Abstract
Background:
Enhanced recovery protocols (ERPs) have been used to improve patient outcomes and resource utilization after surgery. These evidence-based interventions include patient education, standardized anesthesia protocols, and limited fasting, but their use among pediatric populations is lagging. We aimed to determine baseline recovery practices within pediatric surgery departments participating in an ERP implementation trial for elective inflammatory bowel disease (IBD) operations.
Methods:
To measure baseline ERP adherence, we administered a survey to a staff surgeon in each of the 18 participating sites. The survey assessed demographics of each department and utilization of 21 recovery elements during patient encounter phases. Mixed-methods analysis was used to evaluate predictors and barriers to ERP element implementation.
Results:
The assessment revealed an average of 6.3 ERP elements being practiced at each site. The most commonly practiced elements were using minimally invasive techniques (100%), avoiding intra-abdominal drains (89%), and ileus prophylaxis (72%). The preoperative phase had the most elements with no adherence including patient education, optimizing medical comorbidities, and avoiding prolonged fasting. There was no association with number of elements utilized and total number of surgeons in the department, annual IBD surgery volume, and hospital size. Lack of buy-in from colleagues, electronic medical record adaptation, and resources for data collection and analysis were identified barriers.
Conclusions:
Higher intervention utilization for IBD surgery was associated with elements surgeons directly control such use of laparoscopy and avoiding drains. Elements requiring system-level changes had lower use. The study characterizes the scope of ERP utilization and the need for effective tools to improve adoption.
Keywords: recovery, enhanced recovery, enhanced recovery protocol, inflammatory bowel disease, Crohn’s disease, ulcerative colitis
Introduction
Approximately 25% of patients with inflammatory bowel disease (IBD) present before the age of 181. Within five years, 5-34% of patients with pediatric onset Crohn’s disease (CD) and 7-20% of patients with ulcerative colitis (UC) will require surgical intervention2-9. If surgery is indicated, rates of postoperative complications are high secondary to underlying factors such as malnutrition and use of immunomodulators10-13. Given the propensity toward a complicated surgical course, standardized care implementing best practices is advised for any pediatric surgeon involved in the care of a patient with IBD.
Enhanced recovery protocols (ERPs) are a group of interventions established in the literature to improve outcomes, resource utilization, and satisfaction for patients undergoing surgery. Their goal is to minimize the physical, psychologic and physiologic insult while also hastening recovery14. Initially developed in adult populations for patients undergoing colorectal surgery, they have been found to decrease complications, length of stay, opioid use, and hospital costs14-20. The basic tenets of ERPs include perioperative patient education, limited fasting, euvolemic fluid resuscitation, early enteral intake and mobilization, and limited use of opioids. Elements span the pre-, intra-, and postoperative phases of care and involve care coordination among surgeons, anesthesiologists, and nursing providers. Further, ERPs require periodic audits for adherence and analysis of patient outcomes. Their adoption has been endorsed by leading professional organizations such as the American College of Surgeons (ACS) and Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), but challenges to adoption and implementation remain, particularly among pediatric surgeons21,22. A recent American Pediatric Surgeon Association (APSA) survey highlighted pediatric surgeons’ opinions regarding applicability of a pediatric specific ERP comprising 21 individual elements23. Of the respondents only 68% reported being moderately to extremely familiar with ERPs, and only 19% were currently implementing a complete ERP.
The lack of widespread ERP utilization among pediatric surgeons can be attributed to the significant amount of planning required and the barriers present to influence system-wide change24. In order to accelerate adoption of ERPs in children undergoing elective gastrointestinal surgery for IBD, our research team developed a multicenter implementation trial. The purpose of the current study is to conduct a baseline assessment of each participating site’s current adherence to recovery elements and identify barriers to implementation.
1. Materials and Methods
1.1. Study Design
This study was a mixed-methods baseline assessment of the 18 pediatric hospitals participating in a multicenter implementation trial (Figure 1). Each site is a member of the Pediatric Surgery Research Collaborative (PedSRC). A 50-item survey (Appendix A) was distributed through REDCap, an academic and internet-based data capture tool used for research studies, to each of the pediatric surgeon site leaders who routinely perform IBD surgery25,26. The survey was a mix of closed- and open-ended items including hospital and surgical department characteristics, interventions currently used for elective colorectal operations in IBD patients, and perceived barriers to implementing a standardized protocol for this cohort. The ERP elements being evaluated were previously agreed upon by a review of the literature and a modified Delphi process27. The study was evaluated by the Institutional Review Board at Ann & Robert H. Lurie Children’s Hospital of Chicago and considered exempt from review. The survey was distributed August 2018.
Fig. 1.

List of sites participating in the enhanced recovery protocol implementation trial in no particular order and their location.
1.2. Elements and Barriers
Surgical site leaders were asked to evaluate how often each of the 21 ERP elements were routinely utilized at their respective center, using 28 items of the survey. Redundancy was introduced to serve as an internal control for reported adherence. For instance, perioperative antibiotic administration was considered practiced if there was a protocol in place for preoperative administration and for appropriate intraoperative re-dosing. Adherence to an element was determined if the frequency of practice reached specific thresholds as defined in Appendix B. Response options for closed-ended items included a mixture of varying scales including 5-point Likert scales (1-Never to 5-Always) and percentage of utilization (0-100% by 20% increments). Other aspects of ERP implementation were surveyed, including if practices had an enhanced recovery coordinator. Low implementing institutions at this baseline assessment were defined as practicing less than 6 elements vs high implementers whom practiced 6 or more ERP elements. The baseline survey also measured whether sites collected data on elective IBD patients. Survey items included: participation in the National Surgical Quality Improvement Program, collection of data surrounding compliance with ERP elements, and specific clinical and patient reported outcomes. Response options were “yes” and “no”.
Barriers to implementation were identified through an open-ended question where site leaders were asked to identify hurdles to implementing a recovery protocol. The text responses were analyzed by two researchers who independently identified common themes and then met to reconcile any differences.
1.3. Data Analysis
Descriptive statistics for hospital characteristics, elements practiced, and barriers to implementation were calculated. Bivariate analyses (Pearson’s correlation, t-test, chi-square test) were performed to evaluate the association of hospital and surgical department characteristics with number of elements implemented. The software used for data analysis was SPSS 25 (Armonk, NY: IBM Corporation).
2. Results
2.1. Description of participating sites and element adherence
All of the 18 participating sites completed the 51-item survey. The average number of surgeons at the participating sites who performed elective bowel surgery in children with IBD was 5.7 (Standard Deviation (SD) 3.5), with 2.2 surgeons (SD 1.6) being in practice for less than five years. The participating hospitals had an average of 306 beds (SD 145) with n=14 (78%) being in major metropolitan areas and the remaining n=4 (22%) being in an urban setting. When considering baseline data collection, the survey showed 16 sites (89%) participated in the American College of Surgeons National Surgical Quality Improvement Program and only one site collected data on ERP compliance. Table 1 compares self-reported structural elements between low and high implementation sites.
Table 1.
Demographic information about the participating sites and bivariate analyses comparing low and high ERP sites.
| Practice Information | n | Low ERP (n=11) |
High ERP (n=7) |
p-value |
|---|---|---|---|---|
| Number of surgeons, M(SD) | 9.6 (5.3) | 10.3 (6.6) | 8.5 (2.5) | .431 |
| Number of surgeons in practice for less than 5 years, M(SD) | 2.2 (1.6 | 2.2 (1.7) | 2.2 (1.4) | .988 |
| Number of surgeons who operate on children with IBD electively, M(SD) | 5.7 (3.5) | 6.0 (3.5) | 5.4 (3.9) | .753 |
| Number of beds in the hospital, M(SD) | 306 (145) | 313.6 (169.1) | 295.4 (108.9) | .804 |
| Number of pediatric ICU patient beds, M(SD) | 36.2 (19.7) | 36.6 (24.3) | 35.7 (10.8) | .927 |
| Annual pediatric IBD surgery volume, M(SD) | 34.2 (28.2) | 36.2 (32.9) | 31 (20.8) | .712 |
| Hospital location | .605 | |||
| Major metropolitan | 14 (77.8%) | 9 (64.3%) | 5 (35.7%) | |
| Urban | 4 (22.2%) | 2 (50.0%) | 2 (50%) | |
| Hospital infrastructure | .017 | |||
| Free standing | 12 (66.7%) | 5 (41.7%) | 7 (58.3%) | |
| Wing within adult hospital | 6 (33%) | 6 (100%) | 0 (0%) | |
| Electronic medical record | .311 | |||
| Cerner | 9 (50%) | 5 (55.6%) | 4 (57.1%) | |
| EPIC | 8 (44.4%) | 6 (75.0%) | 2 (25.0%) | |
| Sunrise | 1 (5.6%) | 0 (0%) | 1 (100.0%) | |
| Surgical patients on a designated floor | .518 | |||
| Always | 4 (22.2%) | 3 (75.0) | 1 (25.0%) | |
| Mostly | 14 (77.8%) | 8 (57.1%) | 6 (42.9%) | |
| Urgency of surgeries performed for children with IBD | .120 | |||
| Mostly elective | 9 (50%) | 7 (77.8%) | 2 (22.2%) | |
| Mostly emergent | 2 (11.1%) | 0 (0%) | 2 (100%) | |
| Even proportion of elective/emergent | 7 (38.9%) | 4 (57.1%) | 3 (42.9%) | |
| Anesthesiology leader identified | .914 | |||
| Yes | 10 (55.6%) | 6 (60.0%) | 4 (40.0%) | |
| No | 8 (44.4%) | 5 (62.5%) | 3 (37.5%) | |
| Collect ERP compliance data | .231 | |||
| Yes | 2 (11.1%) | 2 (100%) | 0 (0%) | |
| No | 16 (88.9%) | 9 (56.3%) | 7 (43.8%) | |
| Pain team managed by anesthesia | .829 | |||
| Yes | 15 (83.3%) | 9 (60.0%) | 6 (40.0%) | |
| No | 3 (16.7%) | 2 (66.7%) | 1 (33.3%) | |
| Participation in a national surgical quality improvement program | .734 | |||
| Yes | 16 (88.9%) | 10 (62.5%) | 6 (37.5%) | |
| No | 2 (11.1%) | 1 (50.0%) | 1 (50.0%) |
ERP – Enhanced recovery protocol; Low ERP – implementation of <6 elements; High ERP – implementation of ≥6 elements
2.2. Surgeon factors associated with baseline ERP utilization
When surgery department level factors were evaluated there was no correlation with the total number of surgeons or the number of surgeons in practice <5 years and the number of elements implemented (r=0.350, p=0.15 and r=−0.402, p=0.09, respectively). There was no difference in the total number of surgeons who perform elective IBD surgery between the low and high implementing sites (6.0 vs 5.4, respectively, p=0.75).
2.3. Site-level factors associated with baseline ERP utilization
There was no significant difference in number of total or intensive care beds between low and high implementing sites. Further, there was no difference in average annual surgical volume between the two types of sites (Low – 36.2 cases vs High – 31.0 cases, p=0.71). However, all sites that were incorporated into an adult hospital were low implementers and a higher proportion (58%) of free-standing hospitals were high implementers (p=0.017).
2.4. Element adherence
The range of elements implemented at participating sites was 2-10 with a mean of 6.3 (SD 2.4). One site self-identified as being an ERP implementer and practiced only 5 elements. Five elements, not implemented by any of the sites, included: optimizing medical comorbidities, avoiding prolonged fasting, standardized anesthesia protocol, and having a patient advocate or liaison. All eight elements requiring anesthesia collaboration had <75% implementation. Nine out of the remaining thirteen elements relying solely on the surgical service were implemented by <75% of the sites. There were no preoperative interventions practiced at a rate >50% (Table 2). The most common preoperative element utilized was patient and family education (8 sites, 44%).
Table 2.
ERP element implementation frequency across 18 sites.
| Site | Preoperative Elements | Intraoperative Elements | Postoperative Elements | ||||||||||||||||||||||
| Patient Advocate Liaison |
Optimize Medical Comorbidities |
Avoid Prolonged Fasting |
Provider Education | Administer Non- Opioid Analgesia |
Patient and Family Education |
Preoperative Total | Standardized Anesthetic Protocol |
Hypothermia Prevention |
Thromboembolism Prophylaxis |
Pre-incision Antibiotic Prophylaxis |
Prevention of Nausea/Vomiting |
Avoiding Intra- abdominal Drains |
Minimally Invasive Techniques |
Intraoperative Total | Goal Directed/Near- Zero Fluid Therapy |
Audit Protocol Compliance |
Early oral Nutrition | Early Mobilization | Opioid-Sparing Pain Regimen |
Avoiding Foley Placement |
Avoiding Nasogastric Tubes |
Ileus Prophylaxis | Postoperative Total | Total Element Utilization | |
| 1 | - | - | - | - | - | - | 0 | - | - | - | - | - | ✓ | ✓ | 2 | - | - | - | - | - | - | - | - | 0 | 2 (10%) |
| 2 | - | - | - | - | - | - | 0 | - | - | ✓ | ✓ | - | - | ✓ | 3 | - | - | - | - | - | - | - | ✓ | 1 | 4 (19%) |
| 3 | - | - | - | - | - | - | 0 | - | - | - | - | ✓ | ✓ | ✓ | 3 | - | - | - | - | - | - | - | ✓ | 1 | 4 (19%) |
| 4 | - | - | - | - | - | - | 0 | - | - | - | - | ✓ | ✓ | ✓ | 3 | - | ✓ | - | - | - | - | - | - | 1 | 4 (19%) |
| 5 | - | - | - | - | - | - | 0 | - | - | - | ✓ | - | ✓ | ✓ | 3 | - | - | - | - | - | - | ✓ | - | 1 | 4 (19%) |
| 6 | - | - | - | - | - | - | 0 | - | - | - | - | ✓ | ✓ | ✓ | 3 | - | - | - | - | - | ✓ | - | ✓ | 2 | 5 (24%) |
| 7 | - | - | - | ✓ | - | - | 1 | - | - | - | ✓ | ✓ | ✓ | ✓ | 4 | - | - | - | - | - | - | - | - | 0 | 5 (24%) |
| 8 | - | - | - | - | - | - | 0 | - | - | ✓ | ✓ | - | ✓ | ✓ | 4 | - | - | - | - | - | ✓ | ✓ | - | 2 | 6 (29%) |
| 9 | - | - | - | - | - | ✓ | 1 | - | - | ✓ | ✓ | - | ✓ | ✓ | 4 | - | - | - | - | - | - | - | ✓ | 1 | 6 (29%) |
| 10 | - | - | - | - | - | ✓ | 1 | - | - | ✓ | ✓ | ✓ | - | ✓ | 4 | - | - | - | - | - | - | - | ✓ | 1 | 6 (29%) |
| 11 | - | - | - | - | ✓ | - | 1 | - | - | - | - | ✓ | ✓ | ✓ | 3 | - | - | - | - | - | - | ✓ | ✓ | 2 | 6 (29%) |
| 12 | - | - | - | - | - | ✓ | 1 | - | - | - | ✓ | ✓ | ✓ | ✓ | 4 | - | - | - | - | - | - | ✓ | ✓ | 2 | 7 (33%) |
| 13 | - | - | - | - | - | - | 0 | - | ✓ | ✓ | - | ✓ | ✓ | ✓ | 5 | - | - | - | - | - | - | ✓ | ✓ | 2 | 7 (33%) |
| 14 | - | - | - | - | - | ✓ | 1 | - | - | - | - | ✓ | ✓ | ✓ | 3 | - | - | ✓ | ✓ | - | ✓ | ✓ | ✓ | 5 | 9 (43%) |
| 15 | - | - | - | - | - | ✓ | 1 | - | - | ✓ | - | ✓ | ✓ | ✓ | 4 | - | - | - | - | ✓ | ✓ | ✓ | ✓ | 4 | 9 (43%) |
| 16 | - | - | - | - | - | ✓ | 1 | - | - | ✓ | - | - | ✓ | ✓ | 3 | - | - | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 6 | 10 (48%) |
| 17 | - | - | - | - | - | ✓ | 1 | - | - | ✓ | ✓ | - | ✓ | ✓ | 4 | - | - | - | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 10 (48%) |
| 18 | - | - | - | - | - | ✓ | 2 | - | - | - | ✓ | - | ✓ | ✓ | 3 | - | - | - | ✓ | ✓ | ✓ | ✓ | ✓ | 5 | 10 (48%) |
| Total Site Utilization | 0 (0%) | 0 (0%) | 0 (0%) | 1 (6%) | 2 (11%) | 8 (44%) | 0 (0%) | 1 (6%) | 8 (44%) | 9 (50%) | 10 (56%) | 16 (89%) | 18 (100%) | 0 (0%) | 1 (6%) | 2 (11%) | 4 (22%) | 4 (22%) | 7 (39%) | 10 (56%) | 13 (72%) | ||||
The intraoperative phase had the two most highly practiced elements, minimally invasive techniques such as laparoscopy (18 sites, 100%) and avoidance of intraperitoneal/perianastomotic drains (16 sites, 89%). Pre-incision antibiotic prophylaxis had an unexpected low utilization due to an absence of a protocol being in place for re-dosing during the operation. Only one site had an anesthesia protocol to prevent intraoperative hypothermia.
In the postoperative phase the third most common intervention was found, postoperative ileus prophylaxis (13 sites, 72%). This phase had the element that would require the most resources, audit protocol compliance, and only one site reported its use. Six of these eight interventions rely solely on the surgical service but still showed low implementation.
2.5. Barriers to implementation
The majority of respondents (n=15, 83%) reported that they perceive their organization to be committed or very committed to quality improvement (Table 3). Although the relationship was not statistically significant, sites that were “committed or very committed” implemented fewer ERP elements when compared to sites that were “somewhat committed” or “not committed” to ERPs (−1.6 elements, P=0.311). Furthermore, all but one site committed to QI was able to identify at least one barrier to implementation. The most commonly reported was buy-in from surgeon and anesthesia colleagues (n=9, 50%), resources for implementation (n=7, 39%), data collection and analysis (n=6, 33%), and electronic medical record adaptation (n=3, 17%) (Figure 2). Some site leaders further expanded on their concern of buy-in by citing resistant colleagues to be, “afraid of complications” and their institution to require a, “new culture” while, “aligning the vision” of QI.
Table 3.
Participating site demographics.
| Site | Total Element ERP Implementation |
Perceived Institutional Commitment to QI |
Colleague Resistant to ERP |
Total Surgeons in Practice |
Total Surgeons in Practice < 5 Years |
Total Surgeons Performing Elective IBD Surgery |
Total Beds in Hospital |
Total PICU Beds |
Annual IBD Surgical Volume |
Self- Identified ERP Adherence |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | Very Committed | No | 16 | 6 | 4 | 300 | 40 | 55 | No |
| 2 | 4 | Very Committed | No | 22 | 3 | 14 | 350 | 30 | 120 | No |
| 3 | 4 | Very Committed | Unsure | 8 | 3 | 8 | 310 | 35 | 10 | No |
| 4 | 4 | Not Committed | Unsure | 8 | 1 | 8 | 255 | 20 | 12 | No |
| 5 | 4 | Committed | Yes | 21 | 5 | 5 | 750 | 100 | 50 | No |
| 6 | 5 | Very Committed | Unsure | 6 | 1 | 6 | 90 | 20 | 7 | No |
| 7 | 5 | Very Committed | No | 4 | 1 | 4 | 175 | 12 | 10 | Yes |
| 8 | 6 | Committed | No | 3 | 1 | 3 | 400 | 18 | 35 | No |
| 9 | 6 | Very Committed | No | 9 | 1 | 9 | 250 | 30 | 20 | No |
| 10 | 6 | Committed | No | 12 | 1 | 3 | 350 | 50 | 50 | No |
| 11 | 6 | Committed | No | 5 | 2 | 2 | 220 | 48 | 30 | No |
| 12 | 7 | Very Committed | Unsure | 13 | 4 | 13 | 250 | 40 | 30 | No |
| 13 | 7 | Very Committed | Unsure | 8 | 2 | 8 | 379 | 50 | 40 | No |
| 14 | 9 | Somewhat Committed | No | 7 | 2 | 3 | 250 | 40 | 20 | No |
| 15 | 9 | Very Committed | No | 9 | 4 | 2 | 289 | 32 | 70 | No |
| 16 | 10 | Very Committed | Yes | 10 | 3 | 3 | 500 | 44 | 17 | No |
| 17 | 10 | Committed | Unsure | 8 | 0 | 6 | 200 | 24 | 35 | No |
| 18 | 10 | Somewhat Committed | Yes | 5 | 1 | 3 | 200 | 20 | 5 | No |
ERP – enhanced recovery protocol; IBD – inflammatory bowel disease; PICU – pediatric intensive care unit; QI – quality improvement
Fig 2.
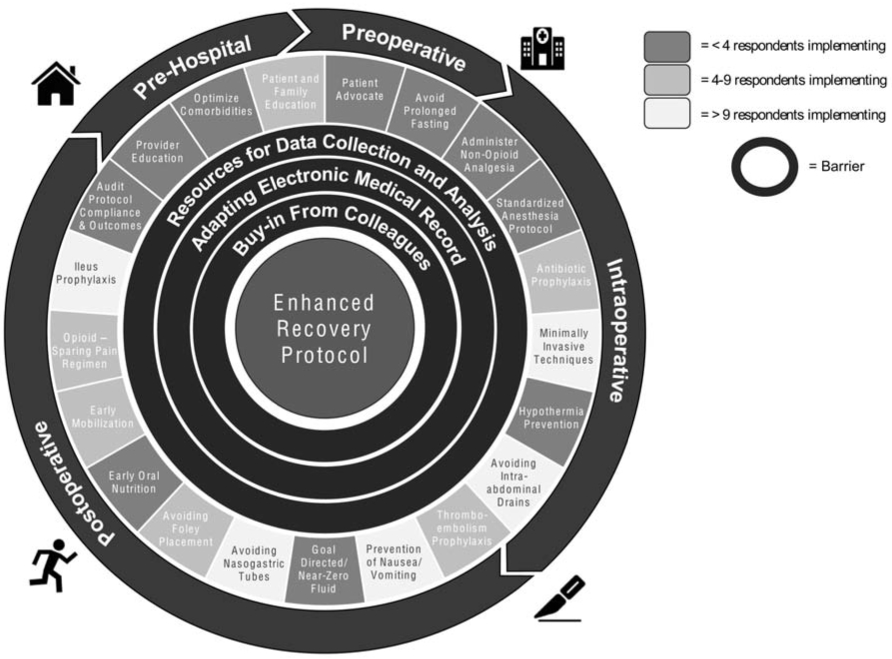
Baseline enhanced recovery protocol element implementation by patient encounter phase and associated barriers.
3. Discussion
Our baseline assessment of ERP use for children undergoing surgery for IBD at 18 sites participating in a planned prospective trial revealed variable adherence to specific elements ranging from ubiquitously endorsed use of minimally invasive techniques to lacking standardized protocols for key elements such as fasting guidelines and anesthetic care. These sites have significant heterogeneity in terms of surgical practices and staffing. Key hospital-level differences include urban versus rural setting, nesting of pediatric care within adult hospitals, and accessible infrastructure. Further, the surgical departments at the sites represent a wide range of total staff, elective IBD surgical volume, and resources available for quality improvement efforts. This heterogeneity of sites will provide a rich diversity of perspectives for the future prospective implementation trial. Furthermore, we have identified key facilitators and barriers to ERP implementation such as collection of reliable data and harnessing buy-in and support from colleagues and hospital leadership.
There were no sites implementing greater than half of the 21 ERP elements. This baseline level of recovery practice supports the need for an organized implementation intervention that will facilitate ERP adoption and adherence. The preoperative phase of a patient encounter had the least ERP baseline implementation and thus offers the most opportunity to design an intervention that partners with patients and their caregivers. The low adherence in the preoperative phase was expected due to these ERP elements needing more devotion of resources in the form of personnel or educational materials. ERP elements which require collaboration had low baseline implementation compared to ERP elements that relied solely on the efforts of the surgical team in isolation. This was noted across all phases of a patient encounter. This was most notable in the intraoperative phase where the interventions relying primarily on anesthesia had low implementation and interventions requiring few resources and primarily surgical decisions were practiced more.
There remains a significant barrier to surgeon buy-in for ERPs. The postoperative phase element adoption illustrates this well, when it was observed that four out of the six interventions which rely only on surgeon practice are utilized by less than half of the sites. This may be attributed to the historical dogma against their adoption and the hesitancy of colleagues to change practice. This is evidenced by the fact that although 10 sites (56%) avoided nasogastric tube use only 4 sites (22%) progressed to also allow early oral nutrition. The reported hurdles occur at multiple levels as defined by a socio-ecological model: intrapersonal, interpersonal, community, and policy24. Solutions will therefore need to be directed at each level. An intrapersonal target for modification includes individual attitudes toward ERPs, while an interpersonal focus for improvement would be identifying an anesthesia champion. A community level solution may involve surgical practice characteristics such as consolidating the number of surgeons performing IBD surgery. Lastly, a policy level solution encompasses gaining institutional buy-in and promoting awareness in the pediatric surgery field.
A previous study matched pediatric patients undergoing elective IBD surgery without ERPs to adult controls with ERPs and they found pediatric patients to have a three day longer length of stay, delay to regular diet, and delay to mobilization28. Similarly, in a retrospective review of a pediatric institution’s experience with implementing an ERP on IBD patients it was noted to decrease length of stay by two days, time to regular diet by one day, perioperative opioid use, and volume of intraoperative fluids29. Interestingly, over the two-year implementation period the median number of ERP interventions per patient increased from 5 to 11. This highlights the pragmatic workflow of instituting a new protocol. Some institutions will have the cultural agreement and resources to implement all elements at once, while others will only be able to start practicing a fraction of the recommended interventions and slowly adopt more recovery elements over time. This was expressed in the survey where one site leader commented, “we are moving forward with existing resources”.
One of the strengths of the upcoming implementation trial is the range of department- and hospital-level factors represented across the study sites. Although they are all tertiary centers, the variability lends itself to a generalizable cohort for which a robust quality improvement effort can be adopted by sites not currently in the trial. Further, it emphasizes the major gap in evidence-based solutions being practiced in elective IBD operations among pediatric surgeons. Although we were unable to elucidate associations of department and most hospital level factors with total adherence, this observation highlighted the deficiency of enhanced recovery being a focus for pediatric surgeons despite resources being available at select institutions.
The significance of this study is its focus on exploring barriers to and facilitators of implementation among surgical teams treating pediatric IBD patients. The aim of the next phase of the trial is to uncover details surrounding obstacles to ERP adoption, understand the rationale of poor compliance of elements, and institutional facilitators for sustainable implementation by conducting provider interviews. Identified barriers and facilitators are likely common to many of the participating sites given the overall low adherence. Another principal aim of the trial will be to uncover the number of elements needed to have an efficacious protocol. For instance, institutions practicing only five elements may not have alter their outcomes much compared to institutions with no ERP adoption, but when ten elements are able to be practiced, a significant improvement could be observed.
Next steps also include developing a toolkit to adapt ERPs to fit local contexts and thereby gain buy-in from both frontline clinicians and hospital leadership. This will, in turn, leverage support for full-time ERP staff and establish an environment devoted to quality improvement making future adherence to evidence-based solutions for valuable care more quickly accepted. The toolkit will comprise several instruments able to facilitate ERP implementation including patient- and family-centered counseling materials, pre- and postoperative order sets, defined ERP coordinator roles, and instructional videos on how to support early adopters and formalize inter-institutional communication for information sharing. Ultimately this multicenter effort will generate resources and an expanded evidence base for ERPs in children undergoing elective IBD surgery.
4. Conclusion
Despite results demonstrating the safety, shorter hospital length of stay, and improved outcomes associated with ERP use, ERP adherence is low and significant obstacles to ERP implementation remain. Obstacles include resistance to change from colleagues, lack of devoted personnel, and absence of analytic resources. There is a significant motivation to improve surgical recovery and when it is coupled with effective tools to overcome hurdles there will be a pronounced shift in practice patterns and most importantly, enhanced care.
Highlights.
Enhanced recovery principles have low rates of implementation among pediatric surgeons
Minimally invasive techniques (e.g. laparoscopy) have the highest utilization
Enhanced recovery elements in the preoperative phase have the lowest utilization
Elements requiring coordination between more than one department have low utilization
Acknowledgments
We want to thank the members of the Pediatric Surgery Research Collaborative (PedSRC) for contributing to this study.
This research was funded, in part, by the Crohn’s & Colitis Foundation's Litwin IBD Pioneers Award (Raval, Award Number 571096). NUCATS is funded in part by a Clinical and Translational Science Award (CTSA) grant from the National Institutes of Health (NIH), UL1TR001422.
Abbreviations:
- ERP
Enhanced recovery protocol
Appendix
Appendix A
Enhanced Recovery Survey Questions
-
1.Responder's information
- Name
- Hospital
- Title
-
2.
How many surgeons are in your practice? (please estimate)
-
3.
How many surgeons in your group have been in practice for less than 5 years? (please estimate)
-
4.
How many surgeons in your practice perform elective gastrointestinal tract surgery for children with inflammatory bowel disease (IBD)? (please estimate)
-
5.Please describe the hospital at which the enhanced recovery protocol study will be conducted. Select one answer for A - C separately.
- Major metropolitan area (Population >1,000,000) Urban (Population 50,000 - 999,999) Rural (Population < 50,000)
- Academic (Medical school affiliation and resident training) Non-academic (No affiliation and no training)
- Free standing children's hospital Children's wing within an adult hospital
-
6.
Roughly how many beds are in your hospital?
-
7.
Roughly how many pediatric intensive care unit (PICU) beds do you have?
-
8.Do you utilize an electronic medical record (EMR)?
- Yes
- No
-
8a.Please indicate the EMR.
- Epic
- Cerner
- Other
-
8b.
Please indicate the type of EMR that you use.
-
9.How often are your patients who undergo an elective operation for IBD cared for on the same surgical floor?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
10.Do you have a either a physical therapy or occupational therapy team in your hospital?
- Yes
- No
-
11.
Please estimate a range (e.g. 40-60) of how many surgical procedures are performed in children with IBD at your institution per year?
-
12.Describe the urgency of these operations.
- Mostly Elective
- Mostly Emergent
- Even proportion
-
13.For an elective total abdominal colectomy, what percent of your IBD patients would undergo a laparoscopic operation?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
14.Do you use an enhanced recovery protocol for pediatric patients undergoing elective IBD procedures?
- Yes
- No
-
14a.Do you have an enhanced recovery coordinator identified? This may include an alternative health care provider (e.g. nurse practitioner, physician assistant, or registered nurse).
- Yes, we have identified our enhanced recovery coordinator
- No, we have not identified our enhanced recovery coordinator
-
14aa.In which setting is the enhanced recovery coordinator responsible?
- Outpatient
- Inpatient
- Both
- Other
-
14ab.
In what other setting is the enhanced recovery coordinator responsible?
-
14b.Do you have a specific pediatric anesthesiologist who will work with you to implement an enhanced recovery protocol?
- Yes
- No
-
14c.Do you collect data on enhanced recovery protocol compliance?
- Yes
- No
-
15.Who usually writes the post-operative orders for your patients? Select one answer for A-D
- Attending
- Never
- Rarely
- Sometimes
- Mostly
- Always
- Resident
- Never
- Rarely
- Sometimes
- Mostly
- Always
- Alternative health care provider (e.g. nurse practitioner or physician assistant)
- Never
- Rarely
- Sometimes
- Mostly
- Always
- Other
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
15da.Enter the title of the other individual who usually writes the post-operative orders for your patients.
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
16.Does your institution have a pain team managed by anesthesia?
- Yes
- No
-
17.Who primarily manages postoperative pain? Select one answer for A-B.
- Surgery Team
- Never
- Rarely
- Sometimes
- Mostly
- Always
- Anesthesia/Pain Management Team
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
18.Do you participate in National Surgical Quality Improvement Program - Pediatric (NSQIP Peds)?
- Yes
- No
-
18a.Do you collect outcomes data on your elective IBD patients?
- Yes
- No
-
18b.Which outcomes do you measure? Please choose all that apply.
- Length of stay
- Wound complications (e.g. surgical site infection, wound dehiscence)
- Pneumonia
- Urinary tract infection
- Complication requiring non operative intervention (e.g. interventional radiology percutaneously draining fluid collection)
- Unplanned admission to the ICU
- Unplanned intubation
- Deep vein thrombosis
- Pulmonary embolism
- Unplanned blood transfusion
- Reoperation
- Mortality
- Readmission
- Other
-
18ba.
Enter the other outcomes that you measure.
-
19.Do you currently participate in ImproveCareNow?
- Yes
- No
-
20.What is your perception of your institution's overall commitment to quality improvement, i.e. would your administrators help facilitate implementation with resource allocation?
- Not Committed
- Somewhat Committed
- Neutral Committed
- Very Committed
-
21.Do you have a colleague resistant to implementing an enhanced recovery protocol for elective IBD patients?
- Yes
- No
- Unsure
-
22.
Describe any barriers you foresee for implementing an enhanced recovery protocol.
-
23.Is there an enhanced recovery checklist that follows the patient throughout their entire course of care including pre-operative planning in the clinic, pre-, intra-, and post-operative care in the hospital?
- Yes
- No
-
24.How frequently do you discuss discharge criteria with the patient and family prior to elective IBD operations?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
25.How often are cases delayed or cancelled due to a patient's poor nutritional status (e.g. low albumin)?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
26.Do you currently prescribe a mechanical bowel prep prior to elective IBD operations?
- Yes
- No
-
27.Do you currently prescribe an oral antibiotic bowel prep prior to elective IBD operations?
- Yes
- No
-
28.Does your institution currently allow a clear liquid diet up to 2 hours before the operation?
- Yes
- No
-
28a.How often do your elective IBD patients receive a carbohydrate load such as 20oz of Gatorade or juice 2 hours before the operation?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
29.How often do you administer non-opioid pre-operative analgesia? Examples include oral gabapentin and Tylenol in the pre-operative holding area.
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
30.Do you have a pain management team or specialist that would place regional blocks?
- Yes
- No
-
31.How often do you use sequential compression devices for children greater than age 12?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
32.Do you use pharmacologic venous thromboembolism (VTE) prophylaxis (e.g. subcutaneous heparin or lovenox) for elective IBD patients?
- Yes
- No
-
32a.When do you order the medication to be given?
- Preoperatively
- Postoperatively
- Both
-
33.Is there a protocol to decrease surgical site infection?
- Yes
- No
-
33a.How often do you administer pre-operative intravenous antibiotics less than one hour before incision?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
33b.Does a process exist to ensure antibiotics are re-dosed at appropriate time intervals?
- Yes
- No
-
33c.Is there a protocol in place to limit OR traffic to essential personnel?
- Yes
- No
-
33d.Is there a protocol for preoperative hand hygiene?
- Yes
- No
-
33e.Is there a protocol for sign in/time out/sign out?
- Yes
- No
-
33f.Do you have a standardized protocol for skin prep?
- Yes
- No
-
33g.What percent of the time are wound protectors used?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
33h.Is there a dedicated wound closure instrument tray?
- Yes
- No
-
33i.Does a protocol exist to ensure the operative team changes gowns and gloves prior to the start of the closure?
- Yes
- No
-
33j.Is there a protocol for irrigating the wound?
- Yes
- No
-
33k.Is there a sterile re-draping that happens prior to the start of closure?
- Yes
- No
-
33l.Is there a wound cleansing protocol for postoperative day 2-7 such as topical chlorhexidine or bacitracin?
- Yes
- No
-
34.Does your anesthesia team have a standardized intraoperative protocol for enhanced recovery?
- Yes
- No
-
34a.Do you have a specified normothermia protocol?
- Yes
- No
-
34b.Do you have a protocol in place to achieve a normal glucose range?
- Yes
- No
-
34c.Is there and standard protocol for induction agents and muscle relaxant?
- Yes
- No
-
34d.How often is an inhaled anesthetic used?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
34e.Is there a standardized ventilation strategy?
- Yes
- No
-
34f.What percent of your elective IBD cases have a near zero intra operative fluid balance?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
35.What percent of patients receive intraperitoneal drains after elective IBD operations?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
36.How often do you use nasogastric tubes after elective IBD operations?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
37.How often do you allow oral intake of clear liquids starting in the post anesthesia care unit and then advance diet as tolerated?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
38.Do you schedule anti-emetics postoperatively?
- Yes
- No
-
39.What percent of patients ambulate on postoperative day (POD) 0?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
40.What percent of patients participate in aggressive pulmonary toilet on POD 0?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
41.What percent of your patients undergoing elective IBD procedures have their Foley catheter removed on or before POD 1?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
42.What percent of patients receive non-opioids for first line pain control post-operatively?
- 0-20%
- 21-40%
- 41-60%
- 61-80%
- 81-100%
-
43.Which of the following strategies are utilized at your institution to prevent post-operative ileus? Choose all that apply.
- Gum chewing
- Protocol for electrolyte replacement
- Protocol for schedule laxatives
- Other
-
43a.
Enter the other strategy utilized at your institution to prevent post-operative ileus.
-
44.Do you cluster vitals, medicine administration, and other nursing care to allow for maximum sleep at night?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
45.How often do you contact the patient and/or caregiver (via phone, email or electronic chart communication) within one week of discharge?
- Never
- Rarely
- Sometimes
- Mostly
- Always
-
46.When do you typically have patients with elective IBD operations follow up in clinic after discharge?
- <1week
- 1-2 weeks
- 2-3 weeks
- 3-4 weeks
- > 4 weeks
-
47.How often would you like to receive feedback on enhanced recovery outcomes and compliance?
- Weekly
- Monthly
- Quarterly
- Semi-annually
-
48.Who do you envision will be collecting data for the enhanced recovery protocol study? Choose all that apply.
- Enhanced recovery coordinator
- Research resident
- Student
- Nurse
- Research coordinator from the hospital
- Other
-
48a.
Enter the title of the other individual who will be collecting data for the enhanced recovery protocol study.
-
49.Please rank the following enhanced recovery protocol outcomes in order of how important they are to you, with 9 representing the lowest importance and 1 the highest importance.
- Length of Stay
- Lower resource utilization
- Wound infection rate
- >Opioid utilization
- Readmision rate
- Patient reported outcomes
- Return to baseline activity
- Reoperation rate
- Standardization of care
-
49a.
If there is another enhanced recovery protocol outcome you feel is important, enter it here.
-
49b.
Indicate how you would rank the additional outcome that you entered, with 9 representing the lowest importance and 1 the highest importance.
-
50.
Do you have any concerns or comments for us as we begin the enhanced recovery protocol study?
Appendix B
| Element | Survey Code Requirement |
|---|---|
| 1. Patient and Family Education and Engagement | 24(Always) |
| 2. Patient Advocate Liaison (PAL) | 14a(Y) + 14aa(Both) |
| 3. Provider Education | 14a(Y) |
| 4. Optimize medical comorbidities | 25(Always) + 34b(Y) |
| 5. Avoid prolonged fasting | 28(Y) + 28a(Always) |
| 6. Administer non-opioid analgesia | 29(Always) |
| 7. Venous thromboembolism prophylaxis | 31(Always) |
| 8. Pre-incision antibiotic prophylaxis | 33a(Always) + 33b(Y) + 33f(Y) |
| 9. Standardized anesthetic protocol | 14b(Y) + 34(Y) + 34c(Y) + 34f(81-100%) |
| 10. Surgical procedure (i.e. minimally invasive techniques) | 13(81-100%) |
| 11. Prevention of nausea/vomiting | 38(Y) |
| 12. Avoiding nasogastric tubes | 36(0-20%) |
| 13. Standardized hypothermia prevention | 34a(Y) |
| 14. No intraperitoneal/perianastomotic drains | 35(0-20%) |
| 15. Goal directed/near-zero fluid therapy | 34f(81-100%) |
| 16. Avoiding or early removal of urinary drains | 41(81-100%) |
| 17. Prevention of ileus through gut stimulation | 43(Any box checked) |
| 18. Opioid sparing pain regimen | 30(y) + 42(81-100%) |
| 19. Early oral nutrition | 37(Always) |
| 20. Early mobilization | 39(81-100%) |
| 21. Audit protocol compliance/outcomes | 14c(Y) + 18a(Y) + 23(Y) |
Footnotes
This work was presented at the 2019 Crohn’s & Colitis Foundation Investigators Research Symposium and the 3rd Annual ERAS USA Conference.
The authors have no financial or personal disclosures or conflicts of interest.
Level of Evidence: Level III
Type of Study: Mixed-methods Survey
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kelsen J, Baldassano RN. Inflammatory bowel disease: the difference between children and adults. Inflamm Bowel Dis. 2008;14 Suppl 2:S9–11. doi: 10.1002/ibd.20560 [DOI] [PubMed] [Google Scholar]
- 2.Adamiak T, Walkiewicz-Jedrzejczak D, Fish D, et al. Incidence, clinical characteristics, and natural history of pediatric IBD in Wisconsin: a population-based epidemiological study. Inflamm Bowel Dis. 2013;19(6):1218–1223. doi: 10.1097/MIB.0b013e318280b13e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benchimol EI, Mack DR, Nguyen GC, et al. Incidence, outcomes, and health services burden of very early onset inflammatory bowel disease. Gastroenterology. 2014;147(4):803–813.e7; quiz e14-15. doi: 10.1053/j.gastro.2014.06.023 [DOI] [PubMed] [Google Scholar]
- 4.Vernier-Massouille G, Balde M, Salleron J, et al. Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology. 2008;135(4):1106–1113. doi: 10.1053/j.gastro.2008.06.079 [DOI] [PubMed] [Google Scholar]
- 5.Malmborg P, Grahnquist L, Ideström M, et al. Presentation and progression of childhood-onset inflammatory bowel disease in Northern Stockholm County. Inflamm Bowel Dis. 2015;21(5):1098–1108. doi: 10.1097/MIB.0000000000000356 [DOI] [PubMed] [Google Scholar]
- 6.Nordenvall C, Rosvall O, Bottai M, et al. Surgical Treatment in Childhood-onset Inflammatory Bowel Disease–A Nationwide Register-based Study of 4695 Incident Patients in Sweden 2002-2014. J Crohns Colitis. 2018;12(2):157–166. doi: 10.1093/ecco-jcc/jjx132 [DOI] [PubMed] [Google Scholar]
- 7.Gower-Rousseau C, Dauchet L, Vernier-Massouille G, et al. The natural history of pediatric ulcerative colitis: a population-based cohort study. Am J Gastroenterol. 2009;104(8):2080–2088. doi: 10.1038/ajg.2009.177 [DOI] [PubMed] [Google Scholar]
- 8.Malaty HM, Abraham BP, Mehta S, Garnett EA, Ferry GD. The natural history of ulcerative colitis in a pediatric population: a follow-up population-based cohort study. Clin Exp Gastroenterol. 2013;6:77–83. doi: 10.2147/CEG.S40259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larsen MD, Qvist N, Nielsen J, Kjeldsen J, Nielsen RG, Nørgård BM. Use of Anti-TNFα Agents and Time to First-time Surgery in Paediatric Patients with Ulcerative Colitis and Crohn’s Disease. J Crohns Colitis. 2016;10(6):650–656. doi: 10.1093/ecco-jcc/jjw017 [DOI] [PubMed] [Google Scholar]
- 10.Amil-Dias J, Kolacek S, Turner D, et al. Surgical Management of Crohn Disease in Children: Guidelines From the Paediatric IBD Porto Group of ESPGHAN. J Pediatr Gastroenterol Nutr. 2017;64(5):818–835. doi: 10.1097/MPG.0000000000001562 [DOI] [PubMed] [Google Scholar]
- 11.Fehmel E, Teague WJ, Simpson D, et al. The burden of surgery and postoperative complications in children with inflammatory bowel disease. J Pediatr Surg. 2018;53(12):2440–2443. doi: 10.1016/j.jpedsurg.2018.08.030 [DOI] [PubMed] [Google Scholar]
- 12.Nguyen GC, Elnahas A, Jackson TD. The impact of preoperative steroid use on short-term outcomes following surgery for inflammatory bowel disease. J Crohns Colitis. 2014;8(12):1661–1667. doi: 10.1016/j.crohns.2014.07.007 [DOI] [PubMed] [Google Scholar]
- 13.Zimmerman LA, Zalieckas JM, Shamberger RC, Bousvaros A. Postoperative complications of pediatric patients with inflammatory bowel disease treated with vedolizumab. J Pediatr Surg. 2018;53(7):1330–1333. doi: 10.1016/j.jpedsurg.2017.12.001 [DOI] [PubMed] [Google Scholar]
- 14.Varadhan KK, Lobo DN, Ljungqvist O. Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin. 2010;26(3):527–547, x. doi: 10.1016/j.ccc.2010.04.003 [DOI] [PubMed] [Google Scholar]
- 15.Gustafsson UO, Scott MJ, Schwenk W, et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37(2):259–284. doi: 10.1007/s00268-012-1772-0 [DOI] [PubMed] [Google Scholar]
- 16.Nygren J, Thacker J, Carli F, et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37(2):285–305. doi: 10.1007/s00268-012-1787-6 [DOI] [PubMed] [Google Scholar]
- 17.Miller TE, Thacker JK, White WD, et al. Reduced length of hospital stay in colorectal surgery after implementation of an enhanced recovery protocol. Anesth Analg. 2014;118(5):1052–1061. doi: 10.1213/ANE.0000000000000206 [DOI] [PubMed] [Google Scholar]
- 18.Thiele RH, Rea KM, Turrentine FE, et al. Standardization of care: impact of an enhanced recovery protocol on length of stay, complications, and direct costs after colorectal surgery. J Am Coll Surg. 2015;220(4):430–443. doi: 10.1016/j.jamcollsurg.2014.12.042 [DOI] [PubMed] [Google Scholar]
- 19.Stone AB, Grant MC, Pio Roda C, et al. Implementation Costs of an Enhanced Recovery After Surgery Program in the United States: A Financial Model and Sensitivity Analysis Based on Experiences at a Quaternary Academic Medical Center. J Am Coll Surg. 2016;222(3):219–225. doi: 10.1016/j.jamcollsurg.2015.11.021 [DOI] [PubMed] [Google Scholar]
- 20.Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M. Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531–1541. doi: 10.1007/s00268-013-2416-8 [DOI] [PubMed] [Google Scholar]
- 21.Ban KA, Gibbons MM, Ko CY, Wick EC. Surgical Technical Evidence Review for Colorectal Surgery Conducted for the AHRQ Safety Program for Improving Surgical Care and Recovery. J Am Coll Surg. 2017;225(4):548–557.e3. doi: 10.1016/j.jamcollsurg.2017.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carmichael JC, Keller DS, Baldini G, et al. Clinical Practice Guidelines for Enhanced Recovery After Colon and Rectal Surgery From the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum. 2017;60(8):761–784. doi: 10.1097/DCR.0000000000000883 [DOI] [PubMed] [Google Scholar]
- 23.Short HL, Taylor N, Thakore M, et al. A survey of pediatric surgeons’ practices with enhanced recovery after children’s surgery. J Pediatr Surg. 2018;53(3):418–430. doi: 10.1016/j.jpedsurg.2017.06.007 [DOI] [PubMed] [Google Scholar]
- 24.Gramlich LM, Sheppard CE, Wasylak T, et al. Implementation of Enhanced Recovery After Surgery: a strategy to transform surgical care across a health system. Implement Sci. 2017;12(1):67. doi: 10.1186/s13012-017-0597-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Short HL, Taylor N, Piper K, Raval MV. Appropriateness of a pediatric-specific enhanced recovery protocol using a modified Delphi process and multidisciplinary expert panel. J Pediatr Surg. 2018;53(4):592–598. doi: 10.1016/j.jpedsurg.2017.09.008 [DOI] [PubMed] [Google Scholar]
- 28.West MA, Horwood JF, Staves S, et al. Potential benefits of fast-track concepts in paediatric colorectal surgery. J Pediatr Surg. 2013;48(9):1924–1930. doi: 10.1016/j.jpedsurg.2013.02.063 [DOI] [PubMed] [Google Scholar]
- 29.Short HL, Heiss KF, Burch K, et al. Implementation of an enhanced recovery protocol in pediatric colorectal surgery. J Pediatr Surg. 2018;53(4):688–692. doi: 10.1016/j.jpedsurg.2017.05.004 [DOI] [PubMed] [Google Scholar]


