Abstract
Objectives:
Being a caregiver of an older adult is often associated with poor psychological outcomes and stress. Individual differences, such as personality, may moderate responses to caregiving. In this study, we examined (a) personality and psychological health of family caregivers compared to non-caregivers and (b) tested interactions between caregiver status and personality (both domains and facets) in predicting psychological outcomes.
Methods:
Data were from an online sample of caregivers of older relatives (N = 491; 71.9% females) and matched controls (N = 491). Participants completed the Big Five Inventory-2 and a comprehensive set of psychological health and well-being measures.
Results:
Compared to non-caregivers, caregivers had higher neuroticism, lower energy level (extraversion facet) and higher compassion (agreeableness facet). They also reported higher depression, anxiety, loneliness, and lower well-being and life satisfaction. Personality traits and facets had strong associations with psychological outcomes, and these associations were similar across the two groups. Only a few significant interactions between caregiver status and personality were found: For instance, higher neuroticism (in particular, higher scores on anxiety and depression facets) exacerbated anxiety among caregivers.
Conclusions:
Personality is a relevant correlate of psychological health. In the context of caregiving, its assessment may help to identify caregivers at risk of poor outcomes and inform intervention programs. Further research is needed to replicate the findings and investigate longitudinal interrelations among variables.
Keywords: caregivers, control group, older adults, personality traits and facets, psychological health
Family caregiving is an important component of care for older adults. It is estimated that about 14% (34 million) of Americans provide care for a middle aged or older adult with an illness, disability or memory problems (National Alliance for Caregiving, 2015). It is often a spouse or an adult child that assumes the role of caregiver to help the elder relative (the care-recipient) with self-care tasks, such as getting dressed, bathing or showering, transportation and management of medications and finances. Without this help, older adults would need to live in long-term care facilities or nursing homes.
Researchers and practitioners recognize the importance of family caregiving and the need to support their work. Many caregivers feel burdened by their responsibilities and family problems and experience negative psychological consequences (Schulz & Sherwood, 2008; Vitaliano, Strachan, Dansie, Goldberg, & Buchwald, 2014). For example, caregivers tend to report higher levels of perceived stress, anxiety and depressive symptoms, when compared to non-caregiver controls (see Lavela & Ather, 2010 and Pinquart & Sörensen, 2003 for reviews). This pattern is found for caregivers of patients across a number of health conditions, including cancer and dementia or other neurodegenerative syndromes (e.g., Kim et al., 2019; Livingston, Manela, & Katona, 1996; Mallya & Fiocco, 2018; Musich, Wang, Kraemer, Hawkins, & Wicker, 2017; Trevino, Prigerson, & Maciejewski, 2018).
However, there is considerable variability in the response to caregiving. That is, not all caregivers report poor psychological health (Roth et al., 2009) and some even report positive outcomes (e.g., Lynch, Shuster, & Lobo, 2018). For example, some caregivers derive a sense of gratification and satisfaction in their role (e.g., Noonan, Tennstedt, Rebelsky, 1996; Lynch et al., 2018; Metzelthin et al., 2017). Some feel confident in managing caregiving demands (for example, managing medical information or difficult interactions with the care-recipient) and experience less stress than others (Hajek & König, 2016; Hampton & Newcomb, 2018).
One of the factors that may contribute to this heterogeneity is personality—relatively stable patterns of thoughts, feelings and behaviors that characterize individuals across situations and time. Personality can be summarized along five broad dimensions, known as the “Big Five” traits (John, Naumann, & Soto, 2008; McCrae & Costa, 2008): neuroticism (i.e., being emotionally unstable), extraversion (i.e., being sociable and energetic/active), openness (i.e., being creative and open-minded), agreeableness (i.e., having compassion and willingness to cooperate), and conscientiousness (i.e., being organized and responsible). In line with diathesis-stress models (Ingram & Luxton, 2015; see also Vitaliano et al., 2014; Vitaliano, Young, Zhang, 2004), individual differences in these dimensions may modify (i.e., moderate) response to caregiving stress (Hajek & König, 2018a; Löckenhoff, Duberstein, Friedman, & Costa, 2011). That is, personality may be a pre-existing vulnerability (or resource) that interact with the experience of caregiving to contribute to greater (or less) distress. Neuroticism, for example, has been associated with psychological vulnerabilities and caregiving burden (e.g., Hoerger et al., 2016; Kang, Lee, Lee, & Kim, 2007; Kim, Duberstein, Sörensen, & Larson, 2005; Melo, Maroco & de Mendonça, 2011; Reis, Gold, Andres, Markiewicz, & Gauthier, 1994). For example, in a study with caregivers of dementia patients (n = 476), Kim and colleagues (2017) found higher neuroticism to be associated with elevated depressive symptoms and burden, and lower health-related quality of life. Other studies have also found that neuroticism is associated with more negative perceptions of the caregiving situation (Reis et al., 1994), higher sensitivity to caregiving demands and care-recipient behavior problems (Koerner & Kenyon, 2007), and worse perceived health (Hoerger et al., 2016; Löckenhoff et al., 2011). These results suggest that individuals higher in neuroticism may be more vulnerable to caregiving-related stress than individuals low on this trait.
In contrast to Neuroticism, other traits may be a resource that helps buffer the negative effects of caregiving. Extraversion and agreeableness have been associated with higher self-rated health and quality of life (Hoerger et al., 2016; Kim et al., 2017; Löckenhoff et al., 2011) and lower burden and depression in caregiver samples (Kim et al., 2017; Melo et al., 2011). As more sociable and compassionate, individuals higher on these traits may adapt better to the caregiver role and have access to social resources (e.g., family and friends support) that help to face caregiving demands (as suggested by Koerner, Kenyon, Shirai, 2009; see also Hajek & König, 2018a). Conscientiousness and openness have been associated with better outcomes (i.e., self-rated health) in response to difficult situations, including caregiving (Löckenhoff et al., 2011; Löckenhoff, Sutin, Ferrucci, & Costa, 2008). However, the association of these traits with caregiving outcomes is less consistent and varies across samples and outcome measures (Kim et al., 2017; Melo et al., 2011).
There are a number of ways the literature on caregivers’ personality and psychological health could be expanded to evaluate the hypothesized theoretical moderation model in Figure 1. First, most studies of family caregivers focus on a single dimension of personality (most often, neuroticism) and its association with depression or psychological symptoms. However, all five traits need to be considered and examined in relation to outcomes, other than depression/distress. For example, social isolation and feelings of loneliness are common among caregivers (e.g., McRae et al., 2009) in part because of restrictions imposed by their role (Vasileiou et al. 2017). Traits like neuroticism may exacerbate such feelings. Moreover, relatively little is known about how personality is associated with positive outcomes, such as caregivers’ well-being and life satisfaction (though see, Hajek & König, 2018a). Second, specific facets of the broad personality traits may be particularly relevant. Facets often have greater predictive power for specific behaviors and outcomes than their corresponding traits (Terracciano, Löckenhoff, Crum, Bienvenu, & Costa, 2008; Terracciano et al., 2009). In the context of caregiving, it is possible that facets that reflect an interpersonal or pro-social orientation (for example, the compassion facet of agreeableness or the sociability facet of extraversion) play an important role in psychological health and overall well-being. Third, research on personality and caregiving outcomes has relied almost exclusively on caregiving-only samples (though see Kim & Knight, 2018 and Hajek & König, 2018a). Without a comparison group, it is not possible to formally test which traits and facets of personality moderate the relation between caregiver status and psychological health. One exception is Hajek and König (2018a) who used a sample of caregivers and non-caregivers and found that higher agreeableness (but not other traits) attenuated the negative effect of caregiving on life satisfaction. This work should be extended to a more comprehensive measure of personality that includes facets as well as to additional measures of psychological distress and well-being. Finally, there might be differences in personality associated with caregiver status that may suggest a selection effect. For instance, a study found that individuals high in neuroticism were more likely to take over the responsibility to provide care for a relative/spouse in need (Rohr, Wagner, & Lang, 2013). Indeed individuals high in neuroticism may tend to select (or be selected into) situations that are negative or stressful for themselves (Barker, 2011; Kendler, Gardner, & Prescott, 2003).
Figure 1.
Hypothesized moderation model
To address the above research gaps and questions, the present study uses a case-control design to examine personality and psychological health among caregivers of older adult relatives and a matched control group. Using the Big Five Inventory-2 (BFI-2; Soto & John, 2017) and a comprehensive set of outcome measures, we first test for differences between the two groups. We hypothesize caregivers to score higher on most traits, particularly on neuroticism, and report poor psychological outcomes compared to controls—higher psychological symptoms (depression and anxiety) and loneliness and lower well-being and life satisfaction. Second, we examine personality in association with psychological health and its possible moderating role in the relation between caregiver status and psychological outcomes (see Figure 1). Based on the literature reviewed above, we hypothesize neuroticism to exacerbate psychological symptoms and feelings of loneliness among caregivers, while agreeableness and extraversion (particularly facets reflecting interpersonal or pro-social orientation) to attenuate caregiving negative consequences and promote well-being.
Methods
Participants and Procedure
A survey was distributed using Qualtrics Online Panels, a large company that offers participant recruitment services for researchers (www.qualtrics.com). Qualtrics panels has been successfully used in prior studies to target specific populations, such as family caregivers (e.g., Flood-Grady et al., in press). When signing up with Qualtrics, panel members provide information about themselves on many variables, including caregiving status. Based on these profiles, potential participants who meet inclusion criteria for a study are invited to participate and can choose to op-in, if interested. For the current study, the target population was n = 500 caregivers. Respondents were eligible if they were caring for a spouse or relative aged 60 years or older who suffered from a severe health condition, such as dementia, cancer or another long-term illness. To further verify caregiver status, the survey included two initial screening questions: “Are you currently taking care of a family member with a severe chronic health condition? [ ] Yes, [ ] No”, and “Is this family member… [ ] 60 years old or older, [ ] 59 years old or younger”. Only respondents who met the inclusion criteria proceeded to the survey. The survey included: (1) questions on respondent’s socio-demographic characteristics; (2) questions on the caregiving experience, the relation with the care-recipient and his/her condition; (3) self-report questionnaires of personality and psychological health outcomes (see below); and (4) an autobiographical memory task (participants recalled and rated an important personal memory). In addition to caregivers, we recruited a control group of non-caregivers to complete the survey; the survey and instructions were adapted for administration to control respondents (see survey flow, Figure S1, supplemental online material). The control group was matched to the caregiver group based on age (within a 5-year range) and sex and included a similar number of individuals with high school diploma or lower education as the caregiver group. In both groups, the questionnaires and memory task were counterbalanced across participants; on average, it took about 40 minutes to complete the survey.1 Respondents were compensated for their time directly by Qualtrics.
Immediately after data collection, responses were screened to identify invalid cases and careless respondents. For the caregiver group, 837 respondents met inclusion criteria and initiated the survey. Of these, 248 discontinued compilation and 86 were flagged as invalid (e.g., duplicates) or careless cases (e.g., respondents visualized the entire survey but did not respond to part of the questions). For the control group, 1,917 respondents initiated the survey. Of these respondents, 1,331 discontinued and 82 were flagged as invalid or careless. This resulted in 503 and 504 responses collected for the caregiver and control group, respectively. Prior to data analysis, a second quality check identified an additional 25 invalid cases to exclude from the analyses, 12 for the caregiver group and 13 for the control group. The final sample included 491 family caregivers and 491 non-caregiver controls. For the purpose of this study, we focused on personality and the psychological outcomes. Detailed information on response rates and data cleaning are provided in the online supplemental material (see Figure S2). The Institutional Review Board of the Florida State University approved all materials and procedures.
Measures
Personality
Participants completed the BFI-2 (Soto & John, 2017), a 60-item measure of five major personality traits and 15 specific facets: neuroticism (anxiety, depression, and emotional volatility), extraversion (sociability, assertiveness, energy level), openness (intellectual curiosity, aesthetic sensitivity, and creative imagination), agreeableness (compassion, respectfulness, trust), and conscientiousness (organization, productiveness, responsibility). Items (e.g., I am someone who... “Is outgoing, sociable” for extraversion) were rated on a scale from 1 (strongly disagree) to 5 (strongly agree). Every scale included 6 reverse-keyed items (2 for each facet scale). We computed means across items for each personality trait and corresponding facets; strait-line responses were excluded from analyses (n = 1 caregiver; n = 4 controls). Alpha reliabilities across traits ranged from .84 (agreeableness) to .91 (neuroticism) for the caregiver group, and from .82 (extraversion) to .91 (neuroticism) for the control group (median alpha for both groups = .85). For facets, alphas ranged from .60/.65 (intellectual curiosity facet of openness) to .82/.83 (depression facet of neuroticism), for caregivers/controls, respectively (median alpha = .73).
Psychological Outcomes
Symptoms of depression and anxiety.
All participants completed an 8-item version of the Patient Health Questionnaire (PHQ-8) and a 7-item version of the Generalized Anxiety Disorder (GAD-7) scale (Kroenke, Spitzer, Williams, & Löwe, 2010). PHQ-8 assesses the frequency of 8 depressive symptoms (e.g., “feeling tired or having little energy”) over the past 2 weeks with ratings from 0 (not at all) to 3 (nearly every day). GAD-7 measures common symptoms of anxiety (e.g., “feeling nervous, anxious, or on edge”) on the same response scale of the PHQ-8. Sum scores were computed for both PHQ-8 (range = 0-24) and GAD-7 (range = 0-21); higher scores indicated higher levels of depression and anxiety. Alpha reliability of PHQ-8 was ≥.88 and the reliability of GAD-7 was .93 for both caregivers and controls.
Loneliness.
Participants completed the 3-item version of the Revised-University of California at Los Angeles Loneliness scale (Hughes, Waite, Hawkley, & Cacioppo 2004). Each item (e.g. “How much of the time do you feel … isolated from others?) was rated from 1 (hardly ever or never) to 3 (often). A sum score was computed for this scale (range = 3-9); higher scores indicated feelings of loneliness. Alpha reliability was ≥.88 for the caregiver and control groups.
Well-being and life satisfaction.
The 8-item Flourishing Scale (FS; Diener et al., 2009), is an overall index of well-being and positive functioning, and the 5-item Satisfaction with Life Scale (SWLS; Kobau, Sniezek, Zack, Lucas, & Burns, 2010) measures satisfaction with life. Each item was rated on a scale from 1 (strongly disagree) to 5 (strongly agree). Sum scores were computed for FS (range = 8-40) and SWLS (range = 5-25); higher scores on these scales indicated higher levels of well-being and life satisfaction. In both groups, alpha reliabilities of FS and SWLS were respectively .89 and ≥.90.
Control Variables
Participants reported their age in years (continuous), sex, race/ethnicity (white vs. non-white), marital status (married or in a committed relationship vs. non-married), level of education (from 1 = “Did not complete high school degree” to 6 = “Professional degree or doctorate”), household income (from 1 = “less than $10,000”, 2 = “$10,00 to 19,999”, […], to 12 = “$150,000 or more”), and employment (employed vs. retired or unemployed). They also indicated age, sex and race/ethnicity and type of relationship with the care-recipient (i.e., whether he/she was a spouse, parent, sibling, or other). Caregiving-related variables were the main health condition for which the person required care, time spent as caregiver (number of years/months), whether the participant was living with the care-recipient, the number of hours of assistance per day, and tasks typically performed (e.g., whether he/she provided help in getting in/out of bad, getting dressed, bathing or showering, etc.; possible range 1-12).
Statistical Analysis
Descriptive statistics and frequencies were used to describe the caregiver and control groups, and t-tests and chi-square tests were used to compare the two groups on sociodemographic variables. We then examined personality and psychological health of family caregivers in comparison to non-caregivers. Specifically, we ran univariate analyses of covariance (ANCOVAs) with caregiver status (caregiver vs. non-caregiver) as the independent variable, each personality trait and corresponding facets as the dependent variables, and age, sex, race/ethnicity, marital status, education level, and household income, and employment as covariates. The assumption of homogeneity of variance was tested using the Levene statistic, and no violations were found. Effect sizes were estimated using partial η2; according to Cohen (1988), η2 values of .01, .06 and .14 correspond to small, medium and large effect sizes, respectively. The same analytic approach was used to test for differences between caregivers and controls for psychological symptoms (depression and anxiety), loneliness, well-being and life satisfaction; no large violation of the homogeneity assumption were observed for these analyses.
A second set of analyses examined personality association with psychological health and its possible moderating role on the relation between caregiving status and psychological outcomes. We first regressed each outcome on each personality trait and corresponding facet (entered separately), accounting for caregiver status and socio-demographic factors (age centered and squared, sex, race/ethnicity, marital status, education level, and household income, and employment). We then formally tested interactions by adding a product term between caregiver status and personality (caregiver status × trait/facet of interest) to predict each outcome. Interaction terms were computed with standardized scores. There was no evidence of multicollinearity (VIF values <.3.00). In sensitivity analyses, we examined personality associations with the outcomes in each group, separately; for the caregiver group, we controlled for caregiving-related variables in addition to socio-demographic factors.
Results
Sample Characteristics
Caregivers were primarily female (71.9%), older (M = 65.4, SD = 7.5, range = 22-95; 45.8% over the age of 65), white (91.4%), married or in a relationship (74.5%), with a bachelor degree or higher level of education (40.1%) and retired (55.2%) or unemployed (12.4%). Household income was between $30,000 and $39,999 for most caregivers. Fifty-two percent cared for a spouse/partner, 36.5% for a parent, 6.1% for a sibling, and 5.1% for another relative (e.g., parent-in-law, aunt, cousin). The mean length of time as caregiver was 8.4 years (median = 5 years). Caregivers provided an average of 11 hours of assistance a day; 70.5% lived with the care-recipient. The mean age of care-recipients was 77 years (range = 60-100); care-recipients were 48.5% males and 9.2% non-white. The health conditions for which they needed assistance were Alzheimer’s disease or other dementia (28.1%), cancer (13%), heart conditions (13.8%), lung diseases (7.7%), diabetes (11%), stroke (8.4%), other conditions such as multiple sclerosis and Parkinson’s disease (12.6%), or more than one conditions (5.3%). Secondary conditions were also reported (e.g., mobility problems); over 90% of care-recipients had at least one secondary health problem. Caregivers assisted their relative/spouse in a variety of tasks (M = 7.5, SD = 2.6), most commonly preparing meals and cleaning the house (~90%), assisting with transportation (~90%), bathing and getting dressed (~46%), managing medication (~70%), and finances (~84%).
Compared to controls, caregivers were more likely to be married or in a relationship (chi-square = 46.8, df = 1, p <.01; 74.8% caregivers vs. 53.9% controls had a spouse/partner) and less likely to identify with a race/ethnic group other than white (chi-square = 6.0, df = 1, p <.05; 8.6% caregivers vs. 13.4% controls were non-white). There were no other socio-demographic differences between the two groups.
Group Comparisons: Personality and Psychological Health
As showed in Table 1, there were very few significant differences between caregivers and controls in terms of personality. At the domain-level, caregivers had higher scores on neuroticism compared to non-caregivers. This difference extended to two of the three facets: caregivers scored higher on the anxiety and depression facets of this trait. There were no other domain-level differences. At the facet-level, caregivers scored higher on the compassion facet of agreeableness and lower on the energy level facet of extraversion. Caregivers tended to show emotional concerns for others’ well-being but were less active compared to non-caregivers. There were no other facet-level differences.
Table 1.
Comparisons between caregivers and controls
| Caregivers | Controls | ANCOVAs | ||||
|---|---|---|---|---|---|---|
| M | (SE) | M | (SE) | F | η 2 | |
| Personality traits | ||||||
| Neuroticism | 2.67 | (.04) | 2.47 | (.04) | 13.347*** | .01 |
| Extraversion | 3.16 | (.03) | 3.17 | (.03) | 0.116 | .00 |
| Openness | 3.66 | (.03) | 3.63 | (.03) | 0.598 | .00 |
| Agreeableness | 4.11 | (.03) | 4.05 | (.03) | 2.118 | .00 |
| Conscientiousness | 4.03 | (.03) | 4.08 | (.03) | 1.289 | .00 |
| Neuroticism facets | ||||||
| Anxiety | 3.10 | (.04) | 2.85 | (.04) | 14.878*** | .01 |
| Depression | 2.50 | (.04) | 2.23 | (.04) | 17.424*** | .02 |
| Emotional volatility | 2.41 | (.04) | 2.31 | (.04) | 2.541 | .00 |
| Extraversion facets | ||||||
| Sociability | 3.07 | (.05) | 2.98 | (.05) | 2.089 | .00 |
| Assertiveness | 3.21 | (.04) | 3.16 | (.04) | 0.730 | .00 |
| Energy level | 3.20 | (.04) | 3.40 | (.04) | 11.333*** | .01 |
| Openness facets | ||||||
| Intellectual curiosity | 3.68 | (.03) | 3.65 | (.03) | 0.372 | .00 |
| Aesthetic sensitivity | 3.55 | (.04) | 3.51 | (.04) | 0.365 | .00 |
| Creative Imagination | 3.76 | (.04) | 3.72 | (.04) | 0.517 | .00 |
| Agreeableness facets | ||||||
| Compassion | 4.30 | (.03) | 4.19 | (.03) | 5.325* | .01 |
| Respectfulness | 4.34 | (.03) | 4.33 | (.03) | 0.111 | .00 |
| Trust | 3.69 | (.04) | 3.63 | (.04) | 1.018 | .00 |
| Conscientiousness facets | ||||||
| Organization | 3.98 | (.04) | 4.03 | (.04) | 0.890 | .00 |
| Productiveness | 3.99 | (.03) | 4.05 | (.03) | 1.339 | .00 |
| Responsibility | 4.11 | (.03) | 4.15 | (.03) | 0.639 | .00 |
| Negative outcomes | ||||||
| Depressive symptoms | 6.19 | (.23) | 3.93 | (.23) | 46.251*** | .05 |
| Anxiety symptoms | 6.33 | (.24) | 3.30 | (.24) | 75.306*** | .07 |
| Loneliness | 5.37 | (.09) | 4.44 | (.09) | 54.913*** | .05 |
| Positive outcomes | ||||||
| Well-being | 31.12 | (.26) | 32.11 | (.26) | 6.838** | .01 |
| Life Satisfaction | 15.51 | (.24) | 17.00 | (.24) | 18.643*** | .02 |
Note. N = 969 for personality variables and N = 974 for psychological outcomes. For each variable, we reported estimated marginal means (standard errors), F statistics (degree of freedom, df = 1, 968/973), and effect sizes (η2) computed after controlling for age, sex, race/ethnicity, marital status, education level, household income and employment.
p ≤ .001
p ≤.01
p <.05.
There were differences between caregivers and controls on every measure of psychological health (Table 1).2 Specifically, caregivers reported more depressive symptoms, anxiety, and loneliness than non-caregivers. They also had lower well-being and life satisfaction.
Of note, differences between the two groups were small-to-medium in size; η2 values were ~.01 for personality variables and ~.06 for outcome measures.
Association between Personality Variables and Psychological Outcomes
Personality traits and facets were associated significantly with psychological outcomes (Table 2). In particular, higher Neuroticism was associated with higher scores on depression, anxiety, and loneliness and lower scores on well-being and life satisfaction, independent of caregiver status and socio-demographic covariates. In contrast, higher extraversion, agreeableness, conscientiousness and openness were associated with fewer symptoms of distress and higher well-being and life satisfaction. These traits were also associated with less feelings of loneliness. At the facet-level, all neuroticism facets were associated similarly with psychological outcomes. For the other domains, the strongest associations were observed for the energy level facet of extraversion, the trust facet of agreeableness, the responsibility and productivity facets of conscientiousness, and the creative imagination facet of openness (Table 2). Of note, when examining each group separately, regression coefficients were similar across caregivers and controls (see Table S1 and S2, supplemental material); for caregiver respondents, associations remained the same when further controlling for caregiving-related covariates, including whether caring for a patient with dementia versus other condition.
Table 2.
Association of personality traits and facets with psychological health outcomes
| Depression | Anxiety | Loneliness | Well-being | Satisfaction with life |
|
|---|---|---|---|---|---|
| Personality traits | |||||
| Neuroticism | .646*** | .650*** | .526*** | −.633*** | −578*** |
| Extraversion | −340*** | −.242*** | −.265*** | .486*** | .359*** |
| Openness | −.150*** | −.111*** | −.070* | .329*** | .157*** |
| Agreeableness | −264*** | −.210*** | −.231*** | .453*** | .289*** |
| Conscientiousness | −.296*** | −.181*** | −.211*** | .399*** | .265*** |
| Neuroticism facets | |||||
| Anxiety | .546*** | .622*** | .449*** | −.496*** | −.500*** |
| Depression | .678*** | .626*** | .580*** | −.689*** | −.643*** |
| Emotional volatility | .484*** | .470*** | .361*** | −.491*** | −.383*** |
| Extraversion facets | |||||
| Sociability | −.196*** | −.154*** | −.179*** | .303*** | .197*** |
| Assertiveness | −.177*** | −.123*** | −.128*** | .288*** | .225*** |
| Energy level | −.438*** | −.298*** | −.320*** | .565*** | .438*** |
| Openness facets | |||||
| Intellectual curiosity | −.141*** | −.095** | −.063* | .299*** | .137*** |
| Aesthetic sensitivity | −.060 | −.050 | .017 | .193*** | .082** |
| Creative Imagination | −.177*** | −.132*** | −.132*** | .334*** | .174*** |
| Agreeableness facets | |||||
| Compassion | −.149*** | −.096** | −.137*** | .327*** | .153*** |
| Respectfulness | −.233*** | −.173*** | −.178*** | .371*** | .209*** |
| Trust | −.274*** | −.247*** | −.255*** | .431*** | .346*** |
| Conscientiousness facets | |||||
| Organization | −.185*** | −.092** | −.120*** | .238*** | .176*** |
| Productiveness | −.294*** | −.171*** | −.220*** | .434*** | .292*** |
| Responsibility | −.294*** | −.216*** | −.215*** | .369*** | .218*** |
| Caregiver Status | .216*** | .272*** | .231*** | −.084** | −.138*** |
Note. N = 969 (caregiver group n = 486; control group n = 483). Standardized linear regression coefficients (βs) are reported; analyses controlled for caregiver status (caregiver vs. non-caregiver), age (centered and squared), sex, race/ethnicity, marital status, education level, household income, and employment. Analyses separated for each group are reported in the online supplemental material. In general, the associations between personality and outcome variables were similar across caregivers and controls (see Table S1 and S2).
p ≤ .001
p ≤.01
p <.05.
Only few significant interactions between caregiving and personality factors were observed in predicting psychological outcomes. One significant interaction was found between caregiving and domain-level neuroticism in predicting symptoms of anxiety (βCaregiver Status × Neuroticism = .074, p = .023). This interaction was also apparent for the anxiety facet (βCaregiver Status × Anxiety facet = .091, p = .006) and depression facet (βCaregiver Status × Depression facet = .071, p = .035) of neuroticism. That is, caregivers high on neuroticism—in particular, those high on the anxiety and depression facets—reported more symptoms of anxiety, compared to controls who scored similarly high on this trait (Figure 2; see also Figure S3, online supplemental material). In addition, we observed an interaction between caregiver status and the productiveness facet of conscientiousness in predicting life satisfaction (βCaregiver Status × Productivity facet = −.086, p = .047); even at high levels of productiveness, caregivers reported lower life satisfaction than controls (see Figure S3). This latter interaction was not hypothesized at priori and likely due to chance. No other significant interactions between caregiver status and personality domains nor facets were found.
Figure 2.
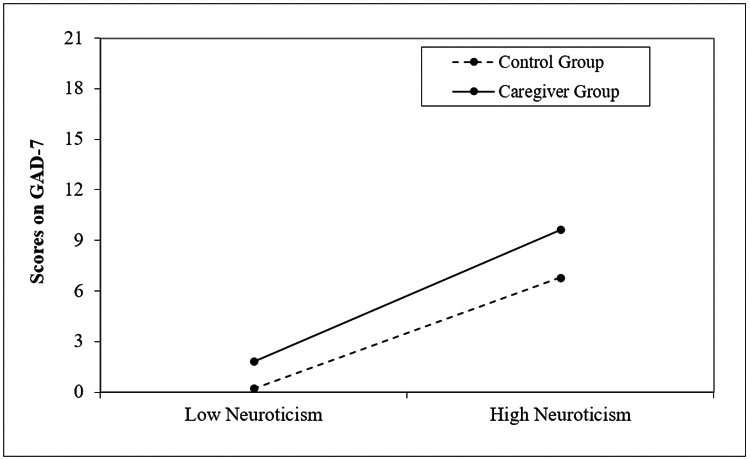
Neuroticism-moderating effects on anxiety symptoms
Discussion
The present research examined personality and psychological health in caregivers of older relatives and matched controls. As expected, we observed modest but significant differences between these two groups. Consistent with prior work (see Vitaliano et al., 2014), the experience of caregiving posed stress on the individual: Caregivers not only reported higher depression and anxiety, but also felt lonelier and had lower well-being and life satisfaction. There were also a few differences in personality, with caregivers being higher in neuroticism, lower in energy (extraversion facet), and higher in compassion (agreeableness facet) than non-caregivers.
Of note, personality had strong associations with psychological health outcomes. Participants high in neuroticism tended to report poor psychological health (e.g., higher depression/anxiety) compared to those low on this trait. In contrast, those high in extraversion (in particular, energy level), agreeableness (trust), conscientiousness (responsibility and productiveness), and openness (creative imagination), had more favorable outcomes (e.g., higher well-being and life satisfaction). This pattern of associations was similar to that observed in studies with both caregiver and non-caregiver adult samples (Löckenhoff et al., 2008, 2011).
Contrary to our expectations, most of these associations were independent of caregiver status. One exception, however, was observed for neuroticism. Between-person differences on this trait were hypothesized to have a negative association with caregivers’ response to stress (see e.g., Kim et al., 2017; Melo et al., 2011). Koerner and Kenyon (2007), for example, reported caregivers higher in neuroticism to be more sensitive to care-related demands and care-recipient behavior problems, compared to the low-neuroticism counterparts. Yet, this study (as others) did not include a comparison group. In the current work, caregivers high in neuroticism did report higher scores on anxiety relative to controls. However, this differential association was not observed for other outcomes. As such, we found only partial support to the hypothesis that neuroticism exacerbates the negative outcomes associated with caregiving.
Findings from prior studies indicated that prosocial dispositions—being more agreeable and oriented to others—is helpful for coping with difficult situations in general, and caregiving demands in particular (see e.g., Koerner et al., 2009). For example, caregivers higher in agreeableness and extraversion were found to be more satisfied with their role and with life than caregivers lower on these traits (see Hajek & König, 2018a; Koerner et al., 2009). In the current study, however, no significant interactions were observed between caregiver status and these traits.
It is important to note that the differences observed in personality between caregivers and controls may reflect selection effects. For example, when a spouse or other relative is in need, individuals high in neuroticism may be less likely to refuse care responsibilities and feel more obligated to assume the caregiver role (see Rohr et al., 2013). As hypothesized, we did observe higher scores on neuroticism for the caregiver group. There were, however, differences that we did not anticipate: Caregivers were higher on the compassion facet of agreeableness and lower on the energy level of extraversion. These differences could have existed prior to the caregiver role. Likewise, personality could have changed in response to caregiving (i.e., socialization effects; Hajek & König, 2018b; Hoerger et al., 2014). Because of the cross-sectional nature of the study, we cannot distinguish between selection and socialization effects.
A few additional limitations need to be noted. Specifically, this study targeted caregivers of older relatives, without any recruitment restrictions based on the type of relationship with the care-recipient nor the type and stage of illness. Caregiving-related stress and demands may vary in intensity based on these factors. More work is needed to study specific groups of caregivers (i.e., spousal vs. adult child caregivers) and their responses to different caregiving phases, from the moment of the care-recipient’s diagnosis, to later hospitalization, and transition out of caregiving. Moreover, we considered exclusively the caregiver. Caregiver personality and stress may also be associated with care-recipients’ health and outcomes. Longitudinal studies are needed to investigate temporal pathways and possible reciprocal influences among caregiver and care-recipients’ variables.
The current findings have both theoretical and clinical implications. From a theoretical perspective, personality is relevant for psychological health, independent of caregiver status. But, consistent with diathesis-stress models of caregiving (Vitaliano et al., 2004), some dispositions (i.e., neuroticism) may increase risk for poor outcomes (i.e., anxiety). From a clinical perspective, personality assessment may help to identify caregivers at risk of poor outcomes and inform interventions (see Chapman, Hampson, & Clarkin, 2014). That is, personality-informed interventions might be developed to support caregivers’ psychological health. For example, personalized messages or communications based on the individual personality profile may increase the effectiveness of psychosocial education programs directed to caregivers. Indeed, the effectiveness of various type of caregivers’ intervention could partly depend on personality (Terracciano et al., in press). For example, extroverts may adhere more and find more beneficial group-based programs while introverts could find uncomfortable or even detrimental for their well-being interventions in a group setting. Individuals who score low on openness may prefer traditional or religion-based programs. Individuals high in neuroticism are likely to benefit the most from interventions that enhance coping skills and other strategies to manage their emotions. Matching caregivers to the education program or intervention that is relevant to their individual vulnerabilities and resources means that the money spent delivering the program/intervention would have greater net benefit and cost effectiveness. In turn, it is likely that more “personalized care” for family caregivers would reduce costs for the health system that are associated with patients’ hospitalization and nursing home care.
Overall, this study applied a case-control design to examine personality profiles and psychological health among caregivers and considered facets of personality. Further studies are now needed to identify longitudinal associations between personality and psychological outcomes of caregivers.
Supplementary Material
Acknowledgments
Funding Details
This work was supported by the Institute for Successful Longevity, 2017 Planning Grant program, at the Florida State University. Investigators have also received support from the National Institute on Aging of the National Institutes of Health, Award Numbers R01AG053297 and R56AG064952. The content is solely the responsibility of the authors and does not necessarily represent the official views of funding agencies.
Footnotes
Disclosure Statement
No conflict of interest was reported by the authors.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
About 45% of the sample completed first the memory task and then the questionnaires. There were no order effects for outcome variables (t-tests, p >.05), except for life satisfaction (t(980) = 2.85, p = .004); those completing the memory task first had higher scoring in life satisfaction (M = 16.79, SD = 5.42) than those completing first the questionnaires (M = 15.81, SD = 5.31).
Note that most caregivers (N = 138/491) reported that the main reason for which their relative needed assistance was because he/she suffered from Alzheimer’s disease or another form of dementia. No differences in personality were observed based on the type of caregiving— dementia caregivers vs. other type of caregivers. Caregivers of dementia patients did report psychological distress compared to other caregivers and non-caregivers. That is, they scored higher on depression (F(2,973) = 32.103, p <.001, η2 = .06; M = 7.72 [SE = .43] for dementia caregivers, M = 5.59 [SE = .27] for other caregivers, and M = 3.94 [SE = .23] for non-caregivers), anxiety (F(2,973) = 42.497, p <.001, η2 = .08; M = 7.50 [SE = .45] for dementia caregiver, M = 5.87 [SE = .29] for other caregivers, and M = 3.31 [SE = .24] for non-caregivers), and loneliness (F(2,973) = 33.276, p <.001, η2 = .06; M = 5.84 [SE = .16] for dementia caregiver, M = 5.19 [SE = .10] for other caregivers, and M = 4.44 [SE = .09] for non-caregivers). There were no differences in well-being nor life satisfaction between dementia caregivers and other caregivers; however, both groups scored lower than non-caregivers on these measures.
Contributor Information
Martina Luchetti, Department of Behavioral Sciences and Social Medicine, College of Medicine, Florida State University, Tallahassee, USA
Antonio Terracciano, Department of Geriatrics, College of Medicine, Florida State University, Tallahassee, USA
Yannick Stephan, Euromov, University of Montpellier, Montpellier, France
Damaris Aschwanden, Department of Geriatrics, College of Medicine, Florida State University, Tallahassee, USA
Angelina R. Sutin, Department of Behavioral Sciences and Social Medicine, College of Medicine, Florida State University, Tallahassee, USA
References
- Barker DB (2011). Self‐selection for stressful experiences. Stress and Health, 27, 194–205. doi: 10.1002/smi.1325 [DOI] [Google Scholar]
- Chapman BP, Hampson S, & Clarkin J (2014). Personality-informed interventions for healthy aging: Conclusions from a National Institute on Aging work group. Developmental psychology, 50, 1426–1441. doi: 10.1037/a0034135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Diener E, Wirtz D, Tov W, Kim-Prieto C, Choi D, Oishi S, & Biswas-Diener R (2009). New measures of well-being: Flourishing and positive and negative feelings. Social Indicators Research, 39, 247–266. doi: 10.1007/978-90-481-2354-4_12 [DOI] [Google Scholar]
- Flood-Grady E, Neil JM, Paige SR, Lee D, Damiani RE, Hough D, ... & Krieger JL (in press). A pilot study determining comprehension and the acceptability of a cancer research study website for cancer patients and caregivers. Journal of Cancer Education. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek A, & König HH (2016). Informal caregiving and subjective well-being: Evidence of a population-based longitudinal study of older adults in Germany. Journal of the American Medical Directors Association, 17, 300–305. doi: 10.1016/j.jamda.2015.10.015 [DOI] [PubMed] [Google Scholar]
- Hajek A, & König HH (2018a). The relation between personality, informal caregiving, life satisfaction and health-related quality of life: Evidence of a longitudinal study. Quality of Life Research, 27, 1249–1256. doi: 10.1007/s11136-018-1787-6 [DOI] [PubMed] [Google Scholar]
- Hajek A, & König HH (2018b). Informal caregiving and personality: Results of a population-based longitudinal study in Germany. PloS One, 13, e0203586. doi: 10.1371/journal.pone.0203586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampton MM, & Newcomb P (2018). Self-efficacy and stress among informal caregivers of individuals at end of life. Journal of Hospice & Palliative Nursing, 20, 471–477. doi: 10.1097/NJH.0000000000000464 [DOI] [PubMed] [Google Scholar]
- Hoerger M, Chapman BP, Prigerson HG, Fagerlin A, Mohile SG, Epstein RM, ... & Duberstein PR (2014). Personality change pre-to post-loss in spousal caregivers of patients with terminal lung cancer. Social Psychological and Personality Science, 5, 722–729. doi: 10.1177/1948550614524448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoerger M, Coletta M, Sörensen S, Chapman BP, Kaukeinen K, Tu X, & Duberstein PR (2016). Personality and perceived health in spousal caregivers of patients with lung cancer: The roles of neuroticism and extraversion. Journal of Aging Research, 5659793. doi: 10.1155/2016/5659793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26, 655–672. doi: 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram RE, & Luxton DD (2005). Vulnerability-stress models. In Hankin B and Abela JR (Eds.), Development of psychopathology: A vulnerability-stress perspective (pp. 32–46). SAGE Publications, Inc. [Google Scholar]
- John OP, Naumann LP, & Soto CJ (2008). Paradigm shift to the integrative Big Five Trait Taxonomy. In John OP, Robins RW, & Pervin LA (Eds.), Handbook of personality: Theory and Research (pp. 114–158). London, NY: The Guilford Press. [Google Scholar]
- Kang JW, Lee JH, Lee DW, & Kim MJ (2007). Correlation between caregivers personality traits and burden in caregiver of dementia. Journal of the Korean Geriatrics Society, 11, 221–228. [Google Scholar]
- Kendler KS, Gardner CO, & Prescott CA (2003). Personality and the experience of environmental adversity. Psychological Medicine, 33, 1193–1202. doi: 10.1017/S0033291703008298 [DOI] [PubMed] [Google Scholar]
- Kim G, Allen RS, Wang SY, Park S, Perkins EA, & Parmelee P (2019). Caregiving roles and subjective physical and mental health status among older adults: Do racial/ethnic differences exist? The Gerontologist, 59, 499–508. doi: 10.1093/geront/gnx196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y, Duberstein PR, Sörensen S, & Larson MR (2005). Levels of depressive symptoms in spouses of people with lung cancer: Effects of personality, social support, and caregiving burden. Psychosomatics, 46, 123–130. doi: 10.1176/appi.psy.46.2.123 [DOI] [PubMed] [Google Scholar]
- Kim S, & Knight BG (2018). Caregiving subgroups differences in the associations between the resilience resources and life satisfaction. Journal of Applied Gerontology, 37, 1540–1563. doi: 10.1177/0733464816669804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SK, Park M, Lee Y, Choi SH, Moon SY, Seo SW, ... & Han SH (2017). Influence of personality on depression, burden, and health-related quality of life in family caregivers of persons with dementia. International Psychogeriatrics, 29, 227–237. doi: 10.1017/S1041610216001770 [DOI] [PubMed] [Google Scholar]
- Kobau R, Sniezek J, Zack MM, Lucas RE, & Burns A (2010). Well‐being assessment: An evaluation of well‐being scales for public health and population estimates of well‐being among US adults. Applied Psychology: Health and Well‐Being, 2, 272–297. doi: 10.1111/j.1758-0854.2010.01035.x [DOI] [Google Scholar]
- Koerner SS, & Kenyon DB (2007). Understanding “good days” and “bad days”: Emotional and physical reactivity among caregivers for elder relatives. Family Relations, 56, 1–11. doi: 10.1111/j.1741-3729.2007.00435.x [DOI] [Google Scholar]
- Koerner SS, Kenyon DB, & Shirai Y (2009). Caregiving for elder relatives: Which caregivers experience personal benefits/gains? Archives of Gerontology and Geriatrics, 48, 238–245. doi: 10.1016/j.archger.2008.01.015 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, & Löwe B (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. General Hospital Psychiatry, 32, 345–359. doi: 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- Lavela SL, & Ather N (2010). Psychological health in older adult spousal caregivers of older adults. Chronic Illness, 6, 67–80. doi: 10.1177/1742395309356943 [DOI] [PubMed] [Google Scholar]
- Livingston G, Manela M, & Katona C (1996). Depression and other psychiatric morbidity in carers of elderly people living at home. BMJ, 312, 153–156. doi: 10.1136/bmj.312.7024.153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch SH, Shuster G, & Lobo ML (2018). The family caregiver experience-examining the positive and negative aspects of compassion satisfaction and compassion fatigue as caregiving outcomes. Aging & Mental Health, 22, 1424–1431. doi: 10.1080/13607863.2017.1364344 [DOI] [PubMed] [Google Scholar]
- Löckenhoff CE, Duberstein PR, Friedman B, & Costa PT Jr (2011). Five-factor personality traits and subjective health among caregivers: The role of caregiver strain and self-efficacy. Psychology and Aging, 26, 592. doi: 10.1037/a0022209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löckenhoff CE, Sutin AR, Ferrucci L, & Costa PT Jr (2008). Personality traits and subjective health in the later years: The association between NEO-PI-R and SF-36 in advanced age is influenced by health status. Journal of Research in Personality, 42, 1334–1346. doi: 10.1016/j.jrp.2008.05.006 [DOI] [Google Scholar]
- Mallya S, & Fiocco AJ (2018). Impact of informal caregiving on cognitive function and well-being in Canada. International Psychogeriatrics, 30, 1049–1055. doi: 10.1017/S1041610217002605 [DOI] [PubMed] [Google Scholar]
- Melo G, Maroco J, & de Mendonça A (2011). Influence of personality on caregiver’s burden, depression and distress related to the BPSD. International Journal of Geriatric Psychiatry, 26, 1275–1282. doi: 10.1002/gps.2677 [DOI] [PubMed] [Google Scholar]
- McCrae RR, & Costa PT Jr. (2008). Empirical and theoretical status of the Five-Factor Model of personality traits. In Boyle GJ, Matthews G, Saklofske DH (Eds.), The SAGE Handbook of Personality Theory and Assessment: Personality Theories and Models (Vol. 1) (pp. 273–294). [Google Scholar]
- McRae C, Fazio E, Hartsock G, Kelley L, Urbanski S, & Russell D (2009). Predictors of loneliness in caregivers of persons with Parkinson’s disease. Parkinsonism & Related Disorders, 15, 554–557. doi: 10.1016/j.parkreldis.2009.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metzelthin SF, Verbakel E, Veenstra MY, Van Exel J, Ambergen AW, & Kempen GI (2017). Positive and negative outcomes of informal caregiving at home and in institutionalised long-term care: A cross-sectional study. BMC Geriatrics, 17, 232. doi: 10.1186/s12877-017-0620-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musich S, Wang SS, Kraemer S, Hawkins K, & Wicker E (2017). Caregivers for older adults: Prevalence, characteristics, and health care utilization and expenditures. Geriatric Nursing, 38, 9–16. doi: 10.1016/j.gerinurse.2016.06.017 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving and the AARP Public Policy Institute (2015). Caregiving in the U.S. 2015 – Focused Look at Caregivers of Adults Age 50+. Retrieved from: https://www.caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Care-Recipients-Over-50_WEB.pdf
- Noonan AE, Tennstedt SL, & Rebelsky FG (1996). Making the best of it: Themes of meaning among informal caregivers to the elderly. Journal of Aging Studies, 10, 313–327. doi: 10.1016/S0890-4065(96)90004-3 [DOI] [Google Scholar]
- Pinquart M, & Sörensen S (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250. doi: 10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Reis MF, Gold DP, Andres D, Markiewicz D, & Gauthier S (1994). Personality traits as determinants of burden and health complaints in caregiving. The International Journal of Aging and Human Development, 39, 257–271. doi: 10.2190/6LYN-YFWQ-P87D-MKWX [DOI] [PubMed] [Google Scholar]
- Rohr MK, Wagner J, & Lang FR (2013). Effects of personality on the transition into caregiving. Psychology and Aging, 28, 692–700. doi: 10.1037/a0034133 [DOI] [PubMed] [Google Scholar]
- Roth DL, Perkins M, Wadley VG, Temple EM, & Haley WE (2009). Family caregiving and emotional strain: Associations with quality of life in a large national sample of middle-aged and older adults. Quality of Life Research, 18, 679–688. 10.1007/s11136-009-9482-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, & Sherwood PR (2008). Physical and mental health effects of family caregiving. Journal of Social Work Education, 44, 105–113. doi: 10.5175/JSWE.2008.773247702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto CJ, & John OP (2017). The next Big Five Inventory (BFI-2): Developing and assessing a hierarchical model with 15 facets to enhance bandwidth, fidelity, and predictive power. Journal of Personality and Social Psychology, 113, 117–143. doi: 10.1037/pspp0000096 [DOI] [PubMed] [Google Scholar]
- Terracciano A, Artese A, Yeh J, Edgerton L, Granville L, Aschwanden D, ... & Katz P (2019). Effectiveness of Powerful Tools for Caregivers on caregiver burden and on care recipient behavioral and psychological symptoms of dementia: A randomized controlled trial. Journal of the American Medical Directors Association. doi: 10.1016/j.jamda.2019.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Crum RM, Bienvenu OJ, & Costa PT (2008). Five-Factor Model personality profiles of drug users. BMC psychiatry, 8, 22. doi: 10.1186/1471-244X-8-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Sutin AR, McCrae RR, Deiana B, Ferrucci L, Schlessinger D, ... & Costa PT Jr (2009). Facets of personality linked to underweight and overweight. Psychosomatic Medicine, 71, 682–689. doi: 10.1097/PSY.0b013e3181a2925b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevino KM, Prigerson HG, & Maciejewski PK (2018). Advanced cancer caregiving as a risk for major depressive episodes and generalized anxiety disorder. Psycho‐Oncology, 27, 243–249. doi: 10.1002/pon.4441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasileiou K, Barnett J, Barreto M, Vines J, Atkinson M, Lawson S, & Wilson M (2017). Experiences of loneliness associated with being an informal caregiver: A qualitative investigation. Frontiers in psychology, 8, 585. doi: 10.3389/fpsyg.2017.00585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Strachan E, Dansie E, Goldberg J, & Buchwald D (2014). Does caregiving cause psychological distress? The case for familial and genetic vulnerabilities in female twins. Annals of Behavioral Medicine, 47, 198–207. doi: 10.1007/s12160-013-9538-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitaliano PP, Young HM, & Zhang J (2004). Is caregiving a risk factor for illness? Current Directions in Psychological Science, 13, 13–16. doi: 10.1111/j.0963-7214.2004.01301004.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


