Abstract
Background:
Parenting confidence is an important factor in fostering optimal health and development of infants with medical complexity. However, our understanding of how parents of medically complex infants describe development of confidence is limited. The purpose of this mixed-methods study was to describe the nature and development of parenting confidence.
Methods:
A mixed-method design was used to examine how parents described their level of confidence. Ten parents of infants with medical complexity. Quantitative measures provided patterns of confidence and qualitative data focused on parent descriptions of confidence. Parents completed online surveys at 3 time points: (1) study enrollment, (2) infant discharge from hospital, and (3) 3 months after discharge. Parents were purposively sampled, using their confidence patterns, for qualitative phone interviews.
Results:
Our analysis of quantitative findings revealed 3 confidence patterns: (1) increasing, (2) stable, and (3) varying. Parents described their confidence as either (1) a state of being confident or (2) how they behaved in the parenting role. Parents felt both certain and uncertain in their level of confidence and described confidence as being situationally dependent.
Implications for Practice:
Parenting confidence needs to be cultivated through encouragement and repeated exposure to parenting behaviors. Nurses are well-suited to help identify parents with low confidence to support parents so that they can develop confidence.
Implications for Research:
Because there is variability in parent confidence during this critical early period of life, future research should consider a larger cohort of parents that compares confidence in diverse parent groups (ie, married vs living together couples, same-sex couples, and single parents). Research should also examine effective strategies to promote confidence and associated long-term health and developmental outcomes.
Keywords: medical complexity, mixed-methods, NICU, parenting, parenting confidence, parenting self-efficacy
For any new parent, the progression from being a novice to an expert parent takes time and practice.1 Yet, when the transition to parenthood is challenged by hospitalization of a sick infant, parents report feeling overwhelmed,2 have difficultly feeling like a parent,3 and experience emotional distress.4,5 The normal transition to parenthood allows for close, frequent, and constant interaction with their infant6; however, during hospitalization there may be limited interaction and separation from the infant. Parents must adjust to an unfamiliar environment and modify their behaviors (eg, the caregiving tasks connected with parenting an infant), attitudes, and expectations, which can make it difficult to feel like a parent. Parenting behaviors include specific tasks connected to caring for an infant, which allow them to become more confident in their parenting role.
Learning to parent an infant who is in an intensive care can be challenging for any parent, but especially for parents who have an infant with medical complexity. Medically complex infants have one or more chronic conditions, are often technology dependent (eg. medication, oxygen requirements, and feeding tube), and have more severe functional limitations.7,8 The medical complexity of the infant, rather than the condition itself, is a more salient predictor of parenting confidence.9,10 Medically complex infants demand that their parents acquire new, unfamiliar healthcare-related skills and incorporate them into their parenting toolkit. An infant with more technological dependence (eg, medication, feeding tubes, and ventilation) requires greater adaptability on behalf of the parent. Confidence helps to buffer parental demands and challenging situations, supporting parental adaptation to unfamiliar and complex caregiving.
Parenting confidence is defined as one’s internal belief or judgment about their ability to be successful in their parenting role and foster their child’s growth and development.11 A confident or “expert” parent is more empowered to manage multiple parenting demands and often perceives these demands as less stressful than other parents.12–14 A longitudinal study found that mothers of infants with medical complexity had a significant increase in confidence over time.15 Parents of medically complex infants need to have a certain level of confidence with basic parenting skills as well as all aspects of complex medical caregiving. Becoming an expert parent implies gaining confidence in managing any challenging situations that might arise, especially those that are healthcare related. However, our understanding of how parents describe the growth of confidence is far less understood. Using a mixed-methods approach, the purpose of this analysis was to identify patterns of confidence and describe parents’ perspective about the nature and development of having confidence in their parenting role.
METHODS
Design
A sequential mixed-method study was conducted to examine how parents of medically complex infants report confidence in their parenting role. First, quantitative data were collected related to parenting confidence and infant medical caregiving complexity across 3 time points (enrollment, discharge, and 3 months after discharge). After the data were collected and analyzed, patterns were identified based on parenting confidence scores, and these patterns were used to purposively sample parents for qualitative interviews. The qualitative data were used to further elaborate and explain the development of parenting confidence and interpret the quantitative findings. Institutional review board approval was granted by the Duke University Medical System. Parents provided written consent prior to the start of data collection.
Participants
A total of 10 parents (9 mothers and 1 father) who had an infant diagnosed with a complex chronic condition were purposively selected for interviews. Eligibility was determined by their infants’ medical diagnosis as listed in the Complex Chronic Conditions Classification System developed by Feudtner et al.16 Parents with multiple gestation births, those younger than 18 years, and adoptive or foster parents were not included in this study, given the potential differences in parenting experiences within those contexts.
Procedures
Quantitative Data Collection
Parents completed online surveys at 3 time points: (1) study enrollment (admission to hospital), (2) infant discharge from hospital, and (3) 3 months after discharge. Parents were purposively sampled for phone interviews after they completed all 3 surveys and their confidence pattern was identified.
Measures
Karitane Parent Confidence Scale.
The Karitane Parent Confidence Scale is a 15-item, task-specific measure of parental confidence that can be used with mothers and fathers of infants 0 to 12 months old. Items are scored 0 to 3, for total scores that range from 0 to 45, with higher scores indicating greater confidence. This scale has a clinical index where scores less than 39 might indicate parents at risk of having low confidence who need support in their parenting role. Both internal consistency (α = 0.81, 0.84) and test-retest reliability (r = 0.88) are strong.17 Scores from parents over the study period were used to identify confidence patterns for the purposive sampling.
Technology Dependence Scale.
The Technology Dependence Scale (TDS)18 is a validated measure of technology dependence that captures the degree of medical caregiving complexity. This scale was created by neonatal and pediatric experts at the authors’ institution to identify change in technology dependence (ie, illness severity) over time, in different settings and across phases and types of illness. The TDS is a cumulative quantitative measure of an infant’s daily technological requirement in the hospital or home environment, which includes location of care, type of feeding, respiratory support, invasive lines, and medications. In total, there are 11 categories of technology support. The more frequent monitoring or greater amount of technological support, the higher the TDS score. Each point increment indicates increasing severity, with higher scores representing a greater dependence on technology, giving a continuous range of possible scores. Scoring was based on a retrospective chart review of the infant’s record.
Demographics.
Parent and infant demographic data were collected in the online survey. Information included parent age, sex, race/ethnicity, education, income, marital status, parent role, number of children, social support, prenatal diagnosis of infant illness, and previous experience with hospitalization. Infant data included gestational age, primary diagnosis, birth height and weight, type of feeding, and technology requirements.
Qualitative Data Collection.
During the consent process, parents were informed about the selection process for a phone interview after completion of the third and final survey and asked whether they were interested in participating. Parents had the option to express interest or decline participation in the phone interview again via a question in the final survey. We used a purposive sampling strategy to select parents for the interviewing from those who had expressed interest in participating in the interview (n = 39). The authors identified confidence patterns through visual inspection of confidence scores across data collection time points and 3 patterns were identified: (1) stable (high or low); (2) increasing; and (3) varying. Parents were then selected who were classified in each of these patterns and reflected variability in infant diagnosis, marital status, and hospital unit to ensure representative sample for interviews.19 The selection of parents was an ongoing, iterative process as parents completed the final survey. Parents were selected until the sample reflected all confidence patterns, had diverse demographic characteristics, and data saturation was reached.
The interview was scheduled based on the parent’s availability and preference. They were encouraged to find a comfortable setting to conduct the phone interview where they would not be interrupted. Parents were reminded about audio recording prior to the start of the interview. Interviews lasted an average of 30 to 40 minutes. Use of verbal cues (eg, use of names, courteous and positive verbal language, and interested tone of voice) helped to establish a rapport with parents during the interview. The interviewer had also met parents in person during the course of data collection. Audio files and transcripts were secured on a research-encrypted folder behind a firewall. Transcripts were completed by an independent transcriptionist and reviewed by the first author against their audio files for accuracy.
To understand how parents developed a sense of confidence in their parenting role, parents were asked the following questions: (1) Describe what being confident as a parent means to you? (2) Was there a point in which you felt a change in your confidence? (3) What about this experience has influenced you the most? Data were analyzed using directed content analysis.20 Analysis was supported by NVivo qualitative data analysis software; QSR International (12.2.0). Transcripts were read completely prior to the start of coding to become familiar with the interview content. Codes were reflective of general parenting concepts (eg, parenting role, confidence, behaviors, and hospital experience) as well as data-based codes reflecting the interview content (eg, acceptance, emotions, feeding, and expectations).21 The authors developed a code list, including a definition for each code. The first author coded all interviews and coauthors reviewed coded interviews as a check on the accuracy of the coding. To ensure the validity of our analysis, we used recommended strategies to strengthen the integrity, authenticity, and credibility.22 The following were strategies used: use of computer software to support systematic review of coded data, regular decision-making meetings, and memos of discussions were used to maintain record of analytic decisions and processes throughout data management, coding, and analysis. An audit trail recorded decisions about coding, themes, and interpretation of data.
FINDINGS
Demographics
Nine mothers and 1 father (n = 10) were interviewed. Parent mean age was 33.7 (±2.8) years, 70% were non-Hispanic white, 50% had a high school degree, 80% were married, and 50% had an income between $25,000 and $50,000. Infant diagnosis categories included congenital birth defect (n = 4), complex heart (n = 3), and extreme prematurity (n = 2). Sixty percent of infants were diagnosed prenatally and 45% of infants were the first child in the family.
Confidence and Complexity Patterns
As previously mentioned, parents were purposively sampled based on their confidence pattern across the 3 study time points: (1) stable (high or low) (n = 3); (2) increasing (n = 4); and (3) varying (n = 3). Most of the parents in this study increased in their sense of confidence over time or reported high, stable confidence in their parenting ability (n = 6). There were also patterns associated with the medical complexity of infants identified from the TDS scores (see Table 1). In general, medical complexity decreased over time, most notably at 3 months after discharge. Parents who had infants with decreasing complexity had a pattern of increasing parenting confidence over time (n = 3). For those parents whose confidence patterns varied (n = 3), their infants were more likely to have higher medical caregiving complexity (eg, more technology dependence) across all 3 times. Of note, several infants (n = 4) had high complexity scores (>10) at 3 months, an indication of high medical caregiving needs. Figure 1 compares parent confidence and complexity patterns.
TABLE 1.
Confidence and Medical Complexity Patterns
| Parent | Confidence Pattern | PC Scores | Complexitv Pattern | T D S Score | ||||
|---|---|---|---|---|---|---|---|---|
| En | Dc | 3mo | En | Dc | 3mo | |||
| P1 | Increasing | 38a | 40 | 40 | Decreasing | 34.75 | 15.50 | 2.00 |
| P2 | Increasing | 10 | 39 | 40 | Decreasing | 29.75 | 16.25 | 6.25 |
| P3 | Stable/high (mother) | 44 | 44 | 45 | Stable/high | 34.25 | 22.75 | 22.00b |
| P4 | Stable/low (father) | 34 | 35 | 31 | ||||
| P5 | Increasing | 37 | 42 | 44 | Decreasing | 18.50 | 14.50 | 4.00 |
| P6 | Increasing | 37 | 36 | 43 | Stable/high | 26.25 | 23.75 | 19.00 |
| P7 | Varying (high/low/high) | 44 | 38 | 41 | Varying | 20.75 | 22.00 | 10.25 |
| P8 | Varying (low/high/low) | 32 | 41 | 38 | Stable/high | 24.00 | 21.50 | 12.25 |
| P9 | Stable/high | 43 | 44 | 44 | Stable/low | 7.50 | 7.50 | 3.75 |
| P10 | Varying (low/high/low) | 37 | 42 | 32 | Stable/high | 16.25 | 16.50 | 8.00 |
Abbreviations: DC, discharge; En, enrollment; PC, parent confidence; TDS, Technology Dependence Scale; 3mo, 3 months after discharge.
Italicized text indicates scores below the clinical index <39.
Infant hospitalized at 3 months.
FIGURE 1.
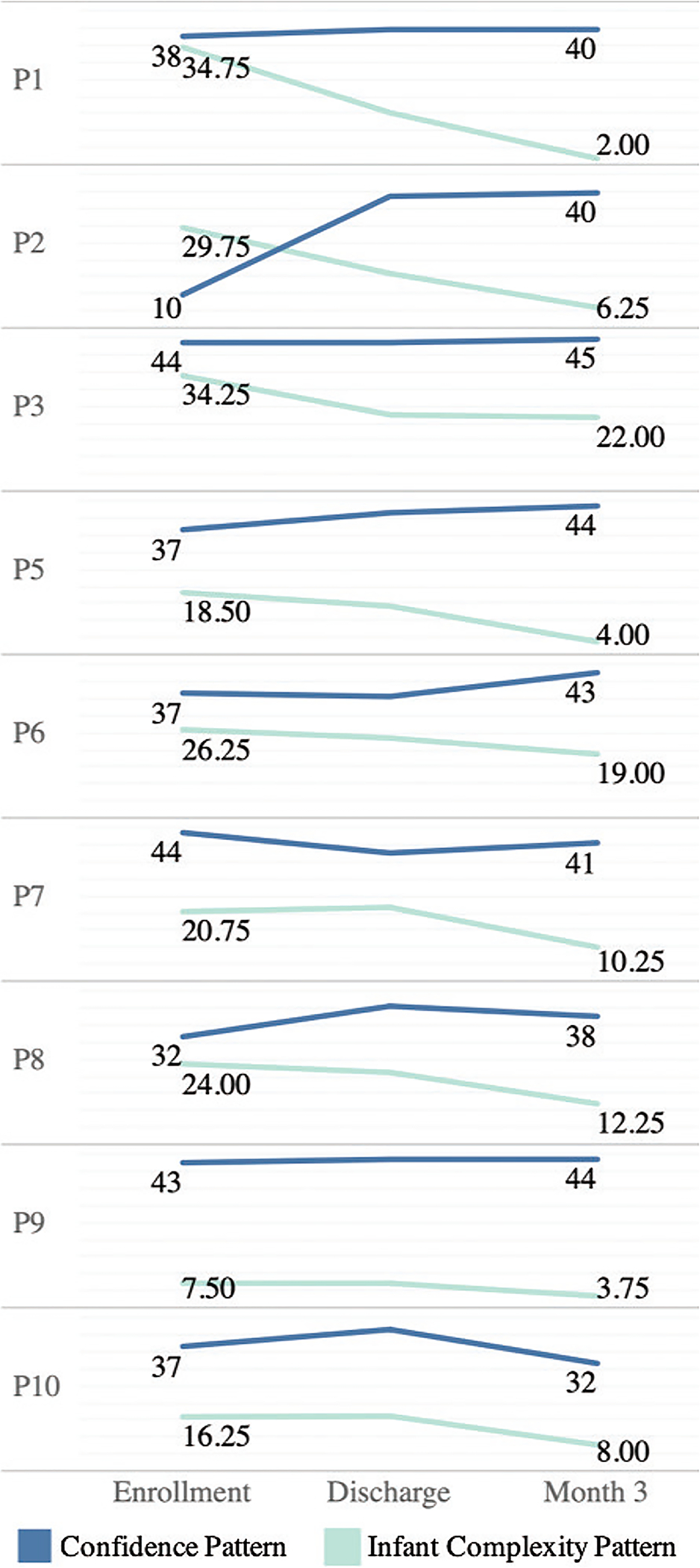
Comparison of confidence and complexity patterns by parent.
Describing Confidence
During the qualitative interviews, parents were asked to describe how they developed confidence in their parental role. Findings revealed that parents described their confidence as either (1) a state of being confident (ie, a feeling) (n = 6) or (2) how they behaved (eg, provided care) (n = 4) in the parenting role. Parents were coded into the 2 types based on how they described confidence in the interviews. Parents who described how they felt about being confident used more emotional language, whereas parents who spoke more about their behavior described confidence in terms of the things they did as a parent for their infant. Table 2 matches the confidence patterns with descriptions of confidence, with representative quotes. Most parents (n = 7) used feelings to describe their sense of confidence and they were more likely to have an increasing confidence trajectory pattern (n = 4) than parents who described their confidence in terms of behaviors.
TABLE 2.
Matching Confidence Patterns and Descriptions
| Confidence Pattern (Quantitative) | Confidence Type (Qualitative) | Representative Quotes |
|---|---|---|
| Stable/high (n = 2) | Behaving | Being able to provide them with what they need, provide them with things that they will want. |
| Feeling | I guess feeling comfortable in everything that you need to do for your child; being in touch with your child. Anything different with [him/her] personality; being that person that knows your child better than anyone. | |
| Stable/low (n = 1) | Behaving | Being able to provide for my children; I mean we may not always be able to give them what they deserve but at least I can always provide them with what they need. |
| Increasing (n = 4) | Feeling | It just kind of came naturally. When you spend the time getting to know [him/her] and being a part of the care.I don’t know if you become more confident or if you become comfortable. I don’t know if the two are the same, and then you just learn to accept things. |
| Varying (n = 3) | Behaving | Knowing that I can give medicine, do everything that needs to be done without having to question myself and being able to teach others what I know. |
| Feeling | I trust my own decision; I don’t second guess it. It’s just kind of instinct so I kind of just know. I feel confident that I’m doing the best that I can um as a mother. |
Parents used words like certain, unsure, and/or comfortable to describe their sense of confidence. Five parents specifically talked about feeling secure or certain in how much confidence they had, I trust my own decision. I don’t second guess it (P8). It just came naturally (P5). Feeling confident as a parent, knowing that I can do everything that needs to be done without having to question myself (P7). Other parents described their confidence by discussing how they accepted their situation or felt comfortable with it. I don’t know if you become more confident or you become more comfortable. I don’t know if the two are the same (P2). The confidence comes from just being comfortable in being in touch with your child … just being that person that knows your child better than anyone (P9).
Five parents described how being physically present with their child, learning more about their infant, or caring for their child helped calm their fears and contributed to growth in their confidence. The best way to keep him from coming back [to the hospital] is to educate the parent as best as you can … I think they did a really good job on that because I did feel confident. We did have some hiccups, but he hasn’t been hospitalized because of something I did wrong. He was hospitalized afterwards but it was getting to that time for him to have his surgery (P10). Parents described being confident because they believed were doing their best for their child.
Uncertainty and Growth of Confidence Regardless of whether parents described confidence as an emotional state of being or how they behaved, often parents felt uncertain about their level of confidence and described how confidence shifted depending on circumstances. Parents could easily describe moments when they felt certain and uncertain in their level of confidence. One mother talked about an upcoming appointment for her infant requiring sedation for an MRI, and although she had experience with her son undergoing surgery and other procedures, she stated, there’s a lot of factors that are terrifying, so I don’t know if its confidence or you just accept things as they come. You know we know the doctor and we know the questions to ask (P2). Another parent wondered if the uncertainty she felt as a parent resulted in a readmission to the hospital for her infant. Every day something new happens. Like when he was in the hospital for the two months, I felt like I failed him because I should have known something was wrong. I was like, “If I would have done things, he wouldn’t be here.” And everybody’s like, “No, you don’t know.” I have to remind myself that he is not like every other kid (P4). Even though this mother expressed uncertainty in her confidence, her confidence pattern reflected a stable high pattern throughout the study. Her infant also had consistently high technology dependence scores. Thus, this case example might be indicative of a mother who reports feeling confident in her overall caregiving ability but questions her personal sense of confidence when faced with a new challenge or stressor. Confidence for some parents may represent an overall feeling but not a stable one, my confidence has improved but I don’t know if it’s going to be completely be at 100%, ever (P2).
There were other factors that parents felt contributed to their confidence that were not indicative of their general feelings or behaviors. These included having other children, the difference between the experience of parenting within the hospital and outside of the hospital, and relationships with healthcare providers. Parents with other children expressed how different parenting was in the context of having a child with medical complexity and parenting in the hospital environment. Several noted they were comfortable with “basic” parenting skills like diapering, feeding, and soothing, but learning how to perform these skills in the hospital setting, or at home with additional equipment and technology, necessitated new skills to competently perform the task. One mother noted, We weren’t allowed to do whatever we wanted with her … we knew it was coming but it was still a little blindsiding cause you’re so used to being the absolute primary caregiving for your children … there are those things you take for granted when you have normally gestated children, it’s like co-parenting with eight other moms at the same time (P1). Parents described remastering basic parenting skills because everything was so different, it’s just as overwhelming if not more than having your first child (P2). In addition to feeling overwhelmed, the experience of hospitalization provoked a myriad of emotions such as fear, worry, and feelings of failure.
Parents reported that gaining confidence in their parenting role within the context of medical complexity was greatly improved with positive reassurance from nurses and opportunities for engagement in care activities. Parents mentioned how important nurses were because they answered questions, provided education, and helped parents feel comfortable in the hospital environment. Parents believed being present with their infant contributed to the infant’s progress. I really do believe that me being there, getting to know him and being a part of his care, helped him progress (P5). A few parents talked about the relationship they built with nursing staff. Parents were grateful for supportive relationships with nurses because they provided hope, were a source of comfort during crises, and helped them prepare for caring for their infant at home.
In addition to questions asked about confidence, parents were asked how the experience of having an infant hospitalized influenced them. Parents recognized positive outcomes both personally and for their family after the hospitalization. Parents expressed immense gratitude for the lifesaving measures used to save their child and the providers that cared for their child. Some parents saw their child as a source of strength and motivation to be the best possible parent, Seeing the strength babies can have. Because he would come back from a surgery with a smile on his face when he woke up. And seeing how strong he is helps me be strong (P4). This experience, be it good or bad has taught me a lot about myself. It’s taught me a lot about what I’m capable of doing, how to control my emotions and strengthened me to be stronger for [my baby] that I can do it. This is something that is not impossible (P6). Other parents discussed the positive outcomes for their family and others, I learned to have a lot more empathy for people (P3). Advocating and realizing that there’s healthcare needs that need research and just raising awareness (P6). To take one day at a time, it really opened my eyes to what others might be experiencing. I have learned to live each day like it’s the last day (P8). Parents described learning how to manage daily challenges and do the complex caregiving associated with their infant’s diagnosis. They found ways to incorporate caring for their child’s special needs into their daily routine. They recognized their infant’s milestones and growth, even if on a delayed developmental trajectory. Several parents described their experience as a positive one, this whole experience has taught me that every day is a gift. It’s a gift with [my baby], it’s a gift for us … this made me realize and appreciate just how fragile every moment is (P6).
DISCUSSION
Our study revealed that a parent’s sense of confidence and their belief in their ability to be successful in the parental role varies across situational challenges, especially with parenting an infant with complex care needs. These findings are consistent with the self-efficacy theory in that becoming an “expert” in parenting includes both belief in one’s own capacity and repeated exposure to engage in behaviors that allow the parent to become confident.23 Parenting confidence is both the belief that they can manage a treatment regime successfully and have the competence to engage in repeated caregiving behaviors. Confidence empowers parents to persevere with ongoing challenges and complex caregiving behaviors associated with unpredictable disease trajectories.
This study was one of the first to describe confidence patterns in a medically complex population. The majority of parents reported stable-high or increasing confidence, which is a normative parenting process, even in the midst of having a child with complex care needs. This is consistent with findings from Troutman et al24 in which mothers of irritable infants displayed higher levels of parenting self- efficacy over time. Therefore, a mother who effectively responds to her distress-prone infant in ways that calms her child (ie, the desired outcome) would in turn increase her sense of confidence. Parents whose confidence varied across time were also more likely to have scores below the clinical index, indicating clinically low confidence and in need of additional support. Despite reporting higher confidence at time of discharge, 2 parents were below the clinical cut-off after being home with their infant, even though their infant’s caregiving complexity scores had decreased substantially. While the reason for their low confidence is not known, maybe these parents experienced unexpected challenges in the first 3 months or there are other personal or family factors influencing lack of confidence that is not related to the infant.
Parents of medically complex infants may also underestimate their level of confidence. One study found that parents who focused more on their child’s health were less financially stable, had less education, and their infant had a new complex chronic condition when compared with parents who were more focused on spiritual well-being.25 This suggests focusing on the condition and overall health helped them cope by attending to the immediate needs of their child. Thus, it is important to consider that a greater sense of worry or difficulties in family or social support might be affecting their perception of confidence.
Parents described positive aspects of parenting an infant with medical complexity even though they sometimes felt uncertain about their level of confidence. Parents made meaning out of their situation by giving a positive value or outcome to their traumatic experience.26 These parents used positive reappraisal as a way to reframe their stressful experience. They attributed “meaning” to their experience by speaking about what they learned about themselves or how they gained a new perspective. These coping mechanisms are useful and successful adaptation techniques to manage to stressful experiences,27 and meaning-focused coping can further enhance confidence. Beighton and Wills28 found that parents of children with intellectual disability reported a greater sense of personal strength, more confidence, and increased appreciation for life. Families become resilient and learn to normalize these extra caregiving activities by incorporating them into daily routines.29 These findings offer further evidence that parents develop resiliency in the midst of medical challenges aided by nurses and other health professionals.
Our study findings revealed one of the most impactful experiences to parents was their relationship with nurses. Positive reassurance and opportunities for engagement in care activities encouraged by nurses positively influenced a parent’s sense of confidence.30 The additional caregiving time requires patience, expert knowledge, new skills, focused and attentive energy, and often means time away from other family members, such as a partner or siblings. Nurses are uniquely positioned to offer adaptive strategies to parents and can provide parents with caregiving expertise they need for their infants, and can provide emotional support to encourage the normalization process,31 but nurses also need to have the time and supportive work environments to accomplish this goal.32 It is important for parents to learn self-care and find a balance that is sustainable for themselves, their infant, and their family.
Infants with medical complexity may only have a slight decrease in their caregiving complexity at the time of discharge; thus, parents have to adapt how they manage their infant’s care in the home environment. Interaction with the healthcare system continues through infant follow-up clinics and various specialist appointments, so there are opportunities to identify and assess how parents are adapting and managing infant care. Screening of parents who may be at risk of having low confidence could be incorporated into the care plan both during and after hospitalization. Proactive identification of parents who may be at clinical risk for low confidence is likely to reduce the frequency of emergency department visits and potential hospitalizations.33 Clinicians could use this information to provide additional support to parents by way of peer-to-peer parent programs, a focused-needs assessment, and/or additional home health support. The ease with which a confidence measure can be administered makes it a useful tool in a variety of settings to screen parents as one indicator of parenting adaptability. Nurses, social workers, and discharge coordinators can be trained to assess parenting to provide focused emotional or social support to parents or connect them with community-based programs.34
Limitations
There are a few limitations to this study. There was only one father interviewed reducing the findings to primarily the mother’s perspective and did not include a diverse background of parenting contexts (eg, adolescents, adoptive, or multiple gestation births). Another limitation of this study is that self-esteem or other psychological factors were not measured in this study. Self-esteem is a strong predictor of confidence35 and exploring additional interpersonal factors, like self-esteem and social determinants, may help explain some of the individual variability noted in the patterns. Thus, more information is needed to understand factors that may have influenced why some parents continue to report low confidence even after being home with their infant. Future studies could focus on the father’s perspective, as they provide valuable insights when asked36 and explore additional intrapersonal factors to assess how confidence is developed in different contexts. More qualitative and mixed-methods studies are needed with larger samples to offer diverse perspectives from fathers, adoptive parents, and teenage parents, and to follow parents for a longer period. Future studies would also benefit from including infant health and developmental measures to better understand how confidence may be impacting infant health and development.
CONCLUSION
The current study is novel in its approach to understand how parents of infants with medical complexity describe feeling confident in their parenting role. The knowledge revealed in the findings, from the confidence trajectory patterns to the detailed parent descriptions of confidence, offers a comprehensive view of how parents gain a sense of confidence. Without doubt, parents of infants with medical complexity demonstrate resiliency amid challenges. Continued identification and support for parents to help them build their own capacity in the parenting role remains a top priority for healthcare providers and researchers.
What This Study Adds.
Description of parent confidence patterns among parents of infants with medical complexity.
Highlights how confidence may be situationally dependent.
Suggestions for future research related to understanding how parents develop different confidence patterns.
| Summary of Recommendations for Practice and Research | |
|---|---|
| What we know: |
|
| What needs to be studied: |
|
| What can we do today that would guide caregivers in the practice setting considering use of this evidence for guiding practice: |
|
Acknowledgments
This work was supported by grants from National Institute for Nursing Research at the National Institute of Health (F31-NR017101) and small grants from the National Association of Neonatal Nurses and Florida Association of Neonatal Nurse Practitioners.
Authors would like to acknowledge institutional support from the Duke University School of Nursing where this analysis occurred.
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Ashlee J. Vance, National Clinical Scholars Program, Institute for Healthcare Policy and Innovation, University of Michigan, and National Clinical Scholars Program, Institute Department of Systems, Populations, and Leadership, School of Nursing, University of Michigan School of Nursing, Ann Arbor;.
Kathleen Knafl, University of North Carolina at Chapel Hill School of Nursing, Chapel Hill;.
Debra H. Brandon, Department of Pediatrics, Duke University School of Nursing, and School of Medicine, Duke University, Durham, North Carolina..
References
- 1.Vazquez V, Cong X. Parenting the NICU infant: a meta-ethnographic synthesis. Int J Nurs Sci. 2014;1(3):281–290. [Google Scholar]
- 2.October TW, Fisher KR, Feudtner C, Hinds PS. The parent perspective: “being a good parent” when making critical decisions in the PICU. Pediatr Crit Care Med. 2014;15(4):291–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hagen IH, Iversen VC, Svindseth MF. Differences and similarities between mothers and fathers of premature children: a qualitative study of parents’ coping experiences in a neonatal intensive care unit. BMC Pediatr. 2016;16(92):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loewenstein K, Barroso J, Phillips S. The experiences of parents in the neonatal intensive care unit: an integrative review of qualitative studies within the transactional model of stress and coping. J Perinat Neonatal Nurs. 2019;33(4):340–349. [DOI] [PubMed] [Google Scholar]
- 5.Brandon DH, Tully KP, Silva SG, et al. Emotional responses of mothers of late-preterm and term infants. J Obstet Gynecol Neonatal Nurs. 2011;40(6):719–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belsky J, Jaffee SR. The Multiple Determinants of Parenting. In: Cicchetti D, Cohen DJ, eds. Developmental Psychopathology. 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc; 2015:38–85. [Google Scholar]
- 7.Berry JG, Hall DE, Kuo DZ, et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA Pediatr. 2011;305(7):682–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Russell CJ, Simon TD. Care of children with medical complexity in the hospital setting. Pediatr Ann 2014;43(7):e157–162. [DOI] [PubMed] [Google Scholar]
- 9.Benzies KM, Trute B, Worthington C. Maternal self-efficacy and family adjustment in households with children with serious disability. J Fam Stud. 2013;19(1):35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goudie A, Narcisse MR, Hall DE, Kuo DZ. Financial and psychological stressors associated with caring for children with disability. Fam Syst Health. 2014;32(3):280–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vance AJ, Brandon DH. Delineating among parenting confidence, parenting self-efficacy, and competence. ANS Adv Nurs Sci. 2017;40(4):E18–E37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ardelt M, Eccles JS. Effects of beliefs and promotive parenting strategies on inner-city youth. J Fam Issues. 2001;22(8):944–972. [Google Scholar]
- 13.Silver EJ, Heneghan AM, Bauman LJ, Stein RE. The relationship of depressive symptoms to parenting competence and social support in inner-city mothers of young children. Matern Child Health J. 2006;10(1):105–112. [DOI] [PubMed] [Google Scholar]
- 14.Kohlhoff J, Barnett B. Parenting self-efficacy: links with maternal depression, infant behaviour and adult attachment. Early Hum Dev. 2013;89(4):249–256. [DOI] [PubMed] [Google Scholar]
- 15.Vance AJ, Pan W, Malcolm WH, Brandon DH. Development of parenting self-efficacy in mothers of high-risk infants. Early Hum Dev 2020;141:104946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crncec R, Barnett B, Matthey S. Development of an instrument to assess perceived self-efficacy in the parents of infants. Res Nurs Health. 2008;31(5):442–453. doi: 10.1002/nur.20271 [DOI] [PubMed] [Google Scholar]
- 18.Docherty SL, Brandon D, Allen KA, Jones C, Miles M, Levy J. Development and Validation of the Pediatric Technology Dependence Scale. Presented at: 25th Annual Southern Nursing Research Society Conference; 2011; Jacksonville, Florida. [Google Scholar]
- 19.Teddlie C, Yu C. Mixed Methods Sampling. J Mixed Methods Res. 2007;1(1):77–100. [Google Scholar]
- 20.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. [DOI] [PubMed] [Google Scholar]
- 21.Morgan DL. Paradigms lost and pragmatism regained: methodological implications of combining qualitative and quantitative methods. J Mixed Methods Res. 2007;1(1):48–76. [Google Scholar]
- 22.Whittemore R, Chase S, Mandle CL. Validity in qualitative research. Qual Health Res. 2001;11(4):522–537. [DOI] [PubMed] [Google Scholar]
- 23.Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clin Psychol Rev. 2005;25(3):341–363. [DOI] [PubMed] [Google Scholar]
- 24.Troutman B, Moran TE, Arndt S, Johnson RF, Chmielewski M. Development of parenting self-efficacy in mothers of infants with high negative emotionality. Infant Mental Health J. 2012;33(1):45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feudtner C, Walter JK, Faerber JA, et al. Good-parent beliefs of parents of seriously ill children. JAMA Pediatr. 2015;169(1):39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park CL, Folkman S. Meaning in the context of stress and coping. Rev Gen Psychol 1997;1(2):115–144. [Google Scholar]
- 27.Hastings RP, Taunt HM. Positive perceptions in families of children with developmental disabilities. Am J Ment Retard. 2002;107(2):116–127. [DOI] [PubMed] [Google Scholar]
- 28.Beighton C, Wills J. Are parents identifying positive aspects to parenting their child with an intellectual disability or are they just coping? A qualitative exploration. J Intellect Disabil. 2017;21(4):325–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knafl KA, Deatrick JA, Knafl GJ, Gallo AM, Grey M, Dixon J. Patterns of family management of childhood chronic conditions and their relationship to child and family functioning. J Pediatr Nurs. 2013;28(6):523–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mooney-Doyle K, Dos Santos MR, Szylit R, Deatrick JA. Parental expectations of support from healthcare providers during pediatric life-threatening illness: a secondary, qualitative analysis. J Pediatr Nurs. 2017;36:163–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang Y, Wei M, Shen N, Zhang Y. Identifying factors related to family management during the coping process of families with childhood chronic conditions: a multi-site study. J Pediatr Nurs. 2015;30(1): 160–173. [DOI] [PubMed] [Google Scholar]
- 32.Hallowell SG, Rogowski JA, Lake ET. How nurse work environments relate to the presence of parents in neonatal intensive care. Adv Neonatal Care. 2019;19(1):65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coller RJ, Klitzner TS, Saenz AA, Lerner CF, Nelson BB, Chung PJ. The medical home and hospital readmissions. Pediatrics. 2015;136(6):e1550–1560. [DOI] [PubMed] [Google Scholar]
- 34.Amorim M, Alves E, Kelly-Irving M, Silva S. Needs of parents of very preterm infants in neonatal intensive care units: a mixed methods study. Intensive Crit Care Nurs. 2019;54:88–95. [DOI] [PubMed] [Google Scholar]
- 35.Leerkes E, Crockenberg S. The development of maternal self-efficacy and its impact on maternal behavior. Infancy. 2002;3(2):227–247. [DOI] [PubMed] [Google Scholar]
- 36.Hearn G, Clarkson G, Day M. The role of the NICU in father involvement, beliefs, and confidence: a follow-up qualitative study. Adv Neonatal Care 2020;20(1):80–89. [DOI] [PubMed] [Google Scholar]


