Abstract
Primary pulmonary Hodgkins lymphoma is a rare and enigmatic neoplasm commonly seen in females. The aim of this case report is to emphasize that pulmonary lymphoma should be considered as a differential diagnosis in a young patient presenting with a lung mass and B symptoms. Extensive clinical details, imaging should be done to rule out the secondary involvement of lung by other lymphomas.
Keywords: Classical Hodgkin lymphoma, Primary pulmonary lymphoma, Immunohistochemistry, Histoplasmosis, Lung
Introduction
It was only in 1832 that the disease, now called Hodgkin's lymphoma, was first described by Sir Thomas Hodgkin.1 The hallmark cells of this disease can be identified as either mononucleated Hodgkin cells or Reed–Sternberg cells.2. This is a lymphoid malignancy that largely involves lymphoid organs. Extranodal involvement can be in the form of contiguous spread or by hematogenous dissemination. Pulmonary involvement as an extranodal site is seen in 6%–11% of cases with bilateral lung involvement seen in nearly 4.3% of cases. Primary pulmonary Hodgkin's lymphoma (PPHL) is an extremely rare disease which predominantly affects the upper lobes of the lung and is more common in older women.3 Pulmonary involvement as a multisite involvement is seen in approximately 15%–40% of the patients with Hodgkin's disease.4 PPHL is diagnosed only if there is no extrapulmonary disease at the time of diagnosis or within three months of diagnosis. Fewer than 100 cases have been reported until now. The pulmonary involvement may be in the form of mass lesion, cavity, or nodules. Here, we report a case of PPHL in a young male patient with coexisting pulmonary histoplasmosis.
Case report
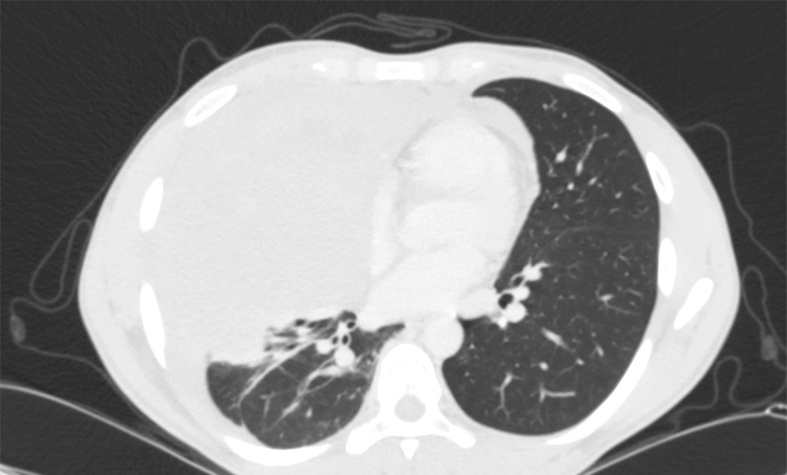
A 24-year-old male patient presented with a two-year history of pain in the right shoulder and breathlessness. The pain was insidious in onset, gradually worsening, sharp, localized laterally, and was moderately severe in intensity. The pain was often relieved by rest and painkillers. Breathlessness was exertional, insidious in onset, gradually progressive with no seasonal, postural, diurnal variation. It was not associated with a cough or pleuritic chest pain. Breathlessness used to be relieved by rest. There was history of weight loss with loss of appetite. There was no history of a cough or fever. General examination revealed pallor. There was no palpable lymphadenopathy. Chest examination revealed absent breath sounds in the right infraclavicular and infraaxillary area. Other systemic examination was within normal limits. Laboratory investigations showed Erythrocyte Sedimentation Rate (ESR) −76 mm fall in first hour, Hb − 10.7 g/dl, WBC count of 2100/mm3, and sputum for Acid Fast Bacilli (AFB) and blood culture were both negative. His other biochemical and hematological examinations were within normal limits. Radiograph of the shoulder and cervical spine were performed as an initial workup in which no abnormality was detected. A chest radiograph of posteroanterior view showed right upper lobe mass lesion (Fig. 1). 2D echocardiography was performed which showed dilated right ventricle (RV) (mild), RV dysfunction, and mild tricuspid regurgitation with moderate pulmonary hypertension. Contrast Enhanced Computed Tomography (CECT) chest showed a mass lesion measuring 14.7 × 14 × 18 cm in the right upper lobe (Fig. 2). The lesion appeared to be epicentered in the anterior and posterior segments of the right upper lobe. Areas of necrosis were also seen in the lesion. Positron Emission Tomography Computed Tomography (PET CT) was performed which revealed hypermetabolic right upper lobe lung mass with right pleural effusion. Bone marrow aspiration and biopsy were performed which revealed normal trilineage differentiation. Excision biopsy was planned. However, the surgery was abandoned as the tumor was encasing the superior vena cava. Biopsy taken at the time of surgery showed infiltration of the lung parenchyma by inflammatory cells comprising lymphocytes, plasma cells, and eosinophils. Interspersed among these cells were atypical cells which were large with multiple hyperchromatic nuclei and amphophilic cytoplasm (Fig. 3). An immunohistochemical panel comprising cytokeratin, leukocyte common antigen, CD20, CD15, CD30, PAX2, BOB1, EBV-LMP, napsin, thyroid transcription factor, and CD34 was put up. The neoplastic large cells showed positivity for CD15 and CD30. The rest of the IHC markers were negative. In addition to the abovementioned findings, epithelioid cells granulomas were also noted. The adjacent lung parenchyma showed large areas of necrosis, and alveoli were stuffed with foamy macrophages. Periodic Acid-Schiff (PAS) and Grocott-Gomori's Methenamine Silver (GMS) stain were performed which revealed 3–4 micron of budding yeast forms (Fig. 4). Based on the imaging and histopathological findings, diagnosis of PPHL with histoplasmosis was made. The patient was started on itraconazole and chemotherapeutic drugs with six cycles of kl which includes Adriamycin, bleomycin, vinblastine, and dacarbazine.
Fig. 1.
Chest radiograph showing a mass lesion in the right lung predominantly involving the right middle zone and silhouetting the right heart border with blunting of the right costophrenic angle.
Fig. 2.
Computerized tomography (CT) scan of the chest showing a right upper lobe mass lesion.
Fig. 3.
H&E stain with 100× magnification of lung biopsy showing large atypical lymphoid cells.
Fig. 4.
Gomori's Methenamine silver stain (600×) showing 3- to 4-micron budding yeast forms suggestive of histoplasma.
Discussion
The commonest malignancy seen in the lung is of epithelial origin, and lymphoma constitutes less than 1% of all lung malignancies. PPHL is extremely uncommon, accounting for 3.6% of extranodal lymphomas.3 The commonest variant of Hodgkin's lymphoma seen in the lung is nodular sclerosis variant comprising 70% of PPHL followed by mixed cellularity.4 As the lung can be secondarily involved by the lymphoma, thorough workup of the patient should be carried out. Kern et al.5 suggested the criteria for diagnosing PPHL. These include that the disease should present predominately in the lung at the time of diagnosis. There should not be involvement of lymph nodes by Hodgkin's lymphoma at the time of the diagnosis or within three months of the diagnosis. The cases with lymphadenopathy or other organ involvement and in patients in whom pulmonary lymphoma appears to be an extension of mediastinal lymphoma should not be diagnosed as PPHL. In our patient, the tumor was present predominately in the right lung. Our patient did not have any lymphadenopathy, hepatomegaly, or splenomegaly at the time of diagnosis. PPHL is seen predominately in elderly women. Male-to-female ratio is 1:1.4. According to the study conducted by Radin6, PPHL was more common in women and mean age of presentation was 42.5 years. A study conducted by Nakachi et al. showed that age of patients ranged from 17 to 60 years and there was no sex predilection. Hodgkin's lymphoma is not restricted to any specific age group.7 Our patient was a young 24-year-old male. PPHL commonly presents with a cough with dyspnea, fever, night sweats, and weight loss. Our patient also presented with breathlessness and weight loss. PPHL commonly involves the upper lobe and is rarely bilateral. Based on radiological findings, it is difficult to differentiate between PPHL from lung involvement by other lymphomas. However, radiologically, PPHL typically involves the superior portions of the lungs, whereas secondary involvement of the lung by Hodgkin's lymphoma shows multiple nodular lesions involving one or both lung fields. It is necessary to grade that the PPHL as treatment will vary with the stage of the disease. The Ann Arbor pulmonary lymphoma staging system is used to stage pulmonary lymphomas. Pulmonary lymphomas are characterized by four stages depending on the involvement of the lung only, hilar lymph node, and mediastinal or whether lymph nodes below the diaphragm are involved or not.
The four stages of pulmonary lymphomas are given as follows: stage IE: lung only, could be bilateral, stage II 1E: lung and hilar lymph nodes; stage II 2E: lung and mediastinal lymph nodes, stage II 2 EW: lung and chest wall or diaphragm; stage III: lung and lymph nodes below the diaphragm; stage IV: diffuse.8 Recent modalities for treatment include combination chemotherapy. Few reports available in the literature suggested that if PPHL is diagnosed in early stages, it could be effectively treated with radiotherapy alone.9
PPHL with histoplasmosis is not reported in literature until now. One case report of Hodgkin's lymphoma with tuberculosis has been reported. in our patient; there was a huge lung mass which was causing bronchial cutoff leading to fungal infection in an immunocompetent individual. The incidence of primary pulmonary is very low, and a high index of suspicion is required to diagnose the disease.
Conclusion
PPHL is an uncommon neoplasm with limited studies documented in the literature. A high index of suspicion should be kept in mind whenever a young patient presents with a lung mass. A diligent search should be carried out to rule out the secondary involvement of the lung by other lymphomas.
Conflicts of interest
The authors have none to declare.
References
- 1.McElnay P.J., Pawade J., Chandratreya L., West D. Giant thoracic mass: an unusual presentation of primary pulmonary Hodgkin's lymphoma. BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-200909. bcr2013200909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lluch-Garcia R., Briones-Gomez A., Castellano E.M., Sanchez-Toril F., Lopez A., Brotons B. Primary pulmonary Hodgkin's lymphoma. Cancer Res J. 2010;17(6):106–108. doi: 10.1155/2010/252746. 2010 Nov-Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Homma M., Yamochi-Onizuka T., Shiozawa E. Primary pulmonary classical Hodgkin lymphoma with two recurrences in the mediastinum: a case report. J Clin Exp Hematop. 2010;50:151–157. doi: 10.3960/jslrt.50.151. [DOI] [PubMed] [Google Scholar]
- 4.Schild M.H., Wong W.W., Valdez R., Leis J.F. Primary pulmonary classical Hodgkin lymphoma:a case report. J Surg Oncol. 2014;110:341–344. doi: 10.1002/jso.23624. [DOI] [PubMed] [Google Scholar]
- 5.Kern W.H., Crepeau A.G., Jones J.C. Primary Hodgkin's disease of the lung. Report of four cases and review of the literature. Cancer. 1961;14:1151–1165. doi: 10.1002/1097-0142(196111/12)14:6<1151::aid-cncr2820140604>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 6.Radin A.I. Primary pulmonary Hodgkin's disease. Cancer. 1990;65:550–563. doi: 10.1002/1097-0142(19900201)65:3<550::aid-cncr2820650328>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 7.Nakachi S., Nagasaki A., Owan I. Primary pulmonary Hodgkin lymphoma -two case reports and a review of the literature. Jpn J Canc Chemother. 2003;34:2279–2282. [PubMed] [Google Scholar]
- 8.Cartier Y., Johkoh T., Honda O., Muller N.L. Primary pulmonary Hodgkin's disease : CT findings in three patients. Clin Radiol. 1999;54:182–184. doi: 10.1016/s0009-9260(99)91012-7. [DOI] [PubMed] [Google Scholar]
- 9.Parissis H. Forty years literature review of primary lung lymphoma. J Cardiothorac Surg. 2011;6:23. doi: 10.1186/1749-8090-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]