Abstract
Introduction
A calculator estimating likelihood of vaginal birth after cesarean (VBAC) has been promoted by the Society for Maternal and Fetal Medicine (SMFM) but little is known about how it is used and perceived in practice. Cut-offs for prohibiting labor after cesarean are discouraged by its developers, but such uses may be widespread. The purpose of this study was to determine how calculators predicting VBAC are used and perceived in midwifery practices.
Method
Certified nurse-midwives and certified midwives currently providing labor after cesarean care were surveyed between 1/17/19 and 2/7/19. Quantitative and text data were collected regarding the uses and perceptions of calculators among midwives and their colleagues. We compared these findings to midwives’ perceptions of their ability to accommodate patient wishes for labor after cesarean. We used descriptive content analysis to evaluate themes occurring in text responses.
Results:
There were 1305 valid responses. A requirement to use calculator scores for patient counseling was reported by 527 (40.4%) of responding midwives. Over 1 in 5 midwives reported scores were used to discourage or prohibit labor after cesarean. Almost half reported some or strong disagreement with physician colleagues regarding calculator use. Inter-professional agreement and disagreement centered on how scores are used to direct clinical care or restrict patient options. Calculator scores were used in more than twice as many midwives’ practices to discourage rather than encourage labor after cesarean. Descriptive analysis of text revealed 4 themes regarding calculators: Inconsistent Use, Information Counseling, Informed Consent, and Influence Patient Management or Options
Discussion:
Calculators predicting likelihood of VBAC success are widely used in midwifery settings and are more often used to discourage than encourage labor after cesarean. Midwives reported both directive and non-directive counseling based on calculator scores.
Precis.
Calculators predicting likelihood of vaginal birth after cesarean are widely used in midwifery practices, and more often to discourage than encourage labor after cesarean.
INTRODUCTION
Low rates of vaginal birth after cesarean (VBAC) are important modifiable contributors to high cesarean rates in the United States.1-5 In 2010, the National Institutes of Health convened an expert panel to review safety issues surrounding VBAC and issued recommendations supporting increased uptake of labor after cesarean.5,6 Most of these recommendations have been endorsed and reaffirmed by the American College of Obstetrician Gynecologists (ACOG) and the American College of Nurse Midwives (ACNM).4,5,7,8 Yet in 2018, less than 14% of women with prior cesarean had vaginal births in subsequent pregnancies in the United States.8
The most widely used VBAC calculator is promoted by the Society for Maternal Fetal Medicine (SMFM) (https://mfmunetwork.bsc.gwu.edu/PublicBSC/MFMU/VGBirthCalc/vagbirth.html). The SMFM VBAC calculator uses a mix of medical and demographic data, including race and ethnicity, to generate a percentage score predicting the likelihood of a vaginal birth if labor after cesarean is undertaken rather than an elective repeat cesarean. Calculator use is encouraged as a counseling adjunct, however its role is incompletely addressed.9,10 Because lower score cut-offs for harm prevention have not been established, use of VBAC prediction scores as a contraindication to labor after cesarean is expressly discouraged by SMFM and should not outweigh women’s preferences and values in providing access to services.7
We previously published a review of some of the major limitations of this tool. Limitations include poor accuracy when predicted success drops below 40%; questionable use of racial categories as biological predictors of success; lack of clinically useful correlation of predicted unsuccessful labor after cesarean with harm to mother or baby; and lack of consideration of institutional, provider and patient factors which are known to influence cesarean rates. We raised concern that these limitations could render the calculator prone to misuse and misinterpretation.9
Little research exists on how widely VBAC prediction scores are used or how women or providers understand, value and utilize this information.2 Anecdotally, documentation of calculator scores is a standard of informed consent in some institutions, and some practices and providers employ formal or informal thresholds below which labor after cesarean is discouraged or even forbidden. Yet a search of the literature revealed no documentation regarding the actual or perceived use of this calculator among either physicians or midwives.
The purpose of this study was to determine midwives’ experiences with and perceptions of VBAC prediction calculator use, their ability to meet patient desires for VBAC, inter-professional attitudes toward calculators, and manner in which calculators are used to counsel and advise the public. Because little literature exists on these topics, we included both open and closed ended questions to capture a broad range of responses.
METHODS
We surveyed 11,333 midwives in the American Midwifery Certification Board (AMCB) database. The AMCB is the national certifying body for all certified nurse midwives and certified midwives (CNMs/CMs) in the United States. This database includes CNMs and CMs practicing in US hospitals, and many midwives practicing in out of hospital settings.
Only midwives who had previously agreed to receive surveys approved by AMCB were contacted. We excluded midwives not providing care to persons with prior cesarean births. An email invitation was sent to all eligible midwives by the AMCB on 1/17/2019 and reminder emails were sent at 7 and 14 days following the initial request. The survey remained open for 21 days. Email addresses were never available to the investigators.
Study data were collected and managed using REDCap electronic data capture tool hosted at University of Illinois at Chicago (UIC).10,11 REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.
The survey consisted of multiple choice and free text responses to questions regarding uses of VBAC prediction calculators by midwives and colleagues. We asked about the general supportiveness of midwives and their colleagues toward VBAC and midwives’ perceived ability to accommodate patient desires for labor after cesarean (“nearly all the time,” “sometimes,” or “rarely”). We surveyed whether practices had requirements to use VBAC prediction calculators in counseling (“yes,” “no,” “sometimes,” “depends on provider,” and “don’t know”). The responses yes, sometimes, and “depends on provider” are combined and reported as “any requirement.” We asked whether calculator scores were used to prohibit, discourage or encourage labor after cesarean, and if so, whether explicit cut-offs were used. The survey is available as a supplement (Supporting Information: Appendix S1).
De-identified raw data were retrieved by investigators directly from UIC servers and imported to a web application for managing, analyzing, and presenting qualitative and mixed method research data, for further cleaning and descriptive analysis (Dedoose version 8.0.35, SocioCultural Research Consultants, Los Angeles, CA).
We report responses to 3 free text follow up questions: “Additional comments about VBAC in your practice or facility” and “How else are TOLAC calculators used in your practice?” and “Please describe agreement or disagreement regarding TOLAC success predictor use in your setting.” We considered free text responses augmentation to the quantitative survey as opposed to discrete qualitative research.12 Text responses were analyzed using content and thematic analysis as described by Sandleowski13,14and Vaismoradi.12 Responses were considered in the context of the preceding questions and coded iteratively, then categorized into meaningful themes by the lead author.12-14 Themes were then compared to text by the other authors using the interrater reliability testing procedure included in the Dedoose program.
There were no incentives, gifts, or reimbursements offered for survey participation. No personal, geographic or contact data were collected from participants. An IRB exemption was granted by the University of Illinois, Chicago.
Survey respondents and reviewers commented on the use of the term trial of labor after cesarean (TOLAC) which was used in the survey. We agree that the term vaginal birth after cesarean (VBAC) is more apt and less suggestive of failure. We retain “TOLAC” when referring to survey wording and adopt “VBAC” or simply “labor” in the remainder of the article.
RESULTS
Surveys were sent to 11,333 midwives certified by the AMCB and 1592 responded for an overall response rate of 14.0%. A total of 185 either were not practicing or not offering TOLAC in their scope of practice. These were omitted from analysis. A total of 1398 midwives reported they offer labor after cesarean in their practice. We did not specifically query midwives who did not use calculators, but 93 volunteered this information in text responses. A few of these nonetheless shared experiences and opinions regarding calculators. These 93 were also omitted from this analysis, although we acknowledge this may represent an undercount. Responses from the remaining 1305 midwives are described in table 1. Survey items reported in this paper are presented in supplement S1.
Table 1:
Midwives’ perception of vaginal birth prediction calculator uses in their practices N=1305
| Requirement to use Calculator |
n (%) |
|---|---|
| Any requirement | 527 (40.4) |
| No requirement | 701 (53.7) |
| Don’t Know | 77 (5.9) |
| Use of calculator in counselinga | |
| Encourage VBAC | 125 (9.6) |
| Discourage VBAC | 234 (17.9) |
| Prohibit VBAC | 92 (7.0) |
| Prohibit or discourage VBACb | 288 (21.8) |
| Not used to influence decision making | 786 (60.2) |
| No response | 200 (15.3) |
| Able to accommodate TOLAC | |
| Nearly all the time | 1103 (84.5) |
| Sometimes or rarely | 124 (9.5) |
| No response | 78 (6.0) |
| Interprofessional agreement about calculator usec | |
| On the same page | 564 (43.2) |
| Some differences | 416 (31.9) |
| Strong disagreement | 71 (5.4) |
| No response | 254 (19.5) |
Abbreviations. TOLAC: trial of labor after cesarean MD: medical doctor CNM: certified nurse midwife VBAC: vaginal birth after cesarean
Totals greater than 100% because some midwives reported multiple uses
Calculated by adding the two categories of Prohibit (n=92) and Discourage (n=234) and subtracting those using calculator for both purposes (n=38)
Denominator =1051 (254 non respondents omitted)
One hundred sixty text responses were coded and organized into themes by the lead author. Agreement ranged from 0.8-1.0 (Cohen’s Kappa) among all authors and for all themes reported in this paper. Responses were categorized into 4 themes: Information Counseling, Informed Consent, Influence Patient Management or Options and Inconsistent Use.
Requirement to use calculators
Results of multiple option questions about the uses of calculator scores are presented in table 1. Most requirements to use a VBAC calculator originated with collaborating physicians rather than midwives themselves. Five hundred twenty-seven respondents (40.4%) reported at least some requirement by collaborating physicians to use the VBAC calculator. The majority denied any requirement (n=701, 50.3%) or were not aware of any requirement (n=77, 5.9%) to use a VBAC calculator in options counseling (table 1).
How VBAC calculators are perceived and used
Sixty percent (n=786) of respondents reported using scores for nonrestrictive and non-directive purposes. Two themes, Information Counseling, and Informed Consent described these nondirective uses.
Theme: Information Counseling
These responses indicated that no effort was made to use calculator scores to direct patients’ decisions to labor versus undergo repeat cesarean. They did not mention mandates or requirement for use or documentation of scores. They often specifically mentioned that calculator scores were only one piece of the counseling process or that the patient retains both options and is the ultimate decision maker. For example, there were many comments such as these: “They are used for our and patient knowledge. Patients can still opt to TOLAC even if they have a low chance of success” and “[Calculator scores are] one of many pieces of information that can inform decision making for the pregnant person. Information being an important ingredient in patient autonomy.” These comments signal that the meaning patients assign to calculator prediction scores is not overridden by providers. Similarly, others acknowledge the incomplete and imperfect nature of prediction, placing context around calculator scores: “[Scores are used] just for information; not expected to be infallibly predictive.”
Statements like these seem consistent with the perception of calculator scores as neutral, value free information. In the absence of restrictive cut offs, one would understand that calculator scores could be included in counseling without explicitly restricting access to VBAC.
Theme: Informed Consent
This theme included the terms “consent”, “documentation counseling” or clearly described a charting and /or legal purpose for the calculator score. These comments describe informed consent as routine, perhaps perfunctory, and non-directive. Like the theme Information Sharing, they imply value neutrality rather than guiding or restricting choices. These themes were not mutually exclusive, and many midwives described both informational and consent purposes. “I think they are mainly for documentation. We go with a patient-preference model and believe that anyone who wants a shot at it (VBAC) deserves one” and “It is part of charting and TOLAC consent.”
Using scores to restrict access to VBAC
The remainder of respondents reported using VBAC prediction calculators in more directive ways. Ninety-two (7%) reported using score cut offs to prohibit labor after cesarean; 234 (17.9%) reported using cut offs to discourage VBAC (table 1). We combined prohibiting and discouraging VBAC into one value by adding them, then subtracting those using scores for both purposes, so they were not over counted. A total of 288 (21.8% of all midwives surveyed) used calculator score cut offs to either prohibit or discourage VBAC. This is over twice the number (n=125, 9.6%) who reported using scores to encourage labor (table 1).
Figure 1 compares midwives in practices using prediction calculator scores to encourage, versus prohibit or discourage VBAC, according to whether they are required to use calculator scores when counseling patients. Practices requiring prediction calculator use (n=527) were twice as likely to use it for the purpose of discouraging or prohibiting VBAC (n=203, 38.5%) than practices with no requirement (n=101, 19.2%). Practices using VBAC calculators with no requirement to do so were three times more likely to use scores to discourage or prohibit rather than encourage courage VBAC (10.2% vs 3.3%).
Figure 1.
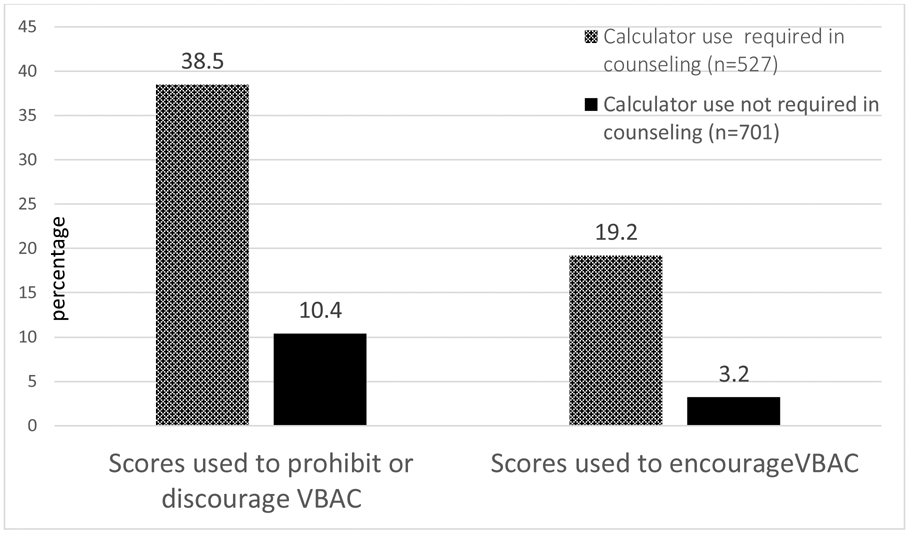
Uses of VBAC prediction calculator scores to encourage, prohibit or discourage vaginal birth after cesarean by physician requirement to use in counseling
Abbreviations. VBAC: vaginal birth after cesarean
Theme: Influence Patient Management or Options.
This theme illustrates using calculator scores to trigger changes in clinical management or curtail patient options. Unlike the themes of Informed Consent or Information Counseling, this theme described concrete roles for VBAC prediction calculator scores in the shaping the options available to persons with prior cesareans, or the level of support they will experience from the care team.
Of the midwives whose practices use prediction calculator score cut offs to restrict access to VBAC, 130 (10%) quoted specific cut offs for prohibiting or discouraging labor. Most of these (n=95) discouraged labor after cesarean unless the VBAC calculator prediction score was at least 50%. For example, “[Calculators] can help convince collaborating physician to “approve” women for TOLAC as long as they score >50%” and “We will offer induction if calculator is >60%.”
Most midwives in practices using calculators to guide or influence patient options did not identify numeric cut-offs for decision making. Many described vague or fluid cut-offs and policies that often varied by provider or other circumstance:
Our department requires MFM [Maternal Fetal Medicine] calculation and documentation of result in prenatal records as part of counseling…. specific cut-off depends on provider. Low numbers get more of a “well you can try if you want…” attitude. Some providers choose a specific number [for cut-off].
Some comments describe how discouraging labor may differ from prohibiting VBAC, depending on the meaning the prediction calculator scores have for providers, but not patients:
Physicians tend to see a low score and decide before labor had even started that she won’t be successful. [They] have a negative attitude and quicker to intervene. Midwives tend to take the score and combine it with subjective features of the women-like how motivated she is, and the narrative she has created around the last birth vs this one.
Theme: Inconsistent Use
These comments illustrate provider inconsistency within practices regarding the use of VBAC calculator scores. This theme often overlapped other themes, especially the theme Influence Patient Management or Options. Midwives identified inconsistent use of calculators among providers as problematic for patients planning VBAC when providers differ on the importance or meaning of calculator scores.
Each collaborating physician has their own opinion about the benefits of a TOLAC calculator, so it depends on who is on backup and can even change during the course of labor, if the collaborating physician changes.
I have found there are a lot more variables than the calculator includes. I have very detailed and realistic conversations with women. I generally use the calculator when I do not support a TOLAC and need some sort of data to help support me when discussing with patient.
A few of our more conservative providers use the calculators--but a lot of the management comes down to what provider is on at the time of admission to L&D.
All patients are required to have a consult with one of the doctors to be “approved” for VBAC. The calculation is done then. Most physicians use the calculator but not all. All of the MFM’s use it if they do the consult. Some physicians are less supportive and so it varies as to how the patient perceives their ability to VBAC even if the numbers are the same.
Ability to accommodate patient desires for labor after cesarean
We surveyed midwives’ perceptions of their ability to accommodate patient desire for VBAC. The majority (n=1103, 84.5%) reported they were able to accommodate desires for VBAC “nearly all the time.” Only 124 (9.5%) perceived themselves as able to accommodate patient desires for labor after cesarean less than “nearly all the time” (table 1). Even among midwives in practices where scores are used to prohibit VBAC outright the majority (n=71, 77.2%) reported being able to accommodate desires for labor after cesarean “nearly all the time” (table 2).
Table 2.
Required uses of calculator scores among midwives able to accommodate patient desire for VBAC “nearly all the time”
| Requirement to use Calculator in counseling |
n (%) |
|---|---|
| aAny requirement | 443 (84.1) |
| bNo requirement | 595 (84.9) |
| Specific use of calculator in counseling | |
| cEncourage VBAC | 104 (83.2) |
| dDiscourage VBAC | 184 (78.6) |
| eProhibit VBAC | 71 (77.2) |
| fNot used to influence decision making | |
| 680 (86.5) | |
Abbreviations. VBAC: vaginal birth after cesarean
Denominator all 527 respondents with any requirement to use prediction calculator
Denominator all 701 respondents with no requirement to use prediction calculator
Denominator all 125 respondents using prediction calculator to encourage labor after cesarean
Denominator all 234 respondents using prediction calculator to discourage labor after cesarean
Denominator all 92 respondents using prediction calculator to prohibit labor after cesarean
Denominator all 786 respondents not using prediction calculator to influence labor versus cesarean decisions
While being required to use a calculator was associated with increased use of calculators to prohibit or discourage VBAC (figure1), it did not diminish midwives’ sense of being able to accommodate patient desires for VBAC. Midwives reported being able to accommodate patient desires for labor after cesarean “nearly all the time” at similar rates whether they were required (n=443, 84.1%) or had no requirement to use the calculator (n=595, 84.9%) (table 2).
Inter-professional agreement
Eighty-one percent (n=1051) of midwives responded to a multiple option question, “How would you describe inter-professional attitudes about TOLAC success prediction calculators?” Under half (n=564, 43.2%) of all midwives reported being “on the same page” as physicians regarding the calculator. Four hundred eighty-seven (46.3%) reported either “some differences” or “strong disagreement” with physicians. An open-ended question followed: “Please describe agreement or disagreement regarding TOLAC success prediction calculators in your setting.” Both agreement and disagreement centered around the theme of using calculator scores to influence patient management or options.
Midwives in our practice feel women should be well counseled but then given the opportunity to choose regardless of the number. Physicians see low numbers as a reason to strongly discourage attempts.
We all agree that we do not care what the number is: if a woman meets our criteria, is aware of the risks and benefits and still desires a VBAC, we will allow her to try. In other practices in our community, we have heard a 60% hard cut-off, no exceptions.
I don’t necessarily think that midwives, as a group, would have different opinions from physicians, as a group. Individuals from within both professions might differ in their views of the idea of automating clinical decision-making.
DISCUSSION
This study provides new information regarding how VBAC calculators are used in midwifery practices and midwives’ perceptions of those uses in the United States. Use of VBAC calculators in midwifery practices are widespread. Two of every five of our respondents reported some requirement by collaborating physicians to use calculators. Practicing under a requirement to use calculators was associated with using scores to discourage or prohibit VBAC substantially more than encouraging VBAC. Almost 40% of midwives in practices with requirements to use calculators reported they are used to prohibit or discourage VBAC; less than 20% reported using them to encourage VBAC. Even among respondents with no requirement to use calculators, they are used more often to discourage (10.4%) rather than encourage (3.3%) VBAC. Use of calculator scores to discourage labor was much more common than outright prohibition (table 1).
Midwives reported both nondirective, informational uses of calculators, as well as option limiting uses by both midwives and collaborators. Text responses provided examples of inconsistent use of calculators within practices, and both directive and non-directive patient counseling. Midwives reported inconsistent and arbitrary use of calculator scores by providers, especially physicians, within their practices, limiting patient’s ability to pursue VBAC.
It is worth noting that even among midwives using calculators to prohibit, discourage, or otherwise restrict labor after cesarean, only 17-23% perceived a diminished ability to accommodate patients’ desire for VBAC. Regardless of the reported uses of calculators within their practices, 77-83% of midwives perceived themselves as able to accommodate patient desires VBAC “nearly all the time” (table 2). The absence of a correlation between restrictive policies and perceived ability to satisfy patient demand is paradoxical. It may reflect patient self-selection, acceptance of calculator-based restrictions among patients and midwives, or small numbers of patients affected by calculator-based restrictions in individual practices. We have no corroborating information (practice statistics, loss to follow up, patient perceptions) which validate or dispute these perceptions.
Limitations
This survey reflects a convenience sample not scientifically representative of all US midwives. The majority of practicing CNMs/CMs were solicited and our response rate (11,333, 14.0%) was low. While recent work suggests low response rates may have little impact on bias,15-17 some bias should be presumed. We know that some respondents who do not currently use calculators nonetheless reported views about their use. While we omitted these from the sample, others may not have been identified. Statistical findings should therefore be interpreted with caution. We did not collect provider or practice demographics which may have allowed for more detailed analyses. All views are those of practicing midwives. The views of physician collaborators, persons with prior cesareans or other stakeholders were considered only indirectly, as interpreted by midwife respondents. A more detailed survey might have clearly and comprehensively distinguished between current actual use, prior use, and opinion regarding calculators.
Strengths
While use of calculators has been encouraged by SMFM for nearly 10 years, to our knowledge, little information exists regarding actual clinical use of calculators by providers in the United States. This study provides a direct report of uses, perceptions, and some consequences of VBAC calculators among practicing CNMs/CMs in the United States. While promoted as a counseling adjunct, this study documents important differences between intended and actual use of VBAC calculators in practice. To our knowledge, this is the first study to document that VBAC calculators are used to restrict patient choice and access to care, counter to SMFM recommendations. We also document the nature of some interprofessional disagreement regarding those policies.
CONCLUSION
Use of VBAC calculators is common within midwifery practices and this study raises many questions about their application. Uses and perceptions of calculators appear heterogenous among midwives and interprofessionally. Many midwives are required by collaborators to use VBAC calculators in counseling patients and many report interprofessional differences about whether and how scores should be used to shape or restrict women’s access to VBAC . Policies requiring VBAC prediction calculator use appear strongly associated with discouraging or prohibiting labor after cesarean. Both ACOG and SMFM promote VBAC calculator use but oppose categorical prohibition of labor based on calculator scores. These findings illustrate a clear need for debate and discussion regarding appropriate use of this tool. Those promoting the SMFM VBAC prediction calculator should acknowledge and vigorously oppose its misuse, and provide explicit guidelines promoting meaningful, patient centered, shared decision making.
Supplementary Material
Quick Points.
Forty percent of midwifery practices reported some requirement to use calculator scores in counseling women about mode of birth after prior cesarean.
Over 1 in 5 midwives are in practices using calculator scores to prohibit or discourage labor after cesarean.
Calculator scores are used more frequently to prohibit or discourage labor after cesarean than to encourage it.
Midwives reported a range of formal and informal uses and protocols for prediction calculator scores and frequent disagreement within practices about these uses.
Even in very restrictive settings most midwives feel able to accommodate labor after cesarean requests and feel supported by colleagues in doing so.
Acknowledgements:
This grant was supported in part by, National Institutes of Health, through Grants UL1TR002003; and 1R01HD089935. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health."
The authors would like to thank the American Midwifery Certification Board (AMCB) for their assistance disseminating this survey and to all the midwives who responded.
We would also like to thank Dr. Chang Park, University of Illinois, Chicago College of Nursing for assistance with statistical software.
Footnotes
The authors have no conflicts of interest to disclose
Contributor Information
Patrick D. Thornton, Department of Women, Children and Family Health Science, University of Illinois Chicago College of Nursing, Chicago, Illinois.
Kylea Liese, Department of Women, Children and Family Health Science, University of Illinois Chicago College of Nursing, Chicago, Illinois.
Kirby Adlam, University of Illinois Hospital, Chicago, Illinois.
Katherine Erbe, University of Illinois Hospital, Chicago, Illinois.
Barbara L McFarlin, Department of Women, Children and Family Health Science, University of Illinois Chicago College of Nursing, Chicago, Illinois.
References
- 1.Black M, Entwistle VA, Bhattacharya S, Gillies K. Vaginal birth after caesarean section: Why is uptake so low? Insights from a meta-ethnographic synthesis of women’s accounts of their birth choices. BMJ Open. 2016;6(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Metz TD, Stoddard GJ, Henry E, Jackson M, Holmgren C, Esplin S. How do good candidates for trial of labor after cesarean (TOLAC) who undergo elective repeat cesarean differ from those who choose TOLAC? Am J Obstet Gynecol. 2013;208(6):458.e1–458.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landon MB, Grobman WA, Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. What We Have Learned About Trial of Labor After Cesarean Delivery from the Maternal-Fetal Medicine Units Cesarean Registry. Semin Perinatol. 2016;40(5):281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ACNM. American College of Nurse - Midwives Responds to ACOG ’ s 2010 VBAC Recommendations. Silver Springs; 2010. Accessed 2020-2-10 [Google Scholar]
- 5.National Institutes of Health. National Institutes of Health Consensus Development Conference Statement. Semin Perinatol. 2010;34(5):351–365. doi: 10.1053/j.semperi.2010.06.002 [DOI] [PubMed] [Google Scholar]
- 6.Miller ES, Grobman WA. Obstetric outcomes associated with induction of labor after 2 prior cesarean deliveries. Am J Obstet Gynecol. 2015;213(1):89.e1–89.e5. [DOI] [PubMed] [Google Scholar]
- 7.Committee on Practice Bulletins-Obstetrics. Vaginal Birth After Cesarean Delivery Practice Bulletin No. 205. Obstet Gynecol. 2019;133(2):e110–e127. [DOI] [PubMed] [Google Scholar]
- 8.Martin JA, Hamilton BE OM. Births in the United States, 2018 NCHS Data Brief No 346. Hyattsville, MD; 2019. [PubMed] [Google Scholar]
- 9.Thornton P Limitations of Vaginal Birth After Cesarean Success Prediction. J Midwifery Women’s Heal. 2018;63(1):115–120. [DOI] [PubMed] [Google Scholar]
- 10.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs Heal Sci. 2013;15(3):398–405. [DOI] [PubMed] [Google Scholar]
- 13.Sandelowski M, Leeman J. Writing Usable Qualitative Health Research Findings. Qual Health Res. 2012;22(10):1404–1413. [DOI] [PubMed] [Google Scholar]
- 14.Sandelowski M What’s in a name? Qualitative description revisited. Res Nurs Heal. 2010;33(1):77–84. [DOI] [PubMed] [Google Scholar]
- 15.Phillips AW, Friedman BT, Utrankar A, Ta AQ, Reddy ST, Durning SJ. Surveys of health professions trainees: Prevalence, response rates, and predictive factors to guide researchers. Acad Med. 2017;92(2):222–228. [DOI] [PubMed] [Google Scholar]
- 16.Lasater KB, Jarrín OF, Aiken LH, McHugh MD, Sloane DM, Smith HL. A Methodology for Studying Organizational Performance: A Multistate Survey of Front-line Providers. Med Care. 2019;57(9):742–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hendra R, Hill A. Rethinking Response Rates: New Evidence of Little Relationship Between Survey Response Rates and Nonresponse Bias. Eval Rev. 2019;43(5):307–330. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


