Abstract
Human papillomavirus (HPV) has been linked to genital warts and multiple cancers affecting both men and women. Despite college students’ high risk for HPV, their vaccination rates remain suboptimal. The current observational study examined the relationship between social norms and human papillomavirus (HPV) vaccine intentions and potential mechanisms underlying this relationship among undergraduates. Participants (N=190; 66.8% female) completed a survey assessing HPV vaccine social norms, attitudes, self-efficacy, and intentions. Three mediation analyses were conducted to examine whether self-efficacy and attitudes mediated the relationship between social norms (i.e., parents, friends, doctor) and intentions, controlling for demographic and health care covariates. Social norms were indirectly related to intentions through self-efficacy and attitudes in multiple models (ps<.05). Specifically, perceiving greater support for HPV vaccination from one’s friends, parents, and doctor was related to greater HPV vaccine self-efficacy, which, in turn, was related to increased vaccine intentions. In addition, perceiving greater parental and doctor support for HPV vaccination was related to more favorable attitudes towards the vaccine, which, in turn, were related to increased vaccine intentions. Findings suggest potential targets for future interventions to promote HPV vaccination among young adults.
Keywords: human papillomavirus vaccination, social norms, self-efficacy, attitudes, Theory of Planned Behavior
Introduction
Most sexually active individuals in the United States will be infected with at least one human papillomavirus (HPV) strain during their lifetime [1]. The majority of HPV infections resolve without treatment; however, persistent infections from high-risk HPV types can develop into oropharyngeal, cervical, anal, vulvar, vaginal, and penile cancers [1-3]. The HPV vaccine is most effective prior to any sexual experience, and thus, the target age range for vaccination is in early adolescence [1-4]. The vaccine series can be administered to males and females starting at age 9 [2-4] and is approved for use through age 45 [2].
Young adults in the United States are at significantly higher risk for HPV infection compared to other age groups [5]. The Advisory Committee on Immunization Practices (ACIP) recommends all previously unvaccinated males and females receive “catch-up vaccination” through age 26 [4]. Although the vaccine is approved through age 45, the ACIP recommends that individuals ages 27-45 years old engage in shared decision-making about HPV vaccination with their provider [4]. Although college-aged individuals are at high risk for being exposed to HPV [5], only 40 - 69% of female college students and 8 - 43% of male college students report initiating the HPV vaccine series [6-8]
The Theory of Planned Behavior (TPB) provides a framework for studies of HPV vaccine intentions and uptake in college students and young adults [9, 10]. TPB is used to explain engagement in a specific behavior by examining beliefs, such as attitudes, self-efficacy, intentions, and subjective social norms about the behavior [11]. Consistent with this theory, greater social norms (i.e., perceptions that important others support HPV vaccination) have been associated with greater vaccine intentions and uptake among college students and young adults [9, 10, 12-15]. However, many studies have focused on global social norms rather than examining relations between specific social norms (e.g., parents, peers, doctor) and young adults’ HPV vaccine intentions and behaviors. Studies also have yet to identify mechanisms through which social norms may influence HPV vaccine intentions.
TPB suggests that perceived behavioral control, a construct comparable to self-efficacy or the belief in one’s ability to accomplish a task, may be associated with both social norms and intentions to receive the HPV vaccine [10]. Consistent with this theory, self-efficacy is related to social norms for other health behaviors in college students, such as obtaining adequate sleep and condom use [16, 17]. Additionally, greater self-efficacy for HPV vaccination has been associated with increased vaccine acceptability and intentions in college students [18-20] and young adults [21]. Findings from qualitative research suggest that self-efficacy may be one mechanism through which social norms influence college students’ intentions to be vaccinated [22, 23]. For example, among college women, support from their mother and healthcare provider to receive the HPV vaccine appeared to foster their belief that they could complete the necessary steps to be vaccinated in the future [22]. In another qualitative study, college women reported that family members’ assistance in overcoming barriers to HPV vaccination (e.g., paying for the vaccine, scheduling the vaccine appointment) bolstered their confidence in their ability to be vaccinated [23]. Friends were only viewed as important in HPV vaccine decision-making when they related their personal experiences with vaccination, thereby increasing perceptions of vaccine safety and intentions to be vaccinated [22].
Attitudes about HPV vaccination is another TPB construct that may help explain the relationship between social norms and vaccine intentions [10]. These attitudes include positive or negative opinions of the HPV vaccine (e.g., getting the HPV vaccine would be foolish) as well as the belief that HPV vaccination leads to positive or negative outcomes (e.g., getting the HPV vaccine will prevent cancer) [11]. Theory suggests that young adults’ perception that important others support their receipt of the HPV vaccine might increase their positive attitudes towards obtaining it and, in turn, their vaccine intentions. Believing that important others see value in obtaining the HPV vaccination may influence how one views the vaccine [22, 23], whereas negative attitudes from important others toward the vaccine may contribute to inaction [24]. For example, a qualitative study of female college students revealed how support for the HPV vaccine from important others might influence their attitudes about the vaccine through social motivation (e.g., trust in their provider, friends modeling vaccination behaviors) [22]. Another qualitative study of college women suggested that descriptive peer norms (i.e., having friends who have been vaccinated) may serve to reduce stigma about the HPV vaccine [23]. Conversely, negative attitudes toward the vaccine from important others may lead to the decision to not initiate the vaccine series [24]. Indeed, among unvaccinated young adults, attitudes about the HPV vaccine have been related to perceived social norms regarding vaccination, controlling for vaccine intentions [11]. Additionally, a number of studies with college students and young adults have found a relationship between attitudes about the HPV vaccine and intentions to receive the vaccine [7, 9-11, 13, 25, 26].
The present study expands prior research on the relationship between social norms and HPV vaccine intentions by considering specific social norms (parent, friend, and doctor) separately and examining potential mechanisms that might underlie their relationships to vaccine intentions. This study focused on college students given their high risk for HPV, ability to make HPV vaccination decisions for themselves, and suboptimal vaccination rates [5]. In the current study, we focused on college students in Indiana, one of the lowest-ranking states for HPV vaccination rates among young adults [27]. Based on the TPB [10], we hypothesized that greater perceived parental, friend, and doctor norms for HPV vaccination would be related to increased intentions to receive the HPV vaccine. Further, we hypothesized that increased self-efficacy for HPV vaccination and positive attitudes about the HPV vaccine would mediate the relationships between each of the three social norms and vaccine intentions. Study findings have direct implications for intervention development to promote HPV vaccination in this population.
Material and Methods
Participants and Procedures
Undergraduates were recruited through a psychology participant pool at an urban, public university in Indiana to participate in a cross-sectional, observational study. Participants (N=434) were between 18 and 35 years of age and fluent in English. Following verbal informed consent procedures, participants completed an anonymous online survey (mean completion time: 39.27 minutes (SD=9.4 minutes) administered in a campus computer lab in groups ranging from 1 to 15 people. Participants were seated with space between them to facilitate privacy when responding to the survey. Data were collected between January and December 2015. Due to anonymous data collection, the Indiana University-Purdue University Indianapolis IRB identified the study as exempt.
Measures
HPV vaccination status.
Participants were given a written description of the HPV vaccine and then were asked one yes/no question to indicate if they had heard of the vaccine prior to study participation [28]. Those who had heard of the vaccine were asked whether they had ever received it [28]. Individuals who had not heard of the vaccine and those who reported that they had not received the vaccine were considered unvaccinated. Only unvaccinated individuals were included in the current analyses.
HPV vaccination intentions.
Intentions to receive the HPV vaccine were measured with five items [10]. Participants rated on a 7-point scale how likely they were to: (1) get more information about the HPV vaccine, (2) consider getting the vaccine, (3) try to get the vaccine, (4) actually get the vaccine, and (5) get the vaccine if a doctor offered it (1=very unlikely to 7=very likely). This subscale showed excellent reliability in the current sample (α=0.95).
Subjective social norms.
Subjective social norms for HPV vaccination were measured with three items [11]. Participants were asked to indicate their degree of agreement with three separate statements that their friends, parents, and doctor support their receipt of the vaccine on a 7-point scale (1=very strongly disagree to 7=very strongly agree).
Self-efficacy.
Self-efficacy was measured with three items [10]. On a 7-point scale (1=disagree strongly to 7=agree strongly), participants rated their confidence in their ability to get the HPV vaccine even if: (1) it is expensive, (2) getting the shot hurts a little, and (3) it means finding time to go to the doctor three times. The scale had excellent reliability in the current study (α=0.80).
Attitudes toward the HPV vaccine.
Attitudes toward the HPV vaccine were measured with five items [11]. Participants were asked to indicate how: (1) good or bad, (2) wise or foolish, (3) pleasant or unpleasant, (4) effective or ineffective, and (5) painless or painful they believed receiving the HPV vaccine would be on a 7-point scale. The scale had acceptable reliability in the current sample (α=0.73).
Demographic, healthcare, and sexual experience variables.
Participants reported demographic information, including gender, age, race/ethnicity, sexual orientation, and current relationship status. Participants also responded to the following healthcare variables: (1) their health insurance status [29]; (2) how many times they had seen a healthcare provider in the past 12 months (dichotomized as having seen a provider in the last year [yes/no]) [29]; and (3) whether a provider had ever recommended that they obtain the HPV vaccine [29]. In addition, participants reported whether they had prior sexual experience and the number of sexual partners in the past three months (dichotomized as having been sexually active in the past three months [yes/no]) [30].
Statistical Analyses
Statistical analyses were conducted using SPSS statistical software (SPSS Inc., version 24, Armonk, NY, 2016). Given our focus on vaccine intentions, participants who had received the vaccine were excluded from analyses (15 men and 207 women out of 434 total). Additionally, because the vaccine was not approved for individuals over 26 years of age at the time the data were collected [31], participants over the age of 26 (n=8) were excluded. Further, 14 participants were excluded from analyses due to missing data on key variables (e.g., vaccine status, age). Thus, data from 190 participants were analyzed in the present study.
First, descriptive statistics were examined and Pearson correlations were calculated between study variables. Next, multiple mediation analyses were conducted to test the hypothesis that self-efficacy and attitudes mediate the relationships between social norms (parent, doctor, and friend) and intentions to receive the HPV vaccine. A multiple mediation model tests both the overall mediation effect for the mediators in the model (total indirect effect) and the independent effects of the mediators (specific indirect effects) [32, 33]. Each type of social norm was examined in a separate multiple mediation analysis. Participant gender, visiting a healthcare provider in the past 12 months, physician recommendation, and health insurance status were control variables in all analyses, given their prior associations with HPV vaccine intentions [7, 34-36]. Mediation analyses were conducted using Preacher and Hayes’ bootstrapping procedures (5,000 resamples) in SPSS (version 24; IBM Corp, Armonk, NY) macros. Due to repeating analyses, an adjusted confidence interval of 99% was used. All analyses were two-tailed.
Results
Participant Characteristics
Participant demographics are presented in Table 1. The majority of participants (N=190) were female (66.8%), White (68.9%), heterosexual (92.1%), and had health insurance (89.5%). The average participant age was 19.4 years (SD=1.6). Most (76.8%) had previously heard of the HPV vaccine, and 48.6% of those who had heard of the vaccine reported that their doctor or another healthcare professional had recommended that they receive it. Additionally, the majority (82.6%) had visited a healthcare provider in the past 12 months. Two-thirds of participants (66.8%) had had at least one sexual experience, and 55.2% had been sexually active in the prior three months.
Table 1.
Participant Demographics (N=190)
| Mean (SD), n (%) | |
|---|---|
| Age (years) | 19.4 (1.6) |
| Gender | 127 (66.8%) female |
| Race/ethnicity | 131 (68.9%) White, non-Hispanic 18 (9.5%) Asian 15 (7.9%) Black/African American 14 (7.3%) Other/More than one race 12 (6.3%) Hispanic/Latino/a |
| Health insurance status | 170 (89.5%) insured |
| Visited healthcare provider in the past year | 89 (46.8%) yes |
| Had previously heard of HPV vaccine | 146 (76.8%) yes |
| Provider recommended HPV vaccine | 71 (37.4%) yes |
| Sexual orientation | 175 (92.1%) heterosexual 5 (2.6%) bisexual 4 (2.1%) gay 3 (1.6%) not sure 2 (1.1%) did not respond/missing 1 (0.5%) something else |
| Currently in a romantic relationship | 97 (51.1%) yes |
| Sexually active in the past 3 months | 105 (55.2%) yes |
| Have had at least one sexual experience | 127 (66.8%) yes |
HPV = human papillomavirus.
Bivariate Associations between Social Norms, Self-efficacy, and HPV Vaccine Intentions
Correlations between main study variables are presented in Table 2. Each of the social norms for HPV vaccination were positively correlated with self-efficacy (ps < .001) and vaccine intentions (ps < .001). In other words, stronger perceptions that their parents, friends, or doctor supported receipt of the HPV vaccine were associated with increased self-efficacy and intentions to receive the vaccine. Additionally, more favorable attitudes towards the HPV vaccine was correlated with perceiving stronger social norms for HPV vaccination from parents and doctors (ps < .001). Additional correlations between study variables including gender and healthcare experiences are displayed in Table 2.
Table 2.
Correlations between TPB Variables, Healthcare Experiences, and Intentions to Receive the HPV Vaccine
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Intentions | - | ||||||||
| 2. Social norms - friends | 0.43 | - | |||||||
| p-value | <0.001 | ||||||||
| 3. Social norms - parent | 0.49 | 0.65 | - | ||||||
| p-value | <0.001 | <0.001 | |||||||
| 4. Social norms - doctor | 0.28 | 0.41 | 0.46 | - | |||||
| p-value | <0.001 | <0.001 | <0.001 | ||||||
| 5. Self-efficacy | 0.53 | 0.26 | 0.42 | 0.28 | - | ||||
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 6. TPB - attitudes | 0.48 | 0.13 | 0.41 | 0.36 | 0.45 | - | |||
| p-value | <0.001 | 0.08 | <0.001 | <0.001 | <0.001 | ||||
| 7. Gender | 0.09 | 0.05 | −0.001 | 0.16 | 0.04 | −0.06 | - | ||
| p-value | 0.24 | 0.54 | 0.99 | 0.03 | 0.59 | 0.45 | |||
| 8. Visited healthcare provider in past year | 0.11 | −0.04 | 0.11 | 0.14 | 0.16 | 0.03 | 0.17 | - | |
| p-value | 0.14 | 0.59 | 0.14 | 0.06 | 0.02 | 0.64 | 0.02 | ||
| 9. Health insurance status | −0.06 | −0.02 | −0.04 | −0.01 | 0.03 | −0.02 | −0.02 | 0.19 | - |
| p-value | 0.41 | 0.76 | 0.58 | 0.89 | 0.64 | 0.78 | 0.75 | 0.01 | |
| 10. Healthcare provider recommended HPV vaccine |
0.01 | −0.001 | 0.06 | 0.47 | 0.12 | 0.05 | 0.31 | 0.17 | 0.02 |
| p-value | 0.87 | 0.99 | 0.42 | <0.001 | 0.10 | 0.51 | <0.001 | 0.02 | 0.82 |
Note. TPB = Theory of Planned Behavior. HPV = human papillomavirus. Gender is coded as 0=male, 1=female. Provider visit, provider recommendation, and health insurance are coded as 0=no, 1=yes.
Mediation
The potential mediating roles of self-efficacy and attitudes about the HPV vaccine in the associations between social norms and intentions to receive the vaccine were examined using three bias-corrected bootstrapped multiple mediation analyses. All models included gender, health insurance status, physician recommendation, and visit with a healthcare provider in the past year as covariates.
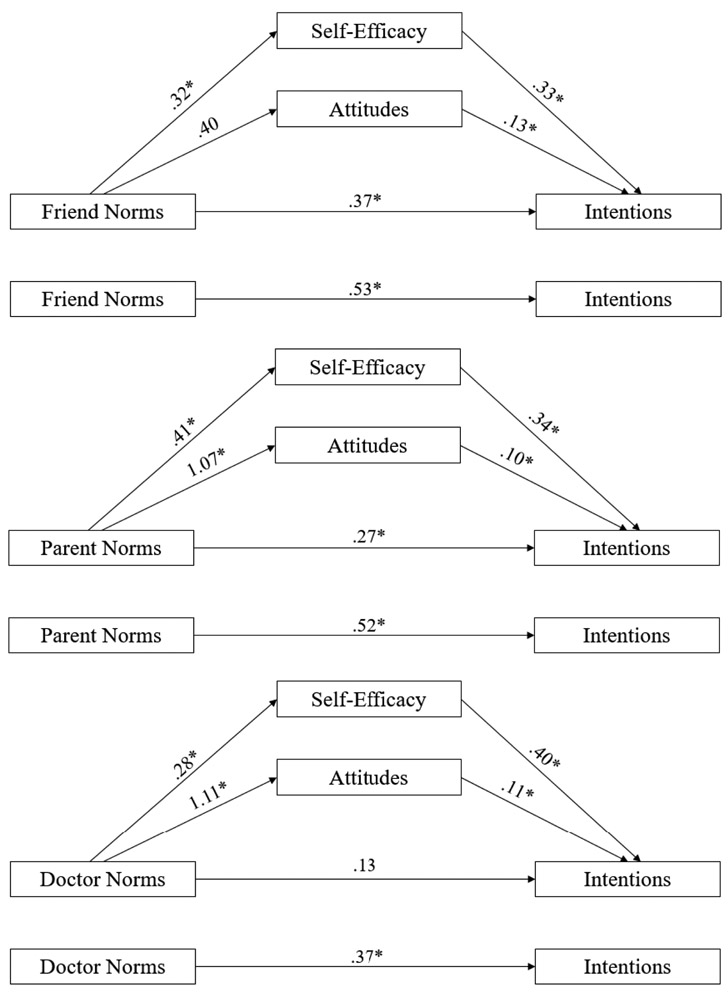
Friend norms.
Results indicated that friend norms, self-efficacy, HPV vaccine attitudes, and covariates accounted for 46% of the variation in HPV vaccine intentions. Friend norms had a significant indirect effect on intentions through self-efficacy (indirect effect=0.10; 99% CI=0.03-0.21; see Figure 1a). Perceiving stronger friend norms for vaccination was associated with greater self-efficacy for vaccination which, in turn, was associated with greater intentions to receive the vaccine. However, positive attitudes towards the vaccine did not mediate the relationship between friend norms and vaccine intentions (indirect effect=0.05; 99% CI=−0.03-0.15; see Figure 1a).
Parent norms.
Results indicated that parent norms, self-efficacy, HPV vaccine attitudes, and covariates accounted for 42% of the variation in HPV vaccine intentions. Parent norms had a significant indirect effect on HPV vaccine intentions through self-efficacy (indirect effect=0.14; 99% CI=0.06-0.25) and HPV vaccine attitudes (indirect effect=0.10; 99% CI=0.01-0.20; see Figure 1b). Perceiving stronger parent norms for vaccination was associated with greater self-efficacy and more favorable attitudes towards the vaccine, which, in turn, were associated with greater intentions to receive the vaccine.
Doctor norms.
Results indicated that doctor norms, self-efficacy, HPV vaccine attitudes, and covariates accounted for 38% of the variation in HPV vaccine intentions. Doctor norms had a significant indirect effect on HPV vaccine intentions through self-efficacy (indirect effect =.11; 99% CI=0.02-0.24; see Figure 1c) and HPV vaccine attitudes (indirect effect=0.12; 99% CI=0.03-0.25; see Figure 1c). Perceiving stronger doctor norms was associated with greater self-efficacy and more favorable attitudes towards the vaccine, which, in turn, were associated with greater intentions to receive the vaccine.
Discussion
The current study is the first to quantitatively examine mechanisms by which specific social norms (friend, parent, and doctor) may affect college students’ intentions to receive the HPV vaccine. Our results suggest that perceiving greater support from one’s friends, parents, and doctor for HPV vaccination is related to greater self-efficacy for vaccination which, in turn, is related to increased vaccine intentions. Additionally, findings suggest that perceiving greater support for HPV vaccination from parents and doctors – but not friends – is related to more favorable attitudes towards the vaccine, which, in turn, are related to increased vaccine intentions. Findings are grounded in the TPB and converge with prior research suggesting that social norms for other health behaviors (e.g., sleep, condom use) are related to college students’ intentions and behaviors through self-efficacy [16, 17]. Results are also consistent with qualitative findings that perceived social support for HPV vaccination bolsters self-efficacy for vaccine completion in college women [22].
Additionally, our findings suggest that doctor and parental support for HPV vaccination may relate more strongly to HPV vaccine attitudes than friend support for vaccination. This pattern is consistent with qualitative research suggesting that friends are less influential in the HPV vaccine decision-making process among young adults [22, 24]. Young adults have reported varying degrees of trust in their friends’ opinion of the HPV vaccine, especially if they have not been vaccinated themselves [22, 24].
Our findings inform future intervention research to increase HPV vaccination rates among college students. In particular, if replicated longitudinally, results suggest that increasing perceived support for the HPV vaccine from multiple sources (e.g., parents, peers, healthcare providers) may lead to students’ increased intentions to receive the HPV vaccine. To date, limited intervention research designed to increase HPV vaccine intentions or uptake has been conducted with U.S. college students and/or young adults [18, 37-41]. Only one intervention trial examined the importance of the source of the information (e.g., peer, provider) in providing HPV vaccine education to college students [37]. Specifically, this randomized control trial for college women featured narratives delivered by either a peer, an expert (i.e., a physician), or both and incorporated theory-driven cognitive factors such as perceived susceptibility to HPV and self-efficacy for vaccination [37]. The group that received messages from both a peer and a physician were twice as likely to obtain the vaccine than control groups that either received an informational video, a link to a campus website about HPV vaccination, or no message. Converging with the current findings, effects of the intervention were mediated by self-efficacy such that those who received the combined peer and expert message reported higher vaccine self-efficacy, which, in turn, predicted greater intentions to obtain the vaccine [37]. An important next step will be to compare the combined and separate effects of messages about the HPV vaccine from a parent, peer, or physician, especially for ethnocultural groups with strong norms for following parental guidance.
Prior studies have suggested that provider recommendation is the strongest predictor of HPV vaccine receipt among young adults [42, 43]. More than one-third (37%) of the present sample, all of whom were unvaccinated, reported receiving an HPV vaccine recommendation from a healthcare provider. Of note, however, only a moderate correlation (r = .47) was found between perceived doctor norms for vaccination and physician recommendation. This finding may reflect variation in the quality or strength of provider recommendations, highlighting the need for provider education on effective methods for delivering recommendations. In addition, although multi-level intervention trials that facilitate a strong provider recommendation have improved HPV vaccination among adolescents [44, 45], a paucity of interventions have targeted providers and clinics providing care to college students. The only systems-level intervention for this population incorporated electronic health record alerts in the charts of unvaccinated male patients at a university student health center, which resulted in HPV vaccine initiation rates rising from 5% to 25% among male patients [39]. Research identifying effective elements of provider communication about the HPV vaccine with young adults is needed as are interventions that test the efficacy of multi-level and multi-component strategies to promote HPV vaccination in this population.
The current findings suggest that positive communication about the HPV vaccine from providers and important others may promote vaccine intentions by improving attitudes and increasing self-efficacy. To target these variables, future interventions may include strong recommendations and approval for the vaccine from multiple sources, specifically highlighting HPV vaccine benefits, safety, and efficacy as well as young adults’ risk of HPV infection. Prior research has demonstrated that self-efficacy also mediates the relationships between both perceived barriers and perceived risk and HPV vaccination among female college students [20]. Thus, educational messages that directly address common HPV vaccine barriers (e.g., cost, fear of shots, multiple trips to clinic for completion doses, cultural or religious considerations) [24, 35, 46] may also improve self-efficacy.
Limitations of the current study should be noted. The study was cross-sectional, and thus mediating relationships warrant replication in longitudinal studies. In addition, the majority of the sample was White and female, and all attended an urban public university in Indiana. Further research is needed to determine the generalizability of study findings to college students with different demographics and those in other regions of the United States. Another limitation is that we did not obtain medical record confirmation of participants’ HPV vaccine status; however, prior research has supported the validity of self-reported HPV vaccination (i.e., over 90% sensitivity) [47]. We also did not measure subsequent vaccine uptake among those who were unvaccinated. However, prior studies have found that HPV vaccine intentions are significantly associated with subsequent HPV vaccine uptake among college students [48]. Finally, we did not assess whether participants had discussed the HPV vaccine with their parents or peers.
Conclusions
Given college students’ high risk for HPV infection [5] and suboptimal vaccination rates [6-8], effective interventions are needed to promote HPV vaccination in this population. Previous interventions to increase HPV vaccination have largely focused on young children and adolescents and their parents [44, 49]. If replicated longitudinally, our results support testing HPV vaccine interventions for college students that aim to improve self-efficacy for vaccination and attitudes about the HPV vaccine by facilitating positive communication about the vaccine with providers and important others.
Figure 1.
a. Model depicting the relationship between friend norms and intentions to receive the HPV vaccine through self-efficacy and attitudes. Values are unstandardized. Analyses controlled for gender, healthcare provider recommendation, health insurance, and visit to a healthcare provider in the past year.
*p<0.001.
b. Model depicting the relationship between parent norms and intentions to receive the HPV vaccine through self-efficacy and attitudes. Values are unstandardized. Analyses controlled for gender, healthcare provider recommendation, health insurance, and visit to a healthcare provider in the past year.
*p<0.001.
c. Model depicting the relationship between doctor norms and intentions to receive the HPV vaccine through self-efficacy and attitudes. Values are unstandardized. Analyses controlled for gender, healthcare provider recommendation, health insurance, and visit to a healthcare provider in the past year.
*p<0.001.
Acknowledgements:
Preliminary study results were presented at the 2016 Indiana University-Purdue University Indianapolis Research Day in Indianapolis, Indiana. All authors have approved the final article.
Funding: Dr. Christy’s work was funded by the National Cancer Institute while she was a postdoctoral fellow at H. Lee Moffitt Cancer Center and Research Institute (R25CA090314; PI: T. H. Brandon). Dr. Winger’s work was funded by the American Cancer Society (130526-PF-17-054-01-PCSM; PI: J. G. Winger). Dr. Mosher’s work was funded by the National Cancer Institute (K05CA175048; PI: V. L. Champion). The funding agencies had no role in designing the study, interpreting the data, writing the manuscript, or the decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the American Cancer Society.
Footnotes
Compliance with Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Contributor Information
Madison E. Stout, Department of Psychology, Oklahoma State University, Stillwater, Oklahoma 74078, USA; Department of Psychology, Indiana University-Purdue University Indianapolis, Indianapolis, Indiana 46202, USA.
Shannon M. Christy, Department of Health Outcomes and Behavior, Division of Population Science, H. Lee Moffitt Cancer Center and Research Institute, Tampa, Florida 33612, USA; Department of Oncologic Sciences, Morsani College of Medicine, University of South Florida, Tampa, Florida 33612, USA; Department of Psychology, Indiana University-Purdue University Indianapolis, Indianapolis, Indiana 46202, USA.
Joseph G. Winger, Department of Psychiatry and Behavioral Sciences, Division of Behavioral Medicine, Duke University School of Medicine, Durham, North Carolina 27705, USA.
Susan T. Vadaparampil, Department of Health Outcomes and Behavior, Division of Population Science, H. Lee Moffitt Cancer Center and Research Institute, Tampa, Florida 33612, USA; Department of Oncologic Sciences, Morsani College of Medicine, University of South Florida, Tampa, Florida 33612, USA.
Catherine E. Mosher, Department of Psychology, Indiana University-Purdue University Indianapolis, Indianapolis, Indiana 46202, USA.
References
- [1].Centers for Disease Control and Prevention (CDC). (2016). Human Papillomavirus (HPV), www.cdc.gov/hpv/parents/whatishpv.html. [accessed 10 July 2019].
- [2].Food and Drug Administration (FDA). (2018). Gardasil. https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm094042.htm. [accessed 10 July 2019].
- [3].Centers for Disease Control and Prevention (CDC). (2016). HPV Vaccine Recommendations, www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html, [accessed 10 July 2019].
- [4].Meites E, Szilagyi PG, Chesson HW, Unger ER, Romero JR, & Markowitz LE (2019). Human papillomavirus vaccination for adults: Updated recommendations of the Advisory Committee on Immunization Practices. Morbidity and Mortality Weekly Report, 68(32), 698–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Satterwhite CL, Torrone E, Meites E, et al. (2008). Sexually transmitted infections among US women and men: Prevalence and incidence estimates. Sexually Transmitted Infections, 40(3), 187–193. [DOI] [PubMed] [Google Scholar]
- [6].Thompson EL, Vamos CA, Vazquez-Otero C, Logan R, Griner S, & Daley EM (2016). Trends and predictors of HPV vaccination among U.S. College women and men. Preventive Medicine, 86, 92–98. [DOI] [PubMed] [Google Scholar]
- [7].Wilson AR, Hashibe M, Bodson J, et al. (2016). Factors related to HPV vaccine uptake and 3-dose completion among women in a low vaccination region of the USA: An observational study. BMC Womens Health, 16(1), 41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Williams WW, Lu P, O’Halloran A, et al. (Washington, D.C.: 2002). Surveillance of vaccination coverage among adult populations—United States, 2014 MMWR Surveillance Summaries, 65(1), 1–36. [DOI] [PubMed] [Google Scholar]
- [9].Catalano HP, Knowlden AP, Birch DA, Leeper JD, Paschal AM, & Usdan SL (2017). Using the Theory of Planned Behavior to predict HV vaccination intentions of college men. Journal of American College Health, 65(3), 197–207. [DOI] [PubMed] [Google Scholar]
- [10].Gerend MA & Shepherd JE (2012). Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine, 44(2), 171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Fisher WA, Kohut T, Salisbury CM, & Salvadori MI (2013). Understanding human papillomavirus vaccination intentions: Comparative utility of the theory of reasoned action and the theory of planned behavior in vaccine target age women and men. Journal of Sexual Medicine, 10(10), 2455–2464. [DOI] [PubMed] [Google Scholar]
- [12].Allen JD, Mohllajee AP, Shelton RC, Othus MK, Fontenot HB, & Hanna R (2009). Stage of adoption of the human papillomavirus vaccine among college women. Preventive Medicine, 48(5), 420–425. [DOI] [PubMed] [Google Scholar]
- [13].Krawczyk AL, Perez S, Lau E, et al. (2012). Human papillomavirus vaccination intentions and uptake in college women. Health Psychology, 31(5), 685–693. [DOI] [PubMed] [Google Scholar]
- [14].Ratanasiripong NT (2015). Factors Related to Human Papillomavirus (HPV) Vaccination in College Men. Public Health Nursing, 32(6), 645–653. [DOI] [PubMed] [Google Scholar]
- [15].Ratanasiripong NT, Cheng AL, & Enriquez M (2013). What college women know, think, and do about human papillomavirus (HPV) and HPV vaccine. Vaccine, 31(10), 1370–1376. [DOI] [PubMed] [Google Scholar]
- [16].Asare M (2015). Using the theory of planned behavior to determine the condom use behavior among college students. American Journal of Health Studies, 30(1), 43–50. [PMC free article] [PubMed] [Google Scholar]
- [17].Knowlden AP, Sharma M, & Bernard AL (2012). A theory of planned behavior research model for predicting the sleep intentions and behaviors of undergraduate college students. Journal of Primary Prevention, 33(1), 19–31. [DOI] [PubMed] [Google Scholar]
- [18].Mehta P, Sharma M, & Lee RC (2013). Designing and evaluating a health belief model-based intervention to increase intent of HPV vaccination among college males. International Quarterly of Community Health Education, 34(1), 101–117. [DOI] [PubMed] [Google Scholar]
- [19].Schaefer Ziemer K, & Hoffman MA (2013). Beliefs and attitudes regarding human papillomavirus vaccination among college-age women. Journal of Health Psychology, 18(10), 1360–1370. [DOI] [PubMed] [Google Scholar]
- [20].Christy SM, Winger JG, & Mosher CE (2019). Does self-efficacy mediate the relationships between social-cognitive factors and intentions to receive HPV vaccination among young women? Clinical Nursing Research, 28(6), 708–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Petrovic K, Burney S, & Fletcher J (2011). The relationship of knowledge, health value and health self-efficacy with men’s intentions to receive the human papillomavirus (HPV) vaccine. Journal of Health Psychology, 16(8), 1198–1207. [DOI] [PubMed] [Google Scholar]
- [22].Thompson EL, Vamos CA, Straub DM, Sappenfield WM, & Daley EM (2018). Human papillomavirus vaccine information, motivation, and behavioral skills among young adult US women. Preventive Medicine, 23(14), 1832–1841. [DOI] [PubMed] [Google Scholar]
- [23].Hopfer S, & Clippard JR (2011). College women’s HPV vaccine decision narratives. Qualitative Health Research, 21(2), 262–277. [DOI] [PubMed] [Google Scholar]
- [24].Hirth JM, Batuuka DN, Gross TT, Cofie L, & Berenson AB (2018). Human papillomavirus vaccine motivators and barriers among community college students: Considerations for development of a successful vaccination program. Vaccine, 36(8), 1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Bennett KK, Buchanan JA, & Adams AD (2012). Social-cognitive predictors of intention to vaccinate against the human papillomavirus in college-age women. Journal of Social Psychology, 152(4), 480–492. [DOI] [PubMed] [Google Scholar]
- [26].Ratanasiripong NT (2012). A review of human papillomavirus (HPV) infection and HPV vaccine-related attitudes and sexual behaviors among college-aged women in the United States. Journal of American College Health, 60(6), 461–470. [DOI] [PubMed] [Google Scholar]
- [27].Centers for Disease Control and Prevention (CDC). (2015). Behavioral Risk Factor Surveillance System, Indiana Statewide Survey Data, https://secure.in.gov/isdh/reports/brfss/2014/M11.01.htm, [accessed 10 July 2019].
- [28].Centers for Disease Control and Prevention (CDC). (2008). 2008 National Immunization Survey-Teen Hard Copy Questionnaire. In. Hyattsville, MD: Centers for Disease Control and Prevention. [Google Scholar]
- [29].National Cancer Institute (NCI). (2014). Health information national trends survey (HINTS). In. http://hints.cancer.gov/2014, [accessed 10 July 2019].
- [30].Penke L Revised sociosexual orientation inventory In Davis CM, Yarber WL, Bauserman R, Schreer G, Davis SL, editors. Handbook of Sexuality-Related Measure, Thousand Oaks: Sage Publication Inc; 2011;622:625. [Google Scholar]
- [31].U.S. Food and Drug Administration. Human Pappilomavirus 9-valent Vaccine, Recombinant (Report No. BL 125508/15 supplemental approval letter, December 14, 2015). www.fda.gov/downloads/BiologicsBloodVaccines/Vaccines/ApprovedProducts/UCM477341.pdf2015, [accessed 10 July 2019]
- [32].MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58, 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Preacher KJ & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- [34].Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, & Vichnin MD (2011). Predictors of HPV vaccine uptake among women aged 19-26: Importance of a physician's recommendation. Vaccine, 29(5), 890–895. [DOI] [PubMed] [Google Scholar]
- [35].Conroy K, Rosenthal SL, Zimet GD, et al. (2009). Human papillomavirus vaccine uptake, predictors of vaccination, and self-reported barriers to vaccination. Journal of Womens Health, 18(10), 1679–1686. [DOI] [PubMed] [Google Scholar]
- [36].Zimet GD, Weiss TW, Rosenthal SL, Good MB, & Vichnin MD (2010). Reasons for non-vaccination against HPV and future vaccination intentions among 19-26 year-old women. BMC Womens Health, 10(1), 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Hopfer S (2012). Effects of a narrative HPV vaccination intervention aimed at reaching college women: A randomized controlled trial. Prevention Science, 13(2), 173–182. [DOI] [PubMed] [Google Scholar]
- [38].Hayes KN, Pan I, Kunkel A, McGivney MS, & Thorpe CT (2018). Evaluation of targeted human papillomavirus vaccination education among undergraduate college students. Journal of American College Health, 1–9. [DOI] [PubMed] [Google Scholar]
- [39].Martin S, Warner EL, Kirchhoff AC, Mooney R, Martel L, & Kepka D (2018). An electronic medical record alert intervention to improve HPV Vaccination Among Eligible Male College Students at a University Student Health Center. Journal of Community Health, 43(4), 756–760. [DOI] [PubMed] [Google Scholar]
- [40].Paiva AL, Lipschitz JM, Fernandez AC, Redding CA, & Prochaska JO (2014). Evaluation of the acceptability and feasibility of a computer-tailored intervention to increase human papillomavirus vaccination among young adult women. Journal of Community Health, 62(1), 32–38. [DOI] [PubMed] [Google Scholar]
- [41].Staples JN, Wong MS, & Rimel BJ (2018). An educational intervention to improve human papilloma virus (HPV) and cervical cancer knowledge among African American college students. Gynecologic Oncology, 149(1), 101–105. [DOI] [PubMed] [Google Scholar]
- [42].Gerend MA, Shepherd MA, Lustria MLA, & Shepherd JE (2016). Predictors of provider recommendation for HPV vaccine among young adult men and women: Findings from a cross-sectional survey. Sexually Transmitted Infections, 92(2), 104–107. [DOI] [PubMed] [Google Scholar]
- [43].Gorbach PM, Cook R, Gratzer B, et al. (2017). Human papillomavirus vaccination among young men who have sex with men and transgender women in 2 US cities, 2012–2014. Sexually Transmitted Infections, 44(7), 436–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Holloway GL (2019). Effective HPV vaccination strategies: What does the evidence say? An integrated literature review. Journal of Pediatric Nursing, 44, 31–41. [DOI] [PubMed] [Google Scholar]
- [45].Vollrath K, Thul S, & Holcombe J (2018). Meaningful methods for increasing human papillomavirus vaccination rates: An integrative literature review. Journal of Pediatric Healthcare, 32(2), 119–132. [DOI] [PubMed] [Google Scholar]
- [46].Ferrer HB, Trotter C, Hickman M, & Audrey S (2014). Barriers and facilitators to HPV vaccination of young women in high-income countries: A qualitative systematic review and evidence synthesis. BMC Public Health, 14(1), 700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Rolnick S, Parker E, Nordin J, et al. (2013). Self-report compared to electronic medical record across eight adult vaccines: Do results vary by demographic factors? Vaccine, 31(37), 3928–3935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Patel DA, Zochowski M, Peterman S, Dempsey AF, Ernst S, & Dalton VK (2012). Human papillomavirus vaccine intent and uptake among female college students. Journal of American College Health, 60(2), 151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Walling EB, Benzoni N, Dornfeld J, et al. (2016). Interventions to improve HPV vaccine uptake: A systematic review. Pediatrics, 138(1), e20153863. [DOI] [PubMed] [Google Scholar]