Abstract
Objective
We aimed to review data about delaying strategies for the management of hepatobiliary cancers requiring surgery during the covid-19 pandemic.
Background
Given the covid-19 pandemic, many jurisdictions, to spare resources, have limited access to operating rooms for elective surgical activity, including cancer, thus forcing deferral or cancellation of cancer surgeries. Surgery for hepatobiliary cancer is high-risk and particularly resource-intensive. Surgeons must critically appraise which patients will benefit most from surgery and which ones have other therapeutic options to delay surgery. Little guidance is currently available about potential delaying strategies for hepatobiliary cancers when surgery is not possible.
Methods
An international multidisciplinary panel reviewed the available literature to summarize data relating to standard-of-care surgical management and possible mitigating strategies to be used as a bridge to surgery for colorectal liver metastases, hepatocellular carcinoma, gallbladder cancer, intrahepatic cholangiocarcinoma, and hilar cholangiocarcinoma.
Results
Outcomes of surgery during the covid-19 pandemic are reviewed. Resource requirements are summarized, including logistics and adverse effects profiles for hepatectomy and delaying strategies using systemic, percutaneous and radiation ablative, and liver embolic therapies. For each cancer type, the long-term oncologic outcomes of hepatectomy and the clinical tools that can be used to prognosticate for individual patients are detailed.
Conclusions
There are a variety of delaying strategies to consider if availability of operating rooms decreases. This review summarizes available data to provide guidance about possible delaying strategies depending on patient, resource, institution, and systems factors. Multidisciplinary team discussions should be leveraged to consider patient- and tumour-specific information for each individual case.
Keywords: covid-19, coronavirus, hepatobiliary cancer, hcc, metastases, cholangiocarcinoma, gallbladder carcinoma
INTRODUCTION
The evolving covid-19 pandemic is placing unprecedented pressures on health systems. Many jurisdictions have cancelled or delayed elective surgical activity to spare precious hospital, critical care, and personal protective equipment resources; to increase system capacity; and to limit nosocomial spread of covid-191–4. This sudden scale-back in operative resources has led to re-triaging and prioritization of elective surgeries, including cancer cases. As covid-19 pressures on local resources mount, operative case categorization changes, and criteria become more stringent, resulting in a higher number of cancer surgeries potentially being deferred5.
Delays in cancer surgery could risk losing a window for resection, compromising curative-intent surgery, or delaying palliation, with impacts that can vary depending on the timing of the delay in the cancer care continuum. Furthermore, as hospital resources—including critical-care and specialized staff—become less available, perioperative outcomes could worsen. The ability to progress patients through the usual postoperative care pathways and to rescue potential complications could be compromised. In the mode of “safety first,” that compromised ability shifts the risk–benefit balance of surgery for individual patients and diseases, making changes to the usual decision-making and triaging for surgical cancer care inevitable and necessary.
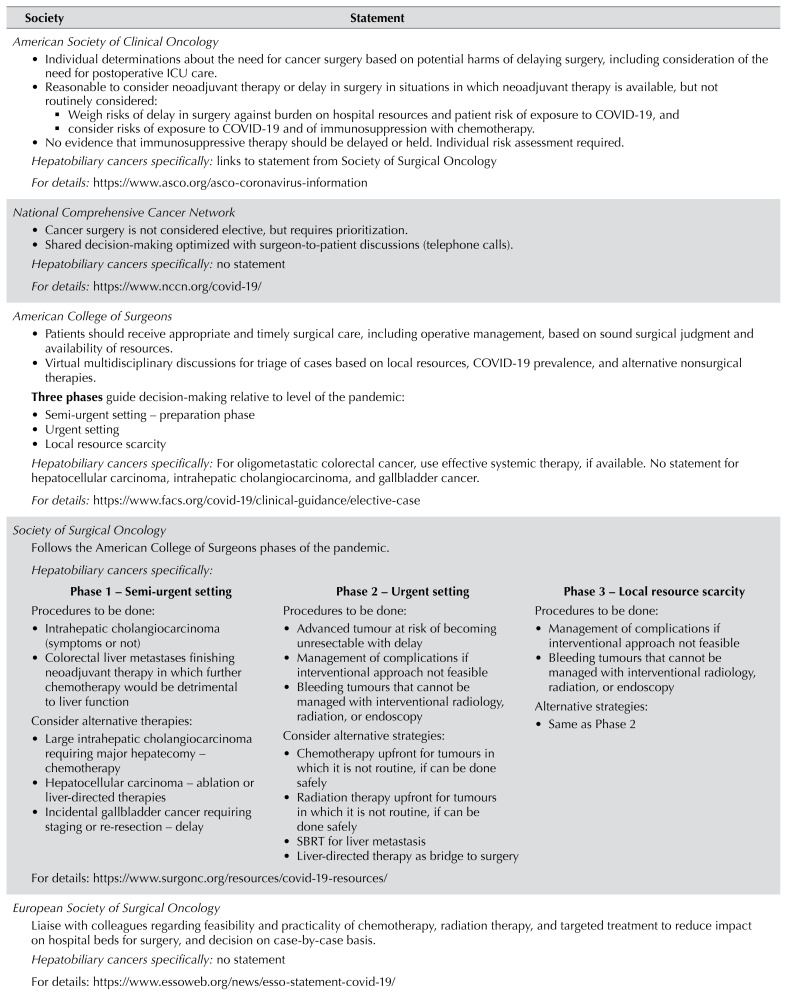
Governing bodies and surgical societies have released statements about the need to delay and prioritize elective surgeries, including those for cancer5,6. However, those high-level statements lack either detailed disease- and patient-specific guidance or the data and resource information to support decision-making (Table I)7–9.
TABLE I.
Summary of statements from major surgical and oncology societies about cancer surgery and hepatobiliary malignancy during the COVID-19 pandemic
| Society | Statement | |
|---|---|---|
American Society of Clinical Oncology
For details: https://www.asco.org/asco-coronavirus-information | ||
|
| ||
National Comprehensive Cancer Network
| ||
| Hepatobiliary cancers specifically: no statement For details: https://www.nccn.org/covid-19/ | ||
|
| ||
American College of Surgeons
For details: https://www.facs.org/covid-19/clinical-guidance/elective-case | ||
|
| ||
|
Society of Surgical Oncology Follows the American College of Surgeons phases of the pandemic. Hepatobiliary cancers specifically: | ||
| Phase 1 – Semi-urgent setting | Phase 2 – Urgent setting | Phase 3 – Local resource scarcity |
Procedures to be done:
|
Procedures to be done:
|
Procedures to be done:
|
| For details: https://www.surgonc.org/resources/covid-19-resources/ | ||
|
| ||
|
European Society of Surgical Oncology Liaise with colleagues regarding feasibility and practicality of chemotherapy, radiation therapy, and targeted treatment to reduce impact on hospital beds for surgery, and decision on case-by-case basis. Hepatobiliary cancers specifically: no statement For details: https://www.essoweb.org/news/esso-statement-covid-19/ | ||
|
Americas Hepato-Pancreato-Biliary Association Follows the American College of Surgeons phases of the pandemic. Hepatobiliary cancers specifically:
| ||
| Phase 1 – Semi-urgent setting | Phase 2 – Urgent setting | Phase 3 – Local resources scarcity | |
|
|
|
| For details: https://www.sages.org/sages-ahpba-recommendations-surgical-management-of-hpb-cancer-covid-19/ | ||
ICU = intensive care unit; SBRT = stereotactic body radiation therapy; TACE = transarterial chemoembolization.
The logistics of care and operating room availability can shift quickly as the pandemic evolves, and surgical decisions have to rapidly adapt. Multiple factors to consider for each case include not just the usual disease and patient factors (chance for cure or further spread of the cancer, risk for complications), but also, particularly in the pandemic, hospital resource use [for example, the need for an intensive care unit (icu) stay], the likelihood of prolonged hospitalization, and risk of exposure to and outcomes of covid-19. Weighing all those considerations requires an understanding of expectations with standard-of-care surgery, available mitigating or delaying strategies and their outcomes, and the risks posed by covid-19 infection.
The aim of the present review was to provide detailed information to support decision-making for the surgical management of hepatobiliary cancers that can be adapted to rapidly evolving situations and surgical resource availability. Rather than developing guidelines or recommendations that could quickly become obsolete, we aimed to summarize within a single review the data to support difficult discussions and decisions. We focus on surgically treatable intrahepatic malignancies and endorse the logistics of operating room workflow and protocols during the pandemic that have previously been outlined3,10,11.
METHODS
A non-systematic search was conducted of the literature (as of 10 April 2020), surgical and oncology society guidelines, and expert statements about the management of the most common hepatobiliary malignancies in surgical oncology practice:
■ Colorectal liver metastases (crlms)
■ Hepatocellular carcinoma (hcc)
■ Gallbladder carcinoma (gbc)
■ Intrahepatic cholangiocarcinoma (icc)
■ Hilar cholangiocarcinoma
Relevant data about standard-of-care surgical management and possible mitigating strategies to be used as a bridge to surgery were extracted and summarized. The components of care summarized for each treatment strategy were: short-term outcomes (morbidity and mortality), long-term oncologic outcomes (survival), factors influencing and tools predicting outcomes, and resource requirements for therapy delivery. When available, we also abstracted data about patient outcomes with delays in surgery.
The search and data abstraction were performed by 2 authors (SB, JH), with subsequent review by a multidisciplinary (surgical, medical, and radiation oncology), international (North America, Australasia, and Europe) group of oncologists to ensure applicability within various health systems and in countries at different phases of the current pandemic. No formal consensus criteria were applied to the review.
RESULTS
Risk of COVID-19 for the Surgical Oncology Patient
Data about outcomes of covid-19–infected cancer patients are limited, particularly with respect to surgical oncology. Repeated visits to the hospital, risk from social and nosocomial contacts, and the immunosuppressive effects of surgical stress could contribute to a higher risk of developing covid-19 for patients with cancer12,13. However, that risk is highly confounded by the prevalence of asymptomatic covid-19 in the community and the lag between infection and symptoms. Information about vulnerability to covid-19 can guide decision-making for surgical cancer patients. Comorbidities associated with higher risk from covid-19 (for example, hypertension, diabetes, pulmonary disease, cardiovascular disease) and age could be used to arrive at the most optimal risk–benefit balance14.
Two major epidemiologic studies from China drew data from 18 and 10 cancer patients infected with covid-19 and suggested a higher rate of icu admission, need for ventilation, and death (39%) in that patient population compared with the general population (8%)12,13. The case fatality rate for all cancer patients with covid-19 infection is reported to be higher than the overall case fatality rate (5.6% vs. 2.3%), although no details are available about that subpopulation15. However, most Chinese patients with cancer and covid-19 in those series were 4 years or more from their initial cancer diagnosis, and only 1 had undergone surgery and 3 had received chemotherapy within a month of covid-19 infection12. A Chinese series of hospitalized patients with covid-19 that included 105 patients with and 233 without cancer observed that patients with cancer experienced higher rates of severe events of icu admission, mechanical ventilation, and death16. After adjusting for age, sex, and comorbidities, cancer was not independently associated with increased odds of icu admission (odds ratio: 1.5; 95% confidence interval: 0.70 to 3.1) or death (odds ratio: 2.2; 95% confidence interval: 0.46 to 5.2). Overall, those data cannot definitively support the idea that delaying therapy would protect from covid-19 infection. However, covid-19 infection manifesting during the postoperative period is associated with poor outcomes. An early publication described 34 patients who were operated on while incubating covid-19 that manifested clinically after surgery; all developed pneumonia, 44% required icu admission, and 20% died17. A large multicentre cohort study at 235 hospitals in 24 countries included 1128 patients who underwent any operation and were diagnosed with covid-19 within a window of 7 days preoperatively to 30 days postoperatively18. The overall 30-day mortality rate was 23.8%, and the rate of pulmonary complications was 51.2%.
Standard of Care and Role of the Multidisciplinary Team
Despite the limitations imposed by the covid-19 pandemic, surgeons should strive to provide standard-of-care therapy. All treatment decisions, particularly those in which standard therapy has to be altered or delayed, must be made in a multidisciplinary team. Given that access to chemotherapy and radiation therapies might also be restricted, ongoing communication with oncology colleagues is essential. Treatment options, risks and benefits, and the perceived outcome of each intervention have to be discussed with the patient to arrive at the situational best solution and at informed consent with the patient. Notably, patients and surgeons will have different personalities, values, and expectations, all of which could affect choice of treatment. However, opting for risk-averse pathways might also be justified for the common good in a situation in which resources and access to intensive care support might be restricted.
Therapeutic Options and Resource Use
Table II summarizes general resource use for possible treatment strategies, to be interpreted in light of specific institutional care processes and resource availability before, during, and after the pandemic.
TABLE II.
Safety profile and resource use for treatment strategies
| Strategy | Safety profile (adverse effects) | Clinical setting | Length of stay | Unplanned ICU admissiona | Typical PPEb | Immunosuppression |
|---|---|---|---|---|---|---|
| Hepatectomy | Major morbidity: 20% Mortality: 2% | Inpatient | 3–6 Days | 5%–10% | Yes | Relative: postoperative SIRS |
| Systemic therapy | Depends on regimen. Consider neutropenia and lymphopenia. | Outpatient | Recurrent visits (every 1–3 weeks) | Rare | Yes | Yes |
| Percutaneous ablation | 4% Grade 3 events | Outpatient Inpatient (possible OR) |
1 Day 1–2 Days |
Rare | Yes | No |
| Ablative radiation therapy (SBRT) | 6%–7% Grade 3 gastrointestinal events (if proximity to duodenum or stomach) | Outpatient | 3–5 Daily visits | Rare | No | No |
| Intra-arterial liver embolization | 15%–30% Pain, fatigue, vomiting | Outpatient Inpatient (possible OR) |
1 Day (might require repeats, 4–6 weeks apart) 1–2 Days |
Rare | Yes | No |
Excludes routine planned postoperative admissions for monitoring.
That is, mask, gown, gloves—PPE requirements for usual care (could vary during COVID-19 pandemic, depending on institutional protocols).
ICU = intensive care unit; PPE = personal protective equipment; SIRS = systemic inflammatory response syndrome; OR = operating room; SBRT = stereotactic body radiation therapy.
Hepatectomies are a heterogeneous group of procedures, ranging from laparoscopic wedge resection of a single segment to trisegmentectomy with bile duct resection and reconstruction19. Patients at highest risk of morbidity and mortality after hepatectomy are those with comorbidities, an age of 75 years or greater, or underlying cirrhosis; those undergoing major liver resection (≥4 liver segments), synchronous colorectal and liver resection, and biliary reconstruction; and those needing blood transfusions19–21. The risk of requiring care in an icu after surgery is higher for patients undergoing major hepatectomy and those receiving blood transfusions22. For patients with minor liver disease, a laparoscopic approach can be beneficial, with lower morbidity and a shorter hospital stay19.
The risk of morbidity and mortality can be predicted using the National Surgical Quality Improvement Program developed by the American College of Surgeons based on multi-institutional prospectively validated data23. Blood transfusion is another important marker of postoperative morbidity and higher use of resources after hepatectomy, and can be estimated using the validated transfusion risk score based on data about preoperative anemia, background liver disease, and extent of planned hepatectomy24,25. Transfusion is especially important to consider, given that the covid-19 pandemic can lead to allogeneic blood shortages as a result of physical distancing and confinement policies26.
Chemotherapy is delivered in an outpatient setting. It involves repeated visits to cancer clinics, with associated risks related to social exposure because of travel, waiting room crowding, and sequential use of a chemotherapy chair that could increase the risk of exposure to covid-19 infection. Moreover, chemotherapy means exposure to agents that might compromise the quality of the liver remnant and create a risk of immunosuppression27.
Percutaneous ablation, such as radiofrequency ablation (rfa), can be delivered as outpatient care in radiology suites or in the operating room, depending on the institution. Grade 3 adverse events in percutaneous ablation occur in 4%–5% of patients28. Ablative radiation therapy [stereotactic body radiation therapy (sbrt)] is an outpatient procedure in radiation therapy facilities. The adverse effects profile of sbrt is minimal, with a 6%–7% risk of grade 3 gastrointestinal toxicity29,30.
Finally, liver embolization is typically performed in the radiology suite or in the operating room, as an outpatient or inpatient procedure, depending on the institution. Post-embolization syndrome—with fever, abdominal pain, and elevated transaminases—is the most frequent complication31. For transarterial chemoembolization (tace, using drug-eluting beads containing irinotecan) in patients with crlms, 15%–30% experience either pain, vomiting, fatigue, or fever, with most adverse events being grade 232,33. For tace in patients with hcc, most adverse effects are also grade 2. Across studies, 20%–30% of patients experience either pain, fever, nausea, or fatigue, and 5%–30% can develop ascites depending on liver function31.
Colorectal Liver Metastases
Hepatectomy and Oncologic Outcomes
The 5-year overall survival (os) for patients with resectable crlms (liver only) can reach 60%, with a median os of 74 months after curative-intent surgery34,35. In a retrospective series of patients with fewer than 4 metachronous metastases treated between 2000 and 2010, longer time from diagnosis to crlm resection was associated with worse os36. Median os was 76 months in patients who underwent surgery within 3 months of diagnosis, compared with 58 months for those whose surgery occurred later, adjusted for preoperative receipt of chemotherapy.
Systemic Therapy
Median survival with systemic therapy alone for unresectable crlms has been reported to be 22 months for patients who do not achieve conversion to resectability37; other series have reported durations up to 40 months38. The availability of effective systemic therapies has led to an increased use of neoadjuvant chemotherapy. In patients with resectable liver metastases (low disease burden), upfront surgery is often favoured. However, for patients with larger lesions or borderline resectable disease, neoadjuvant chemotherapy is the preferred approach. In the neoadjuvant setting, chemotherapy can be used to assess disease biology and patient selection, with potential benefit in recurrence-free survival, but no proven gain in os39,40.
Recent guidance from the American College of Surgeons (24 March 2020) recommends that surgery be delayed for patients with oligometastatic colorectal cancer for which effective systemic therapy is available41. If case prioritization requires a delay in resection of crlms, administration of chemotherapy before resection would be reasonable. For patients who are finishing pre-hepatectomy chemotherapy initiated before an operating room resource restriction, consideration can be given to continuing with further cycles depending on patient tolerance and the balance between risk of hepatotoxicity from chemotherapy (given the expected future liver remnant) and the risk for disappearing metastases that will complicate future curative-intent resection.
Ablation
Data about the outcomes of percutaneous ablation come from cohorts of patients with unresectable crlms. In a phase ii randomized trial involving 119 patients with unresectable, liver-only crlms, better median os was observed for rfa combined with systemic therapy (45.6 months) than for systemic therapy alone (40.5 months)38. In retrospective studies of resectable disease, risk of local recurrence is higher and os is lower with ablative techniques than with resection42–44. Local recurrence and 5-year os after ablation are reported at 37% and 27% respectively for isolated crlms42. As evidenced by an ongoing randomized noninferiority trial comparing hepatectomy with ablation for resectable liver metastases, percutaneous ablation is considered by some to be a potential curative option for crlms45.
Retrospective series of patients with unresectable liver metastases treated with sbrt have shown promising disease control. Local control rates at 2 years range from 57% to 100% in patients with poor prognosis and unresectable disease46. In a phase ii trial comparing sbrt plus chemotherapy with chemotherapy alone for oligometastases (13% liver), median os was prolonged at 41 months for the sbrt regimen compared with 28 months for chemotherapy alone. Compared with percutaneous ablation, sbrt can treat larger lesions, but might be limited for crlms localized near the stomach or duodenum29,30. Treatment intent with sbrt is not curative; if used as a mitigating strategy, liver resection would subsequently be required. Surgery after sbrt is feasible, although not well described47.
If there is no access to the operating room or if pursuing chemotherapy is not possible (or both), ablation could be a delaying strategy to ensure local control while awaiting surgery. Curative-intent treatment requires subsequent resection of the ablated lesion when operating resources are available. The choice for ablation also depends on its technical limitations (tumour size, number, and localization) and required resources depending on institutional protocols (inpatient vs. outpatient care; operating room).
TACE
Another approach for patients with unresectable or medically inoperable disease is tace, with a goal of local control and improved os. No prospective comparison of tace with resection has been conducted. In the unresectable setting, tace using drug-eluting beads containing irinotecan has an overall radiologic response rate between 60% and 80%, and a median os ranging from 14 to 25 months33,48.
Clinical Risk Tools
Multiple patient and disease factors influence oncologic outcomes after hepatectomy for crlms; clinical risk tools can assist in estimating outcomes if necessary for decision-making49. The most common tool is the Clinical Risk Score50,51. Rated from 0 to 5, the Clinical Risk Score assigns 1 point for each of these factors: node-positive primary tumour, liver metastases larger than 5 cm, more than 1 lesion, serum carcinoembryonic antigen greater than 200 ng/mL, and a disease-free interval less than 12 months. A score of 0 corresponds to a 5-year os of 60%, and a score of 5, to a 5-year os of 14%. The Genetic and Morphological Evaluation score is a more recent tool that incorporates molecular information and has better discrimination than the Clinical Risk Score52. Six preoperative factors produce a total score in the range 0–7: KRAS mutation (1 point), serum carcinoembryonic antigen greater than 20 ng/mL (1 point), node-positive primary tumour (1 point), tumour burden score in the 3–8 range (1 point) or 9 and higher (2 points), and extrahepatic disease (2 points). The 5-year os estimate is 73.4% for patients at low risk (score: 0–1), 50.6% for those at medium risk (score: 2–3), and 11% for those at high risk (score: ≥4).
Hepatocellular Carcinoma
Hepatectomy and Oncologic Outcomes
Patients with Barcelona Clinic Liver Cancer (bclc) stage 0 or A hcc are considered for hepatectomy, with some surgeons considering resection for those with bclc B disease53,54. With hepatectomy, these are the estimates for 5-year os55:
■ for bclc 0: 86%.
■ for bclc A with 1 lesion of 2–5 cm or 2–3 lesions less than 3 cm: 69%.
■ for bclc A with 1 lesion of 5 cm or larger: 57%.
■ for bclc B with 2–3 lesions of 3 cm or larger, or with 4 or more lesions: 50%.
In the present review, we focus on patients who are candidates for resection and who might be delayed or reprioritized during the pandemic. Liver transplantation also plays a crucial role in the management of hcc. Transplantation presents unique considerations related to operating room resource availability, changes in the donor pool, risk for living donors, and risk of infection and transmission of covid-19, which are beyond the scope of the present review and have been summarized elsewhere56–58. Any consideration of strategies meant to mitigate operating room delays for resection of hcc should include the understanding that access to transplantation might still be compromised after the pandemic, such that delaying strategies should not rely on availability of salvage transplantation.
Ablation
Radiofrequency ablation is associated with local recurrence rates of 0.9%, 1.4%, and 25% for hccs of less than 2 cm, less than 3 cm, and 3–5 cm respectively59,60. Although no difference in os has been observed with liver resection or rfa for hccs less than 5 cm in randomized controlled trials, the local recurrence rate is higher with rfa (5-year recurrence-free survival: 51.3% vs. 28.7%; hazard ratio: 0.56; 95% confidence interval: 0.40 to 0.78)61. If ablation is used without subsequent resection, and if the tumour recurs, patients can be candidates for salvage resection or salvage transplantation with outcomes similar to those with upfront transplantation62.
The sbrt modality is used for unresectable hcc, but has not been prospectively compared with resection. Prospective series have demonstrated local control rates between 80% and 100% at 1–3 years63–65. The ability to safely deliver sbrt is restricted by the underlying liver function, with a Child–Pugh score of 8 or greater being a relative contraindication66. The modality can be a bridge to liver transplantation comparable to both tace and rfa67.
TACE
Outcomes of tace have been reported mostly for unresectable hcc, with the 5-year os being 30%68. Literature about neoadjuvant tace for hcc reported no difference in os between tace followed by hepatectomy and hepatectomy alone in higher-risk hcc69. If tace is used as a strategy to delay surgery, resection should eventually follow so as not to compromise os. Although operating time is longer after tace, postoperative morbidity and mortality are unchanged69,70.
Systemic Therapy
Sorafenib and lenvatinib are used for advanced and unresectable hcc, with a median os of 12–13 months being reported in the reflect trial71–73. The emergence of new data showing responses to lenvatinib as evidenced by the Response Evaluation Criteria in Solid Tumors could herald the use of systemic therapy to downstage or delay surgery until optimal conditions are achieved in patients who might not be eligible for other delaying strategies as described earlier.
Clinical Risk Tools
A variety of scoring tools are available to assess outcomes of liver transplantation for hcc, but fewer are available for hepatectomy. A risk score developed using the Surveillance, Epidemiology, and End Results program database incorporates sex, tumour size, number of tumours, presence of bilobar disease, and major vascular invasion to predict os, but has not been externally validated74. The predicted 5-year os is 69% with a low-risk score, 51% with a medium-risk score, and 19% with a high-risk score.
Gallbladder Cancer
Hepatectomy and Oncologic Outcomes
Gallbladder cancer amenable to resection most often presents incidentally after simple cholecystectomy75,76. After a negative metastatic work-up, indications for radical re-resection include T1b or higher node-positive disease or a positive cystic duct margin77. Resected localized gbc (stages I–II) typically has a 5-year os of 50%–60%78,79. Compared with simple cholecystectomy, radical resection with extended cholecystectomy is associated with improved os for T2 and higher disease78. In T1b tumours, radical resection has been associated with a decrease in the risk of local recurrence without improvement in os80. Major liver resection, including multivisceral resection, is advocated by some for os benefit, but in the setting of the pandemic, the associated increased risks of major morbidity, prolonged icu stay, and mortality should be carefully weighed against that benefit81,82. Finally, it should be mentioned that the extent of hepatectomy and lymph node dissection is debated and heterogeneous between studies, and that available data are biased by selection of fitter patients for extended resection83–86.
Delaying Strategies
For incidental gbc eligible for radical re-resection, delaying strategies can include observation with short-term re-imaging or chemotherapy76. Use of chemotherapy is contingent on the availability of an effective regimen for gbc, which can be appreciated based on data from the adjuvant setting. Although the bilcap trial’s intention-to-treat analysis was negative for its primary endpoint, the trial (which included all biliary tract cancers) indicated favourable os with 8 cycles (24 weeks) of capecitabine as adjuvant therapy in the per-protocol population (which excluded ineligible patients and patients failing to complete at least 1 cycle of capecitabine)87. Although statistical significance was not reached in bilcap’s intention-to-treat population, a survival benefit of several months for those patients with usually dismal outcomes can be considered clinically meaningful. Therefore, when tumour control is needed while surgery is delayed, chemotherapy could be considered88. While not supported with data, preoperative chemotherapy appears ethically acceptable given that it is currently the subject of a randomized controlled trial89 and has been introduced as routine in some centres90.
Clinical Risk Tools
Clinical tools for gbc detected incidentally after cholecystectomy or diagnosed on imaging are few, were developed on small cohorts, are not well validated, and include information available only after surgery91–93. One scoring system focused on preoperative factors, but included both surgical and nonsurgical (metastatic) cases94. That system uses age, Eastern Cooperative Oncology Group performance status, serum alkaline phosphatase, tumour size, and presence of metastasis to create a score from 0 to 30 to predict os. In surgical cases, median survival is 37 months for scores of 0–21.9, 30 months for scores of 22–25.9, 15 months for scores of 26–29.9, and 8 months for a score of 30.
Intrahepatic Cholangiocarcinoma
Hepatectomy
The typical curative-intent management of icc is hepatectomy, with a 5-year os of 30%95. Postoperative mortality of 7.6% after hepatectomy for primary liver tumours is considerably higher than the rate typically cited for all hepatectomies19.
Systemic Therapy
Retrospective cohort studies have reported on neoadjuvant chemotherapy for initially unresectable icc. Of 74 patients with locally advanced unresectable disease receiving various chemotherapy regimens (59% being doublet gemcitabine–oxaliplatin), 39 were converted to resectability (53%) after a median of 6 cycles96. Median os after resection in that group was 24 months, compared with 26 months in initially resectable icc.
Ablation
Ablative therapies appear to be effective in icc, although experience is limited. A meta-analysis of rfa reported local tumour progression in 21% of patients and a 5-year os of 25%97. A small series of sbrt observed a median os of 22 months with a 1-year local control rate of 78%98.
TACE
Radioembolization with 90Y and tace have both been used for unresectable icc. Median os was similar for the combination of drug-eluting beads containing irinotecan plus chemotherapy and for chemotherapy (gemcitabine–oxaliplatin) alone, at 12 and 11 months respectively; median os with conventional tace was 6 months99. In a meta-analysis, 90Y radioembolization was associated with a median os of 15 months100.
Clinical Risk Tools
Various prognostic tools have been described for icc, but none are universally accepted101. Few tools incorporate patient characteristics such as age and sex, and most rely on pathology variables that might not be available before surgery102–104. Recently, the LabScore combined carbohydrate antigen 19-9, neutrophil-to-lymphocyte ratio, platelets, and albumin into a published formula to predict 5-year os after resection as 55% for a score of 0–9, 38% for a score of 10–19, and 22% for a score of 20 or more105.
Hilar Cholangiocarcinoma
Hepatectomy and Oncologic Outcomes
For the few resectable hilar cholangiocarcinomas that are amenable to curative-intent treatment, the 5-year os is 8.4% in node-positive disease and 25.9% in node-negative disease106. Given the extent and complexity of hepatectomy, and the need for a biliary–enteric anastomosis, major morbidity and mortality are higher in these patients107.
Chemoradiation
Conversion from unresectable to resectable hilar cholangiocarcinoma has been reported with chemoradiation (11 of 15 patients at a single institution)108. For resectable or borderline resectable disease, single-centre experiences with neoadjuvant chemoradiation for mixed cohorts of hilar and extrahepatic cholangiocarcinoma have reported 90%–100% R0 resection rates and 25%–33% complete pathologic responses109,110. Thus, tumour control appears achievable with preoperative chemoradiation if surgery has to be delayed. Finally, for the select few patients with technically unresectable hilar cholangiocarcinoma who might be considered for transplantation, neoadjuvant chemoradiation offers benefits in selection and prognosis111.
SUMMARY
The covid-19 pandemic affects many treatment decisions for patients with and without the virus. Reduced access to the operating room and lessened availability of critical care services for postoperative management could force the use of treatment strategies outside the standard of care to delay surgery. A variety of delaying strategies could be considered if operating room availability decreases. All strategies have pros and cons for patients and health systems that should be weighed. The quality and availability of data are variable. Evidence comparing typical curative-intent surgery with delaying options is rarely available. In the present review, we summarized the available data to provide some guidance with respect to possible delaying strategies depending on patient, resource, institution, and systems factors. Multidisciplinary team discussions should be leveraged to consider patient- and tumour-specific information to make the best possible decision for each individual case. Finally, it is important to emphasize that the nonsurgical therapies discussed should be used only with the goal of maintaining tumour control while awaiting hepatectomy. Curative-intent resection remains the cornerstone of therapy and the ultimate goal.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Spinelli A, Pellino G. covid-19 pandemic: perspectives on an unfolding crisis. Br J Surg. 2020;107:785–7. doi: 10.1002/bjs.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the covid-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020 doi: 10.6004/jnccn.2020.7560. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Brindle ME, Gawande A. Managing covid-19 in surgical systems. Ann Surg. 2020;272:e1–2. doi: 10.1097/SLA.0000000000003923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iacobucci G. covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ. 2020;368:m1106. doi: 10.1136/bmj.m1106. [DOI] [PubMed] [Google Scholar]
- 5.American College of Surgeons (acs) COVID-19: Elective Case Triage Guidelines for Surgical Care [Web page] Chicago, IL: ACS; 2020. [Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case; cited 27 August 2020] [Google Scholar]
- 6.Morrison S. Elective surgery [media release] Canberra, Australia: Government of Australia; 2020. [Available online at: https://www.pm.gov.au/media/elective-surgery; cited 25 March 2020] [Google Scholar]
- 7.National Comprehensive Cancer Network (nccn) Short-Term Recommendations for Cutaneous Melanoma Management During COVID-19 Pandemic. Plymouth Meeting, PA: NCCN; 2020. [Available online at: https://www.nccn.org/covid-19/pdf/Melanoma.pdf; cited 27 August 2020] [Google Scholar]
- 8.Dietz JR, Moran MS, Isakoff SJ, et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the covid-19 pandemic. The COVID-19 Pandemic Breast Cancer Consortium. Breast Cancer Res Treat. 2020;181:487–97. doi: 10.1007/s10549-020-05644-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bartlett DL, Howe JR, Chang G, et al. Management of cancer surgery cases during the covid-19 pandemic: considerations. Ann Surg Oncol. 2020;27:1717–20. doi: 10.1245/s10434-020-08461-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brat GA, Hersey SP, Chhabra K, Gupta A, Scott J. Protecting surgical teams during the covid-19 outbreak: a narrative review and clinical considerations. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003926. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a covid-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth. 2020;67:756–8. doi: 10.1007/s12630-020-01617-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liang W, Guan W, Chen R, et al. Cancer patients in sars-cov-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–7. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang T, Du Z, Zhu F, et al. Comorbidities and multi-organ injuries in the treatment of covid-19. Lancet. 2020;395:e52. doi: 10.1016/S0140-6736(20)30558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (covid-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [online ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Dai M, Liu D, Liu M, et al. Patients with cancer appear more vulnerable to sars-cov-2: a multi-center study during the covid-19 outbreak. Cancer Discov. 2020 doi: 10.1158/2159-8290.CD-20-0422. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of covid-19 infection. eClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100331. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative sars-cov-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lassen K, Nymo LS, Olsen F, et al. Contemporary practice and short-term outcomes after liver resections in a complete national cohort. Langenbecks Arch Surg. 2019;404:11–19. doi: 10.1007/s00423-018-1737-3. [DOI] [PubMed] [Google Scholar]
- 20.Bennett S, Baker LK, Martel G, et al. The impact of perioperative red blood cell transfusions in patients undergoing liver resection: a systematic review. HPB (Oxford) 2017;19:321–30. doi: 10.1016/j.hpb.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Ulyett S, Shahtahmassebi G, Aroori S, et al. Comparison of risk-scoring systems in the prediction of outcome after liver resection. Perioper Med (Lond) 2017;6:22. doi: 10.1186/s13741-017-0073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim SH, Lee JG, Kwon SY, Lim JH, Kim WO, Kim KS. Is close monitoring in the intensive care unit necessary after elective liver resection? J Korean Surg Soc. 2012;83:155–61. doi: 10.4174/jkss.2012.83.3.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen ME, Bilimoria KY, Ko CY, Hall BL. Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg. 2009;208:1009–16. doi: 10.1016/j.jamcollsurg.2009.01.043. [DOI] [PubMed] [Google Scholar]
- 24.Lemke M, Law CH, Li J, et al. on behalf of the hpbconcept team. Three-point transfusion risk score in hepatectomy. Br J Surg. 2017;104:434–42. doi: 10.1002/bjs.10416. [DOI] [PubMed] [Google Scholar]
- 25.Lemke M, Mahar A, Karanicolas PJ, Coburn NG, Law CHL, Hallet J. Three point transfusion risk score in hepatectomy: an external validation using the American College of Surgeons–National Surgical Quality Improvement Program (acs-nsqip) HPB (Oxford) 2018;20:669–75. doi: 10.1016/j.hpb.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Pagano MB, Hess JR, Tsang HC, et al. Prepare to adapt: blood supply and transfusion support during the first 2 weeks of the 2019 novel coronavirus (covid-19) pandemic affecting Washington State. Transfusion. 2020;60:908–11. doi: 10.1111/trf.15789. [DOI] [PubMed] [Google Scholar]
- 27.Al-Shamsi HO, Alhazzani W, Alhuraiji A, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (covid-19) pandemic: an international collaborative group. Oncologist. 2020;25:e936–45. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lahat E, Eshkenazy R, Zendel A, et al. Complications after percutaneous ablation of liver tumors: a systematic review. Hepatobiliary Surg Nutr. 2014;3:317–23. doi: 10.3978/j.issn.2304-3881.2014.09.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanuki N, Takeda A, Oku Y, et al. Stereotactic body radiotherapy for small hepatocellular carcinoma: a retrospective outcome analysis in 185 patients. Acta Oncol. 2014;53:399–404. doi: 10.3109/0284186X.2013.820342. [DOI] [PubMed] [Google Scholar]
- 30.Takeda A, Sanuki N, Kunieda E. Role of stereotactic body radiotherapy for oligometastasis from colorectal cancer. World J Gastroenterol. 2014;20:4220–9. doi: 10.3748/wjg.v20.i15.4220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng X, Sun P, Hu QG, Song ZF, Xiong J, Zheng QC. Transarterial (chemo)embolization for curative resection of hepatocellular carcinoma: a systematic review and meta-analyses. J Cancer Res Clin Oncol. 2014;140:1159–70. doi: 10.1007/s00432-014-1677-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin RCG, Joshi J, Robbins K, et al. Hepatic intra-arterial injection of drug-eluting bead, irinotecan (debiri) in unresectable colorectal liver metastases refractory to systemic chemotherapy: results of multi-institutional study. Ann Surg Oncol. 2011;18:192–8. doi: 10.1245/s10434-010-1288-5. [DOI] [PubMed] [Google Scholar]
- 33.Fiorentini G, Aliberti C, Mulazzani L, et al. Chemoembolization in colorectal liver metastases: the rebirth. Anticancer Res. 2014;34:575–84. [PubMed] [Google Scholar]
- 34.Hallet J, Sa Cunha A, Adam R, et al. on behalf of the French Colorectal Liver Metastases Working Group, Association Française de Chirurgie. Factors influencing recurrence following initial hepatectomy for colorectal liver metastases. Br J Surg. 2016;103:1366–76. doi: 10.1002/bjs.10191. [DOI] [PubMed] [Google Scholar]
- 35.Pawlik TM, Scoggins CR, Zorzi D, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg. 2005;241:715–22. doi: 10.1097/01.sla.0000160703.75808.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leal JN, Bressan AK, Vachharajani N, et al. Time-to-surgery and survival outcomes in resectable colorectal liver metastases: a multi-institutional evaluation. J Am Coll Surg. 2016;222:766–79. doi: 10.1016/j.jamcollsurg.2016.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Folprecht G, Gruenberger T, Bechstein W, et al. Survival of patients with initially unresectable colorectal liver metastases treated with folfox/cetuximab or folfiri/cetuximab in a multidisciplinary concept (celim study) Ann Oncol. 2014;25:1018–25. doi: 10.1093/annonc/mdu088. [DOI] [PubMed] [Google Scholar]
- 38.Ruers T, Van Coevorden F, Punt CJ, et al. on behalf of the European Organisation for Research and Treatment of Cancer, the Gastro-Intestinal Tract Cancer Group, the Arbeitsgruppe Lebermetastasen und tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie, and the National Cancer Research Institute Colorectal Clinical Study Group. Local treatment of unresectable colorectal liver metastases: results of a randomized phase ii trial. J Natl Cancer Inst. 2017;109 doi: 10.1093/jnci/djx015. djx015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ciliberto D, Prati U, Roveda L, et al. Role of systemic chemotherapy in the management of resected or resectable colorectal liver metastases: a systematic review and meta-analysis of randomized controlled trials. Oncol Rep. 2012;27:1849–56. doi: 10.3892/or.2012.1740. [DOI] [PubMed] [Google Scholar]
- 40.Nordlinger B, Sorbye H, Glimelius B, et al. Perioperative folfox4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (eortc 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol. 2013;14:1208–15. doi: 10.1016/S1470-2045(13)70447-9. [DOI] [PubMed] [Google Scholar]
- 41.American College of Surgeons (acs) COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures [Web page] Chicago, IL: ACS; 2020. [Available at: https://www.facs.org/covid-19/clinical-guidance/triage; cited 28 August 2020] [Google Scholar]
- 42.Aloia TA, Vauthey JN, Loyer EM, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg. 2006;141:460–6. doi: 10.1001/archsurg.141.5.460. [DOI] [PubMed] [Google Scholar]
- 43.White RR, Avital I, Sofocleous CT, et al. Rates and patterns of recurrence for percutaneous radiofrequency ablation and open wedge resection for solitary colorectal liver metastasis. J Gastrointest Surg. 2007;11:256–63. doi: 10.1007/s11605-007-0100-8. [DOI] [PubMed] [Google Scholar]
- 44.Schiffman SC, Bower M, Brown RE, Martin RCG, McMasters KM, Scoggins CR. Hepatectomy is superior to thermal ablation for patients with a solitary colorectal liver metastasis. J Gastrointest Surg. 2010;14:1881–6. doi: 10.1007/s11605-010-1339-z. [DOI] [PubMed] [Google Scholar]
- 45.Puijk RS, Ruarus AH, Vroomen LGPH, et al. Colorectal liver metastases: surgery versus thermal ablation (collision)—a phase iii single-blind prospective randomized controlled trial. BMC Cancer. 2018;18:821. doi: 10.1186/s12885-018-4716-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wild AT, Yamada Y. Treatment options in oligometastatic disease: stereotactic body radiation therapy—focus on colorectal cancer. Visc Med. 2017;33:54–61. doi: 10.1159/000454685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gasent Blesa JM, Laforga Canales J, Alberola Soler A, Peiró Monzó F, Bertelli Puche J, Alberola Candel V. Isolated colorectal liver metastases locally progressing after stereotactic body radiotherapy rescued with surgery. Curr Oncol. 2009;16:76–80. doi: 10.3747/co.v16i5.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fiorentini G, Aliberti C, Tilli M, et al. Intra-arterial infusion of irinotecan-loaded drug-eluting beads (debiri) versus intravenous therapy (folfiri) for hepatic metastases from colorectal cancer: final results of a phase iii study. Anticancer Res. 2012;32:1387–95. [PubMed] [Google Scholar]
- 49.Mahar AL, Compton C, Halabi S, Hess KR, Weiser MR, Groome PA. Personalizing prognosis in colorectal cancer: a systematic review of the quality and nature of clinical prognostic tools for survival outcomes. J Surg Oncol. 2017;116:969–82. doi: 10.1002/jso.24774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230:309–18. doi: 10.1097/00000658-199909000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Beamish P, Lemke M, Li J, et al. on behalf of the hpbconcept team. Validation of Clinical Risk Score for colorectal liver metastases resected in a contemporary multicenter cohort. HPB (Oxford) 2017;19:675–81. doi: 10.1016/j.hpb.2017.03.010. [DOI] [PubMed] [Google Scholar]
- 52.Margonis GA, Sasaki K, Gholami S, et al. Genetic and Morphological Evaluation (game) score for patients with colorectal liver metastases. Br J Surg. 2018;105:1210–20. doi: 10.1002/bjs.10838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–14. doi: 10.1016/S0140-6736(18)30010-2. [DOI] [PubMed] [Google Scholar]
- 54.Wada H, Eguchi H, Noda T, et al. Selection criteria for hepatic resection in intermediate-stage (bclc stage B) multiple hepatocellular carcinoma. Surgery. 2016;160:1227–35. doi: 10.1016/j.surg.2016.05.023. [DOI] [PubMed] [Google Scholar]
- 55.Tsilimigras DI, Bagante F, Sahara K, et al. Prognosis after resection of Barcelona Clinic Liver Cancer (bclc) stage 0, A, and B hepatocellular carcinoma: a comprehensive assessment of the current bclc classification. Ann Surg Oncol. 2019;26:3693–700. doi: 10.1245/s10434-019-07580-9. [DOI] [PubMed] [Google Scholar]
- 56.Gori A, Dondossola D, Antonelli B, et al. Coronavirus disease 2019 and transplantation: a view from the inside. Am J Transplant. 2020;20:1939–40. doi: 10.1111/ajt.15853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kumar D, Manuel O, Natori Y, et al. covid-19: a global transplant perspective on successfully navigating a pandemic. Am J Transplant. 2020;20:1773–9. doi: 10.1111/ajt.15876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Michaels MG, La Hoz RM, Danziger-Isakov L, et al. Coronavirus disease 2019: implications of emerging infections for transplantation. Am J Transplant. 2020 doi: 10.1111/ajt.15832. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Livraghi T, Meloni F, Di Stasi M, et al. Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology. 2008;47:82–9. doi: 10.1002/hep.21933. [DOI] [PubMed] [Google Scholar]
- 60.Mulier S, Ni Y, Jamart J, Ruers T, Marchal G, Michel L. Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg. 2005;242:158–71. doi: 10.1097/01.sla.0000171032.99149.fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Y, Luo Q, Li Y, Deng S, Wei S, Li X. Radiofrequency ablation versus hepatic resection for small hepatocellular carcinomas: a meta-analysis of randomized and nonrandomized controlled trials. PLoS One. 2014;9:e84484. doi: 10.1371/journal.pone.0084484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Muaddi H, Al-Adra DP, Beecroft R, et al. Liver transplantation is equally effective as a salvage therapy for patients with hepatocellular carcinoma recurrence following radiofrequency ablation or liver resection with curative intent. Ann Surg Oncol. 2018;25:991–9. doi: 10.1245/s10434-017-6329-x. [DOI] [PubMed] [Google Scholar]
- 63.Cárdenes HR, Price TR, Perkins SM, et al. Phase i feasibility trial of stereotactic body radiation therapy for primary hepatocellular carcinoma. Clin Transl Oncol. 2010;12:218–25. doi: 10.1007/s12094-010-0492-x. [DOI] [PubMed] [Google Scholar]
- 64.Bujold A, Massey CA, Kim JJ, et al. Sequential phase i and ii trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J Clin Oncol. 2013;31:1631–9. doi: 10.1200/JCO.2012.44.1659. [DOI] [PubMed] [Google Scholar]
- 65.Lasley FD, Mannina EM, Johnson CS, et al. Treatment variables related to liver toxicity in patients with hepatocellular carcinoma, Child-Pugh class A and B enrolled in a phase 1–2 trial of stereotactic body radiation therapy. Pract Radiat Oncol. 2015;5:e443–9. doi: 10.1016/j.prro.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 66.Culleton S, Jiang H, Haddad CR, et al. Outcomes following definitive stereotactic body radiotherapy for patients with Child-Pugh B or C hepatocellular carcinoma. Radiother Oncol. 2014;111:412–17. doi: 10.1016/j.radonc.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 67.Sapisochin G, Barry A, Doherty M, et al. Stereotactic body radiotherapy vs. tace or rfa as a bridge to transplant in patients with hepatocellular carcinoma. An intention-to-treat analysis. J Hepatol. 2017;67:92–9. doi: 10.1016/j.jhep.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 68.Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–71. doi: 10.1053/jhep.2002.33156. [DOI] [PubMed] [Google Scholar]
- 69.Chua TC, Liauw W, Saxena A, et al. Systematic review of neoadjuvant transarterial chemoembolization for resectable hepatocellular carcinoma. Liver Int. 2010;30:166–74. doi: 10.1111/j.1478-3231.2009.02166.x. [DOI] [PubMed] [Google Scholar]
- 70.Tang YL, Qi XS, Guo XZ. Hepatic resection after initial transarterial chemoembolization versus transarterial chemoembolization alone for the treatment of hepatocellular carcinoma: a meta-analysis of observational studies. Asian Pac J Cancer Prev. 2015;16:7871–4. doi: 10.7314/APJCP.2015.16.17.7871. [DOI] [PubMed] [Google Scholar]
- 71.Kudo M. Lenvatinib may drastically change the treatment landscape of hepatocellular carcinoma. Liver Cancer. 2018;7:1–19. doi: 10.1159/000487148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kudo M, Finn RS, Qin S, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–73. doi: 10.1016/S0140-6736(18)30207-1. [DOI] [PubMed] [Google Scholar]
- 73.Yarchoan M, Agarwal P, Villanueva A, et al. Recent developments and therapeutic strategies against hepatocellular carcinoma. Cancer Res. 2019;79:4326–30. doi: 10.1158/0008-5472.CAN-19-0803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dasari BV, Kamarajah SK, Hodson J, et al. Development and validation of a risk score to predict the overall survival following surgical resection of hepatocellular carcinoma in non-cirrhotic liver. HPB (Oxford) 2020;22:383–90. doi: 10.1016/j.hpb.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 75.Fong Y, Jarnagin W, Blumgart LH. Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg. 2000;232:557–69. doi: 10.1097/00000658-200010000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Søreide K, Guest RV, Harrison EM, Kendall TJ, Garden OJ, Wigmore SJ. Systematic review of management of incidental gallbladder cancer after cholecystectomy. Br J Surg. 2019;106:32–45. doi: 10.1002/bjs.11035. [DOI] [PubMed] [Google Scholar]
- 77.Benson AB, D’Angelica MI, Abbott DE, et al. Guidelines insights: hepatobiliary cancers, version 2.2019. J Natl Compr Canc Netw. 2019;17:302–10. doi: 10.6004/jnccn.2019.0019. [DOI] [PubMed] [Google Scholar]
- 78.Taner CB, Nagorney DM, Donohue JH. Surgical treatment of gallbladder cancer. J Gastrointest Surg. 2004;8:83–9. doi: 10.1016/j.gassur.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 79.Wagholikar GD, Behari A, Krishnani N, et al. Early gallbladder cancer. J Am Coll Surg. 2002;194:137–41. doi: 10.1016/S1072-7515(01)01136-X. [DOI] [PubMed] [Google Scholar]
- 80.Lee SE, Kim KS, Kim WB, et al. on behalf of the Korean Association of Hepato-Biliary and Pancreas Surgery. Practical guidelines for the surgical treatment of gallbladder cancer. J Korean Med Sci. 2014;29:1333–40. doi: 10.3346/jkms.2014.29.10.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mizuno T, Ebata T, Yokoyama Y, et al. Major hepatectomy with or without pancreatoduodenectomy for advanced gallbladder cancer. Br J Surg. 2019;106:626–35. doi: 10.1002/bjs.11088. [DOI] [PubMed] [Google Scholar]
- 82.Yamamoto Y, Sugiura T, Ashida R, Okamura Y, Ito T, Uesaka K. Indications for major hepatectomy and combined procedures for advanced gallbladder cancer. Br J Surg. 2017;104:257–66. doi: 10.1002/bjs.10401. [DOI] [PubMed] [Google Scholar]
- 83.Lundgren L, Muszynska C, Ros A, et al. Management of incidental gallbladder cancer in a national cohort. Br J Surg. 2019;106:1216–27. doi: 10.1002/bjs.11205. [DOI] [PubMed] [Google Scholar]
- 84.Kishi Y, Nara S, Esaki M, Hiraoka N, Shimada K. Extent of lymph node dissection in patients with gallbladder cancer. Br J Surg. 2018;105:1658–64. doi: 10.1002/bjs.10913. [DOI] [PubMed] [Google Scholar]
- 85.Torén W, Ansari D, Søreide K, Andersson R. Re-resection for incidentally detected gallbladder cancer: weighing in on the options. Eur J Surg Oncol. 2020;46:495–7. doi: 10.1016/j.ejso.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 86.Søreide K, Harrison EM, Wigmore SJ. Research gaps and unanswered questions in gallbladder cancer. HPB (Oxford) 2018;20:685–6. doi: 10.1016/j.hpb.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 87.Primrose JN, Fox RP, Palmer DH, et al. Capecitabine compared with observation in resected biliary tract cancer (bilcap): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019;20:663–73. doi: 10.1016/S1470-2045(18)30915-X. [DOI] [PubMed] [Google Scholar]
- 88.Azizi AA, Lamarca A, Valle JW. Systemic therapy of gallbladder cancer: review of first line, maintenance, neoadjuvant and second line therapy specific to gallbladder cancer. Chin Clin Oncol. 2019;8:43. doi: 10.21037/cco.2019.07.05. [DOI] [PubMed] [Google Scholar]
- 89.Goetze TO, Bechstein WO, Bankstahl US, et al. Neoadjuvant chemotherapy with gemcitabine plus cisplatin followed by radical liver resection versus immediate radical liver resection alone with or without adjuvant chemotherapy in incidentally detected gallbladder carcinoma after simple cholecystectomy or in front of radical resection of btc (icc/ecc)—a phase iii study of the German registry of incidental gallbladder carcinoma platform (gr)—the aio/calgp/aco–gain–trial. BMC Cancer. 2020;20:122. doi: 10.1186/s12885-020-6610-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cherkassky L, Jarnagin W. Selecting treatment sequence for patients with incidental gallbladder cancer: a neoadjuvant approach versus upfront surgery. Updates Surg. 2019;71:217–25. doi: 10.1007/s13304-019-00670-z. [DOI] [PubMed] [Google Scholar]
- 91.Bai Y, Liu ZS, Xiong JP, et al. Nomogram to predict overall survival after gallbladder cancer resection in China. World J Gastroenterol. 2018;24:5167–78. doi: 10.3748/wjg.v24.i45.5167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen M, Cao J, Zhang B, Pan L, Cai X. A nomogram for prediction of overall survival in patients with node-negative gallbladder cancer. J Cancer. 2019;10:3246–52. doi: 10.7150/jca.30046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang W, Hong HJ, Chen YL. Establishment of a gallbladder cancer–specific survival model to predict prognosis in non-metastatic gallbladder cancer patients after surgical resection. Dig Dis Sci. 2018;63:2251–8. doi: 10.1007/s10620-018-5103-7. [DOI] [PubMed] [Google Scholar]
- 94.Yadav S, Tella SH, Kommalapati A, et al. A novel clinically based staging system for gallbladder cancer. J Natl Compr Canc Netw. 2020;18:151–9. doi: 10.6004/jnccn.2019.7357. [DOI] [PubMed] [Google Scholar]
- 95.Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surg. 2014;149:565–74. doi: 10.1001/jamasurg.2013.5137. [DOI] [PubMed] [Google Scholar]
- 96.Le Roy B, Gelli M, Pittau G, et al. Neoadjuvant chemotherapy for initially unresectable intrahepatic cholangiocarcinoma. Br J Surg. 2018;105:839–47. doi: 10.1002/bjs.10641. [DOI] [PubMed] [Google Scholar]
- 97.Han K, Ko HK, Kim KW, Won HJ, Shin YM, Kim PN. Radiofrequency ablation in the treatment of unresectable intrahepatic cholangiocarcinoma: systematic review and meta-analysis. J Vasc Intervent Radiol. 2015;26:943–8. doi: 10.1016/j.jvir.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 98.Gkika E, Hallauer L, Kirste S, et al. Stereotactic body radiotherapy (sbrt) for locally advanced intrahepatic and extrahepatic cholangiocarcinoma. BMC Cancer. 2017;17:781. doi: 10.1186/s12885-017-3788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kuhlmann JB, Euringer W, Spangenberg HC, et al. Treatment of unresectable cholangiocarcinoma. Eur J Gastroenterol Hepatol. 2012;24:437–43. doi: 10.1097/MEG.0b013e3283502241. [DOI] [PubMed] [Google Scholar]
- 100.Al-Adra DP, Gill RS, Axford SJ, Shi X, Kneteman N, Liau SS. Treatment of unresectable intrahepatic cholangiocarcinoma with yttrium-90 radioembolization: a systematic review and pooled analysis. Eur J Surg Oncol. 2015;41:120–7. doi: 10.1016/j.ejso.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Buettner S, Galjart B, van Vugt JLA, et al. Performance of prognostic scores and staging systems in predicting long-term survival outcomes after surgery for intrahepatic cholangiocarcinoma. J Surg Oncol. 2017;116:1085–95. doi: 10.1002/jso.24759. [DOI] [PubMed] [Google Scholar]
- 102.Sakamoto Y, Kokudo N, Matsuyama Y, et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: analysis of surgical patients from a nationwide survey of the Liver Cancer Study Group of Japan. Cancer. 2016;122:61–70. doi: 10.1002/cncr.29686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hyder O, Marques H, Pulitano C, et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an Eastern and Western experience. JAMA Surg. 2014;149:432–8. doi: 10.1001/jamasurg.2013.5168. [DOI] [PubMed] [Google Scholar]
- 104.Wang Y, Li J, Xia Y, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013;31:1188–95. doi: 10.1200/JCO.2012.41.5984. [DOI] [PubMed] [Google Scholar]
- 105.Tsilimigras DI, Mehta R, Aldrighetti L, et al. on behalf of the International Intrahepatic Cholangiocarcinoma Study Group. Development and validation of a laboratory risk score (LabScore) to predict outcomes after resection for intrahepatic cholangiocarcinoma. J Am Coll Surg. 2020;230:381–91. doi: 10.1016/j.jamcollsurg.2019.12.025. [DOI] [PubMed] [Google Scholar]
- 106.Clark CJ, Wood-Wentz CM, Reid-Lombardo KM, Kendrick ML, Huebner M, Que FG. Lymphadenectomy in the staging and treatment of intrahepatic cholangiocarcinoma: a population-based study using the National Cancer Institute seer database. HPB (Oxford) 2011;13:612–20. doi: 10.1111/j.1477-2574.2011.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ebata T, Nagino M. Perihilar cholangiocarcinoma with emphasis on presurgical management. In: Jarnagin WM, editor. Blumgart’s Surgery of the Liver, Biliary Tract, and Pancreas. 6th ed. Toronto, ON: Elsevier; 2017. pp. 833–85. [Google Scholar]
- 108.Sumiyoshi T, Shima Y, Okabayashi T, et al. Chemoradiotherapy for initially unresectable locally advanced cholangiocarcinoma. World J Surg. 2018;42:2910–18. doi: 10.1007/s00268-018-4558-1. [DOI] [PubMed] [Google Scholar]
- 109.McMasters KM, Tuttle TM, Leach SD, et al. Neoadjuvant chemoradiation for extrahepatic cholangiocarcinoma. Am J Surg. 1997;174:605–8. doi: 10.1016/S0002-9610(97)00203-1. [DOI] [PubMed] [Google Scholar]
- 110.Nelson JW, Ghafoori AP, Willett CG, et al. Concurrent chemoradiotherapy in resected extrahepatic cholangiocarcinoma. Int J Radiat Oncol Biol Phys. 2009;73:148–53. doi: 10.1016/j.ijrobp.2008.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cambridge WA, Fairfield C, Powell JJ, et al. Meta-analysis and meta-regression of survival after liver transplantation for unresectable perihilar cholangiocarcinoma. Ann Surg. 2020 doi: 10.1097/SLA.0000000000003801. [online ahead of print] [DOI] [PubMed] [Google Scholar]