2020; Wu et al., 2020). Therefore, our estimates may represent lower limits after considering the air pollution reductions as a cofactor in COVID-19 case recoveries.
Credit author statement
Z.S.V., K.A., S.C., and J.L. designed research; Z.S.V. performed research; Z.S.V. analyzed data; and Z.S.V., K.A., S.C., and J.L. wrote the paper.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
K.A. was supported by funding from the European Union's Horizon 2020 research and innovation program under Grant Agreement 820655 (EXHAUSTION). We thank the reviewers for their constructive comments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110403.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Achakulwisut P., Brauer M., Hystad P., Anenberg S.C. Global, national, and urban burdens of paediatric asthma incidence attributable to ambient NO2 pollution: estimates from global datasets. Lancet Planet. Health. 2019;3:e166–e178. doi: 10.1016/S2542-5196(19)30046-4. [DOI] [PubMed] [Google Scholar]
- Anenberg S.C., Henze D.K., Tinney V., Kinney P.L., Raich W., Fann N., Malley C.S., Roman H., Lamsal L., Duncan B., Martin R.V., Donkelaar A. Van, Brauer M., Doherty R., Jonson J.E., Davila Y., Sudo K., Kuylenstierna J.C.I. vol. 126. 2018. pp. 1–14. (Estimates of the Global Burden of Ambient PM 2 : 5 , Ozone , and NO 2 on Asthma Incidence and Emergency Room Visits). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aunan K., Ma Q., Lund M.T., Wang S. Population-weighted exposure to PM2.5 pollution in China: an integrated approach. Environ. Int. 2018;120:111–120. doi: 10.1016/j.envint.2018.07.042. [DOI] [PubMed] [Google Scholar]
- Bao R., Zhang A. Does lockdown reduce air pollution? Evidence from 44 cities in northern China. Sci. Total Environ. 2020;731:139052. doi: 10.1016/j.scitotenv.2020.139052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett R., Chen H., Szyszkowicz M., Fann N., Hubbell B., Pope C.A., Apte J.S., Brauer M., Cohen A., Weichenthal S., Coggins J., Di Q., Brunekreef B., Frostad J., Lim S.S., Kan H., Walker K.D., Thurston G.D., Hayes R.B., Lim C.C., Turner M.C., Jerrett M., Krewski D., Gapstur S.M., Diver W.R., Ostro B., Goldberg D., Crouse D.L., Martin R.V., Peters P., Pinault L., Tjepkema M., van Donkelaar A., Villeneuve P.J., Miller A.B., Yin P., Zhou M., Wang L., Janssen N.A.H., Marra M., Atkinson R.W., Tsang H., Quoc Thach T., Cannon J.B., Allen R.T., Hart J.E., Laden F., Cesaroni G., Forastiere F., Weinmayr G., Jaensch A., Nagel G., Concin H., Spadaro J.V. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. Unit. States Am. 2018;115:9592. doi: 10.1073/pnas.1803222115. LP – 9597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury S., Pozzer A., Dey S., Klingmüller K., Lelieveld J. Changing risk factors that contribute to premature mortality from ambient air pollution between 2000 and 2015. Environ. Res. Lett. 2020;15 doi: 10.1088/1748-9326/ab8334. [DOI] [Google Scholar]
- Cohen J., Kupferschmidt K. Strategies shift as coronavirus pandemic looms. Science. 2020;80(367):962. doi: 10.1126/science.367.6481.962. LP – 963. [DOI] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020;261:114465. doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crippa M., Guizzardi D., Muntean M., Schaaf E., Dentener F., van Aardenne J.A., Monni S., Doering U., Olivier J.G.J., Pagliari V., Janssens-Maenhout G. Gridded emissions of air pollutants for the period 1970–2012 within EDGAR v4.3.2. Earth Syst. Sci. Data. 2018;10:1987–2013. doi: 10.5194/essd-10-1987-2018. [DOI] [Google Scholar]
- Cui Y., Zhang Z.-F., Froines J., Zhao J., Wang H., Yu S.-Z., Detels R. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ. Health. 2003;2:15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantas G., Siciliano B., França B.B., da Silva C.M., Arbilla G. The impact of COVID-19 partial lockdown on the air quality of the city of Rio de Janeiro, Brazil. Sci. Total Environ. 2020;729:139085. doi: 10.1016/j.scitotenv.2020.139085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A., Guo Y., Hashizume M., Lavigne E., Zanobetti A., Schwartz J., Tobias A., Tong S., Rocklöv J., Forsberg B., Leone M., De Sario M., Bell M.L., Guo Y.-L.L., Wu C., Kan H., Yi S.-M., de Sousa Zanotti Stagliorio Coelho M., Saldiva P.H.N., Honda Y., Kim H., Armstrong B. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386:369–375. doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gridded Population of the World Version 4 (GPWv4): population count, revision 11. Cent. Int. Earth Sci. Inf. Netw. - CIESIN - Columbia Univ. 2018 doi: 10.7927/H4JW8BX5. [WWW Document] [DOI] [Google Scholar]
- Hoesly R.M., Smith S.J., Feng L., Klimont Z., Janssens-Maenhout G., Pitkanen T., Seibert J.J., Vu L., Andres R.J., Bolt R.M., Bond T.C., Dawidowski L., Kholod N., Kurokawa J.-I., Li M., Liu L., Lu Z., Moura M.C.P., O'Rourke P.R., Zhang Q. Historical (1750–2014) anthropogenic emissions of reactive gases and aerosols from the Community Emissions Data System (CEDS) Geosci. Model Dev. 2018;11:369–408. doi: 10.5194/gmd-11-369-2018. [DOI] [Google Scholar]
- Lelieveld J., Pozzer A., Pöschl U., Fnais M., Haines A., Münzel T. Loss of life expectancy from air pollution compared to other risk factors: a worldwide perspective. Cardiovasc. Res. 2020 doi: 10.1093/cvr/cvaa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., McLinden C., Fioletov V., Krotkov N., Carn S., Joiner J., Streets D., He H., Ren X., Li Z., Dickerson R.R. India is overtaking China as the world's largest emitter of anthropogenic sulfur dioxide. Sci. Rep. 2017;7:14304. doi: 10.1038/s41598-017-14639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Chen R., Sera F., Vicedo-Cabrera A.M., Guo Y., Tong S., Coelho M.S.Z.S., Saldiva P.H.N., Lavigne E., Matus P., Valdes Ortega N., Osorio Garcia S., Pascal M., Stafoggia M., Scortichini M., Hashizume M., Honda Y., Hurtado-Díaz M., Cruz J., Nunes B., Teixeira J.P., Kim H., Tobias A., Íñiguez C., Forsberg B., Åström C., Ragettli M.S., Guo Y.-L., Chen B.-Y., Bell M.L., Wright C.Y., Scovronick N., Garland R.M., Milojevic A., Kyselý J., Urban A., Orru H., Indermitte E., Jaakkola J.J.K., Ryti N.R.I., Katsouyanni K., Analitis A., Zanobetti A., Schwartz J., Chen J., Wu T., Cohen A., Gasparrini A., Kan H. Ambient particulate air pollution and daily mortality in 652 cities. N. Engl. J. Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills I.C., Atkinson R.W., Anderson H.R., Maynard R.L., Strachan D.P. Distinguishing the associations between daily mortality and hospital admissions and nitrogen dioxide from those of particulate matter: a systematic review and meta-analysis. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-010751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad S., Long X., Salman M. COVID-19 pandemic and environmental pollution: a blessing in disguise? Sci. Total Environ. 2020;728:138820. doi: 10.1016/j.scitotenv.2020.138820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakada L.Y.K., Urban R.C. COVID-19 pandemic: impacts on the air quality during the partial lockdown in São Paulo state, Brazil. Sci. Total Environ. 2020;730:139087. doi: 10.1016/j.scitotenv.2020.139087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth G.A., Abate D., Abate K.H., Abay S.M., Abbafati C., Abbasi N., et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz J. Is there harvesting in the association of airborne particles with daily deaths and hospital admissions? Epidemiology. 2001;12 doi: 10.1097/00001648-200101000-00010. [DOI] [PubMed] [Google Scholar]
- Shen H., Shen G., Chen Y., Russell A., Hu Y., Duan X., Meng W., Xu Y., Yun X., Lyu B., Zhao S., Hakami A., Tao S., Smith K.R. EarthArXiv; 2020. Increased Air Pollution Exposure Among the Chinese Population during the National Quarantine in 2020. [DOI] [PubMed] [Google Scholar]
- Vicedo-Cabrera A.M., Sera F., Liu C., Armstrong B., Milojevic A., Guo Y., Tong S., Lavigne E., Kyselý J., Urban A., Orru H., Indermitte E., Pascal M., Huber V., Schneider A., Katsouyanni K., Samoli E., Stafoggia M., Scortichini M., Hashizume M., Honda Y., Ng C.F.S., Hurtado-Diaz M., Cruz J., Silva S., Madureira J., Scovronick N., Garland R.M., Kim H., Tobias A., Íñiguez C., Forsberg B., Åström C., Ragettli M.S., Röösli M., Guo Y.-L.L., Chen B.-Y., Zanobetti A., Schwartz J., Bell M.L., Kan H., Gasparrini A. Short term association between ozone and mortality: global two stage time series study in 406 locations in 20 countries. BMJ. 2020;368:m108. doi: 10.1136/bmj.m108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venter Z.S., Aunan K., Chowdhury S., Lelieveld J. Proceedings of the National Academy of Sciences. 2020. COVID-19 lockdowns cause global air pollution declines. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States: a Nationwide Cross-Sectional Study. medRxiv 2020.04.05.20054502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., Ding H., Jiang L., Chen S., Zheng J., Qiu M., Zhou Y., Chen Q., Guan W. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PloS One. 2015;10 doi: 10.1371/journal.pone.0138146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.