Abstract
Nocardiosis is an infectious disease caused by the gram-positive bacterium Nocardia spp. Although it is commonly accepted that exposure to Nocardia is almost universal, only a small fraction of exposed individuals develop the disease, while the vast majority remain healthy. Nocardiosis has been described as an “opportunistic” disease of immunocompromised patients, suggesting that exposure to the pathogen is necessary, but a host predisposition is also required. Interestingly, increasing numbers of nocardiosis cases in individuals without any detected risk factors, i.e., without overt immunodeficiency, are being reported. Furthermore, a growing body of evidence have shown that selective susceptibility to a specific pathogen can be caused by a primary immunodeficiency (PID). This raises the question of whether an undiagnosed PID may cause nocardiosis affecting otherwise healthy individuals. This review summarizes the specific clinical and microbiological characteristics of patients with isolated nocardiosis published during the past 30 years. Furthermore, it gives an overview of the known human immune mechanisms to fend off Nocardia spp. obtained from the study of PIDs and patients under immunomodulatory therapies.
Keywords: Nocardia, nocardiosis, infection, primary immunodeficiencies, immune response, isolated nocardiosis, PID
Introduction
In 1888, while investigating a disease in cattle called “francine du boeuf,” the veterinarian Edmond Nocard identified a gram-positive, acid-fast agent as causative of this disease (1). A year after, Trevisan named this genus Nocardia in honor of Nocard (2). Shortly thereafter, Eppinger isolated from the brain abscess of a 52-year-old patient, an organism that produced star-shaped colonies when grown in agar. Although he called it Cladothrix asteroides, it was later found to be Nocardia asteroides. This finding made Nocardia be the first human pathogenic aerobic actinomycete described in the literature (3, 4). Since then and until the advent of antibiotics, over 30 cases of nocardiosis were described published, all but three with fatal outcome or very severe sequelae (5). After the generalization of antibiotic therapy, recovery rates improved to 54%, and an increased number of patients were every year (6). At this point, reports started to associate nocardiosis with underlying conditions. The first of such reports was published in 1954 in a patient with nocardiosis during Hodgkin's lymphoma (7). Many reports followed showing cases of nocardiosis in patients with alveolar proteinosis (8), prolonged steroid usage (9, 10), Cushing's syndrome (11), patients under immunosuppressive drugs after transplantation (12) or neoplastic disorders (6) amongst other pathologies (Table 1). Besides, reports started to be published describing severe nocardiosis in patients with primary immunodeficiencies (PID) such as hypogammaglobulinemia (13, 14), or chronic granulomatous disease (CGD) (15–17) (Table 2). At this point, nocardiosis was proposed to be an opportunistic infection (19–21). That notion was accepted in the mid-80s after a growing number of nocardiosis cases were described in patients with AIDS (22–24). Interestingly, epidemiological studies in the United States of America indicated that not all patients with nocardiosis suffer from underlying disease (25, 26). As a matter of fact, according to the Center for Disease Control (CDC), one-third of nocardiosis patients have no known underlying condition. Furthermore, a growing body of evidence shows that severe infectious diseases in otherwise healthy individuals can arise from single-gene inborn errors of immunity (27, 28). Some examples of this are mendelian susceptibility to mycobacterial disease (MSMD) (28), human papillomavirus-associated epidermodysplasia verruciformis (29), invasive pneumococcal disease (30), invasive dermatophytic disease (31), or chronic mucocutaneous candidiasis (32). All these genetic diseases confer a selective susceptibility to a specific pathogen of weak virulence and ubiquitous exposure, much-resembling nocardiosis in patients without identified underlying conditions. In this review, we describe the epidemiological, clinical, and microbiological characteristics of 400 patients with nocardiosis without identified risk factors published during the past 30 years. We have also reviewed what we have learnt from patients with PIDs and patients with different comorbidities about the critical players of human immunity to Nocardia spp.
Table 1.
Some risk factors for nocardiosis.
| Diseases |
|---|
| AIDS |
| Solid-organ transplant |
| Chronic obstructive pulmonary disease |
| Chronic kidney disease |
| Cushing's syndrome |
| Pulmonary fibrosis |
| Diabetes mellitus |
| Systemic Lupus erythematosus |
| Hematopoietic stem cell transplantation |
| Drug abuse |
| Malignancies |
| End-stage renal disease |
| Membranoproliferative glomerulonephritis |
| Lung sarcoidosis |
| Pulmonary proteinosis |
| Alcoholism long history of smoking |
Table 2.
PIDs that can cause nocardiosis.
| Disease | Immunological consequences |
|---|---|
| CGD | Defects in the NADPH oxidase complex that impairs the capacity of phagocytes to produce reactive oxygen species. |
| Hypogammaglobulinemia | Reduction in the titers of circulating antibodies. |
| CVID | Deficient levels of IgG, IgA, and IgM*. |
| Hyper IgE syndrome | Elevated serum IgE level, chronic dermatitis, intense pruritus, and severe recurrent infection. |
| Idiopathic CD4+ T-lymphocytopenia | Low levels of CD4+ T cells. |
| SCID | Lack of B and T cells. |
| MSMD | IL-12 and IL-23 abolishment**. |
| Anti-GM-CSF autoantibodies | Blockade of GM-CSF. |
CVID is a heterogeneous group of diseases that can present with multiple different immunological abnormalities. The immunological consequences shown here are the ones observed in the patient reported in Singh et al. (18).
The genetic causes of MSMD can impair multiple branches of IFN-γ-mediated immunity. The genetic etiologies of MSMD that sometimes curse with nocardiosis impair IL-12 and IL-23 signaling.
Epidemiology
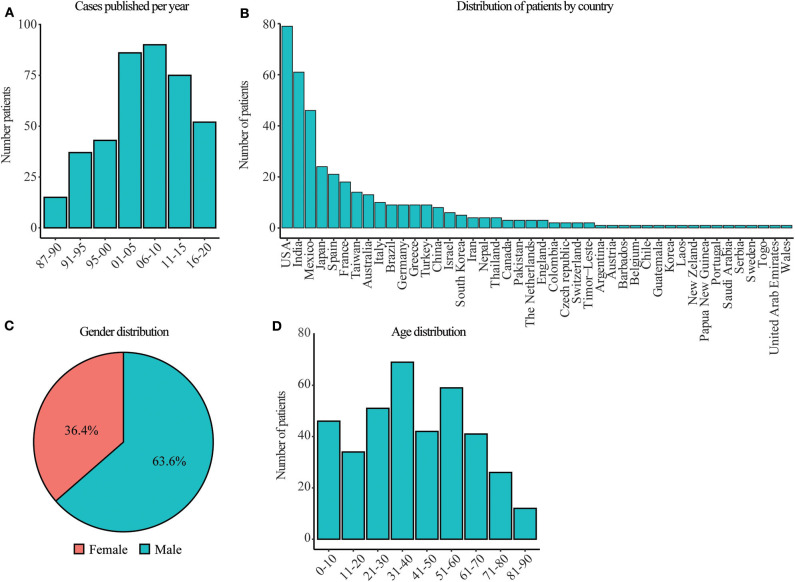
The description of patients with isolated nocardiosis after the HIV outbreak has been increasing steadily since the mid-80s, as evidenced by the number of case reports published in the literature over the last 30 years (Figure 1A). All the reported cases were sporadic, and no underlying condition was identified in any of them. Moreover, they did not come from consanguineous marriages, or the consanguinity was not indicated except in one patient (298). None of these patients were immunologically or genetically studied in search of a PID or other genetic defects. Patients with isolated nocardiosis have been found in 44 different countries spreading through 6 continents (all except Antarctica) with the USA, India, and Mexico having the most cases reported (Figure 1B). Contrary to other infectious diseases, nocardiosis is not a geographically confined disease, consistent with the fact that Nocardia spp. can be found throughout the world. We have observed that the number of males with isolated nocardiosis almost doubles that of female cases, similar to observations in immunocompromised individuals (25) (Figure 1C). Given that Nocardia spp. grow in soil; these gender biases may be due to a difference in exposure caused by the distinct lifestyle and profession of man vs. women. Besides, the female hormone estradiol has been shown to inhibit the growth of Nocardia brasiliensis in vitro, suggesting that the presence of this hormone might also contribute to the gender difference observed (299). Furthermore, this may be an indication of an undiagnosed X-linked immunodeficiency. We have found a homogeneous distribution among age groups in patients with isolated nocardiosis with a slight increase in the numbers of patients in the decades of 31–40 and 51–60 years of age (Figure 1D). This age distribution suggests that disease occurs when exposure to the pathogen happens thought life without any specific age group been overrepresented or more susceptible. Transmission of Nocardia spp. do not occur from person to person, and outbreaks are rare. Since the 80s, a handful of outbreaks have been reported in the UK, France, Japan, Germany, and the US. All in groups of patients interned in hospitals and with some level of immunosuppression (300–306). Therefore, this observation indicates that the leading risk factor in developing nocardiosis is the immune status of the host rather than the virulence of the different Nocardia strains.
Figure 1.
Date, gender, age, and geographical distribution of patients with isolated nocardiosis. (A) Year of publication of patients with isolated nocardiosis since 1987. Around 2010 the number of case series published increased in detriment of individual case reports. In most of those case series, we could not extract the data from individual patients so we excluded them from our analysis. Therefore, the number of cases continuously increases with time despite the graph shows a decrease after 2010. (B) Countries where patients from A were reported. (C) Gender distribution of patients with isolated nocardiosis. (D) Age distribution of patients with isolated nocardiosis published since 1987. The information for these figures was obtained from the references (33–297).
Clinical Presentation
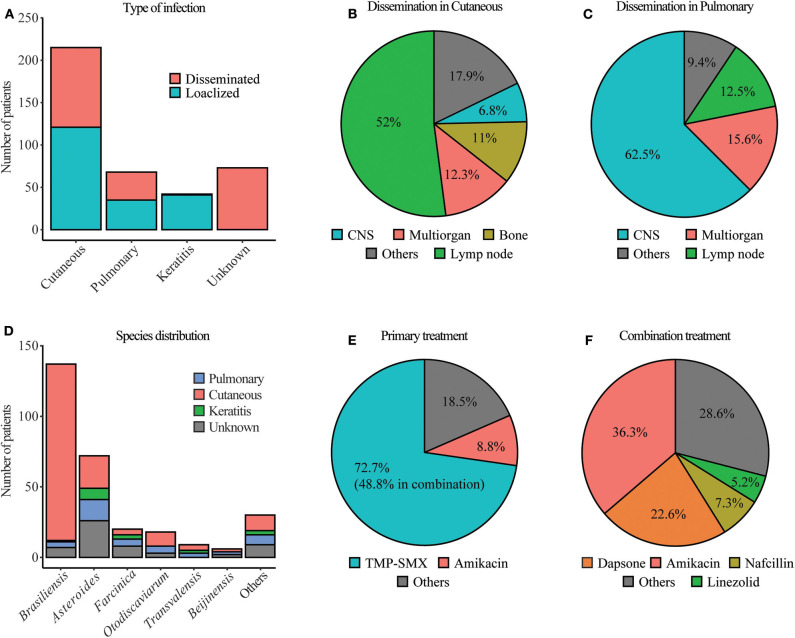
Nocardiosis can present as a cutaneous disease when the bacterium is inoculated in the skin, usually through a puncture or wound, pulmonary when the bacterium is inhaled and gets to the lungs or disseminated when from these initial foci of infection, it spreads to other organs. In most cases, upon infection, the immune system neutralizes this bacterium, and individuals remain asymptomatic or suffer from a mild self-resolving disease that frequently goes undiagnosed. The classical presentation of pulmonary nocardiosis includes cough, fever, dyspnea, fatigue, and chest pain (307). At the radiological level, it can present as a focal or multifocal disease with infiltrates (nodular or consolidated) and pleural effusion (308). In the case of cutaneous or subcutaneous nocardiosis, the lesions usually show expanding nodules, cellulitis, and ulcerative draining lesions. A fraction of cutaneous nocardiosis develops as mycetoma. These lesions are chronic, slow-progressing, and painless, usually in the lower limbs that present with tumefaction, destructive granuloma, deformity, subcutaneous nodules, and discharging sinuses that exude pus (309). In a priori, immunocompetent individuals, a sizable number of patients have keratitis caused by Nocardia spp. Keratitis usually happens after cornea injury in contact lenses wearers, causing the inoculation of the pathogen. It presents as an inflammatory eye condition, pain, photophobia, and visual impairment. If untreated or misdiagnosed, it might lead to endophthalmitis (309). From the primary foci of infection, the disease can disseminate hematogenously potentially to any organ in the body, and after dissemination occurs, mortality and morbidity increase dramatically. Nocardia spp. have a particular tropism for the CNS. When dissemination happens there, the disease tends to present as headache, seizures, mental status change, confusion, ataxia, or focal neurological deficit may appear. A brain abscess is usually visible by computed tomography (CT) or magnetic resonance imaging (MRI) scans (310). It has been proposed that pulmonary nocardiosis is a disease of immunocompromised individuals, while the cutaneous disease is observed in immunocompetent individuals (308). However, in-depth immunological and genetic studies of patients with a priori, no additional risk factors have not been performed, preventing us from concluding if these patients referred to in the literature as immunocompetent have an undiagnosed immunodeficiency. We observed that the majority of cases of isolated nocardiosis showed cutaneous disease (Figure 2A). However, we also found a sizeable number of patients with pulmonary nocardiosis without underlying conditions. In both cases of isolated nocardiosis, cutaneous, and pulmonary, dissemination from the primary foci of infection is about 45% (Figure 2A). Patients with keratitis caused by Nocardia spp., except in one case, do not present with disseminated disease. Besides, 15% of patients reported presented with a disseminated disease without identification of the primary location of the infection (Figure 2A). When dissemination happened, the organs to which the disease disseminated was dependent on the original site of infection. In more than half of the patients with dissemination from cutaneous infection, the organs affected were the lymph nodes closest to the location of infections. In 12% of the cases, the dissemination occurred to multiple organs, and in 11%, cutaneous nocardiosis gave rise to bone involvement, often osteomyelitis (Figure 2B). Other organs such as CNS, muscle, lung, salivary gland, or ovaries were involved in some patients. When dissemination occurred from primary pulmonary infection, 62% of the patients developed CNS nocardiosis, 15% suffered from multiorgan dissemination, and in 12%, the disease disseminated to the closest lymph nodes (Figure 2C). Other organs were also described to be affected in some patients, such as bone or mediastine.
Figure 2.
Microbiology, treatment, and kind of infection in patients with isolated nocardiosis. (A) Type of infection of patients with isolated nocardiosis published since 1987. Unknown represent patients with disseminated nocardiosis in which the primary site of infection was not identified. (B,C) Organs, where the disease disseminated in patients with cutaneous nocardiosis in (B) and pulmonary nocardiosis in (C). Others, represent organs with a frequency of <5% in this group. (D) Distribution of Nocardia species in the different types of nocardiosis at a frequency of <5%. Others represent the species present. (E) Primary treatment of patients with isolated nocardiosis. (F) Therapy that was used in combination with TMP-SMX. Others represent the use of drugs at a frequency of <5%. The information for these figures was obtained from the references (33–297).
Microbiology
Nocardia is a genus of aerobic gram-positive bacteria of the order Actinomycetales. It is characterized by weak acid-fast stain, catalase-positive, presence of mycolic acid in its cell wall, and rod-shaped that grows in branches, sometimes confusing itself with fungi. It can be found in soil and areas rich in organic material. Nocardia has also been reported to be a commensal after it was identified in the skin, lung aspirates, and gingiva from healthy individuals (311–313), although this has recently been refuted (314). At the time of writing this report, there were 109 different Nocardia species with confirmed names according to the List of Prokaryotic names with Standing Nomenclature (LPSN) (https://www.bacterio.net). Among them, 54 had been reported to cause disease in humans (315). We have seen that 23 different species cause disease in otherwise healthy individuals (Table 3). Nowadays, the guidelines for identifying Nocardia up to the species without ambiguity suggest a combination of MALDI-TOF mass spectrometry, gene sequencing, and, ultimately, genome sequencing (315). Using these methods, during the last decades, what was thought to be an individual species, like Nocardia asteroides, has been found to be composed of different species to the point that N. asteroides is no longer a valid nomenclature (315, 316). Unfortunately, most diagnostic labs do not have these capabilities, so N. asteroides is still considered in the clinical setting.
Table 3.
Count of the different Nocardia species identified in patients with isolated nocardiosis.
| Pathogen | n |
|---|---|
| N. brasiliensis | 137 |
| N. asteroides | 68 |
| N. farcinica | 20 |
| N. otitidiscaviarum | 18 |
| N. transvalensis | 9 |
| N. beijingensis | 6 |
| N. nova | 5 |
| N. abscessus | 5 |
| N. wallacei | 3 |
| N. paucivorans | 3 |
| N. takedensis | 2 |
| N. elegans | 2 |
| N. cyriacigeorgica | 2 |
| N. asiatica | 2 |
| N. yamanashiensis | 1 |
| N. vinacea | 1 |
| N. puris | 1 |
| N. pseudobrasiliensis | 1 |
| N. harenae | 1 |
| N. crassostrea | 1 |
| N. caviae | 1 |
| N. arthritidis | 1 |
| N. aobensis | 1 |
Diagnosis
Multiple proteins from N. asteroides and brasiliensis have been described as being specifically recognized by patients who have suffered nocardiosis but not by healthy controls (317–321). These serologic tests are not commercially available, and the ones described are unreliable, making clinical diagnosis difficult (322). The observation of the symptoms and other physical tests like radiologic images may be suggestive of the disease (322). However, observation of Nocardia in cultures is necessary to confirm the diagnosis (309). Identification of the pathogen occurs by growing the clinical specimen (sputum, bronchoalveolar lavage, pleural effusion, pus) on plates like tryptic soy blood agar at 35°C. The identification of Nocardia is usually based on partial acid-fastness, resistance to lysozyme, and presence of chalky white colonies, dichotomous branches, and aerial hyphae (323). Colonies may appear after 2 days, but it is recommended to keep the plates in culture for up to 3 weeks since many species take longer to grow. Therefore, the prolonged incubation required to identify the bacteria that, unfortunately, many laboratories fail to follow, makes nocardiosis and underrepresented and underdiagnosed disease, especially in patients without risk factors. Despite the methodologies described above to identify Nocardia up to the specie, most diagnostic laboratories only have access to conventional biochemical tests such as tyrosine, xanthine, and hypoxanthine decomposition, growth at 45°C, and gelatin hydrolysis (323). The most used molecular biology methods that are found in a diagnostic lab to identify different Nocardia spp. are gene sequencing of 16S rRNA or hsp65. With these limitations in mind and considering that some patients described in this review were diagnosed up to 35 years ago, the most frequently identified species in patients with isolated nocardiosis are; N. brasiliensis, N. asteroids, N. farcinica, N. otodiscaviarum, N. transvalensis and N. Beijinensis (Figure 2D) (Table 3). Around 90% of cases of N. brasiliensis are cutaneous, consistent with what was observed in immunocompromised patients (324). However, the other five species cause cutaneous, pulmonary, or keratitis, with frequencies proportional to their identification in clinical specimens (Figure 2D). This contradicts the notion observed in immunocompromised individuals suggesting that N. brasiliensis causes cutaneous disease while N. asteroides causes pulmonary disease (324). The lack of clinical, epidemiological, and laboratory data undermines the significance of Nocardia spp. as a potential pathogen and causes a delay in the start of appropriate treatment (325). Sometimes the diagnosis only happens post mortem, highlighting the importance and necessity of improving the diagnosis methodologies and better understanding the causes of nocardiosis in these patients without risk factors (326).
Treatment and Outcome
Treatment for nocardiosis has been evolving since the early 20th century. The first successful treatment of a patient with nocardiosis was described in 1907 by Musgrave and Clegg in a 30-year-old woman with mycetoma. Treatment consisted of amputating the affected extremity (327). Since then, only two more patients were successfully treated until the 40s (328, 329). After 1943, an increasing number of survivors were reported due to the use of the first antibiotics (sulfanilamide, penicillin, streptomycin, aureomycin), sulfonamides, and surgical incision and drainage (5). Until sulfonamide therapy became available, the mortality observed in patients with nocardiosis was 76%. After its implementation, mortality dropped to 46% (6). Nowadays, sulfonamides are the drug of choice, despite the first attempt at using them to treat nocardiosis in 1937 was unsuccessful (330). The first successful treatment of nocardiosis with sulfonamides happened a few years after in 1943 (331). In the mid-70s, patients started to be successfully treated with a 1:5 proportion of the dihydrofolate reductase inhibitor trimethoprim and the sulfonamide antibiotic sulfamethoxazole. This combination of drugs is known as TMP-SMX or co-trimoxazole. TMP-SMX has the advantage that it easily reaches antibacterial concentrations in the lung, blood, and central nervous system (332). Despite the question of whether TMP-SMX treatment was more effective than sulfonamides was controversial (333), it became the treatment of choice. It was thought that all Nocardia strains are susceptible to these drugs (334); however, this is not the case, and susceptibility testing should be performed before starting the treatment (335), given that resistance is specie specific (336, 337). Besides, some people are allergic to TMP-SMX, which is sometimes observed after treatment starts with the additional risk that this brings for the patient (338). The standards dictate that for cutaneous disease, TMP-SMX should be administered for 1–3 months, for pulmonary disease during 6–12 months, and for disseminated, especially CNS infection, it should be of 12 months sometimes, even more, depending on the progress of the disease (339). The long treatment necessary to cure nocardiosis with TMP-SMX highlights the commonly induced side effects such as nausea, vomiting, diarrhea, gingival hyperplasia (340), acute pancreatitis (341), myelosuppression, hepatoxicity, and renal insufficiency (308, 338) among others. Seventy-two percent of patients with isolated nocardiosis were treated with TMP-SMX, 8% with the aminoglycoside antibiotic, Amikacin, and the last 18% with other drugs such as the beta-lactam antibiotic imipenem or the penicillin antibiotic nafcillin among others (Figure 2E). In some cases, the treatment occurred only with one drug; however, about half of the patients treated with TMP-SMX had this treatment combined with other medications. This combination therapy involved Amikacin in 36% of the cases, dapsone in 22%, the beta-lactam antibiotic Nafcillin in 7% of the cases, and the oxazolidinone Linezolid in 5% of cases (Figure 2F). The way of administration of the drug varied depending on the kind of disease. In cutaneous or keratitis patients, the treatment was administered mostly topically, while in pulmonary or disseminated, the antibiotics were ingested. In the most severe cases, the medication was injected intravascularly. Antibiotic treatment was used in combination with surgical intervention in 18.3% of cases. Most surgeries consisted of debridement or drainage of affected areas in the lymph nodes, CNS, lungs, or extremities, although other interventions such as limb amputation were observed. Despite treatment, in 23.1% of patients, the disease could not be cured, becoming chronic, the disease recurred after the first episode was thought to be resolved, or the patients had sequelae such as impaired vision, neurological impairment, limb amputation, or severe scarring. Besides, an overall 5.7% of the patient died due to complications caused by nocardiosis. The outcome of these patients gives an idea of the severity of this disease even with appropriate treatment in patients that do not have any additional comorbidity. It also showcases the importance of early diagnosis and the need for better diagnostic and treatment options of isolated nocardiosis.
Human Immunity to Nocardia spp.
Reports investigating how the human immune system fights Nocardia spp. are scarce. However, the study of patients treated with immunosuppressive drugs, anti-cytokine antibody, and information obtained from patients with PIDs has given us a clue of how such immunity is orchestrated (Tables 2, 4). PIDs are a group of diseases caused by single-gene inborn errors of immunity that impair specific cell-types or pathways of the immune system and are characterized by severe infection. The study of these diseases carried out during the last few decades has allowed us to delineate what are the critical and non-redundant cell-types and pathways in immunity against given pathogens (342). By analyzing what PIDs curse with nocardiosis, we can infer some of these anti-Nocardia immune mechanisms. The first PID in which nocardiosis was observed was chronic granulomatous disease (CGD). CGD is characterized by the impaired capacity of phagocytes to produce reactive oxygen species and, therefore, kill certain bacteria, especially catalase-positive ones (343). Early after the description of CGD, pulmonary nocardiosis started to be identified as one of the common infections suffered by these groups of patients (15–17). Since then, numerous reviews and cohort studies have shown the presence of nocardiosis among patients with CGD (343–347). From these groups of PID patients, we have been able to infer that phagocytes play a critical role in human immunity to Nocardia spp. Furthermore, it has been shown that human-derived alpha-defensins from neutrophils can kill certain strains of Nocardia, including farcinica, nova, and asteroides strengthening the evidence of the role of neutrophils in anti-Nocardia immunity (348).
Table 4.
Treatments that affect the immune system and predispose to nocardiosis.
| Treatment | Immunological consequence | Examples of diseases treated |
|---|---|---|
| Anti-BTK | Reduces B cell activation | Hematologic malignancies such aschronic lymphocytic leukemia (CLL). |
| Anti-CD3 | Reduces T cell activation | Solid organ transplant rejection. |
| Anti-CTLA-4 | Enhances T cell immunity | Melanoma, carcinoma. |
| Anti-CD52 | Depletes peripheral blood lymphocytes | Multiple sclerosis, CLL. |
| Steroid | Reduces cellular immunity | Organ transplant rejection, asthma, allergies, dermatitis, Crohn's disease,rheumatoid arthritis. |
| Anti-TNF | Blocks of TNF signaling | Inflammatory bowel disease, Crohn's disease, rheumatoid arthritis. |
| Anty-IL12p40 | Blocks IL-12 and IL-23 signaling | Inflammatory bowel disease, Crohn's disease, psoriasis. |
| Chemotherapy | Affects the bone marrow reducing cellular immunity | Cancer. |
B cells and antibody-mediated immunity seems to be important in immunity against Nocardia spp. In patients with mycetoma, IgG1, 2, 3, 4, and M are higher than those in controls, suggesting an antibody response against Nocardia spp. (349). Interestingly, some patients with hematologic malignancies treated whit anti-BTK therapy develop this disease, highlighting the importance of B cells (350). Antibody disorders have also been described in patients with nocardiosis. In 1977, two cases of nocardiosis were described in patients with hypogammaglobulinemia. This disease consists of a reduction in the titers of antibodies and hence impaired immune response (13, 14). Similarly, a nocardiosis patient with common variable immunodeficiency consisting of deficient levels of IgG, IgA, and IgM was reported (18). Finally, one pediatric patient with hyper IgE syndrome, a disease characterized by elevated serum IgE level, chronic dermatitis, intense pruritus, and severe recurrent infection, died due to Nocardia infection (351). Despite the mechanisms in which B cells and antibody-mediated responses contribute to immunity to Nocardia spp. is not well-understood; the clinical evidence showcases the role of B cell-mediated immunity in fending off Nocardia spp.
The observation that patients who have AIDS develop nocardiosis made evident early on that T cells are essential to keep Nocardia at bay (22–24). Nocardia spp. infection is usually seen in these patients when CD4+ counts drop to 35 cells/μl (352). Consistently, two patients with CD4+ T cell lymphocytopenia that developed pulmonary and CNS nocardiosis have been reported (353, 354). Similarly, dampened cellular immunity in patients treated with corticosteroids long-term also predisposes to nocardiosis (355). Furthermore, treatments that block cell mediated immunity such as CD3 (OKT3) or CD52 in the treatment of autoimmune and autoinflammatory diseases, have also been shown to predispose to nocardiosis (356–358). Finally, a severe combined immunodeficiency patient lacking B and T cells with a Nocardia infection has been reported (111). These studies confirm the role of T cells in immunity against Nocardia and suggest that CD4+ T cells play a pivotal role in such immunity.
Specific cytokines have also been implicated in human immunity to Nocardia spp. It has been observed that PBMCs from patients with mycetoma caused by N. brasiliensis show low IFN-γ production when stimulated with N. brasiliensis lysates ex vivo but a high concentration of IL-4, IL-10, IL-12, and TNF making the authors suggest at TH2 response (359). The widespread use of blocking antibodies against cytokines for therapy of autoimmune and autoinflammatory diseases, confirmed the importance of TNF to fight Nocardia spp. Some patients under treatment with anti-TNF antibodies used to treat Crohn's disease (360) or inflammatory bowel disease (361) to develop nocardiosis as a complication. More extensive studies of cohorts of patients with different conditions, all treated with anti-TNF, confirmed that the blockade of TNF causes nocardiosis in a percentage of those patients (362, 363). Anti-IL-12p40 therapy (Blocking both IL-12 and IL-23) also used for inflammatory diseases such as inflammatory bowel disease has been described to cause nocardiosis in a patient from Australia (364). The vital role of these two cytokines, IL-12 and IL-23, in immunity against Nocardia spp. was confirmed by studying patients with IL-12Rβ1 and IL-12p40 complete deficiencies. These two deficiencies abolish both IL-12 and IL-23 signaling and are genetic etiologies of MSMD. Patients with MSMD display a selective susceptibility to infection by weakly virulent mycobacteria (26). A group of patients with either IL-12p40 or IL-12Rβ1 complete deficiency has been described to curse with nocardiosis combined with Mycobacteria, Salmonella, or Klebsiella. This shows the importance of IL-12 and or IL-23 in immunity against Nocardia spp. (365–368). Furthermore, in a set of mixed lymphocyte reaction experiments with N. farcinica, the authors showed that monocyte-derived DCs co-cultured with T cells are capable of producing high levels of TNF and IL-23 and eliminate engulfed N. farcinica. This experiment corroborates the importance of IL-23 and suggests that DCs contribute to fighting Nocardia (369). Besides, some nocardiosis patients with, a priori, no additional risk factor, have been found to produce neutralizing anti-GM-CSF auto-antibodies (370). Overall, the combination of clinical, pharmacological, immunological, and genetic evidence indicates that TNF, GM-CSF, IL-12, and or IL-23 are essential players in immunity against Nocardia spp.
Concluding Remarks, Is Nocardiosis a PID?
Although nocardiosis is considered a disease of immunocompromised individuals, the evidence shows that individuals, a priory healthy, can also have this disease. The description of such patients has been growing during recent decades, although it is still considered to be underestimated. In this group of patients, the disease is less severe than in immunocompromised individuals. However, even after appropriate treatment, mortality, and morbidity are high. Sometimes this is due to the late diagnosis and late application of the treatment given that this disease is not considered in the differential diagnosis in patients without risk factors. Besides, TMP-SMX, the most frequently used therapy in this group of patients, has numerous side effects. Therefore, the study of patients with isolated nocardiosis is necessary to better understand the causes and pathophysiology of this disease, which will improve its diagnosis and treatment. During the past two decades, the notion that severe infectious disease in patients otherwise healthy can arise from single-gene inborn errors of immunity has taken steam (27, 28). The genetic dissection of diseases such as MSMD (26), human papillomavirus-associated epidermodysplasia verruciformis (29), invasive pneumococcal disease (371), invasive dermatophytic disease (372), or chronic mucocutaneous candidiasis (32) among others, have shown that mutations in one gene can cause a selective susceptibility to one specific kind of pathogens. That has allowed scientists and physicians to delineate the critical and non-redundant players in immunity against that given pathogen and propose preventive treatment to individuals at risk as well as genetic diagnosis and counseling for patients and families. Nocardiosis shows some similarities with the diseases mentioned above since it is also caused by a weakly virulent pathogen of ubiquitous exposure. Patients with a weakened immune system are more susceptible and given that outbreaks only occur among immunosuppressed individuals shows that exposure to Nocardia spp. is necessary, but a host predisposition is also needed. Therefore, isolated nocardiosis may be an undiagnosed PID caused by a single-gene inborn error of immunity that can explain its selective susceptibility to Nocardia spp. infection. To test this hypothesis and to try to improve the diagnosis and treatment of this group of patients, we are recruiting patients with isolated nocardiosis to identify the genetic and immunological causes of this disease.
Author Contributions
RM-B did the literature research, analyzed, and graphed the data and wrote the manuscript.
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
RM-B would like to thank Janet Markle (VUMC), Sergio M. Pontejo (NAIAID, NIH), Jean-Laurent Casanova (The Rockefeller University), Jacinta Bustamante (Université Paris Descartes) for editorial assistance and critical reading.
References
- 1.Nocard EIE. Note sur la maladie des boeufs de la Guadeloupe, connue sous le nom de farcin. Ann Inst Pasteur. (1888) 293–302. [Google Scholar]
- 2.Trevisan I Generi e le Specie delle Batteriacee. Milano: Tipo-lit, Zanaboni e Gabuzzi; (1889) [Google Scholar]
- 3.Eppinger H. Ueber eine neue pathogenic Cladothrix und eine durch sie hervorgerufene Pseudotuberculosis. Wien Klin Wochenschr. (1890) 3: 321–3. [Google Scholar]
- 4.Waksmana SA, Henricib AT. The nomenclature and classification of the actinomycetes. J Bacteriol. (1943) 46:337–41. 10.1128/JB.46.4.337-341.1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cruz PT, Clancy CF. Nocardial osteomyelitis and septicemia. Am J Pathol. (1952) 28:607–27. [PMC free article] [PubMed] [Google Scholar]
- 6.Murray JF, Finegold SM, Froman S, Will DW. The changing spectrum of nocardiosis. a review and presentation of nine cases. Am Rev Respir Dis. (1961) 83:315–30. 10.1164/arrd.1961.83.3.315 [DOI] [PubMed] [Google Scholar]
- 7.Seeliger H, Lange J. Nocardiosis in the final stage of Hodgkin's disease. Z Tropenmed Parasitol. (1954) 3:356–62. [PubMed] [Google Scholar]
- 8.Beeson PB. Nocardiosis as a complication of pulmonary alveolar proteinosis. Ann Intern Med. (1964) 60:314. 10.7326/0003-4819-60-2-314 [DOI] [PubMed] [Google Scholar]
- 9.Kerbel NC. Long-term steroid therapy of the nephrotic syndrome in an adult complicated by fatal nocardiosis. Can Med Assoc J. (1962) 87:129–32. [PMC free article] [PubMed] [Google Scholar]
- 10.Whitmore DN, Gresham GA, Grayson MJ. Nocardiosis in anaemic patients given steroids. J Clin Pathol. (1961) 14:259–63. 10.1136/jcp.14.3.259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danowski TS, Cooper WM, Braude A. Cushing's syndrome in conjunction with Nocardia asteroides infection. Metabolism. (1962) 11:265–72. [PubMed] [Google Scholar]
- 12.Hill RB, Jr, Rowlands DT, Jr, Rifkind D. Infectious pulmonary disease in patients receiving immunosuppressive therapy for organ transplantation. N Engl J Med. (1964) 271:1021–7. 10.1056/NEJM196411122712001 [DOI] [PubMed] [Google Scholar]
- 13.Murray KJ, Ackerman SK, Chou SN, Douglas SD. Hypogammaglobulinemia and Nocardia brain abscesses. Neurosurgery. (1977) 1:297–9. 10.1227/00006123-197711000-00015 [DOI] [PubMed] [Google Scholar]
- 14.Sher NA, Hill CW, Eifrig DE. Bilateral intraocular Nocardia asteroides infection. Arch Ophthalmol. (1977) 95:1415–8. 10.1001/archopht.1977.04450080125015 [DOI] [PubMed] [Google Scholar]
- 15.Stites DP, Glezen WP. Pulmonary nocardiosis in childhood. a case report. Am J Dis Child. (1967) 114:101–5. 10.1001/archpedi.1967.02090220107020 [DOI] [PubMed] [Google Scholar]
- 16.Glezen WP. Infection and chronic granulomatous disease. J Pediatr. (1974) 84:160–1, author reply 161. 10.1016/S0022-3476(74)80587-1 [DOI] [PubMed] [Google Scholar]
- 17.Good RA, Quie PG, Windhorst DB, Page AR, Rodey GE, White J, et al. Fatal (chronic) granulomatous disease of childhood: a hereditary defect of leukocyte function. Semin Hematol. (1968) 5:215–54. [PubMed] [Google Scholar]
- 18.Singh S, Samant R, Rodrigues C. Nocardiosis in a patient with common variable immunodeficiency. J Assoc Physicians India. (2006) 54:495–6. Available at: https://www.ncbi.nlm.nih.gov/pubmed/16909702 [PubMed] [Google Scholar]
- 19.Saltzman HA, Chick EW, Conant NF. Nocardiosis as a complication of other diseases. Lab Invest. (1962) 11:1110–7. [PubMed] [Google Scholar]
- 20.Utz JP. The spectrum of opportunistic fungus infections. Lab Invest. (1962) 11:1018–25. [PubMed] [Google Scholar]
- 21.Cross RM, Binford CH. Is nocardia asteroides an opportunist? (1962) 11:1103–9. [PubMed] [Google Scholar]
- 22.Sharer LR, Kapila R. Neuropathologic observations in acquired immunodeficiency syndrome (AIDS). Acta Neuropathol. (1985) 66:188–98. 10.1007/BF00688583 [DOI] [PubMed] [Google Scholar]
- 23.Rodriguez JL, Barrio JL, Pitchenik AE. Pulmonary nocardiosis in the acquired immunodeficiency syndrome. diagnosis with bronchoalveolar lavage and treatment with non-sulphur containing drugs. Chest. (1986) 90:912–4. 10.1378/chest.90.6.912 [DOI] [PubMed] [Google Scholar]
- 24.Adair JC, Beck AC, Apfelbaum RI, Baringer JR. Nocardial cerebral abscess in the acquired immunodeficiency syndrome. Arch Neurol. (1987) 44:548–50. 10.1001/archneur.1987.00520170074026 [DOI] [PubMed] [Google Scholar]
- 25.Beaman BL, Burnside J, Edwards B, Causey W. Nocardial infections in the United States, 1972–1974. J Infect Dis. (1976) 134:286–9. 10.1093/infdis/134.3.286 [DOI] [PubMed] [Google Scholar]
- 26.Bustamante J. Mendelian susceptibility to mycobacterial disease: recent discoveries. Hum Genet. (2020) 139:993–1000. 10.1007/s00439-020-02120-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Casanova JL. Severe infectious diseases of childhood as monogenic inborn errors of immunity. Proc Natl Acad Sci USA. (2015) 112:E7128–37. 10.1073/pnas.1521651112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Casanova JL. Human genetic basis of interindividual variability in the course of infection. Proc Natl Acad Sci USA. (2015) 112:E7118–27. 10.1073/pnas.1521644112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Jong SJ, Imahorn E, Itin P, Uitto J, Orth G, Jouanguy E, et al. Epidermodysplasia verruciformis: inborn errors of immunity to human beta-papillomaviruses. Front Microbiol. (2018) 9:1222. 10.3389/fmicb.2018.01222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Picard C, Puel A, Bonnet M, Ku CL, Bustamante J, Yang K, et al. Pyogenic bacterial infections in humans with IRAK-4 deficiency. Science. (2003) 299:2076–9. 10.1126/science.1081902 [DOI] [PubMed] [Google Scholar]
- 31.Lanternier F, Pathan S, Vincent QB, Liu L, Cypowyj S, Prando C, et al. Deep dermatophytosis and inherited CARD9 deficiency. N Engl J Med. (2013) 369:1704–14. 10.1056/NEJMoa1208487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Okada S, Puel A, Casanova J-L, Kobayashi M. Chronic mucocutaneous candidiasis disease associated with inborn errors of IL-17 immunity. Clin Transl Immunol. (2016) 5:e114. 10.1038/cti.2016.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abu-Gazala M, Engel A, Stern A, Guralnik L. An unusual case of nocardiosis presented as a mediastinal mass in an immunocompetent patient. Am J Respir Crit Care Med. (2014) 189:492–3. 10.1164/rccm.201308-1546LE [DOI] [PubMed] [Google Scholar]
- 34.Agrawal SM, Raut SS. Primary cutaneous disease due to Nocardia asteroides in an immunocompetent host. Ind J Pathol Microbiol. (2011) 54:185–6. 10.4103/0377-4929.77399 [DOI] [PubMed] [Google Scholar]
- 35.Al Soub H, Almaslamani M, Al Khuwaiter J, El Deeb Y, Abu Khatab M. Primary Nocardia meningitis in a patient without a predisposing condition: case report and review of the literature. Scand J Infect Dis. (2007) 39:737–41. 10.1080/00365540701199873 [DOI] [PubMed] [Google Scholar]
- 36.Al Tawfiq JA, Mayman T, Memish ZA. Nocardia abscessus brain abscess in an immunocompetent host. J Infect Public Health. (2013) 6:158–61. 10.1016/j.jiph.2012.11.012 [DOI] [PubMed] [Google Scholar]
- 37.Alavi Darazam I, Shamaei M, Mobarhan M, Ghasemi S, Tabarsi P, Motavasseli M, et al. Nocardiosis: risk factors, clinical characteristics and outcome. Iran Red Cresc Med J. (2013) 15:436–9. 10.5812/ircmj.2384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alp E, Yildiz O, Aygen B, Sumerkan B, Sari I, Koc K, et al. Disseminated nocardiosis due to unusual species: two case reports. Scand J Infect Dis. (2006) 38:545–8. 10.1080/00365540500532860 [DOI] [PubMed] [Google Scholar]
- 39.Amatya R, Koirala R, Khanal B, Dhakal S. Nocardia brasiliensis primary pulmonary nocardiosis with subcutaneous involvement in an immunocompetent patient. Ind J Med Microbiol. (2011) 29:68–70. 10.4103/0255-0857.76530 [DOI] [PubMed] [Google Scholar]
- 40.Ameen M, Vargas F, Arenas R, Mercado E. V. del. Successful treatment of Nocardia actinomycetoma with meropenem and amikacin combination therapy. Int J Dermatol. (2011) 50: 443–5. 10.1111/j.1365-4632.2010.04748.x [DOI] [PubMed] [Google Scholar]
- 41.Aozasa N, Kiso M, Kaneko T. Primary lymphocutaneous nocardiosis due to Nocardia brasiliensis which was successfully treated with only oral potassium iodide. J Dermatol. (2011) 38:826–8. 10.1111/j.1346-8138.2010.01074.x [DOI] [PubMed] [Google Scholar]
- 42.Arenas R, Ameen M. Giant grains of Nocardia actinomycetoma. Lancet Infect Dis. (2010) 10:66. 10.1016/S1473-3099(09)70347-0 [DOI] [PubMed] [Google Scholar]
- 43.Arias-Miranda IM, Nuno-Mateo FJ, Viejo De La Guerra G, Garcia-Alcalde ML. Nocardiosis. Enferm Infec Microbiol Clin. (2005) 23:637–38. 10.1016/S0213-005X(05)75050-3 [DOI] [PubMed] [Google Scholar]
- 44.Asmar BI, Bashour BN. Septic arthritis due to nocardia asteroides. South Med J. (1991) 84:933–4. 10.1097/00007611-199107000-00032 [DOI] [PubMed] [Google Scholar]
- 45.Astudillo L, Dahan S, Escourrou G, Sailler L, Carreiro M, Ollier S, et al. Cat scratch responsible for primary cutaneous Nocardia asteroides in an immunocompetent patient. Br J Dermatol. (2001) 145:684–5. 10.1046/j.1365-2133.2001.04447.x [DOI] [PubMed] [Google Scholar]
- 46.Babayigit A, Olmez D, Sozmen SC, Makay B, Uzuner N, Karaman O, et al. Infection caused by Nocardia farcinica mimicking pulmonary metastasis in an adolescent girl. Pediatric Emerg Care. (2010) 26:203–5. Retrieved from: https://journals.lww.com/peconline/Fulltext/2010/03000/Infection_Caused_by_Nocardia_farcinica_Mimicking.7.aspx [DOI] [PubMed] [Google Scholar]
- 47.Baghdadlian H, Sorger S, Knowles K, McNeil M, Brown J. Nocardia transvalensis pneumonia in a child. Pediatr Infect Dis J. (1989) 8:470–1. 10.1097/00006454-198907000-00012 [DOI] [PubMed] [Google Scholar]
- 48.Bajracharya L, Gurung R. A case of nocardia keratitis treated successfully with topical amikacin. Nepal J Ophthal. (2012) 4:170–3. 10.3126/nepjoph.v4i1.5870 [DOI] [PubMed] [Google Scholar]
- 49.Banashankari GS, Rudresh HK, Sreeja S, Beena. Nocardial mycetoma: reinfection with a different species at an unusual site - a rare case. Ind J Pathol Microbiol. (2013) 56: 333–334. 10.4103/0377-4929.120424 [DOI] [PubMed] [Google Scholar]
- 50.Bandeira ID, Guimaraes-Silva P, Cedro-Filho RL, de Almeida VRP, Bittencourt AL, Brites C. Primary cutaneous nocardiosis. J Deutschen Dermatol. (2019) 17:327–9. 10.1111/ddg.13770 [DOI] [PubMed] [Google Scholar]
- 51.Baraboutis IG, Argyropoulou A, Papastamopoulos V, Psaroudaki Z, Paniara O, Skoutelis AT. Primary sternal osteomyelitis caused by Nocardia nova: case report and literature review. Brazil J Infect Dis. (2008) 12:257–9. 10.1590/S1413-86702008000300018 [DOI] [PubMed] [Google Scholar]
- 52.Barbara Gomila S, Susana Sabater V, Jesus Merino P, Rafael Igual A, Rosario Moreno M. Absceso cerebral por Nocardia nova. Rev Chil Infectol. (2012) 29:112–3. 10.4067/S0716-10182012000100019 [DOI] [PubMed] [Google Scholar]
- 53.Baroni MR, Norona M, Ronchi S, Mayoral C. Necrotizing lymphadenitis caused by Nocardia asteroides in a healthy girl. Rev Argen Microbiol. (2004) 36:75–7. [PubMed] [Google Scholar]
- 54.Battista AJ, Huysman J, Cunha BA. Nocardia brasiliensis leg ulcer in a child. Pediatr Infect Dis J. (1990) 9:370–1. 10.1097/00006454-199005000-00014 [DOI] [PubMed] [Google Scholar]
- 55.Behaegel J, Ni Dhubhghaill S, Koppen C. Diagnostic challenges in nocardia keratitis. Eye Contact Lens. (2018) 44:S370–2. 10.1097/ICL.0000000000000462 [DOI] [PubMed] [Google Scholar]
- 56.Benes J, Viechova J, Picha D, Horova B, Zatloukal P. Disseminated Nocardia asteroides infection in an immunocompetent woman following an arm injury. Infection. (2003) 31:112–4. 10.1007/s15010-003-3073-x [DOI] [PubMed] [Google Scholar]
- 57.Bernal E, Ahmad N, Lopez P, Gutierrez F. Sindrome linfocutaneo por Nocardia brasiliensis en una paciente inmunocompetente. Enferm Infec Microbiol Clin. (2008) 26:58–60. 10.1157/13114398 [DOI] [PubMed] [Google Scholar]
- 58.Beuret F, Schmitt E, Planel S, Lesanne G, Bracard S. Subtentorial cerebral nocardiosis in immunocompetent patients: CT and MR imaging findings. Diag Intervent Imag. (2015) 96:953–7. 10.1016/j.diii.2015.03.010 [DOI] [PubMed] [Google Scholar]
- 59.Bharathi MJ, Ramakrishnan R, Meenakshi R, Vasu S. Nocardia asteroides canaliculitis: a case report of uncommon aetiology. Ind J Med Microbiol. (2004) 22:123–5. [PubMed] [Google Scholar]
- 60.Bhusal B, Kumar A, Prajna MV, Srinivasan M. Nocardia keratitis following penetrating corneal injury treated with topical ampicillin. Nepal J Ophthalmol. (2016) 8:82–6. 10.3126/nepjoph.v8i1.16143 [DOI] [PubMed] [Google Scholar]
- 61.Bonifaz A, Flores P, Saul A, Carrasco-Gerard E, Ponce RM. Treatment of actinomycetoma due to Nocardia spp. with amoxicillin–clavulanate. Br J Dermatol. (2007) 156:308–11. 10.1111/j.1365-2133.2006.07557.x [DOI] [PubMed] [Google Scholar]
- 62.Bonifaz Alexandro, Espinosa-Diaz S, Argaez J, Hernandez-Castro R, Xicohtencatl-Cortes J, et al. Actinomycetoma due to Nocardia brasiliensis with extension to the ovaries. Euro J Obstet Gynecol. Reprod Biol. (2017) 211:224–5. 10.1016/j.ejogrb.2017.02.023 [DOI] [PubMed] [Google Scholar]
- 63.Bonifaz Alexandro, Ibarra G, Saul A, Paredes-Solis V, Carrasco-Gerard E, et al. Mycetoma in children: experience with 15 cases. Pediatr Infect Dis J. (2007) 26. Retrieved from: https://journals.lww.com/pidj/fulltext/2007/01000/mycetoma_in_children__experience_with_15_cases.11.aspx [DOI] [PubMed]
- 64.Borm W, Gleixner M. Nocardia brain abscess misinterpreted as cerebral infarction. J Clin Neurosci. (2003) 10:130–2. 10.1016/S0967-5868(02)00121-2 [DOI] [PubMed] [Google Scholar]
- 65.Bosamiya SS, Vaishnani JB, Momin AM. Sporotrichoid nocardiosis with cutaneous dissemination. Ind J Dermatol Venereol Leprol. (2011) 77:535. 10.4103/0378-6323.82409 [DOI] [PubMed] [Google Scholar]
- 66.Bottei E, Flaherty JP, Kaplan LJ, Duffee-Kerr L. Lymphocutaneous Nocardia brasiliensis infection transmitted via a cat scratch: a second case. Clin Infect Dis. (1994) 18:649–50. 10.1093/clinids/18.4.649 [DOI] [PubMed] [Google Scholar]
- 67.Brannan PA, Kersten RC, Hudak DT, Anderson HK, Kulwin DR. Primary Nocardia brasiliensis of the eyelid. Am J Ophthalmol. (2004) 138:498–9. 10.1016/j.ajo.2004.04.020 [DOI] [PubMed] [Google Scholar]
- 68.Brecker SJ, Pugey CD. Nocardia asteroides infection of the cauda equina. J Neurol Neurosurg Psychiatry. (1988) 51:309–11. 10.1136/jnnp.51.2.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cakir E, Buyukpinarbasili N, Ziyade S, Selcuk-Duru HN, Bilgin M, Topuz U. Endobronchial nocardiosis in an 11-year-old child. Pediatric Pulmonol. (2013) 48:1144–7. 10.1002/ppul.22740 [DOI] [PubMed] [Google Scholar]
- 70.Cassir N, Million M, Noudel R, Drancourt M, Brouqui P. Sulfonamide resistance in a disseminated infection caused by Nocardia wallacei: a case report. J Med Case Rep. (2013) 7:103. 10.1186/1752-1947-7-103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Castro JG, Espinoza L. Nocardia species infections in a large county hospital in Miami: 6 years experience. J Infect. (2007) 54:358–61. 10.1016/j.jinf.2006.08.003 [DOI] [PubMed] [Google Scholar]
- 72.Casty FE, Wencel M. Endobronchial nocardiosis. Euro Resp J. (1994) 7:1903–5. [DOI] [PubMed] [Google Scholar]
- 73.Chang P, Logemann H. Mini-mycetoma due to Nocardia brasiliensis. Int J Dermatol. (1992) 31:180–1. 10.1111/j.1365-4362.1992.tb03929.x [DOI] [PubMed] [Google Scholar]
- 74.Chawla K, Mukhopadhayay C, Shetty PV. First report of submandibular and parotid abscess due to Nocardia asteroides. Brazil J Infect Dis. (2010) 14:544–5. 10.1016/S1413-8670(10)70108-2 [DOI] [PubMed] [Google Scholar]
- 75.Chedid MBF, Chedid MF, Porto NS, Severo CB, Severo LC. Nocardial infections: report of 22 cases. Rev Instit Med Trop Sao Paulo. (2007) 49:239–46. 10.1590/s0036-46652007000400009 [DOI] [PubMed] [Google Scholar]
- 76.Chen K-W, Lu C-W, Huang T-C-F, Liau Y-L, Lin J-F, Li S-Y, et al. Cutaneous manifestations of Nocardia brasiliensis infection in Taiwan during 2002–2012— clinical studies and molecular typing of pathogen by gyrB and 16S gene sequencing. Diagn Microbiol Infect Dis. (2013) 77:74–8. 10.1016/j.diagmicrobio.2013.05.008 [DOI] [PubMed] [Google Scholar]
- 77.Chen N, Qin Q, Sun K-D, Luo D, Cheng Q-H. An unusual successful treatment with non-sulfonamides: primary cutaneous nocardiosis caused by Nocardia brasiliensis. Therap Clin Risk Manag. (2018) 14:1661–4. 10.2147/TCRM.S169239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen Y-C, Lee C-H, Chien C-C, Chao T-L, Lin W-C, Liu J-W, et al. Pulmonary nocardiosis in southern Taiwan. J Microbiol Immunol Infect. (2013) 46:441–7. 10.1016/j.jmii.2012.07.017 [DOI] [PubMed] [Google Scholar]
- 79.Chung YL, Park JC, Takatori K, Lee KH. Primary cutaneous nocardiosis mimicking lupus erythematosus. Br J Dermatol. (2001) 144:639–41. 10.1046/j.1365-2133.2001.04110.x [DOI] [PubMed] [Google Scholar]
- 80.Comellas J, Morales M, Granell F. Nodular lymphangitis caused by Nocardia asteroides. Enferm Infec Microbiol Clin. (2000) 18:385–8. [PubMed] [Google Scholar]
- 81.Cooper CJ, Said S, Popp M, Alkhateeb H, Rodriguez C, Aguilar MP, et al. A complicated case of an immunocompetent patient with disseminated nocardiosis. Infect Dis Rep. (2014) 6:5327. 10.4081/idr.2014.5327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Crozier JA, Andhavarapu S, Brumble LM, Sher T. First report of Nocardia beijingensis infection in an immunocompetent host in the United States. J Clin Microbiol. (2014) 52:2730–2. 10.1128/JCM.00588-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.De La Iglesia P, Viejo G, Gomez B, De Miguel D, Del Valle A, Otero L. Fatal pulmonary Nocardia farcinica infection. J Clin Microbiol. (2002) 40:1098–9. 10.1128/JCM.40.3.1098-1099.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Debieuvre D, Dalphin JC, Jacoulet P, Breton JL, Boiron P, Depierre A. Disseminated infection due to an unusual strain of Nocardia farcinica. Rev Mal Respir. (1993) 10:356–8. [PubMed] [Google Scholar]
- 85.Denk PO, Thanos S, Thiel HJ. Amikacin may be drug of choice in Nocardia keratitis. Br J Ophthal. (1996) 80:928–9. 10.1136/bjo.80.10.928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Derancourt C, Theodose R, Deschamps L, Liautaud B, Briand E, Derancourt S, et al. Primary cutaneous nocardiosis caused by Nocardia beijingensis. Br J Dermatol. (2012) 167:216–8. 10.1111/j.1365-2133.2012.10832.x [DOI] [PubMed] [Google Scholar]
- 87.Dias M, Nagarathna S, Mahadevan A, Chandramouli B, Chandramuki A. Nocardial brain abscess in an immunocompetent host. Ind J Med Microbiol. (2008) 26:274–7. 10.4103/0255-0857.42052 [DOI] [PubMed] [Google Scholar]
- 88.Dikensoy O, Filiz A, Bayram N, Balci I, Zer Y, Celik G, et al. First report of pulmonary Nocardia otitidiscaviarum infection in an immunocompetent patient from Turkey. Int J Clin Pract. (2004) 58:210–3. 10.1111/j.1368-5031.2004.0133.x [DOI] [PubMed] [Google Scholar]
- 89.Dinulos JG, Darmstadt GL, Wilson CB, Krengel WFIII, Burns JL. Nocardia asteroides septic arthritis in a healthy child. Pediatr Infect Dis J. (1999) 18:308–10. 10.1097/00006454-199903000-00026 [DOI] [PubMed] [Google Scholar]
- 90.Dominguez DC, Antony SJ. Actinomyces and nocardia infections in immunocompromised and nonimmunocompromised patients. J Natl Med Assoc. (1999) 91:35–9. [PMC free article] [PubMed] [Google Scholar]
- 91.Douglas RM, Grove DI, Elliott J, Looke DFM, Jordan AS. Corneal ulceration due to Nocardia asteroides. Austr. N Zeal J Ophthal. (1991) 19:317–20. 10.1111/j.1442-9071.1991.tb00679.x [DOI] [PubMed] [Google Scholar]
- 92.Duran E, Soledad Salvo M, Gil J, Cachon R. Nocardiosis linfocutanea por Nocardia brasiliensis en un paciente inmunocompetente. Med Clin. (2009) 132:404–5. 10.1016/j.medcli.2008.09.006 [DOI] [PubMed] [Google Scholar]
- 93.Eggink CA, Wesseling P, Boiron P, Meis JF. Severe keratitis due to Nocardia farcinica. J Clin Microbiol. (1997) 35:999–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Epelboin L, Woessner J, Roussin C, Benoit-Cattin T, Noca P, Godefroy C, et al. Actinomycetome du genou a Nocardia otitidiscaviarum aux Comores. Annal Dermatol Venereol. (2013) 140:287–90. 10.1016/j.annder.2013.01.426 [DOI] [PubMed] [Google Scholar]
- 95.Eren E, Ulu-Kilic A, Atalay A, Demiraslan H, Parkan O, Koc N. Report of an immunocompetent case with disseminated infection due to Nocardia otitidiscaviarum: identification by 16S rRNA gene sequencing. Infez Med. (2016) 24:71–6. [PubMed] [Google Scholar]
- 96.Estrada-Chavez GE, Estrada R, Fernandez R, Arenas R, Reyes A, Guevara C, et al. Cervical and middle dorsal actinomycetomas from Guerrero State, Mexico. Int J Dermatol. (2017) 56:1146–9. 10.1111/ijd.13775 [DOI] [PubMed] [Google Scholar]
- 97.Faccini-Martinez AA, Zanotti RL, Moraes MS, Falqueto A. Nodular lymphangitis syndrome. Am J Trop Med Hygiene. (2017) 97:1282–4. 10.4269/ajtmh.17-0397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Farina C, Boiron P, Ferrari I, Provost F, Goglio A. Report of human nocardiosis in Italy between 1993 and 1997. Euro J Epidemiol. (2001) 17:1019–22. 10.1023/A:1020010826300 [DOI] [PubMed] [Google Scholar]
- 99.Farina Claudio, Andrini L, Bruno G, Sarti M, Francoise Tripodi M, et al. Nocardia brasiliensis in Italy: a nine-year experience. Scand J Infect Dis. (2007) 39:969–74. 10.1080/00365540701466124 [DOI] [PubMed] [Google Scholar]
- 100.Farina Claudio, Boiron P, Goglio A, Provost F. Human nocardiosis in Northern Italy from 1982 to 1992. Scand J Infect Dis. (1995) 27:23–7. 10.3109/00365549509018968 [DOI] [PubMed] [Google Scholar]
- 101.Farran Y, Antony S. Nocardia abscessus-related intracranial aneurysm of the internal carotid artery with associated brain abscess: a case report and review of the literature. J Infect Public Health. (2016) 9:358–61. 10.1016/j.jiph.2015.11.009 [DOI] [PubMed] [Google Scholar]
- 102.Fergie JE, Purcell K. Nocardiosis in South Texas children. Pediatr Infect Dis J. (2001) 20. Retrieved from: https://journals.lww.com/pidj/Fulltext/2001/07000/Nocardiosis_in_South_Texas_children.15.aspx [DOI] [PubMed]
- 103.Figgis PA, Glanville AR, Harkness JL. Nocardia asteroides pneumonia with bacteraemia. Med J Austr. (2003) 179:171–2. 10.5694/j.1326-5377.2003.tb05481.x [DOI] [PubMed] [Google Scholar]
- 104.Fleetwood IG, Embil JM, Ross IB. Nocardia asteroides cerebral abscess in immunocompetent hosts: report of three cases and review of surgical recommendations. Surg Neurol. (2000) 53:605–10. 10.1016/S0090-3019(00)00242-1 [DOI] [PubMed] [Google Scholar]
- 105.Flores Gonzalez L, Carballo MG, Munoz E, Dionisio de Cabalier ME. Localized nocardiosis. Rev Facul Cienc Med. (1999) 56:105–11. [PubMed] [Google Scholar]
- 106.Freiberg AA, Herzenberg JE, Sangeorzan JA. Thorn synovitis of the knee joint with Nocardia pyarthrosis. Clin Orthop Relat Res. (1993) 287:233–6. 10.1097/00003086-199302000-00037 [DOI] [PubMed] [Google Scholar]
- 107.Freland C, Fur JL, Nemirovsky-Trebucq B, Lelong P, Boiron P. Primary cutaneous nocardiosis caused by Nocardia otitidiscaviarum: two cases and a review of the literature. J Trop Med Hyg. (1995) 98:395–403. [PubMed] [Google Scholar]
- 108.Frickmann H, Jungblut S, Bargon J, Boddinghaus B. Pneumonia induced by nocardia - a case report. Pneumologie. (2004) 58:850–3. 10.1055/s-2004-830099 [DOI] [PubMed] [Google Scholar]
- 109.Fukuda H, Saotome A, Usami N, Urushibata O, Mukai H. Lymphocutaneous type of nocardiosis caused by Nocardia brasiliensis: a case report and review of primary cutaneous nocardiosis caused by N. brasiliensis reported in Japan. J Dermatol. 35:346–53. 10.1111/j.1346-8138.2008.00482.x [DOI] [PubMed] [Google Scholar]
- 110.Gadelha VdB, Nascimento FA, Fiamoncini VK, Freitas S, Augusto Da J, Freitas S, et al. Teaching neuroimages: the tetraplegic gardener: a case of CNS nocardiosis in an immunocompetent patient. Neurology. (2019) 92:e2840–1. 10.1212/WNL.0000000000007663 [DOI] [PubMed] [Google Scholar]
- 111.Georghiou PR, Blacklock ZM. Infection with Nocardia species in Queensland: a review of 102 clinical isolates. Med J Aust. (1992) 156:692–7. 10.5694/j.1326-5377.1992.tb121509.x [DOI] [PubMed] [Google Scholar]
- 112.Gieger A, Waller S, Pasternak J. Nocardia arthritidis keratitis: case report and review of the literature. Nepal J Ophthal. (2017) 9:91–4. 10.3126/nepjoph.v9i1.17543 [DOI] [PubMed] [Google Scholar]
- 113.Gonzalez A, Fakhar K, Gubernick D, Tuli S. Scleritis caused by in vitro linezolid-resistant Nocardia asteroides. Case Rep Ophthalmol Med. (2014) 2014:326957. 10.1155/2014/326957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Grau Perez M, Casabella Pernas A, de la Rosa del Rey Mdel P, Torrado Gonzalez R. Primary cutaneous nocardiosis: a pitfall in the diagnosis of skin infection. Infection. (2017) 45:927–8. 10.1007/s15010-017-1033-0 [DOI] [PubMed] [Google Scholar]
- 115.Gudivada V, Gochhait D, Bhandary C, Mishra N, Siddaraju N. Cutaneous nocardiosis with discharging sinus clinically mimicking tuberculosis diagnosed by cytology. Diagn Cytopathol. (2019) 47:935–8. 10.1002/dc.24217 [DOI] [PubMed] [Google Scholar]
- 116.Gugnani HC, Sehgal VN, Singh VK, Boiron P, Kumar S. 'Nocardia asteroides' mycetoma of the foot. J Euro Acad Dermatol Venereol. (2002) 16:640–2. 10.1046/j.1468-3083.2002.00653_3.x [DOI] [PubMed] [Google Scholar]
- 117.Guiral J, Refolio C, Carrero P, Carbajosa S. Sacral osteomyelitis due to Nocardia asteroids. Acta Orthop. (1991) 62:389–90. 10.3109/17453679108994479 [DOI] [PubMed] [Google Scholar]
- 118.Gyotoku T, Kayashima K, Nishimoto K, Ono T. Cutaneous nocardiosis developing around gravel inserted during a traffic injury. J Dermatol. (2002) 29:803–9. 10.1111/j.1346-8138.2002.tb00227.x [DOI] [PubMed] [Google Scholar]
- 119.Hachisuka H, Ichiki M, Yoshida N, Nakano S, Sasai Y. Primary subcutaneous abscess caused by Nocardia otitidiscaviarum. J Am Acad Dermatol. (1989) 21:137–9. 10.1016/S0190-9622(89)80355-X [DOI] [PubMed] [Google Scholar]
- 120.Hannemann J, Dalitz M, Hell W, Lebeau A, Busch D, Dalhoff K. Generalized nocardiosis with meningoencephalitis in a nonimmunosuppressed female patient. Dtsch Med Wochenschr. (1993) 118:1281–6. [DOI] [PubMed] [Google Scholar]
- 121.Harth Y, Friedman-Birnbaum R, Lefler E, Bergman R. Two patients with simultaneous, unusually located primary cutaneous nocardiosis. J Am Acad Dermatol. (1992) 26:132–3. 10.1016/S0190-9622(08)80531-2 [DOI] [PubMed] [Google Scholar]
- 122.Hernandez-Bel P, Mayorga J, Elva Perez M. Actinomicetoma por Nocardia brasiliensis. Anal Pediatria. (2010). 10.1016/j.anpedi.2010.02.021 [DOI] [PubMed] [Google Scholar]
- 123.Hironaga M, Mochizuki T, Watanabe S. Acute primary cutaneous nocardiosis. J Am Acad Dermatol. (1990) 23(2 Pt 2):399–400. [DOI] [PubMed] [Google Scholar]
- 124.Hisatsugu K, Shigeru H, Makoto M, Iwao Y, Kazuaki Y, Takashi M. A case report of nocardiosis at the cauda equina. J Orthop Sci. (2015) 20:434–8. 10.1007/s00776-013-0460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hong SB, Han K, Son BR, Shin KS, Rim BC. First case of Nocardia nova spinal abscess in an immunocompetent patient. Brazil J Infect Dis. (2012) 16:196–9. 10.1016/S1413-8670(12)70306-9 [DOI] [PubMed] [Google Scholar]
- 126.Hope W, Looke D. Sequential infection with Nocardia farcinica and Cryptococcus neoformans var. gattii in an immunocompetent host. J Inf . (2003) 47:256–9. 10.1016/S0163-4453(03)00083-5 [DOI] [PubMed] [Google Scholar]
- 127.Hornef MW, Gandorfer A, Heesemann J, Roggenkamp A. Humoral response in a patient with cutaneous nocardiosis. Dermatology. (2000) 200:78–80. 10.1159/000018325 [DOI] [PubMed] [Google Scholar]
- 128.Hunter LR, Krinsky AH, Fleener CH. Preseptal cellulitis caused by Nocardia brasiliensis. Am J Ophthalmol. (1992) 114:373–4. 10.1016/S0002-9394(14)71812-4 [DOI] [PubMed] [Google Scholar]
- 129.Ichinomiya A, Nishimura K, Takenaka M, Utani A, Nishimoto K. Mycetoma caused by Nocardia transvalensis with repeated local recurrences for 25 years without dissemination to viscera. J Dermatol. (2014) 41:556–7. 10.1111/1346-8138.12496 [DOI] [PubMed] [Google Scholar]
- 130.Igbaseimokumo U, El Shafie S, Al Khal AL. First human infection of Nocardia crassostreae in an immunocompetent patient. Chin Med J. (2016) 129:114–5. 10.4103/0366-6999.172609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Inamadar AC, Palit A. Primary cutaneous nocardiosis: a case study and review. Ind J Dermatol Venereol Leprol. (2003) 69:386–91. [PubMed] [Google Scholar]
- 132.Ingole KV, Fule RP, Jalgaonkar SV. Primary cutaneous disease due to Nocardia asteriodes–a case report. Ind J Med Sci. (1995) 49:231–2. [PubMed] [Google Scholar]
- 133.Ishihara M, Takada D, Sugimoto K, Oguro H, Gonoi T, Akiyama Y, et al. Primary brain abscess caused by Nocardia otitidiscaviarum. Intern Med. (2014) 53:2007–12. 10.2169/internalmedicine.53.1450 [DOI] [PubMed] [Google Scholar]
- 134.Jansen C, Frenay HME, Vandertop WP, Visser MR. Intracerebral Nocardia asteroides abscess treated by neurosurgical aspiration and combined therapy with sulfadiazine and cefotaxime. Clin Neurol Neurosurg. (1991) 93:253–5. 10.1016/S0303-8467(05)80015-0 [DOI] [PubMed] [Google Scholar]
- 135.Jiang S, Jiang G, Lei TC. Primary cutaneous nocardiosis. J Coll Phys Surg Pakistan. (2014) 24(Suppl 3):S176–7. 10.1001/jama.242.4.333 [DOI] [PubMed] [Google Scholar]
- 136.Jiang Y, Huang A, Fang Q. Disseminated nocardiosis caused by Nocardia otitidiscaviarum in an immunocompetent host: a case report and literature review. Exp Therap Med. (2016) 12:3339–46. 10.3892/etm.2016.3755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Jimenez-Gallo D, Albarran-Planelles C, Galan-Sanchez F, Linares-Barrios M, Giron-Gonzalez JA. Nocardiosis cutanea primaria por Nocardia farcinica. Rev Clin Espan. (2012) 212:e49–51. 10.1016/j.rce.2012.02.015 [DOI] [PubMed] [Google Scholar]
- 138.Johansson B, Fagerholm P, Petranyi G, Claesson Armitage M, Lagali N. Diagnostic and therapeutic challenges in a case of amikacin-resistant Nocardia keratitis. Acta Ophthalmol. (2017) 95:103–5. 10.1111/aos.13182 [DOI] [PubMed] [Google Scholar]
- 139.Johnson P, Ammar H. Nocardia brasiliensis vertebral osteomyelitis and epidural abscess. BMJ Case Rep. (2013) 2013:bcr2012008400. 10.1136/bcr-2012-008400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kalavathy CM, Parmar P, Ramalingam MDK, Kaliamurthy J, Jesudasan CAN, Thomas PA. Trimethoprim–sulphamethoxazole therapy in Nocardia keratitis. Clin Exp Ophthal. (2004) 32:424–8. 10.1111/j.1442-9071.2004.00816.x [DOI] [PubMed] [Google Scholar]
- 141.Kamyab A, Fakhoury JDJ, Sutkowski R, Drelichman E, Jacobs MJ. Fulminant colitis secondary to nocardiosis. Int J Color Dis. (2012) 27:841–2. 10.1007/s00384-011-1327-0 [DOI] [PubMed] [Google Scholar]
- 142.Kandasamy J, Iqbal HJ, Cooke RPD, Eldridge PR. Primary Nocardia farcinica brain abscess with secondary meningitis and ventriculitis in an immunocompetent patient, successfully treated with moxifloxacin. Acta Neurochir. (2008) 150:505–6. 10.1007/s00701-008-1578-x [DOI] [PubMed] [Google Scholar]
- 143.Kapur N, Adib N, Grimwood K. Nocardia brasiliensis infection mimicking juvenile idiopathic arthritis in a 4-year-old girl. Pediatrics. (2013) 132:e1424–7. 10.1542/peds.2012-3086 [DOI] [PubMed] [Google Scholar]
- 144.Kashyap S, Meel R, Pushker N. Eyelid nocardiosis: an unusual presentation. Ind J Pathol Microbiol. (2010) 53:844–5. 10.4103/0377-4929.72079 [DOI] [PubMed] [Google Scholar]
- 145.Kessler R, Follis F, Daube D, Wernly J. Constrictive pericarditis from Nocardia asteroides infection. Annals Thorac Surg. (1991) 52:861–2. 10.1016/0003-4975(91)91228-N [DOI] [PubMed] [Google Scholar]
- 146.Khadka P, Basnet RB, Rijal BP, Sherchand JB. Pulmonary nocardiosis masquerading renascence of tuberculosis in an immunocompetent host: a case report from Nepal. BMC Res Notes. (2018) 11:488 10.1186/s13104-018-3604-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Khan SNH, Sanche SE, Robinson CA, Pirouzmand F. N. Paucivorans infection presenting as a brain abscess. Canad J Neurol Sci. (2006) 33:426–7. 10.1017/S0317167100005436 [DOI] [PubMed] [Google Scholar]
- 148.Kim J, Kang M, Kim J, Jung S, Park J, Lee D, et al. A case of Nocardia farcinica pneumonia and mediastinitis in an immunocompetent patient. Tuberc Respir Dis. (2016) 79:101–3. 10.4046/trd.2016.79.2.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Kim MS, Choi H, Choi KC, Shin BS. Primary cutaneous nocardiosis due to Nocardia vinacea: first case in an immunocompetent patient. Clin Exp Dermatol. (2011) 36:812–4. 10.1111/j.1365-2230.2011.04090.x [DOI] [PubMed] [Google Scholar]
- 150.Kitamura A, Sakurai T, Tomita K, Fujita T, Miki Y, Nakamura T, et al. A case of primary pulmonary nocardiosis with multiple pulmonary nodules successfully treated with moxifloxacin. J Japan Respir Society. (2009) 47:537–42. [PubMed] [Google Scholar]
- 151.Kranick SM, Zerbe CS. Case report from the NIH clinical center: CNS nocardiosis. J Neurovirol. (2013) 19:505–7. 10.1007/s13365-013-0193-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kresch-Tronik NS, Carrillo-Casas EM, Arenas R, Atoche C, Del Rio-Avila C, Ochoa-Carrera LA, et al. (2013). First case of mycetoma associated with Nocardia takedensis. J Dermatol 40:135–6. 10.1111/1346-8138.12009 [DOI] [PubMed] [Google Scholar]
- 153.Kresch-Tronik NS, Carrillo-Casas EM, Arenas R, Atoche C, Ochoa-Carrera LA, Xicohtencatl-Cortes J, et al. Nocardia harenae, an uncommon causative organism of mycetoma: report on two patients. J Med Microbiol 61(Pt 8):1153–5. 10.1099/jmm.0.042044-0 [DOI] [PubMed] [Google Scholar]
- 154.Kroe DM, Shulman N, Kirsch CM, Wehner JH. An anterior mediastinal mass with draining sternal sinus tracts due to Nocardia braziliensis. West J Med. (1997) 167:47–9. [PMC free article] [PubMed] [Google Scholar]
- 155.Krone A, Schaal KP, Brawanski A, Schuknecht B. Nocardial cerebral abscess cured with imipenem/amikacin and enucleation. Neurosurg Rev. (1989) 12:333–40. [DOI] [PubMed] [Google Scholar]
- 156.Kumar TS, Xavier Scott J, Viswanathan S, Agarwal I, Mohan Raj P, Lalitha MK. Cervicofacial nocardiosis in an immunocompetent child. Acta Paediatr. (2005) 94:1342–3. 10.1111/j.1651-2227.2005.tb02100.x [DOI] [PubMed] [Google Scholar]
- 157.Lake EP, Hughart R, Jones ST, Kreppel A, Tsoukas M, Harrington AT. Cutaneous nocardiosis: a conspicuous eyelid eschar. J Pediatr. (2016) 177:327. 10.1016/j.jpeds.2016.06.084 [DOI] [PubMed] [Google Scholar]
- 158.Laurin JM, Resnik CS, Wheeler D, Needleman BW. Vertebral osteomyelitis caused by Nocardia asteroides: report and review of the literature. J Rheumatol. (1991) 18:455–8. [PubMed] [Google Scholar]
- 159.Lazo Torres AM, Galvez Contreras C, Collado Romacho A, Gamir Ruiz FJ, Yelamos Rodriguez F, Lopez Martinez G. Nocardia endocarditis in a native mitral valve. Rev Espan Cardiol. (2004) 57:787–8. 10.1016/s1885-5857(06)60314-9 [DOI] [PubMed] [Google Scholar]
- 160.Lederman ER, Crum NF. A case series and focused review of nocardiosis: clinical and microbiologic aspects. Medicine. (2004) 83:300–13. 10.1097/01.md.0000141100.30871.39 [DOI] [PubMed] [Google Scholar]
- 161.Lee TG, Jin WJ, Jeong WS, Moon SH, Kwon TG, Lee SK, et al. Primary cutaneous nocardiosis caused by Nocardia takedensis. Annals Dermatol. (2017) 29:471–5. 10.5021/ad.2017.29.4.471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Leitner E, Valentin T, Hoenigl M, Lanz P, Flick H, Zollner-Schwetz I, et al. First report of Nocardia asiatica olecranon bursitis in an immunocompetent traveler returning to Austria. J Clin Microbiol. (2013) 51:2461–2. 10.1128/JCM.00517-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Lewis KE, Ebden P, Wooster SL, Rees J, Harrison GAJ. Multi-system infection with Nocardia farcinica therapy with linezolid and minocycline. J Infect. (2003) 46:199–202. 10.1053/jinf.2002.1122 [DOI] [PubMed] [Google Scholar]
- 164.Lin JC, Ward TP, Belyea DA, McEvoy P, Kramer KK. Treatment of Nocardia asteroides keratitis with polyhexamethylene biguanide. Ophthalmology. (1997) 104:1306–11. 10.1016/S0161-6420(97)30143-2 [DOI] [PubMed] [Google Scholar]
- 165.Lin Y-C, Huang Z-Y, Sun J-R, Yu C-M, Wang C-H. First case report of Nocardia brasiliensis infection causing necrotizing fasciitis in an immunocompetent patient. J Microbiol Immunol Infect. (2016) 49:824–5. 10.1016/j.jmii.2016.03.007 [DOI] [PubMed] [Google Scholar]
- 166.Lohmeyer JA, Machens H-G, Werber K-D. A case of severe cutaneous nocardiosis. J H Surg. (2010) 35:72–3. 10.1177/1753193409344814 [DOI] [PubMed] [Google Scholar]
- 167.Lyos AT, Tuchler RE, Malpica A, Spira M. Primary soft-tissue nocardiosis. Annals Plastic Surg. (1995) 34:212–4. 10.1097/00000637-199502000-00019 [DOI] [PubMed] [Google Scholar]
- 168.Magalhaes GM, De Castro Oliveira SC, De Brito Soares AC, Machado-Pinto J, De Resende MA. Mycetoma caused by Nocardia caviae in the first Brazilian patient. Int J Dermatol. (2010) 49:56–8. 10.1111/j.1365-4632.2009.04263.x [DOI] [PubMed] [Google Scholar]
- 169.Maraki S, Chochlidakis S, Nioti E, Tselentis Y. Primary lymphocutaneous nocardiosis in an immunocompetent patient. Annals Clin Microbiol Antimicrob. (2004) 3:24. 10.1186/1476-0711-3-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Maraki S, Scoulica E, Alpantaki K, Dialynas M, Tselentis Y. Lymphocutaneous nocardiosis due to Nocardia brasiliensis. Diagn Microbiol Infect Dis. (2003) 47:341–4. 10.1016/S0732-8893(03)00090-7 [DOI] [PubMed] [Google Scholar]
- 171.Maraki S, Scoulica E, Nioti E, Tselentis Y. Nocardial infection in crete, Greece: review of fifteen cases from 2003 to 2007. Scand J Infect Dis. (2009) 41:122–7. 10.1080/00365540802651905 [DOI] [PubMed] [Google Scholar]
- 172.Marchandin H, Eden A, Jean-Pierre H, Reynes J, Jumas-Bilak E, Boiron P, et al. Molecular diagnosis of culture-negative cerebral nocardiosis due to Nocardia abscessus. Diagn Microbiol Infect Dis. (2006) 55:237–40. 10.1016/j.diagmicrobio.2006.01.023 [DOI] [PubMed] [Google Scholar]
- 173.Marlowe M, Ali-Ahmad D, Cherrick I, Higgins MJ, Kiska DL, Domachowske JB. Central nervous system Nocardiosis in an immunocompetent child. Pediatr Infect Dis J. (2000) 19:661-−2. 10.1097/00006454-200007000-00019 [DOI] [PubMed] [Google Scholar]
- 174.Martinez RE, Couchel S, Swartz WM, Smith MB. Mycetoma of the hand. J Hand Surg. (1989) 14:909–12. 10.1016/S0363-5023(89)80102-9 [DOI] [PubMed] [Google Scholar]
- 175.Masaki T, Masaki T, Miyamoto H, Ohkusu K, Ezaki T. Nocardia elegans infection involving purulent arthritis in humans. J Infect Chemother. (2012) 18:386–9. 10.1007/s10156-011-0311-5 [DOI] [PubMed] [Google Scholar]
- 176.Matsuo K, Takeuchi M, Kawata N, Nabe M, Okamoto M, Tada S, et al. Pulmonary Nocardia otitidiscaviarum infection in an immunocompetent host. J Japan Respir Society. (2000) 38:844–9. [PubMed] [Google Scholar]
- 177.Mehta RS, Jain D, Chitnis DS. Nocardial abscess of spinal cord [1]. Neurol India. (1999) 47:243–4. [PubMed] [Google Scholar]
- 178.Menendez R, Cordero PJ, Santos M, Gobernado M, Marco V. Pulmonary infection with Nocardia species: a report of 10 cases and review. Euro Respir J. (1997) 10:1542–6. [DOI] [PubMed] [Google Scholar]
- 179.Miguel Noriega L, Gonzalez P, Oddo D, Perez J, Frenkel J, Hurtado F, et al. Disseminated nocardiosis in 3 immunocompetent patients. Rev Med Chile. (1995) 123:1263–9. [PubMed] [Google Scholar]
- 180.Mirza SH, Campbell C. Mycetoma caused by Nocardia transvalensis. J Clin Pathol. (1994) 47:85–6. 10.1136/jcp.47.1.85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Misra AS, Biswas A, Deb P, Dhibar T, Das SK, Roy T. Compressive myelopathy due to nocardiosis from dermal lesion. J Assoc Phys India. (2003) 51:318–21. [PubMed] [Google Scholar]
- 182.Mitja O, Hays R, Van Straten C, Robson J, Koka M, Bassat Q. Mycetoma caused by Nocardia yamanashiensis, Papua New Guinea. Am J Trop Med Hygiene. (2012) 86:1043–5. 10.4269/ajtmh.2012.11-0670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Mittal V, Fernandes M. Cotrimoxazole-resistant Nocardia sclerokeratitis: effective therapy with fourth-generation fluoroquinolones. Can J Ophthalmol. (2012) 47:e58–60. 10.1016/j.jcjo.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 184.Mogilner A, Jallo GI, Zagzag D, Kelly PJ. Nocardia abscess of the choroid plexus: clinical and pathological case report. Neurosurgery. (1998) 43:949–52. 10.1097/00006123-199810000-00130 [DOI] [PubMed] [Google Scholar]
- 185.Mongkolrattanothai K, Ramakrishnan S, Zagardo M, Gray B. Ventriculitis and choroid plexitis caused by multidrug-resistant nocardia pseudobrasiliensis. Pediatr Infect Dis J. (2008) 27:666–8. 10.1097/INF.0b013e31816a43bf [DOI] [PubMed] [Google Scholar]
- 186.Montoya J, Carpenter JL, Holmes GP, Hurley DL, Winn R. Disseminated Nocardia transvalensis Infection with osteomyelitis and multiple brain abscesses. Scand J Infect Dis. (2003) 35:189–96. 10.1080/0036554021000026959 [DOI] [PubMed] [Google Scholar]
- 187.Morita H, Torii M, Yokoyama T, Ebi M, Takakuwa O, Nakamura A, et al. A case of pulmonary nocardiosis with a polypoid lesion in a bronchus. J Japan Respir Soc. (2004) 42:893–6. [PubMed] [Google Scholar]
- 188.Moylett EH, Pacheco SE, Brown-Elliott BA, Perry TR, Buescher ES, Birmingham MC, et al. Clinical experience with linezolid for the treatment of nocardia infection. Clin Infect Dis. (2003) 36:313–8. 10.1086/345907 [DOI] [PubMed] [Google Scholar]
- 189.Mu Y-Z, Liu Y, Wang Y-J, Zhang Z-Z. A case report and review of lymphocutaneous nocardiosis caused by Nocardia brasiliensis reported in China. Dermatol Ther. (2019) 32:e13001. 10.1111/dth.13001 [DOI] [PubMed] [Google Scholar]
- 190.Mufti P, Jamil B. Pneumonia caused by Nocardia caviae in a healthy neonate. J Pak Med Assoc. (1995) 45:272–3. [PubMed] [Google Scholar]
- 191.Mukunda BN, Shekar R, Bass S. Solitary spinal intramedullary abscess caused by Nocardia asteroides. South Med J. (1999) 92:1223–4. 10.1097/00007611-199912000-00020 [DOI] [PubMed] [Google Scholar]
- 192.Munoz-Hernandez B, Noyola MC, Palma-Cortes G, Rosete DP, Galvan MA, Manjarrez ME. Actinomycetoma in Arm disseminated to lung with grains of Nocardia brasiliensis with peripheral filaments. Mycopathologia. (2009) 168:37–40. 10.1007/s11046-009-9189-5 [DOI] [PubMed] [Google Scholar]
- 193.Naguib MT, Fine DP. Brain abscess due to Nocardia brasiliensis hematogenously spread from a pulmonary infection. Clin Infect Dis. (1995) 21:459–60. 10.1093/clinids/21.2.459 [DOI] [PubMed] [Google Scholar]
- 194.Naha K, Dasari S, Vivek G, Prabhu M. Primary abdominal Nocardiosis masquerading as tubercular pelvic inflammatory disease in an immunocompetent individual. BMJ Case Rep. (2013) 2013:bcr2012008076. 10.1136/bcr-2012-008076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Naka W, Miyakawa S, Niizeki H, Fukuda T, Mikami Y, Nishikawa T. Unusually located lymphocutaneous nocardiosis caused by Nocardia brasiliensis. Br J Dermatol. (1995) 132:609–13. 10.1111/j.1365-2133.1995.tb08719.x [DOI] [PubMed] [Google Scholar]
- 196.Nakahara Y, Nakahara Y, Ikegami Y, Ishida T, Ushida S, Mochizuki Y, et al. A case of pulmonary nocardiosis diagnosed by percutaneous aspiration. Japan J Thoracic Dis. (1990) 28:651–5. 10.11389/jjrs1963.28.651 [DOI] [PubMed] [Google Scholar]
- 197.Nalini A, Saini J, Mahadevan A. Central nervous system norcardiosis with granulomatous pachymeningitis and osteomyelitis of skull vault. Ind J Pathol Microbiol. (2014) 57:332–4. 10.4103/0377-4929.134735 [DOI] [PubMed] [Google Scholar]
- 198.Navarrete-Navarrete N, Escobar Sevilla J, Toribio Garcia M, Urbano F, Sabio JM, Jimenez-Alonso J. A man with unilateral endophthalmitis: a case of disseminated nocardiosis. Case Rep Infect Dis. (2015) 2015:607421. 10.1155/2015/607421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Nguyen NM, Sink JR, Carter AJ, Asrani F. Nocardiosis incognito: primary cutaneous nocardiosis with extension to myositis and pleural infection. JAAD Case Rep. (2017) 4:33–5. 10.1016/j.jdcr.2017.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Numata S, Numata T, Gonoi T, Matsunaga K. Successful treatment of primary cutaneous Nocardia brasiliensis infection with oral potassium iodide. J Dermatol. (2016) 43:843–4. 10.1111/1346-8138.13293 [DOI] [PubMed] [Google Scholar]
- 201.Oda R, Sekikawa Y, Hongo I. Primary cutaneous nocardiosis in an immunocompetent patient. Intern Med. (2017) 56:469–70. 10.2169/internalmedicine.56.7810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Ogasawara Y, Takita Y, Hiruma M, Mikami Y, Muto M. Primary cutaneous nocardiosis due to Nocardia brasiliensis in an immunocompetent patient. J Dermatol. (2005) 32:230–2. 10.1111/j.1346-8138.2005.tb00754.x [DOI] [PubMed] [Google Scholar]
- 203.Oshiro S, Ohnishi H, Ohta M, Tsuchimochi H. Intraventricular rupture of nocardia brain abscess. Neurol Med. (2003) 43:360–3. 10.2176/nmc.43.360 [DOI] [PubMed] [Google Scholar]
- 204.Ozgenc O, Avci M, Ari A, Celebi IY, Coşkuner SA. Long-term treatment of persistent disseminated Nocardia cyriacigeorgica infection. Brazil J Infect Dis. (2014) 18:556–60. 10.1016/j.bjid.2014.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Pai S, Pai K, Sharma S. Cutaneous nocardiosis: an underdiagnosed pathogenic infection. BMJ Case Rep. (2015) 2015:bcr2014208713. 10.1136/bcr-2014-208713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Palmieri JR, Santo A, Johnson SE. Soil-acquired cutaneous nocardiosis on the forearm of a healthy male contracted in a swamp in rural eastern Virginia. Int Med Case Rep J. (2014) 7:41–7. 10.2147/IMCRJ.S59315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Pandya VB, Petsoglou C. Nocardia transvalensis resistant to amikacin: an unusual cause of microbial keratitis. Cornea. (2008) 27:1082–5. 10.1097/ICO.0b013e3181783a20 [DOI] [PubMed] [Google Scholar]
- 208.Papaventsis D, Siafakas N, Kondyli L, Akritidou M, Pantazi P, Perdikari E, et al. Nocardia puris endophthalmitis. Ind J Med Microbiol. (2009) 27:168–70. 10.4103/0255-0857.49438 [DOI] [PubMed] [Google Scholar]
- 209.Paredes BE, Hunger RE, Braathen LR, Brand CU. Cutaneous nocardiosis caused by Nocardia brasiliensis after an insect bite. Dermatology. (1999) 198:159–61. 10.1159/000018094 [DOI] [PubMed] [Google Scholar]
- 210.Patel R, Sise A, Al-Mohtaseb Z, Garcia N, Aziz H, Amescua G, et al. Nocardia asteroides keratitis resistant to amikacin. Cornea. (2015) 34:1617–9. 10.1097/ICO.0000000000000634 [DOI] [PubMed] [Google Scholar]
- 211.Patil A, Cherian A, Iype T, Sandeep P. Nocardial brain abscess in an immunocompetent individual. Neurol India. (2011) 59:779–82. 10.4103/0028-3886.86571 [DOI] [PubMed] [Google Scholar]
- 212.Patil SP, Gautam MM, Sodha AA, Khan KJ. Primary cutaneous nocardiosis with craniocerebral extension: a case report. Dermatol Online J. (2009) 15:8. [PubMed] [Google Scholar]
- 213.Philit F, Boibieux A, Coppere B, Reverdy ME, Peyramond D, et al. Nocardia asteroides meningitis without brain abscess in an non-immunodepressed adult. Presse Med. (1994) 23:346. [PubMed] [Google Scholar]
- 214.Pintado V, Gomez-Mampaso E, Meseguer MA, Gonzalez-Palacios F, Yturriaga R. Systemic nocardiosis of fatal outcome in a previously health girl. Enferm Infecc Microbiol Clin. (2000) 18:485–6. [PubMed] [Google Scholar]
- 215.Poland GA, Jorgensen CR, Sarosi GA. Nocardia asteroides pericarditis: report of a case and review of the literature. Mayo Clin Proc. (1990) 65:819–24. 10.1016/S0025-6196(12)62573-7 [DOI] [PubMed] [Google Scholar]
- 216.Provost F, Laurent F, Uzcategui LR, Boiron P. Molecular study of persistence of Nocardia asteroides and Nocardia otitidiscaviarum strains in patients with long-term nocardiosis. J Clin Microbiol. (1997) 35:1157–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Pyatigorskaya N, Brugieres P, Hodel J, Mekontso Dessap A, Gaston A. What is your diagnosis? J Neuroradiol. (2010) 37:192–5. 10.1016/j.neurad.2009.07.007 [DOI] [PubMed] [Google Scholar]
- 218.Rafiei N, Peri AM, Righi E, Harris P, Paterson DL. Central nervous system nocardiosis in Queensland: a report of 20 cases and review of the literature. Med. (2016) 95:e5255. 10.1097/MD.0000000000005255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Rajendran C, Kandhari S. Mycetoma due to nocardia brasiliensis: first case report from the union territory of Delhi: Nocavdia brasiliensis-myzetom: erster fallbericht aus der Delhi-Union. Mycoses. (1989) 32:476–81. 10.1111/j.1439-0507.1989.tb02286.x [DOI] [PubMed] [Google Scholar]
- 220.Ramamoorthi K, Pruthvi BC, Rao NR, Belle J, Chawla K. Pulmonary nocardiosis due to Nocardia otitidiscaviarum in an immunocompetent host- a rare case report. Asian Pac J Trop Med. (2011) 4:414–6. 10.1016/S1995-7645(11)60116-8 [DOI] [PubMed] [Google Scholar]
- 221.Raszka D, Popelka S, Jr, Hert J, Jahoda D, Landor I, Vavrik P. Rare case of osteomyelitis of tibial shaft caused by Nocardia cyriacigeorgica. Folia Microbiol. (2018) 63:525–32. 10.1007/s12223-018-0589-0 [DOI] [PubMed] [Google Scholar]
- 222.Ravage ZB, Singerman LJ. Endogenous Nocardial chorioretinitis in an immunocompetent patient. Ret Cases Brief Rep. (2009) 3:27–30. 10.1097/ICB.0b013e31814fae6f [DOI] [PubMed] [Google Scholar]
- 223.Richards ADM, Stewart C, Karthik H, Lake SR. Bilateral subretinal abscesses: the first case of disseminated Nocardia beijingensis in Australia. Clin Exp Ophthal. (2015) 43:843–5. 10.1111/ceo.12575 [DOI] [PubMed] [Google Scholar]
- 224.Roca B, Merino J. Nocardia brain abscess. Int J Infect Dis. (2010) 3:e383–4. 10.1016/j.ijid.2009.07.015 [DOI] [PubMed] [Google Scholar]
- 225.Rodriguez-Lozano J, Arminanzas Castillo C, Ruiz de Alegria Puig C, Ventosa Ayarza JA, Farinas MC, Aguero J, et al. Post-traumatic endophthalmitis caused by Nocardia nova. JMM Case Rep. (2019) 6:e005175. 10.1099/jmmcr.0.005175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Roquer J, Pou A, Herraiz J, Campodarve I, Sequeira T, Vilato J, et al. Primary cerebral abscess due to nocardia presenting as “ghost tumor”: clinical and pathological study. Euro Neurol. (1990) 30:254–7. 10.1159/000117357 [DOI] [PubMed] [Google Scholar]
- 227.Rosendale DE, Myers C, Boyko EJ, Jafek B. Nocardia asteroides cervical osteomyelitis in an immunocompetent host. Otolaryngology. (1988) 99:334–7. 10.1177/019459988809900313 [DOI] [PubMed] [Google Scholar]
- 228.Roubille F, Maxant G, Serre I, Colson P, Battistella P, Calvet B, et al. -L. Fatal systemic nocardia infection revealed by cardiac tamponade. Intern Med. (2010) 49:135–7. 10.2169/internalmedicine.49.2478 [DOI] [PubMed] [Google Scholar]
- 229.Rush RB. Contact lens-associated nocardial necrotizing scleritis. Korean J Ophthal. (2013) 27:291–3. 10.3341/kjo.2013.27.4.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Saarinen KA, Lestringant GG, Czechowski J, Frossard PM. Cutaneous nocardiosis of the chest wall and pleura - 10-Year consequences of a hand actinomycetoma. Dermatology. (2001) 202:131–3. 10.1159/000051613 [DOI] [PubMed] [Google Scholar]
- 231.Sachs MK. Lymphocutaneous Nocardia brasiliensis infection acquired from a cat scratch: case report and review. Clin Infect Dis. (1992) 15:710–1. 10.1093/clind/15.4.710 [DOI] [PubMed] [Google Scholar]
- 232.Salvo Gonzalo S, Grijalba Uche M, Mazon Ramos A, Vila Mendiburu I. Acute otitis media caused by Nocardia asteroides. Acta Otorrinolaringol Espanola. (1996) 47:314–6. [PubMed] [Google Scholar]
- 233.Saoji VA, Saoji VS, Gadegone RW, Menghani PR. Primary cutaneous nocardiosis. Ind J Dermatol. (2012) 57:404–6. 10.4103/0019-5154.100502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Saraca GD, Towersey L, Hay RJ, Londero AT, Martins EC, Amora AT, et al. Mycetoma by Nocardia asteroides: a 9 year follow-up. Rev Instit Med Trop Sao Paulo. (1993) 35:199–204. 10.1590/S0036-46651993000200013 [DOI] [PubMed] [Google Scholar]
- 235.Schiaroli E, Pasticci MB, de Carolis E, Mello E, Pallotto C, Leli C, et al. Diagnosis of Nocardia paucivorans central nervous system infection by DNA sequencing from paraffin-embedded tissue. Infezioni Med. (2016) 24:147–52. [PubMed] [Google Scholar]
- 236.Schiff TA, Goldman R, Sanchez M, McNeil MM, Brown JM, Klirsfeld D, et al. Primary lymphocutaneous nocardiosis caused by an unusual species of Nocardia: Nocardia transvalensis. J Am Acad Dermatol. (1993) 28:336–40. 10.1016/0190-9622(93)70049-Y [DOI] [PubMed] [Google Scholar]
- 237.Schiff TA, McNeil MM, Brown JM. Cutaneous Nocardia farcinica infection in a nonimmunocompromised patient: case report and review. Clin Infect Dis. (1993) 16:756–60. 10.1093/clind/16.6.756 [DOI] [PubMed] [Google Scholar]
- 238.Schwartz JG, McGough DA, Thorner RE, Fetchick RJ, Tio FO, Rinaldi MG. Primary lymphocutaneous Nocardia brasiliensis infection: three case reports and a review of the literature. Diagn Microbiol Infect Dis. (1988) 10:113–20. 10.1016/0732-8893(88)90049-1 [DOI] [PubMed] [Google Scholar]
- 239.Schwartz JG, Tio FO. Nocardial osteomyelitis: A case report and review of the literature. Diagn Microbiol Infect Dis. (1987) 8:37–46. 10.1016/0732-8893(87)90045-9 [DOI] [PubMed] [Google Scholar]
- 240.Secchin P, Trope BM, Fernandes LA, Barreiros G, Ramos-E-Silva M. Cutaneous Nocardiosis simulating cutaneous lymphatic sporotrichosis. Case Rep Dermatol. (2017) 9:119–29. 10.1159/000471788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Seddon M, Ellis-Pegler RB. Lymphocutaneous Nocardia brasiliensis infection: a case report and review. N Zeal Med J. (1995) 108:385–6. [PubMed] [Google Scholar]
- 242.Senard O, Blanot S, Jouvion G, Rodriguez-Nava V, Lortholary O, Join-Lambert O, et al. Fulminant nocardiosis due to a multidrug-resistant isolate in a 12- year-old immunocompetent child. Pediatrics. (2018) 141:e20163131. 10.1542/peds.2016-3131 [DOI] [PubMed] [Google Scholar]
- 243.Shachor-Meyouhas Y, Ravid S, Suhair H, Kassis I. Primary cutaneous Nocardia brasiliensis cellulitis in immunocompetent child. Harefuah. (2012) 151:476–8. [PubMed] [Google Scholar]
- 244.Shah P, Zhu D, Culbertson WW. Therapeutic femtosecond laser-assisted lamellar keratectomy for multidrug-resistant nocardia keratitis. Cornea. (2017) 36:1429–31. 10.1097/ICO.0000000000001318 [DOI] [PubMed] [Google Scholar]
- 245.Shanbhag NU, Karandikar S, Deshmukkh PA. Disseminated orbital actinomycetoma: a case report. Ind J Ophthal. (2010) 58:60–3. 10.4103/0301-4738.58474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Sharma N, Mahajan V, Agarwal S, Katoch V, Das R, Kashyap M, et al. Nocardial mycetoma: diverse clinical presentations. Ind J Dermatol Venereol Leprol. (2008) 74:635–40. 10.4103/0378-6323.45110 [DOI] [PubMed] [Google Scholar]
- 247.Sheffer S, Shreberk-Hassidim R, Olshtain K, Maly A, Zlotogorski A, Ramot Y. Lymphocutaneous nocardiosis caused by Nocardia brasiliensis in an immunocompetent elderly woman. Int J Dermatol. (2016) 55:e45–7. 10.1111/ijd.12988 [DOI] [PubMed] [Google Scholar]
- 248.Shetty VP, Kannappan O, Sarma YS. Salivary gland nocardiosis in an immunocompetent patient. Asian J Surg. (2011) 34:99–101. 10.1016/S1015-9584(11)60028-6 [DOI] [PubMed] [Google Scholar]
- 249.Shifren JD, Milliken RG. An acute Nocardia brasiliensis infection of the hand: a case report. J Hand Surg. (1996) 21:309–10. 10.1016/S0363-5023(96)80128-6 [DOI] [PubMed] [Google Scholar]
- 250.Shimizu A, Ishikawa O, Nagai Y, Mikami Y, Nishimura K. Primary cutaneous nocardiosis due to Nocardia nova in a healthy woman. Br J Dermatol. (2001) 145:154–6. 10.1046/j.1365-2133.2001.04302.x [DOI] [PubMed] [Google Scholar]
- 251.Shishido H, Deguchi K, Miyake S, Akagawa S, Yoshizawa Y. Multiple drugresistant Nocardia asteroides isolated from a patient with pulmonary nocardiosis. Respir Med. (1998) 92:873–5. 10.1016/S0954-6111(98)90391-2 [DOI] [PubMed] [Google Scholar]
- 252.Shivaprakash MR, Rao P, Mandal J, Biswal M, Gupta S, Ray P, et al. Nocardiosis in a tertiary care hospital in North India and review of patients reported from India. Mycopathologia. (2007) 163:267–74. 10.1007/s11046-007-9011-1 [DOI] [PubMed] [Google Scholar]
- 253.Sikimić S, Nonković Z, Cvetković D. Recurrent abscessing pneumonia caused by Nocardia. Vojnosanitetski Pregled. Military-Med Pharmac Rev. (1998) 55:559–63. [PubMed] [Google Scholar]
- 254.Singh AK, Shukla A, Bajwa R, Agrawal R, Srivastwa N. Pulmonary nocardiosis: unusual presentation in intensive care unit. Ind J Crit Care Med. (2018) 22:125–7. 10.4103/ijccm.IJCCM_472_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Singh S, Verma Y, Pandey P, Singh UB. Granulomatous hepatitis by Nocardia species: an unusual case. Int J Infect Dis. (2019) 81:97–9. 10.1016/j.ijid.2019.01.046 [DOI] [PubMed] [Google Scholar]
- 256.Smit LHM, Leemans R, Overbeek BP. Nocardia farcinica as the causative agent in a primary psoas abscess in a previously healthy cattle inspector. Clin Microbiol Infect. (2003) 9:445–8. 10.1046/j.1469-0691.2003.00576.x [DOI] [PubMed] [Google Scholar]
- 257.Soares D, Reis-Melo A, Ferraz C, Guedes Vaz L. Nocardia lung abscess in an immunocompetent adolescent. BMJ Case Rep. (2019) 12. 10.1136/bcr-2018-227499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Solano-Varela DM, Barrios-Vidales EM, Plaza DF, Riveros WM, Guzman J, Chica CE, et al. Immunocompetent patient with a brain abscess caused by Nocardia beijingensis in Latin America: a case report. Medicine. (2019) 98:e14879. 10.1097/MD.0000000000014879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Sorichetti B, Westerberg BD, Tan R, Kozak FK. Nocardia asteroides sinusitis in a pediatric patient: case report with 20 year follow-up and review of the literature. Int J Pediatr Otorhinol. (2015) 79:1152–4. 10.1016/j.ijporl.2015.04.022 [DOI] [PubMed] [Google Scholar]
- 260.Soto-Mendoza N, Bonifaz A. Head actinomycetoma with a double aetiology, caused by Nocardia brasiliensis and N. asteroides. Br J Dermatol. (2000) 143:192–4. 10.1046/j.1365-2133.2000.03615.x [DOI] [PubMed] [Google Scholar]
- 261.Sousa JMP, Wachholz PA, Sette CS, Marques GF, Barreto JA. Mycetoma caused by Nocardia brasiliensis in an immunocompetent patient. J Deutsc Dermatol Gesellsc. (2014) 12:903–5. 10.1111/ddg.12331 [DOI] [PubMed] [Google Scholar]
- 262.Sridhar MS, Cohen EJ, Rapuano CJ, Lister MA, Laibson PR. Nocardia asteroides sclerokeratitis in a contact lens wearer. CLAO J. (2002) 28:66–8. [PubMed] [Google Scholar]
- 263.Sridhar MS, Sharma S, Garg P, Rao GN. Treatment and outcome of Nocardia keratitis. Cornea. (2001) 20:458–62. 10.1097/00003226-200107000-00003 [DOI] [PubMed] [Google Scholar]
- 264.Stanley MW, Deike M, Knoedler J, Iber C. Pulmonary mycetomas in immunocompetent patients: diagnosis by fine-needle aspiration. Diagn Cytopathol. (1992) 8:577–9. 10.1002/dc.2840080607 [DOI] [PubMed] [Google Scholar]
- 265.Steinmetz G, Panas K, Puffinbarger W. An acute nocardia infection in a pediatric hand. J Hand Surg. (2019) 44:343.e3. 10.1016/j.jhsa.2018.03.039 [DOI] [PubMed] [Google Scholar]
- 266.Suzuki C, Kimura T, Arai A, Maeda T, Tomiyama M, Kannari K, et al. A case of brain nocardiosis successfully treated with minocycline. Brain Nerve. (2006) 58:505–8. [PubMed] [Google Scholar]
- 267.Takayanagi K, Kimura Y, Kawakami K, Koyama K, Harada Y, Yamaryo T. A case of pulmonary nocardiosis with Nocardia beijingensis. J Japan Assoc Infect Dis. (2008) 82:43–6. 10.11150/kansenshogakuzasshi1970.82.43 [DOI] [PubMed] [Google Scholar]
- 268.Taneja J, Sen B, Danc N. Pulmonary nocardiosis mimicking malignancy. Ind J Med Microbiol. (2015) 34:117–8. 10.4103/0255-0857.167680 [DOI] [PubMed] [Google Scholar]
- 269.Tantracheewathorn T, Lolekha S, Tantracheewathorn S. Nocardia pneumonia with empyema thoracis in a healthy neonate: a case report. J Med Assoc Thailand. (2004) 87:438–41. [PubMed] [Google Scholar]
- 270.Tellez I, Franco-Paredes C. A woman with chronic subcutaneous swelling of the right foot associated with sinus tracts discharging yellow grains. PLoS Neglect Trop Dis. (2010) 4:e772. 10.1371/journal.pntd.0000772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Tenorio-Abreu A, Iglesias-Martin J, Breval IZY, Delgado-Garcia C. Keratitis by Nocardia farcinica in an immunocompetent patient. Description of the first case in Spain. Rev Espan Quimioter. (2017) 30:385–7. [PubMed] [Google Scholar]
- 272.Thoms K-M, Zimmermann O, Schupp P, Thoms S, Emmert S. Nocardia otitidiscaviarum: cause of long-term cutaneous abscesses on the leg of an immunocompetent man. Arch Dermatol. (2007) 143:1073–87. 10.1001/archderm.143.8.1086 [DOI] [PubMed] [Google Scholar]
- 273.Tilak R, Agarwal D, Lahiri TK, Tilak V. Pulmonary nocardiosis presenting as fungal ball–a rare entity. J Infect Dev Countries. (2008) 2:143–5. 10.3855/T2.2.143 [DOI] [PubMed] [Google Scholar]
- 274.Townell N, Locke T, Gibbons M, Murphy D, Francis J, Nourse C. Mycetoma in Timor-Leste and first report of nocardiosis. Infect Dis Rep. (2018) 10:7804. 10.4081/idr.2018.7804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Trichet E, Cohen-Bacrie S, Conrath J, Drancourt M, Hoffart L. Nocardia transvalensis keratitis: an emerging pathology among travelers returning from Asia. BMC Infect Dis. (2011) 11:296. 10.1186/1471-2334-11-296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Tseng SH, Chen JJ, Hu FR. Nocardia brasiliensis keratitis successfully treated with therapeutic lamellar keratectomy. Cornea. (1996) 15:165–7. 10.1097/00003226-199603000-00009 [DOI] [PubMed] [Google Scholar]
- 277.Tsushima K, Koizumi T, Aoki H, Furuta K, Fujimoto K, Kubo K. A case of acute respiratory distress syndrome caused by systemic nocardiosis. Respiration. (2000) 67:591–2. 10.1159/000029580 [DOI] [PubMed] [Google Scholar]
- 278.Valarezo J, Cohen J, Valarezo L, Spektor S, Shoshan Y, Rosenthal G, et al. Nocardial cerebral abscess: report of three cases and review of the current neurosurgical management. Neurol Res. (2003) 25:27–30. 10.1179/016164103101201076 [DOI] [PubMed] [Google Scholar]
- 279.Valbuena Alvarez R, Cajide Montero J, Ortiz Cabria R, Santos-Ascarza Tabares L, Rodriguez de la Rua Roman J, de la Rosa Kehrmann M, et al. Acute systemic nocardiosis. Renal abscess. Arch Espan Urol. (1996) 49:529–31. [PubMed] [Google Scholar]
- 280.Vanegas S, Franco-Cendejas R, Cicero A, Lopez-Jacome E, Colin C, Hernandez M. Nocardia brasiliensis-associated femorotibial osteomyelitis. Int J Infect Dis. (2014) 20:63–5. 10.1016/j.ijid.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 281.Varghese GK, Ramani R, Bhat KR, Shivananda PG. Nocardia brasiliensis meningitis. Postgr Med J. (1992) 68:986. 10.1136/pgmj.68.806.986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Vongphoumy I, Dance DAB, Dittrich S, Logan J, Davong V, Rattanavong S, et al. Case report: actinomycetoma caused by Nocardia aobensis from Lao PDR with favourable outcome after short-term antibiotic treatment. PLoS Negl Trop Dis. (2015) 9:e0003729. 10.1371/journal.pntd.0003729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Wada A, Matsuda S, Kubota H, Miura H, Iwamoto Y. Primary lymphocutaneous nocardiosis caused by Nocardia otitidiscaviarum. Hand Surg. (2002) 07:285–7. 10.1142/S021881040200114X [DOI] [PubMed] [Google Scholar]
- 284.Wang A, Xu Q, Wang Y, Liao H. Orbital and intracranial Nocardia farcinica infection caused by trauma to the orbit: a case report. BMC Infect Dis. (2019) 19:953. 10.1186/s12879-019-4605-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Wang R, Yao X, Li R. Mycetoma in China: a case report and review of the literature. Mycopathologia. (2019) 184:327–34. 10.1007/s11046-019-00324-z [DOI] [PubMed] [Google Scholar]
- 286.Wang X, Zhou T, Deng D, Guo Y. A case of cutaneous nocardiosis with involvement of the trachea, anterior mediastinum and sternum. Case Rep Dermatol. (2010) 2:177–82. 10.1159/000321635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Wegerle S, Markus A, Weber N, Steffen H, King B, Eder W, et al. Pulmonary nocardiosis with trimethoprime/sulphamethoxazole-resistant Nocardia paucivorans in a patient with no signs of immunosuppression. Pneumologie. (2007) 61:46–51. 10.1055/s-2006-944276 [DOI] [PubMed] [Google Scholar]
- 288.Welsh O, Salinas-Carmona MC, Brown-Elliott BA, Smith T, Cardenas-De La Garza JA, Wallace RJ, Jr. Disseminated actinomycetoma due to Nocardia wallacei. Int J Dermatol. (2018) 57:580–2. 10.1111/ijd.13909 [DOI] [PubMed] [Google Scholar]
- 289.Williams PJ, Robinson J, Hubbard GB. Bleb-associated exogenous nocardia endophthalmitis. JAMA Ophthal. (2017) 135:e17427. 10.1001/jamaophthalmol.2017.4276 [DOI] [PubMed] [Google Scholar]
- 290.Wongthim S, Charoenlap P, Udompanich V, Punthumchinda K, Suwanagool P. Pulmonary nocardiosis in Chulalongkorn Hospital. J Med Assoc Thailand. (1991) 74:271–7. [PubMed] [Google Scholar]
- 291.Wortman PD. Treatment of a Nocardia brasiliensis mycetoma with sulfamethoxazole and trimethoprim, amikacin, and amoxicillin and clavulanate. Arch Dermatol. (1993) 129:564–7. 10.1001/archderm.1993.01680260032002 [DOI] [PubMed] [Google Scholar]
- 292.Yaşar Z, Acat M, Onaran H, Ozgul MA, Fener N, Talay F, et al. An unusual case of pulmonary nocardiosis in immunocompetent patient. Case Rep Pulmonol. (2014) 2014:963482. 10.1155/2014/963482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Yildiz O, Alp E, Tokgoz B, Tucer B, Aygen B, Sumerkan B, et al. Nocardiosis in a teaching hospital in the Central Anatolia region of Turkey: treatment and outcome. Clin Microbiol Infect. (2005) 11:495–9. 10.1111/j.1469-0691.2005.01145.x [DOI] [PubMed] [Google Scholar]
- 294.Z'Graggen WJ, Bregenzer T, Fankhauser H, Arnoux A, Laeng H, Itin PH. Primary cutaneous nocardiosis in an immune-competent patient. Euro J Dermatol. (2001) 11:569–71. [PubMed] [Google Scholar]
- 295.Zhuang K, Tang J, Ran Y. Image gallery: acute primary cutaneous nocardiosis due to Nocardia brasiliensis. Br J Dermatol. (2017) 176:e97. 10.1111/bjd.15394 [DOI] [PubMed] [Google Scholar]
- 296.Zufferey P, Wenger A, Bille J, Hofstetter JR. Disseminated nocardiosis due to Nocardia brasiliensis in an ambulatory patient. Revue Suisse Med Praxis. (1989) 78:718–21. [PubMed] [Google Scholar]
- 297.Zúñiga M, Hunziker MF, Nico MM, Rivitti EA, Festa-Neto C. Actinomycetoma of the scalp due to Nocardia brasiliensis: case report and review of the literature. Int J Dermatol. (2015) 54:695–8. 10.1111/ijd.12107 [DOI] [PubMed] [Google Scholar]
- 298.Mufti P, Jamil B. Pneumonia caused by nocardia caviae in a healthy neonate. J Pak Med Assoc. (1995) 45:272–3. [PubMed] [Google Scholar]
- 299.Hernandez-Hernandez F, Lopez-Martinez R, Mendez-Tovar LJ, Manzano-Gayosso P. Nocardia brasiliensis: in vitro and in vivo growth response to steroid sex hormones. Mycopathologia. (1995) 132:79–85. 10.1007/BF01103779 [DOI] [PubMed] [Google Scholar]
- 300.Lovett IS Houang ET Burge S Turner-Warwick M Thompson FD Harrison AR . An outbreak of Nocardia asteroides infection in a renal transplant unit. Q J Med. (1981) 50:123–35. 10.1093/oxfordjournals.qjmed.a067675 [DOI] [PubMed] [Google Scholar]
- 301.Houang ET Lovett IS Thompson FD Harrison AR Joekes AM Goodfellow M . Nocardia asteroides infection–a transmissible disease. J Hosp Infect. (1980) 1:31–40. 10.1016/0195-6701(80)90029-8 [DOI] [PubMed] [Google Scholar]
- 302.Sahathevan M, Harvey FA, Forbes G, O'Grady J, Gimson A, Bragman S, et al. Epidemiology, bacteriology and control of an outbreak of Nocardia asteroides infection on a liver unit. J Hosp Infect. (1991) 18(Suppl. A):473–80. 10.1016/0195-6701(91)90059-H [DOI] [PubMed] [Google Scholar]
- 303.Exmelin L, Malbruny B, Vergnaud M, Prosvost F, Boiron P, Morel C. Molecular study of nosocomial nocardiosis outbreak involving heart transplant recipients. J Clin Microbiol. (1996) 34:1014–6. 10.1128/JCM.34.4.1014-1016.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Blumel J, Blumel E, Yassin AF, Schmidt-Rotte H, Schaal KP. Typing of Nocardia farcinica by pulsed-field gel electrophoresis reveals an endemic strain as source of hospital infections. J Clin Microbiol. (1998) 36:118–22. 10.1128/JCM.36.1.118-122.1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Kachi S, Okazaki M, Takeda H, Igarashi H, Kobayashi O, Watanabe H, et al. Outbreak of Nocardia farcinica infection with the same pattern in randomly amplified polymorphic DNA analysis. J Hosp Infect. (2006) 62:502–6. 10.1016/j.jhin.2005.02.004 [DOI] [PubMed] [Google Scholar]
- 306.Apostolou A, Bolcen SJ, Dave V, Jani N, Lasker BA, Tan CG, et al. Nocardia cyriacigeorgica infections attributable to unlicensed cosmetic procedures-an emerging public health problem? Clin Infect Dis. (2012) 55:251–3. 10.1093/cid/cis341 [DOI] [PubMed] [Google Scholar]
- 307.Chen J, Zhou H, Xu P, Zhang P, Ma S, Zhou J. Clinical and radiographic characteristics of pulmonary nocardiosis: clues to earlier diagnosis. PLoS ONE. (2014) 9:e90724. 10.1371/journal.pone.0090724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Wilson JW. Nocardiosis: updates and clinical overview. Mayo Clin Proc. (2012) 87:403–7. 10.1016/j.mayocp.2011.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.McNeil MM, Brown JM. The medically important aerobic actinomycetes: epidemiology and microbiology. Clin Microbiol Rev. (1994) 7:357–417. 10.1128/CMR.7.3.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Steinbrink J, Leavens J, Kauffman CA, Miceli MH. Manifestations and outcomes of nocardia infections: comparison of immunocompromised and nonimmunocompromised adult patients. Medicine. (2018) 97:e12436. 10.1097/MD.0000000000012436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Stropnik Z. Isolation of Nocardia asteroides from human skin. Sabouraudia. (1965) 4:41–4. 10.1080/00362176685190111 [DOI] [PubMed] [Google Scholar]
- 312.Rosett W, Hodges GR. Recent experiences with nocardial infections. Am J Med Sci. (1978) 276:279–85. 10.1097/00000441-197811000-00004 [DOI] [PubMed] [Google Scholar]
- 313.Ishikawa O. Aerobic gram-positive pleomorphic rods isolated from dental plaque and gingival crevice. Bull Tokyo Med Dent Univ. (1980) 27:71–7. [PubMed] [Google Scholar]
- 314.Yildiz O, Doganay M. Actinomycoses and Nocardia pulmonary infections. Curr Opin Pulm Med. (2006) 12:228–34. 10.1097/01.mcp.0000219273.57933.48 [DOI] [PubMed] [Google Scholar]
- 315.Conville PS, Brown-Elliott BA, Smith T, Zelazny AM. The complexities of nocardia taxonomy and identification. J Clin Microbiol. (2017) 56:e01419–17. 10.1128/JCM.01419-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ, Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. (2006) 19:259–82. 10.1128/CMR.19.2.259-282.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Sugar AM, Schoolnik GK, Stevens DA. Antibody response in human nocardiosis: identification of two immunodominant culture-filtrate antigens derived from Nocardia asteroides. J Infect Dis. (1985) 151:895–901. 10.1093/infdis/151.5.895 [DOI] [PubMed] [Google Scholar]
- 318.Vera-Cabrera L, Salinas-Carmona MC, Welsh O, Rodriguez MA. Isolation and purification of two immunodominant antigens from Nocardia brasiliensis. J Clin Microbiol. (1992) 30:1183–8. 10.1128/JCM.30.5.1183-1188.1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Salinas-Carmona MC, Vera L, Welsh O, Rodriguez M. Antibody response to Nocardia brasiliensis antigens in man. Zentralbl Bakteriol. (1992) 276:390–7. 10.1016/S0934-8840(11)80546-3 [DOI] [PubMed] [Google Scholar]
- 320.Angeles AM, Sugar AM. Identification of a common immunodominant protein in culture filtrates of three Nocardia species and use in etiologic diagnosis of mycetoma. J Clin Microbiol. (1987) 25:2278–80. 10.1128/JCM.25.12.2278-2280.1987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Boiron P, Provost F. Use of partially purified 54-kilodalton antigen for diagnosis of nocardiosis by Western blot (immunoblot) assay. J Clin Microbiol. (1990) 28:328–31. 10.1128/JCM.28.2.328-331.1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Saubolle MA, Sussland D. Nocardiosis: review of clinical and laboratory experience. J Clin Microbiol. (2003) 41:4497–501. 10.1128/JCM.41.10.4497-4501.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Wauters G, Avesani V, Charlier J, Janssens M, Vaneechoutte M, Delmée M. Distribution of nocardia species in clinical samples and their routine rapid identification in the laboratory. J Clin Microbiol. (2005) 43:2624–8. 10.1128/JCM.43.6.2624-2628.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Law BJ, Marks MI. Pediatric nocardiosis. Pediatrics. (1982) 70:560–5. [PubMed] [Google Scholar]
- 325.Kandi V. Human nocardia infections: a review of pulmonary nocardiosis. Cureus. (2015) 7:e304. 10.7759/cureus.304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Budzik JM, Hosseini M, Mackinnon AC, Jr, Taxy JB. Disseminated Nocardia farcinica: literature review and fatal outcome in an immunocompetent patient. Surg Infect. (2012) 13:163–70. 10.1089/sur.2011.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Musgrave WE, Clegg MT. The etiology of mycetoma. Phillippine J Sc. (1907) B:477–511.14477536 [Google Scholar]
- 328.Steele AE, Lee RI. A case of infection with Nocardia. Bost M S J. (1913) 169:502–3. 10.1056/NEJM191310021691404 [DOI] [Google Scholar]
- 329.de Korté WE. Nocardia cylindracea: a South African otomycosis. Ann Trop Med. (1917) 11:265–78. 10.1080/00034983.1918.11684139 [DOI] [Google Scholar]
- 330.Alestra L, Girolami M. Endocarditi da nocardie. Policlin Med. (1937) 44:441. [Google Scholar]
- 331.Lyons C, Owen CR, Ayers WB. Sulfonamide therapy in actinomycotic infections. Surgery. (1943) 14:99. [Google Scholar]
- 332.Cook F V, Farrar WE, Jr. Treatment of Nocardia asteroides infection with trimethoprim-sulfamethoxazole. South Med J. (1978) 71:512–5. 10.1097/00007611-197805000-00011 [DOI] [PubMed] [Google Scholar]
- 333.Wallace RJJ, Septimus EJ, Williams TWJ, Conklin RH, Satterwhite TK, Bushby MB, et al. Use of trimethoprim-sulfamethoxazole for treatment of infections due to Nocardia. Rev Infect Dis. (1982) 4:315–25. 10.1093/clinids/4.2.315 [DOI] [PubMed] [Google Scholar]
- 334.Scopetti F, Iona E, Fattorini L, Goglio A, Franceschini N, Amicosante G, et al. Activity of antimicrobial drugs evaluated by agar dilution and radiometric methods against strains of Nocardia asteroides isolated in Italy from immunocompromised patients. J Chemother. (1994) 6:29–34. 10.1080/1120009X.1994.11741125 [DOI] [PubMed] [Google Scholar]
- 335.Husain S, McCurry K, Dauber J, Singh N, Kusne S. Nocardia infection in lung transplant recipients. J Hear Lung Transplant. (2002) 21:354–9. 10.1016/S1053-2498(01)00394-1 [DOI] [PubMed] [Google Scholar]
- 336.Muñoz J, Mirelis B, Aragón LM, Gutiérrez N, Sánchez F, Español M, et al. Clinical and microbiological features of nocardiosis 1997–2003. J Med Microbiol. (2007) 56:545–50. 10.1099/jmm.0.46774-0 [DOI] [PubMed] [Google Scholar]
- 337.Southern PM, Jr, Kutscher AE, Ragsdale R, Luttrell B. Susceptibility in vitro of Nocardia species to antimicrobial agents. Diagn Microbiol Infect Dis. (1987) 8:119–22. 10.1016/0732-8893(87)90159-3 [DOI] [PubMed] [Google Scholar]
- 338.Nguyen AT, Gentry CA, Furrh RZ. A comparison of adverse drug reactions between high- and standard-dose trimethoprim-sulfamethoxazole in the ambulatory setting. Curr Drug Saf. (2013) 8:114–9. 10.2174/1574886311308020004 [DOI] [PubMed] [Google Scholar]
- 339.Welsh O, Vera-Cabrera L, Salinas-Carmona MC. Current treatment for nocardia infections. Expert Opin Pharmacother. (2013) 14:2387–98. 10.1517/14656566.2013.842553 [DOI] [PubMed] [Google Scholar]
- 340.Caron F, Meurice JC, Dore P, Perault MC, Breux JP, Patte F. Gingival hyperplasia: a new side effect associated with trimethoprim-sulfamethoxazole (TML-SMX) treatment in pulmonary nocardiosis. Therapie. (1997) 52:73–4. [PubMed] [Google Scholar]
- 341.Bartels RH, van der Spek JA, Oosten HR. Acute pancreatitis due to sulfamethoxazole-trimethoprim. South Med J. (1992) 85:10067. 10.1097/00007611-199210000-00018 [DOI] [PubMed] [Google Scholar]
- 342.Bousfiha A, Jeddane L, Picard C, Al-Herz W, Ailal F, Chatila T, et al. Human inborn errors of immunity: 2019 update of the IUIS phenotypical classification. J Clin Immunol. (2020) 40:66–81. 10.1007/s10875-020-00758-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Winkelstein JA, Marino MC, Johnston RB, Boyle J, Curnutte J, Gallin JI, et al. Chronic granulomatous disease: report on a national registry of 368 patients. Medicine. (2000) 79:155–69. 10.1097/00005792-200005000-00003 [DOI] [PubMed] [Google Scholar]
- 344.de Oliveira-Junior EB, Zurro NB, Prando C, Cabral-Marques O, Pereira PVS, Schimke LF, et al. Clinical and genotypic spectrum of chronic granulomatous disease in 71 Latin American patients: first report from the LASID registry. Pediatr Blood Cancer. (2015) 62:2101–7. 10.1002/pbc.25674 [DOI] [PubMed] [Google Scholar]
- 345.Marciano BE, Spalding C, Fitzgerald A, Mann D, Brown T, Osgood S, et al. Common severe infections in chronic granulomatous disease. Clin Infect Dis. (2015) 60:1176–83. 10.1093/cid/ciu1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Bassiri-Jahromi S, Doostkam A. Actinomyces and nocardia infections in chronic granulomatous disease. J Glob Infect Dis. (2011) 3:348–52. 10.4103/0974-777X.91056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Agudelo-Flórez P, Prando-Andrade CC, López JA, Costa-Carvalho BT, Quezada A, Espinosa FJ, et al. Chronic granulomatous disease in Latin American patients: clinical spectrum and molecular genetics. Pediatr Blood Cancer. (2006) 46:243–52. 10.1002/pbc.20455 [DOI] [PubMed] [Google Scholar]
- 348.Rieg S, Meier B, Fahnrich E, Huth A, Wagner D, Kern W V, et al. Differential activity of innate defense antimicrobial peptides against Nocardia species. BMC Microbiol. (2010) 10:61. 10.1186/1471-2180-10-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Mendez-Tovar LJ, Mondragon-Gonzalez R, Manzano-Gayosso P, Lopez-Martinez R, Hernandez-Hernandez F, Bonifaz A, et al. [Immunoglobulins in patients with Nocardia brasiliensis actinomycetoma]. Rev Argent Microbiol. (2004) 36:174–8. [PubMed] [Google Scholar]
- 350.Tillman BF, Pauff JM, Satyanarayana G, Talbott M, Warner JL. Systematic review of infectious events with the Bruton tyrosine kinase inhibitor ibrutinib in the treatment of hematologic malignancies. Eur J Haematol. (2018) 100:325–34. 10.1111/ejh.13020 [DOI] [PubMed] [Google Scholar]
- 351.Lee WS, Boey CC, Goh AY. Pulmonary nocardiosis in a child with hyperimmunoglobulin E syndrome. Singapore Med J. (1999) 40:278–80. [PubMed] [Google Scholar]
- 352.Pintado V, Gómez-Mampaso E, Cobo J, Quereda C, Meseguer MA, Fortún J, et al. Nocardial infection in patients infected with the human immunodeficiency virus. Clin Microbiol Infect. (2003) 9:716–20. 10.1046/j.1469-0691.2003.00588.x [DOI] [PubMed] [Google Scholar]
- 353.Jayaschandran V, Gjorgova-Gjeorgjievski S, Siddique H. Pulmonary nocardiosis in a patient with idiopathic CD4 T-lymphocytopenia. Respir Case Rep. (2017) 6:e00283. 10.1002/rcr2.283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Adjamian N, Kikam A, Wessell KR, Casselman J, Toller-Artis E, Olasokan O, et al. Nocardia brain abscess and CD4(+) lymphocytopenia in a previously healthy individual. Case Rep. Immunol. (2015) 2015:374956. 10.1155/2015/374956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Ercibengoa M, Càmara J, Tubau F, García-Somoza D, Galar A, Martín-Rabadán P, et al. A multicentre analysis of Nocardia pneumonia in Spain: 2010–2016. Int J Infect Dis. (2020) 90:161–6. 10.1016/j.ijid.2019.10.032 [DOI] [PubMed] [Google Scholar]
- 356.Oh CS, Stratta RJ, Fox BC, Sollinger HW, Belzer FO, Maki DG. Increased infections associated with the use of OKT3 for treatment of steroid-resistant rejection in renal transplantation. Transplantation. (1988) 45:68–73. 10.1097/00007890-198801000-00016 [DOI] [PubMed] [Google Scholar]
- 357.Penkert H, Delbridge C, Wantia N, Wiestler B, Korn T. Fulminant central nervous system nocardiosis in a patient treated with alemtuzumab for relapsing-remitting multiple sclerosis. JAMA Neurol. (2016) 73:757–9. 10.1001/jamaneurol.2016.0146 [DOI] [PubMed] [Google Scholar]
- 358.Sheikh-Taha M, Corman LC. Pulmonary Nocardia beijingensis infection associated with the use of alemtuzumab in a patient with multiple sclerosis. Mult Scler. (2017) 23:872–4. 10.1177/1352458517694431 [DOI] [PubMed] [Google Scholar]
- 359.Mendez-Tovar LJ, Mondragon-Gonzalez R, Vega-Lopez F, Dockrell HM, Hay R, Lopez-Martinez R, et al. Cytokine production and lymphocyte proliferation in patients with Nocardia brasiliensis actinomycetoma. Mycopathologia. (2004) 158:407–14. 10.1007/s11046-004-3126-4 [DOI] [PubMed] [Google Scholar]
- 360.Ali T, Chakraburtty A, Mahmood S, Bronze MS. Risk of nocardial infections with anti-tumor necrosis factor therapy. Am J Med Sci. (2013) 346:166–8. 10.1097/MAJ.0b013e3182883708 [DOI] [PubMed] [Google Scholar]
- 361.Ford AC, Peyrin-Biroulet L. Opportunistic infections with anti-tumor necrosis factor-α therapy in inflammatory bowel disease: meta-analysis of randomized controlled trials. Am J Gastroenterol. (2013) 108:1268–76. 10.1038/ajg.2013.138 [DOI] [PubMed] [Google Scholar]
- 362.Salmon-Ceron D, Tubach F, Lortholary O, Chosidow O, Bretagne S, Nicolas N, et al. Drug-specific risk of non-tuberculosis opportunistic infections in patients receiving anti-TNF therapy reported to the 3-year prospective French RATIO registry. Ann Rheum Dis. (2011) 70:616–23. 10.1136/ard.2010.137422 [DOI] [PubMed] [Google Scholar]
- 363.Wallis RS, Broder MS, Wong JY, Hanson ME, Beenhouwer DO. Granulomatous infectious diseases associated with tumor necrosis factor antagonists. Clin Infect Dis. (2004) 38:1261–5. 10.1086/383317 [DOI] [PubMed] [Google Scholar]
- 364.Lee G, Robosa R, Fong G, Lee FJ, Lowe P, Pinto AN. Adult cervicofacial nocardiosis in the setting of IL-12/23 blockade. Australas J Dermatol. (2019) 60:323–4. 10.1111/ajd.13046 [DOI] [PubMed] [Google Scholar]
- 365.Picard C, Fieschi C, Altare F, Al-Jumaah S, Al-Hajjar S, Feinberg J, et al. Inherited interleukin-12 deficiency: IL12B genotype and clinical phenotype of 13 patients from six kindreds. Am J Hum Genet. (2002) 70:336–48. 10.1086/338625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Luangwedchakarn V, Jirapongsaranuruk O, NiemeLa JE, Thepthai C, Chokephaibulkit K, Sukpanichnant S, et al. A novel mutation of the IL12RB1 gene in a child with nocardiosis, recurrent salmonellosis and neurofibromatosis type I: first case report from Thailand. Asian Pac J Allergy Immunol. (2009) 27:161–5. [PubMed] [Google Scholar]
- 367.Pedraza S, Lezana JL, Samarina A, Aldana R, Herrera MT, Boisson-Dupuis S, et al. Clinical disease caused by Klebsiella in 2 unrelated patients with interleukin 12 receptor beta1 deficiency. Pediatrics. (2010) 126:e971–6. 10.1542/peds.2009-2504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Prando C, Samarina A, Bustamante J, Boisson-Dupuis S, Cobat A, Picard C, et al. Inherited IL-12p40 deficiency: genetic, immunologic, and clinical features of 49 patients from 30 kindreds. Medicine. (2013) 92:109–22. 10.1097/MD.0b013e31828a01f9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Eisenblätter M, Buchal A, Gayum H, Jasny E, Renner Viveros P, Ulrichs T, et al. Nocardia farcinica activates human dendritic cells and induces secretion of interleukin-23 (IL-23) rather than IL-12p70. Infect Immun. (2012) 80:4195–202. 10.1128/IAI.00741-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Rosen LB, Pereira NR, Figueiredo C, Fiske LC, Ressner RA, Hong JC, et al. Nocardia-induced granulocyte macrophage colony-stimulating factor is neutralized by autoantibodies in disseminated/extrapulmonary nocardiosis. Clin Infect Dis. (2015) 60:1017–25. 10.1093/cid/ciu968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Picard C, von Bernuth H, Ghandil P, Chrabieh M, Levy O, Arkwright PD, et al. Clinical features and outcome of patients with IRAK-4 and MyD88 deficiency. Medicine. (2010) 89:403–25. 10.1097/MD.0b013e3181fd8ec3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Corvilain E, Casanova J-L, Puel A. Inherited CARD9 deficiency: invasive disease caused by ascomycete fungi in previously healthy children and adults. J Clin Immunol. (2018) 38:656–93. 10.1007/s10875-018-0539-2 [DOI] [PMC free article] [PubMed] [Google Scholar]