Abstract
目的
通过分析比较非糜烂性反流病(NERD)、反流高敏感(RH)和功能性烧心(FH)患者的食管24 h pH-阻抗监测反流模式, 探讨内镜阴性烧心患者症状可能的发生机制。
方法
选取我院消化科门诊和胃肠功能室的以烧心为主要症状的患者, 通过胃镜、24 h pH-阻抗监测, 最终纳入79例患者, 包括NERD 35例, RH 16例和FH 28例, 进行pH-阻抗数据分析。
结果
NERD组较RH组、FH组酸反流次数显著性增加、弱碱反流次数显著性减少, 差异有统计学意义(P均 < 0.05);NERD组、RH组合计反流次数、混合反流次数、近端酸反流次数及百分比、近端弱酸反流次数及百分比、近端合计反流次数及百分比较FH组显著性增加, 差异有统计学意义(P均 < 0.05);分析反流的酸度, NERD、RH和FH三组中各种反流所占的比例之间差异有统计学意义(P < 0.05), 在NERD组以酸反流为主, 但在RH和FH组, 则以弱酸反流为主, 且弱碱反流也较NERD组显著性增加。
结论
NERD患者与RH患者、FH患者反流模式不同, 前者以酸反流为主, 后两者弱碱反流明显增多; 对于pH-阻抗监测期间无症状或未记录症状的食管酸暴露正常患者, 合计反流次数、混合反流次数、近端反流次数及百分比等阻抗监测指标将有助于鉴别RH和FH。
Keywords: 24 h pH-阻抗监测, 非糜烂性胃食管反流病, 反流高敏感, 功能性烧心
Abstract
Objective
To analyze the differences in reflux patterns in 24-hour esophageal pH-impedance monitoring in patients with non-erosive reflux disease (NERD), reflux hypersensitivity (RH) and functional heartburn (FH) and explore the possible mechanism of symptoms in patients with heartburn and negative endoscopic findings.
Methods
Seventy-nine patients with heartburn as the main symptoms but negative endoscopic findings, including 35 with NERD, 16 with RH and 28 with FH, were enrolled in this study.All the patients underwent 24-h esophageal pH-impedance monitoring and esophagogastroscopy, and the results were compared among the 3 groups.
Results
Acid reflux episode was significantly increased and weakly alkaline reflux episode was significantly decreased in NERD group in comparison with RH group and FH group (P < 0.05).The patients in NERD group showed significantly increased total reflux episode, mixed reflux episode, proximal acid reflux episode, proximal weak acid reflux episode, total proximal reflux episode, percentage of proximal acid reflux, percentage of proximal weak acid reflux, and percentage of total proximal reflux as compared with the other two groups (all P < 0.05).Bolus clear time was significantly prolonged in NERD group compared with that in the other two groups (P < 0.05).Analysis of the reflux acidity showed that the percentages of different reflux episodes differed significantly among the 3 groups (P < 0.05);acid reflux was the main reflux in NERD, while weak acid reflux was the main reflux in RH and FH groups, which had also significantly increased weakly alkaline reflux episodes compared with NERD group.
Conclusions
Patients with NERD, RH and FH had different reflux patterns.Acid reflux is predominant in the NERD, while weakly alkaline reflux is significantly increased RH and FH.In patients with normal esophageal acid exposure but without symptoms or without recorded symptoms during esophageal pH-impedance monitoring, analysis of the total reflux episode, mixed reflux episode, proximal acid reflux episode and percentage can help in the differential diagnosis between RH and FH.
Keywords: 24-hour pH-impedance monitoring, non-erosive esophagus reflux disease, reflux hypersensitivity, functional heartburn
烧心是消化科就诊患者的常见症状,这一症状多发生于北美和欧洲人群,在亚洲人群中相对较少[1-2]。针对我国五个地区的人口调查显示,胃食管反流病(GERD)症状的患病率为3.1% [3]。但近年来在亚洲国家包括我国的烧心症状发病率有逐年升高的趋势[3-6]。一般认为典型的烧心是GERD的特有症状,当然大多数烧心患者(尤其是初治患者)的症状是与GERD有关的,通过抑酸剂治疗多能缓解症状,但仍有部分患者对抑酸治疗完全或部分无效[7-9]。随着食管反流监测的应用,研究者发现烧心谱并非是单一的一种疾病所特有,而是一组具有异质性的不同疾病群体的症状[10-12]。罗马Ⅱ首次建议将内镜阴性烧心患者细分为非糜烂性反流病(NERD)和功能性烧心(FH)两种,而且认为FH是质子泵抑制剂(PPI)治疗失败的主要原因[13-14]。随着对此类疾病认识的深入,罗马标准也进行了相应的更新,现最新的罗马Ⅳ标准[15]将内镜阴性烧心患者分为NERD(异常酸暴露)、反流高敏感(RH,酸暴露正常但症状与反流有关)和FH(酸暴露正常且症状与反流无关)。
在内镜阴性烧心患者的病理生理学中,NERD即病理性酸反流的作用已被公认,但在RH、FH,烧心症状是如何产生的,其病理生理机制目前尚不清楚,尤其是RH,既往作为NERD疾病的一部分,现根据最新的罗马Ⅳ标准已作为单独的一种功能性食管疾病分离出来[16],但这种详细的划分具体的临床意义有多大或者说病理生理学实质上是否为不同的疾病还尚无定论。食管pH-阻抗监测被认为是记录反流事件的金标准[17]。本研究将根据罗马Ⅳ标准[15]分的NERD、RH、FH的pH-阻抗数据进行分析,以探讨内镜阴性烧心患者可能的反流模式、病理生理学机制以及食管pH-阻抗监测对三者的诊断和鉴别诊断价值。
1. 资料和方法
1.1. 研究对象
连续选取2017年3月~2019年2月就诊于西安交通大学第二附属医院消化科的具有典型烧心症状的患者。纳入标准:①18~75岁;②烧心症状持续6个月以上,并已引发患者不适感受(轻度症状≥2 d/周,中重度≥1 d/周);③胃镜示食管黏膜无破损;④行24 h食管pH-阻抗监测前停用PPI至少1周,停用促动力药至少3 d;⑤pH-阻抗监测期间示酸暴露正常者必须要有且记录烧心等反流症状;⑥受试者自愿进入临床试验,并签署知情同意书。排除标准:①消化道器质性疾病及腹部手术史;②合并主要的食管动力障碍;③患有严重的心、肺、脑、肾等疾病;④妊娠或哺乳期的妇女;⑤因各种原因不能接受胃镜、24 h pH-阻抗监测者。本研究通过医院伦理委员会审核批准。
1.2. 胃镜检查
通过胃镜、pH-阻抗监测检查,并根据纳入和排除标准,最终纳入79例患者,其中男35例,女44例;年龄27~71岁。采用OLYMPUS GIF-H260电子胃镜系统检查,重点观察食管有无破损、Barrett食管等。
1.3. 24 h pH-阻抗监测
设备采用荷兰MMS公司生产的Ohmega动态pH-阻抗联合监测系统,阻抗导管上有8个金属电极环,每两个相邻的阻抗电极环代表 1个阻抗测量通道,间隔为2 cm,阻抗通道设定为zl、z2、z3、z4、z5和z6通道,相应距离导管末端是17、15、9、7、5和3cm处。以50 Hz的采样频率记录6个阻抗通道信号。其监测系统还有1个pH电极,大约距导管末端5 cm处。监测的数据保存于便携式记录仪的存储卡内。
操作方法操作过程在本科胃肠功能室完成。所有受试者检查前停服PPI、吗丁啉等影响胃酸分泌或上消化道动力的药物至少1周;检查当日空腹(禁食>8 h,禁水>4 h);检查前要先将pH电极导管用pH 4.0和7.0的缓冲液校准后才进行下一步操作,患者取坐位,采用pH阶梯法来定位导管相应位置:将pH-阻抗导管经鼻腔插入食管,进而插入胃内后,然后缓慢回拉导管,当pH从 < 4突然升到>5时我们判断为LES下缘,然后量其到门齿的距离,重复数遍,将pH电极导管放置在LES上5 cm处,6个阻抗电极导管分别放置在LES以上3、5、7、9、15及17 cm处,在鼻翼两侧固定好导管后,记录仪开始记录24 h pH-阻抗变化的情况,嘱患者监测期间记录进食、烧心等反流症状的日记。为了监测结果能比较真实的反映原有的情况,检查者应保持平时的作息和饮食习惯,避免食用咖啡、浓茶以及酸性食物等。然后患者带管回家,24 h后返院拔出监测导管,并将记录仪的数据导入计算机系统,通过专用软件进行分析。
监测指标包括:①酸暴露评估:以酸暴露时间AET作为是否存在异常酸暴露的指标,AET指LES上5 cm处pH电极测得的pH < 4的时间占总监测时间的百分比,当AET>4.2%时认为存在异常酸暴露;②症状相关性分析:结合监测期间出现的烧心等反流症状可分为与反流相关(包括酸和非酸反流)和与反流无关两种。采用症状相关指数(SI)和症状相关概率(SAP)进行评估。当SI≥50%和(或)SAP>95%可视为阳性;③反流物类型:根据反流物的pH值,分为酸反流、弱酸反流和弱碱反流。根据反流物的阻抗值,分为液体反流、气体反流和混合反流;④食团清除时间;⑤近端反流,即反流至LES上15 cm以上阻抗通道的反流。
使用罗马Ⅳ标准[15]将内镜阴性烧心患者根据是否存在异常酸暴露以及症状是否与反流相关分为NERD(异常酸暴露)、RH(酸暴露正常但症状与反流有关)和FH(酸暴露正常且症状与反流无关)3组。
1.4. 统计学分析
采用SPSS 23.0软件完成。正态分布资料采用Mean±SD表示,组间比较使用方差分析;非正态分布数据采用M(P25,P75)表示,组间比较使用非参数检验(Kruskal-Wallis及Mann-Whitney检验);率的比较采用卡方检验。P < 0.05认为差异有统计学意义。
2. 结果
2.1. 3组基本特征比较
NERD、RH、FH 3组患者在基本特征的比较可见表 1,年龄、性别比差异无统计学意义(P均>0.05),但NERD组的BMI显著高于FH组,差异有统计学意义(F=4.808,P=0.011)。
1.
各组患者基本特征比较
Comparison of gender distribution, age and BMI among the 3 groups
| Item | NERD | RH | FH | χ2/F | P |
| Number[n (%)] | 35 (44.3%) | 16 (20.25%) | 28 (35.45%) | ||
| Male/female | 19/16 | 8/8 | 8/20 | 4.432 | 0.109 |
| Age (year) | 53.43±9.59 | 47.47±12.51 | 49.39±9.50 | 2.221 | 0.105 |
| BMI (kg/m2) | 23.60±2.92 | 22.14±3.05 | 21.39±2.74 | 4.808 | 0.011* |
2.2. 症状与反流关系
在入选的79例患者中,有67例(84.81%)患者在监测过程中出现症状,但仅有24例(30.37%)患者SI和(或) SAP呈阳性。24例中有7例(8.86%)仅SI阳性,6例(7.59%)仅SAP阳性,11例(13.92%)为SI和SAP均阳性。
在24例患者SI和(或)SAP呈阳性的患者中,8例(33.33%)SI和(或)SAP阳性的NERD患者症状均与酸反流相关,在16例RH患者中,7例(29.17%)患者症状与酸反流相关,6例(25.00%)患者症状与弱酸反流相关,3例(12.50%)患者症状与弱碱反流相关(图 1)。
1.
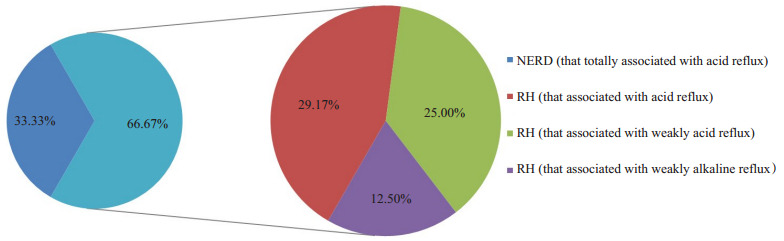
SI和(或)SAP阳性患者中与症状有关的各种反流的占比
Proportions of SI and/or SAP-positive patients with symptomatic reflux.
2.3. 各反流模式次数比较
从表 2可以看出,酸反流次数、弱碱反流次数、合计反流次数和混合反流次数在3组之间差异均有统计学意义(χ2=25.292、7.692、8.031、6.246,P均 < 0.05)。同样,对存在显著性差异的指标进行两两比较结果提示,NERD组酸反流次数较RH组、FH组显著性增加,差异有统计学意义(P均 < 0.05),RH组较FH组酸反流次数增加,但差异无统计学意义(P>0.05);RH组、FH组较NERD组弱碱反流次数显著性增加,差异有统计学意义(P均 < 0.05),而RH组与FH组弱碱反流次数差异无统计学意义(P>0.05);合计反流次数方面,NERD组、RH组较FH组显著性增加,差异有统计学意义(P均 < 0.05)。
2.
各组患者不同反流模式的反流次数比较
Comparison of the number of reflux episodes with different reflux patterns among the 3groups [median (P25, P75)]
| Number of different reflux episodes | NERD | RH | FH | χ2 | P |
| Acid reflux episodes | 23 (14, 37) | 12 (6, 17) | 4 (0, 14) | 25.292 | 0.000* |
| Weakly acid reflux episodes | 18 (11, 33) | 20 (12, 38) | 17 (6, 26) | 2.833 | 0.243 |
| Weakly alkaline reflux episodes | 1 (0, 3) | 5 (0, 14) | 4 (0, 8) | 7.692 | 0.021* |
| Total reflux episodes | 43 (30, 63) | 45 (30, 71) | 27 (15, 47) | 8.031 | 0.018* |
| Liquid reflux episodes | 14 (3, 26) | 11 (6, 22) | 9 (3, 12) | 4.928 | 0.085 |
| Mixed reflux episodes | 34 (24, 42) | 34 (19, 60) | 18 (8, 36) | 6.246 | 0.044* |
| Gas reflux episodes | 28 (16, 61) | 24 (20, 41) | 33 (20, 59) | 0.679 | 0.712 |
NERD组、RH组较FH组混合反流次数显著性增加,差异有统计学意义(P均 < 0.05),而NERD组与RH组差异无统计学意义(P>0.05)。
2.4. 各反流模式比例比较
根据反流物的酸度,NERD组酸反流、弱酸反流和弱碱反流所占的比例分别为52.01%、44.52%、3.47%,RH组3种反流所占的比例分别为24.81%、59.02%、16.17%,FH组3种反流所占的比例分别为25.11%、54.67%、20.22%。卡方检验提示3组中各种反流的比例之间差异有统计学意义(χ2=28.410,P=0.000)。在NERD组以酸反流为主要反流,但在RH和FH组,则以弱酸反流为主,且弱碱反流也较NERD组显著性增加。
2.5. 近端反流模式和食团清除时间比较
在反映近端反流的各指标中,近端酸反流次数及百分比,近端弱酸反流次数及百分比,近端合计反流次数及百分比在3组之间差异有统计学意义(χ2=29.461、26.087、11.734、10.666、22.532、20.455,P均 < 0.05,表 3)。然后两两组间比较显示,NERD组、RH组上述指标均较FH组显著性增加,差异有统计学意义(P均 < 0.05),而NERD组与RH组上述各指标均差异无统计学意义(P均>0.05)。NERD组食团清除时间较RH组、FH组延长,但只有NERD组与FH组比较差异有统计学意义(P < 0.05)。
3.
各组近端反流情况和食团清除时间的比较
Comparison of proximal regurgitation and bolus clearance time among the 3 groups [median (P25, P75)]
| Number or percentage of proximal reflux and bolus clearan | NERD | RH | FH | χ2 | P |
| Acid reflux episodes | 6 (4, 18) | 5 (1, 11) | 1 (0, 2) | 29.461 | 0.000* |
| Weakly acid reflux episodes | 4 (2, 9) | 5 (3, 12) | 2 (1, 4) | 11.734 | 0.003* |
| Weakly alkaline reflux episodes | 0 (0, 1) | 0 (0, 3) | 0 (0, 1) | 2.308 | 0.315 |
| Total reflux episodes | 15 (6, 31) | 13 (7, 34) | 4 (1, 7) | 22.532 | 0.000* |
| Acid reflux episodes (%) | 42 (24, 60) | 50 (33, 68) | 3 (0, 24) | 26.087 | 0.000* |
| Weakly acid reflux episodes (%) | 29 (17, 46) | 29 (18, 44) | 12 (5, 22) | 10.666 | 0.005* |
| Weakly alkaline reflux episodes (%) | 0 (0, 20) | 0 (0, 17) | 0 (0, 11) | 0.735 | 0.692 |
| Total reflux episodes (%) | 36 (22, 50) | 33 (25, 47) | 12 (7, 24) | 20.455 | 0.000* |
| Bolus clearance time (%) | 12 (10, 14) | 10 (9, 13) | 9 (8, 11) | 12.96 | 0.002* |
3. 讨论
到目前为止,内镜阴性烧心不同亚群的患者的流行病学仍然不清楚。以往的研究显示,大约50%的“NERD”患者有正常的酸暴露[18],FH和RH的比例可以从不足10%到75%不等[19-24]。最近有一项基于罗马Ⅳ的关于内镜阴性烧心患者的研究显示,约16.1%的患者为NERD,RH患者约为20.7%, FH患者占大多数,为63.2%[25],而我们的研究显示NERD患者为44.30%,RH为20.25%以及FH 35.45%,这种差异可能由于病例的选择性造成的。
首先我们比较了3组患者的基本特征,发现与RH、FH患者相比,NERD患者BMI明显升高,这一因素已被证明在促进酸反流方面发挥了重要作用[26-29]。
国内研究通过pH-阻抗监测发现,NERD、高敏感食管患者合计反流次数、酸反流次数、混合反流次数较FH患者明显增多,高敏感食管患者合计反流次数、弱酸反流次数、弱碱反流次数、混合反流次数较FH组明显增加[23-24]。与之前的研究基本相似,我们的研究结果发现,RH患者的合计反流次数、混合反流次数与NERD患者相似,均多于FH患者。但与NERD患者相比,RH、FH患者酸反流次数更少,弱碱反流次数更多;除此之外,我们通过比较3组中各种反流的比例,也发现在NERD组以酸反流为主要反流,但在RH和FH组中,则以弱酸反流为主,且弱碱反流也显著增加。弱碱反流指的是食管pH-阻抗监测时pH>7的反流事件,其成分主要包括弱碱性的胃分泌物、胰腺分泌物、胆汁以及反流前所进食物、气体等,非酸反流包括弱酸反流和弱碱反流,一项研究对具有典型烧心、反流症状的内镜阴性患者进行食管pH-阻抗监测,发现在SI和(或)SAP阳性患者中有超过80%的症状都与非酸反流相关[24]。本研究显示了弱碱反流在RH、FH患者较NERD中更为突出,因此推测弱碱反流可能在RH、FH的病理生理学中发挥一定的作用。
近年来认为近端反流在GERD患者的食管症状以及食管外症状的产生中起一定的作用。既往研究结果提示与健康对照组相比,广义NERD患者的近端反流事件明显增多;Bredenoord等[30]的研究显示,正常酸暴露但SAP阳性者近端反流明显增多,并认为这也是导致患者出现反流症状的重要因素;肖英莲等[31]的研究表明NERD患者较FH患者及健康对照组近端反流明显增多,且近端反流以酸反流为主。本研究证实,与FH相比,NERD和RH患者到达食管近端反流事件总的次数及百分比均更高,而且主要是酸反流和弱酸反流。这些数据均证实了反流事件的近端迁移(主要是酸反流和弱酸反流)与NERD和RH烧心症状密切相关。本研究还表明,NERD患者食团清除时间较FH患者明显延长,进一步证实了食管清除障碍在NERD病理生理学中的作用[32-34]。
综上所述,内镜阴性烧心患者是具有不同病理生理学的一组异质性患者,24 h食管pH-阻抗监测发现NERD患者以酸反流为主,但在RH和FH患者中,则以弱酸反流为主,且弱碱反流也显著增加。而且,NERD、RH患者的合计反流次数、混合反流次数、近端反流次数及百分比均明显多于FH患者,这可能有助于鉴别RH患者和FH患者,尤其是对于在24 h食管pH-阻抗监测期间无症状或未记录症状的内镜阴性且酸暴露正常的具有典型烧心、反流症状患者来说可能更有用,避免了频繁接受侵入性监测。然而,必须要强调的是, 在考虑区分NERD患者、RH患者和FH患者时,其反流模式在我们亚组之间尽管会有所差异,但也有部分的重叠,因此带有症状关联分析的pH-阻抗监测目前来说仍然是唯一可靠地对内镜阴性烧心人群进行亚分类的功能性方法。
Biography
张阿静, 硕士, E-mail: 369703906@qq.com
Contributor Information
张 阿静 (Ajing ZHANG), Email: 369703906@qq.com.
张 明鑫 (Mingxin ZHANG), Email: zmx3115@163.com.
References
- 1.Sandhu DS, Fass R. Current trends in the management of gastroesophageal reflux disease. Gut Liver. 2018;12(1):7–16. doi: 10.5009/gnl16615. [Sandhu DS, Fass R. Current trends in the management of gastroesophageal reflux disease[J]. Gut Liver, 2018, 12(1): 7-16.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eusebi LH, Ratnakumaran R, Yuan YH, et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67(3):430–40. doi: 10.1136/gutjnl-2016-313589. [Eusebi LH, Ratnakumaran R, Yuan YH, et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis[J]. Gut, 2018, 67(3): 430-40.] [DOI] [PubMed] [Google Scholar]
- 3.Fock KM, Talley N, Goh KL, et al. Asia-Pacific consensus on the management of gastro-oesophageal reflux disease: an update focusing on refractory reflux disease and Barrett's oesophagus. Gut. 2016;65(9):1402–15. doi: 10.1136/gutjnl-2016-311715. [Fock KM, Talley N, Goh KL, et al. Asia-Pacific consensus on the management of gastro-oesophageal reflux disease: an update focusing on refractory reflux disease and Barrett's oesophagus[J]. Gut, 2016, 65(9): 1402-15.] [DOI] [PubMed] [Google Scholar]
- 4.Tan VP, Wong BC, Wong WM, et al. Gastroesophageal reflux disease: cross-sectional study demonstrating rising prevalence in a Chinese population. J Clin Gastroenterol. 2016;50(1):e1–e7. doi: 10.1097/MCG.0000000000000304. [Tan VP, Wong BC, Wong WM, et al. Gastroesophageal reflux disease: cross-sectional study demonstrating rising prevalence in a Chinese population[J]. J Clin Gastroenterol, 2016, 50(1): e1-e7.] [DOI] [PubMed] [Google Scholar]
- 5.Iwakiri K, Kinoshita Y, Habu Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51(8):751–67. doi: 10.1007/s00535-016-1227-8. [Iwakiri K, Kinoshita Y, Habu Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015[J]. J Gastroenterol, 2016, 51(8): 751-67.] [DOI] [PubMed] [Google Scholar]
- 6.Kim K-M, Cho YK, Bae SJ, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study. Journal of Gastroenterology and Hepatology. 2012;27(4):741–5. doi: 10.1111/j.1440-1746.2011.06921.x. [Kim K-M, Cho YK, Bae SJ, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study[J]. Journal of Gastroenterology and Hepatology, 2012, 27(4): 741-5.] [DOI] [PubMed] [Google Scholar]
- 7.Kethman W, Hawn M. New approaches to gastroesophageal reflux disease. J Gastrointest Surg. 2017;21(9):1544–52. doi: 10.1007/s11605-017-3439-5. [Kethman W, Hawn M. New approaches to gastroesophageal reflux disease[J]. J Gastrointest Surg, 2017, 21(9): 1544-52.] [DOI] [PubMed] [Google Scholar]
- 8.Yadlapati R, DeLay K. Proton pump inhibitor-refractory gastroesophageal reflux disease. Med Clin North Am. 2019;103(1):15–27. doi: 10.1016/j.mcna.2018.08.002. [Yadlapati R, DeLay K. Proton pump inhibitor-refractory gastroesophageal reflux disease[J]. Med Clin North Am, 2019, 103 (1): 15-27.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabbard S, Vijayvargiya S. Functional heartburn: an underrecognized cause of PPI-refractory symptoms. Cleve Clin J Med. 2019;86(12):799–806. doi: 10.3949/ccjm.86a.19006. [Gabbard S, Vijayvargiya S. Functional heartburn: an underrecognized cause of PPI-refractory symptoms[J]. Cleve Clin J Med, 2019, 86 (12): 799-806.] [DOI] [PubMed] [Google Scholar]
- 10.Patel A, Gyawali CP. Gastroesophageal reflux monitoring. JAMA. 2018;319(12):1271–2. doi: 10.1001/jama.2018.1144. [Patel A, Gyawali CP. Gastroesophageal reflux monitoring[J]. JAMA, 2018, 319(12): 1271-2.] [DOI] [PubMed] [Google Scholar]
- 11.Yadlapati R, Vaezi MF, Vela MF, et al. Management options for patients with GERD and persistent symptoms on proton pump inhibitors: recommendations from an expert panel. Am J Gastroenterol. 2018;113(7):980–6. doi: 10.1038/s41395-018-0045-4. [Yadlapati R, Vaezi MF, Vela MF, et al. Management options for patients with GERD and persistent symptoms on proton pump inhibitors: recommendations from an expert panel[J]. Am J Gastroenterol, 2018, 113(7): 980-6.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ribolsi M, Giordano A, Guarino MPL, et al. New classifications of gastroesophageal reflux disease: an improvement for patient management? Expert Rev Gastroenterol Hepatol. 2019;13(8):761–9. doi: 10.1080/17474124.2019.1645596. [Ribolsi M, Giordano A, Guarino MPL, et al. New classifications of gastroesophageal reflux disease: an improvement for patient management[J]? Expert Rev Gastroenterol Hepatol, 2019, 13(8): 761-9.] [DOI] [PubMed] [Google Scholar]
- 13.Clouse RE, Richter JE, Heading RC, et al. Functional esophageal disorders. Gut. 1999;45(suppl 2):Ⅱ31–36. doi: 10.1136/gut.45.2008.ii31. [Clouse RE, Richter JE, Heading RC, et al. Functional esophageal disorders[J]. Gut, 1999, 45(suppl 2): Ⅱ31-36.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savarino E, Zentilin P, Tutuian R, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103(11):2685–93. doi: 10.1111/j.1572-0241.2008.02119.x. [Savarino E, Zentilin P, Tutuian R, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy[J]. Am J Gastroenterol, 2008, 103(11): 2685-93.] [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome Ⅳ. http://www.sciencedirect.com/science/article/pii/S0016508516002237. Gastroenterology. 2016;S0016-S5085(16):00223–7. doi: 10.1053/j.gastro.2016.02.032. [Drossman DA. Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome Ⅳ[J]. Gastroenterology, 2016: S0016-S5085(16)00223-7.] [DOI] [PubMed] [Google Scholar]
- 16.Yamasaki T, Fass R. Reflux hypersensitivity: a new functional esophageal disorder. J Neurogastroenterol Motil. 2017;23(4):495–503. doi: 10.5056/jnm17097. [Yamasaki T, Fass R. Reflux hypersensitivity: a new functional esophageal disorder[J]. J Neurogastroenterol Motil, 2017, 23(4): 495-503.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67(7):1351–62. doi: 10.1136/gutjnl-2017-314722. [Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus[J]. Gut, 2018, 67(7): 1351-62.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mishima I, Adachi K, Arima N, et al. Prevalence of endoscopically negative and positive gastroesophageal reflux disease in the Japanese. Scand J Gastroenterol. 2005;40(9):1005–9. doi: 10.1080/00365520510023260. [Mishima I, Adachi K, Arima N, et al. Prevalence of endoscopically negative and positive gastroesophageal reflux disease in the Japanese[J]. Scand J Gastroenterol, 2005, 40(9): 1005-9.] [DOI] [PubMed] [Google Scholar]
- 19.Savarino E, Marabotto E, Zentilin P, et al. The added value of impedance-pH monitoring to Rome Ⅲ criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig Liver Dis. 2011;43(7):542–7. doi: 10.1016/j.dld.2011.01.016. [Savarino E, Marabotto E, Zentilin P, et al. The added value of impedance-pH monitoring to Rome Ⅲ criteria in distinguishing functional heartburn from non-erosive reflux disease[J]. Dig Liver Dis, 2011, 43(7): 542-7.] [DOI] [PubMed] [Google Scholar]
- 20.Martinez SD, Malagon IB, Garewal HS, et al. Non-erosive reflux disease (NERD): acid reflux and symptom patterns. Aliment Pharmacol Ther. 2003;17(4):537–45. doi: 10.1046/j.1365-2036.2003.01423.x. [Martinez SD, Malagon IB, Garewal HS, et al. Non-erosive reflux disease (NERD): acid reflux and symptom patterns[J]. Aliment Pharmacol Ther, 2003, 17(4): 537-45.] [DOI] [PubMed] [Google Scholar]
- 21.Savarino E, Zentilin P, Tutuian R, et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol. 2012;47(2):159–68. doi: 10.1007/s00535-011-0480-0. [Savarino E, Zentilin P, Tutuian R, et al. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients[J]. J Gastroenterol, 2012, 47(2): 159-68.] [DOI] [PubMed] [Google Scholar]
- 22.Roman S, Keefer L, Imam H, et al. Majority of symptoms in esophageal reflux PPI non-responders are not related to reflux. Neurogastroenterol Motil. 2015;27(11):1667–74. doi: 10.1111/nmo.12666. [Roman S, Keefer L, Imam H, et al. Majority of symptoms in esophageal reflux PPI non-responders are not related to reflux[J]. Neurogastroenterol Motil, 2015, 27(11): 1667-74.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.戴 菲, 陈 芬荣, 邱 偲偲, et al. 24 h多通道食管阻抗-pH监测在鉴别非糜烂性反流病和功能性烧心中的作用. http://www.cqvip.com/qk/88648x/201314/49828728.html. 中华临床医师杂志:电子版. 2013;7(14):108–11. [戴菲, 陈芬荣, 邱偲偲, 等. 24 h多通道食管阻抗-pH监测在鉴别非糜烂性反流病和功能性烧心中的作用[J].中华临床医师杂志:电子版, 2013, 7(14): 108-11.] [Google Scholar]
- 24.宋 惠雯, 蒋 义贵, 张 生君, et al. 非糜烂性胃食管反流病患者的反流事件研究. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=lcxhbzz201604007. 临床消化病杂志. 2016;28(4):220–3. [宋惠雯, 蒋义贵, 张生君, 等.非糜烂性胃食管反流病患者的反流事件研究[J].临床消化病杂志, 2016, 28(4): 220-3.] [Google Scholar]
- 25.Zhang MY, Chen MH, Peng S, et al. The Rome Ⅳ versus Rome Ⅲ criteria for heartburn diagnosis: a comparative study. United European Gastroenterol J. 2018;6(3):358–66. doi: 10.1177/2050640617735084. [Zhang MY, Chen MH, Peng S, et al. The Rome Ⅳ versus Rome Ⅲ criteria for heartburn diagnosis: a comparative study[J]. United European Gastroenterol J, 2018, 6(3): 358-66.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.郭 宝娜, 郭 子皓, 姜 佳丽, et al. 胃食管反流病患者141例的24 h食管阻抗-pH监测结果. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhxhzz201904001. 中华消化杂志. 2019;39(4):217–22. [郭宝娜, 郭子皓, 姜佳丽, 等.胃食管反流病患者141例的24 h食管阻抗-pH监测结果[J].中华消化杂志, 2019, 39(4): 217-22.] [Google Scholar]
- 27.Friedenberg FK, Xanthopoulos M, Foster GD, et al. The association between gastroesophageal reflux disease and obesity. Am J Gastroenterol. 2008;103(8):2111–22. doi: 10.1111/j.1572-0241.2008.01946.x. [Friedenberg FK, Xanthopoulos M, Foster GD, et al. The association between gastroesophageal reflux disease and obesity[J]. Am J Gastroenterol, 2008, 103(8): 2111-22.] [DOI] [PubMed] [Google Scholar]
- 28.Nian YY, Feng C, Jing FC, et al. Reflux characteristics of 113 GERD patients with abnormal 24-h multichannel intraluminal impedance-pH tests. J Zhejiang Univ Sci B. 2015;16(9):805–10. doi: 10.1631/jzus.B1500027. [Nian YY, Feng C, Jing FC, et al. Reflux characteristics of 113 GERD patients with abnormal 24-h multichannel intraluminal impedance-pH tests[J]. J Zhejiang Univ Sci B, 2015, 16(9): 805-10.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.刘 冬梅, 刘 建军, 田 书瑞, et al. 肥胖与胃食管反流病关系的研究. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhxhzz201511001. 中华消化杂志. 2015;35(11):721–5. [刘冬梅, 刘建军, 田书瑞, 等.肥胖与胃食管反流病关系的研究[J].中华消化杂志, 2015, 35(11): 721-5.] [Google Scholar]
- 30.Bredenoord AJ, Weusten BL, Timmer R, et al. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy. Am J Gastroenterol. 2006;101(3):453–9. doi: 10.1111/j.1572-0241.2006.00427.x. [Bredenoord AJ, Weusten BL, Timmer R, et al. Addition of esophageal impedance monitoring to pH monitoring increases the yield of symptom association analysis in patients off PPI therapy [J]. Am J Gastroenterol, 2006, 101(3): 453-9.] [DOI] [PubMed] [Google Scholar]
- 31.肖 英莲, 林 金坤, 彭 穗, et al. 联合食管多通道腔内阻抗-pH监测在诊断胃食管反流病中的价值. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhxhzz200909001. 中华消化杂志. 2009;29(9):513–6. [肖英莲, 林金坤, 彭穗, 等.联合食管多通道腔内阻抗-pH监测在诊断胃食管反流病中的价值[J].中华消化杂志, 2009, 29(9): 513-6.] [Google Scholar]
- 32.Jiang LQ, Ye BX, Wang Y, et al. Esophageal body motility for clinical assessment in patients with refractory gastroesophageal reflux symptoms. J Neurogastroenterol Motil. 2017;23(1):64–71. doi: 10.5056/jnm16047. [Jiang LQ, Ye BX, Wang Y, et al. Esophageal body motility for clinical assessment in patients with refractory gastroesophageal reflux symptoms[J]. J Neurogastroenterol Motil, 2017, 23(1): 64-71.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Savarino E, Gemignani L, Pohl D, et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34(4):476–86. doi: 10.1111/j.1365-2036.2011.04742.x. [Savarino E, Gemignani L, Pohl D, et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease[J]. Aliment Pharmacol Ther, 2011, 34(4): 476-86.] [DOI] [PubMed] [Google Scholar]
- 34.Frazzoni M, de Bortoli N, Frazzoni L, et al. Impedance-pH monitoring for diagnosis of reflux disease: new perspectives. Dig Dis Sci. 2017;62(8):1881–9. doi: 10.1007/s10620-017-4625-8. [Frazzoni M, de Bortoli N, Frazzoni L, et al. Impedance-pH monitoring for diagnosis of reflux disease: new perspectives[J]. Dig Dis Sci, 2017, 62(8): 1881-9.] [DOI] [PubMed] [Google Scholar]


