Abstract
Reexpansion pulmonary edema is a rare complication of thoracocentesis with mortality rates as high as 20%. It presents with tachycardia, hypotension, and hypoxemia within hours after thoracocentesis. The exact pathophysiology is not known. The risk factors for the same should be carefully assessed and considered before chest tube drainage. The treatment is supportive. A case of ipsilateral reexpansion pulmonary edema after chest tube drainage of spontaneous pneumothorax is described and illustrated. He was managed with noninvasive ventilation, inotropes, and other supportive treatment and recovered completely.
Keywords: Reexpansion pulmonary edema, Intercostal drainage tube, Pneumothorax, Thoracocentesis, Lung collapse
Introduction
Many noncardiac causes of pulmonary edema have been described. One of the rare noncardiac causes of pulmonary edema is lung reexpansion subsequent to collapse due to pneumothorax or pleural effusion. The first clinical picture of this condition was described by Pinault in 1853, and the first published case of reexpansion pulmonary edema (REPE) was by Carlson et al1 (1958) in a patient who had pneumothorax and a totally collapsed lung. Risk factors known to be associated with REPE include younger age (<40 years), lung collapse of longer duration (>4 days), one-lung ventilation in thoracoscopic/minimally invasive cardiac surgery, large pneumothorax/pleural effusion (>30% of lung volume), and rapid reexpansion.2, 3
Here, we present a case of REPE after intercostal drainage tube (ICD) insertion in a case of spontaneous pneumothorax.
Case report
A 70-year-old patient, a chronic smoker (30 pack years) and a known case of chronic obstructive pulmonary disease, presented with difficulty in breathing of 1 week duration. Clinical examination revealed pulse rate of 106/min, blood pressure (BP) of 110/78 mmHg, respiratory rate of 24/min, and spO2 of 90% in room air. There was tracheal deviation to left. Chest examination revealed absent breath sounds in all regions of the right hemithorax and hyperresonant note on percussion. Laboratory investigations were normal except leukocytosis (total leukocyte count (TLC) – 15500/cmm). Chest radiograph showed the presence of right-sided pneumothorax, collapse of lung, and tracheal shift to left (Fig. 1).
Fig. 1.
Chest radiograph showing right-sided pneumothorax.
Right-sided ICD was inserted and connected to the underwater seal with no suction attached. ICD insertion was followed by a gush of air, and the patient showed a sigh of relief. The chest radiograph showed reexpansion of the collapsed lung (Fig. 2). The patient was continued on high-flow oxygen. Two hours later, the patient developed severe chest discomfort, cough, and shortness of breath. Clinically he had tachycardia (pulse rate, 110/min) and hypotension (BP, 64/46 mmHg), and saturation of oxygen fell down to 68%. Chest examination revealed coarse crackles all over the right side of the chest. In view of hypotension, urgent electrocardiogram (ECG) was performed which showed no dynamic changes, and evaluation of cardiac enzymes was carried out which were normal. Diagnosis of acute pulmonary thromboembolism was ruled out with appropriate investigations. An urgent bedside portable chest radiograph in the anteroposterior view was performed which showed right-sided pulmonary congestion and opacification of the right hemithorax with ICD in situ (Fig. 3). Based on his clinical and radiological picture, the diagnosis of REPE was made. He was managed with intravenous fluids, inotropic support, and noninvasive ventilation (NIV) support.
Fig. 2.
Chest radiograph showing resolution of pneumothorax after ICD insertion, ICD in situ. ICD, intercostal drainage tube.
Fig. 3.
Chest radiograph showing nonhomogenous opacification of the right hemithorax, suggestive of REPE, ICD in situ. ICD, intercostal drainage tube; REPE, reexpansion pulmonary edema.
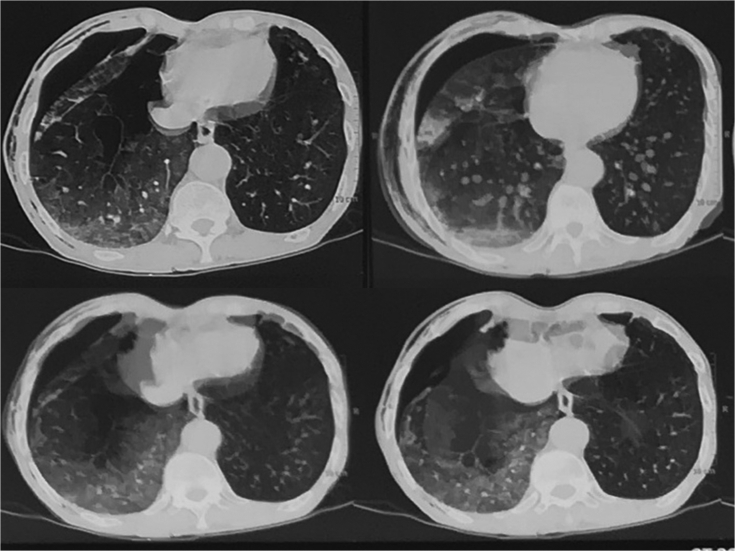
High-resolution computed tomography (HRCT) chest was performed on the next day which revealed resolving right-sided pneumothorax and pulmonary edema (Fig. 4). He was continued with conservative treatment on similar lines for 24 h. His condition improved over 2 days, and his repeat chest radiograph showed expansion of the right lung and resolution of pulmonary edema. NIV and inotropic support was continued for 48 h, along with high-flow oxygen therapy. Air leak from the ICD ceased after 6 days. The ICD was removed, and he was discharged after 1 day of observation with advice of cessation of smoking and continuation of bronchodilators. His follow-up at 1 month and 6 months showed better respiratory reserve and no recurrence of pneumothorax.
Fig. 4.
HRCT chest after 24 h of ICD insertion showing resolving pulmonary edema and pneumothorax. HRCT, high-resolution computed tomography; ICD, intercostal drainage tube.
Discussion
Reexpansion pulmonary edema (REPE) is a rare but potentially life-threatening complication resulting from rapid reexpansion of the collapsed lung after drainage of pleural effusion, pneumothorax, or atelectasis with a mortality rate of around 20%.4
The pathophysiology of REPE is not clearly understood. Possible mechanisms include increased pulmonary capillary permeability due to ventilation and reperfusion of the previously collapsed lung, causing inflammatory response and production of oxygen-derived free radicals. Other mechanisms postulated include increased hydrostatic pressure after increased venous return to the lungs, mechanical disruption of capillaries in the alveoli, and altered clearance of lymphatics.5, 6, 7
Symptoms of REPE include persistent cough (generally > 20 min) which may be associated with pinkish sputum, tachypnea, tachycardia, decrease in oxygen saturation, and hemodynamic instability, a condition akin to pulmonary edema. On radiography, the lung which was previously collapsed shows opacities in the hemithorax. This clinical situation progresses rapidly after ICD insertion and then improves rapidly after supportive treatment. CT chest usually shows ground glass pattern which is seen more in peripheral and basal areas. Thickening of the interlobular septum without pleural effusion may be associated with REPE.8
Onset of persistent cough during thoracocentesis in pleural effusion may be an early indicator of development of REPE, which may suggest termination of procedure. In patients with massive pleural effusion, the amount of aspirated fluid should be less than 1.5 L in one setting. Negative pressures more than 10–20 cm of water should not be used for suction while evacuating a massive pleural effusion or pneumothorax in absence of pleural manometry.5, 9
This condition is usually self-limiting, and treatment is supportive including oxygenation, administration of intravenous fluids, and inotropic support. Nursing the patient in lateral decubitus position on the affected side may decrease the intrapulmonary shunting, thus improving oxygenation in patients with REPE. NIV should be considered in managing these cases. In patients requiring intubation and mechanical ventilation, positive end-expiratory pressure (PEEP) improves the clinical condition within 24–48 h. All patients who recover usually do so within a week with complete resolution of clinical and radiological abnormalities.8, 10
Conclusion
Reexpansion pulmonary edema (REPE) is a relatively unknown but potentially life-threatening complication of thoracocentesis. It is pertinent that professionals involved in these procedures are aware of possible occurrence of REPE after emptying of the pleural cavity. It is important to take necessary care to avoid this condition because of its association with high mortality. Aggressive and early therapeutic measures should be taken if there is a clinical or radiological suspicion of REPE.
Conflicts of interest
The authors have none to declare.
References
- 1.Carlson R.I., Classen K.L., Gollan F., Gobbel W.G., Jr., Sherman D.E., Christensen R.O. Pulmonary edema following the rapid expansion of a totally collapsed lung due to pneumothorax: a clinical and experimental study. Surg Forum. 1958;9:367–371. [PubMed] [Google Scholar]
- 2.Conen A., Joos L., Bingisser R. Ipsilateral reexpansion pulmonary edema after drainage of a spontaneous pneumothorax: a case report. J Med Case Rep. 2007;1:107. doi: 10.1186/1752-1947-1-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baden L.R. Reexpansion pulmonary edema after thoracentesis. N Engl J Med. 2014;370:12. doi: 10.1056/NEJMicm1309844. [DOI] [PubMed] [Google Scholar]
- 4.Mahfood S., Hix W.R., Aaron B.L., Blaes P., Watson D.C. Reexpansion pulmonary edema. Ann Thorac Surg. 1988;45:340–345. doi: 10.1016/s0003-4975(10)62480-0. [DOI] [PubMed] [Google Scholar]
- 5.Kashmani R., Irani F., Okoli K., Mahajan V. Re-expansion pulmonary edema following thoracentesis. CMAJ (Can Med Assoc J) 2010;182:2000–2002. doi: 10.1503/cmaj.090672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sohara Y. Reexpansion pulmonary edema. Ann Thorac Cardiovasc Surg. 2008;14:205–209. [PubMed] [Google Scholar]
- 7.Genofre E.H., Vargas F.S., Teixeira L.R., Vaz M.A.C., Marchi E. Reexpansion pulmonary edema. J Pneumol. 2003;29:101–106. [Google Scholar]
- 8.Dias O.M., Teixeira L.R., Vargas F.S. Reexpansion pulmonary edema after therapeutic thoracentesis. Clinics. 2010;65:1387–1389. doi: 10.1590/S1807-59322010001200026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mahajan V.K., Simon M., Huber G.L. Reexpansion pulmonary edema. Chest. 1979;75:192–194. doi: 10.1378/chest.75.2.192. [DOI] [PubMed] [Google Scholar]
- 10.Verhagen M., van Buijtenen J.M.V., Geeraedts L.M.G. Reexpansion pulmonary edema after chest drainage for pneumothorax: a case report and literature overview. Respiratory Medicine Case Reports. 2015;14:10–12. doi: 10.1016/j.rmcr.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]