Abstract
Background:
With the emergence of illicit fentanyl, fentanyl-involved overdose rates increased from 2013 to 2017 in the United States (US). We describe US trends in opioid-related overdose mortality rates by race, age, urbanicity, and opioid type before and after the emergence of fentanyl.
Methods:
Using the Centers for Disease Control and Prevention’s WONDER database, we estimated crude and age-standardized opioid-related overdose mortality rates at the intersections of race (non-Hispanic [NH] Black and white), age (<55 and ≥55 years), sex (male and female) and urbanicity (urban and rural residence) from 2005–2017. We compare relative changes in mortality from 2013–17, and describe changes in the contributions of fentanyl, heroin, and other opioids to opioid-related overdose mortality.
Results:
From 2013–2017, the overall opioid overdose mortality rate was consistently higher in NH white Americans, however, the rate increase was greater among NH Black (174%) compared to NH white (85%) Americans. The steepest increases occurred in the overdose rates between 2013–2017 among younger (aged <55 years) urban NH Black Americans (178% increase). Among older (≥55 years) adults, only urban NH Black Americans had an increase in overdose-related mortality rate (87% increase). Urban NH Black Americans also experienced the greatest increase in the percent of fentanyl-involved deaths (65% in younger, 61% in older).
Conclusions:
In the era of increased availability of illicitly manufactured fentanyl (2013–2017), there has been a disproportionate increase in opioid-related overdose deaths among urban NH Black Americans. Interventions for urban NH Black Americans are urgently needed to halt the increase in overdose deaths.
Keywords: Fentanyl, overdose, urban, Black Americans, health inequity
1. Background
In 2017, opioid-related overdose deaths reached a record high of 47,600 in the United States (US) and declined by 2% to in 2018 (Hedegaard et al., 2018; Wilson et al., 2020). Although the number of deaths from prescription opioids and heroin were steady from 2016 to 2017, there was a 47% increase in synthetic opioid-related deaths, followed by an additional 10% increase from 2017–2018, mainly driven by illicitly manufactured fentanyl (henceforth referred to as “fentanyl”) (Hedegaard et al., 2020, 2018). Although the exact date is unknown, fentanyl is believed to have emerged in the illicit opioid market around 2013 with supply surges and corresponding fentanyl overdose rates detected nationally beginning in 2014, partly as an unintended consequence of scaled-up interdiction efforts targeting heroin entering the US, creating the demand for easily-concealable opioids (Beletsky and Davis, 2017; Zoorob, 2019). Fentanyl, being more potent and cheaper to produce than heroin, is often sold deceptively as heroin or a brand-named prescription drug such that users often are not aware that the drugs they are taking are adulterated with fentanyl (Ciccarone et al., 2017). The fentanyl-involved overdose mortality rate increased from 1.0 per 100,000 population in 2013 to 9.0 per 100,000 in 2017; the synthetic opioid-related deaths (which include fentanyl, fentanyl analogs, and tramadol but excludes methadone) increased from 9.0 per 100,000 in 2017 to 9.9 per 100,00 (Hedegaard et al., 2018; Wilson et al., 2020). In aggregate, fentanyl is an important driver of opioid-related mortality, but less is known about how the drug has impacted the epidemiology of opioid-related overdose mortality in populations by person, place, and time (Jones et al., 2018).
From the 1970s through the mid-1990s, heroin was the primary driver of opioid-related overdose mortality, and urban Black communities experienced a disproportionate burden of these deaths. In the late 1990s, the heroin epidemic remained relatively constant in Black communities, while the proliferation of prescription opioids caused opioid deaths to soar among whites such that rates surpassed Black opioid-related mortality rates around the year 2000 (Alexander et al., 2018; Spencer et al., 2019). This reversal in the racial gradient of risk garnered a great deal of attention in scientific literature, popular media, and political discourse and policy (Netherland and Hansen, 2016). Perhaps most notably, economists Case and Deaton suggested the recent decline in U.S. life expectancy was the result of rising “deaths of despair,” described as the increase in mortality among working-age white men and women without college degrees driven by drug overdose, suicide, and liver disease deaths (Case and Deaton, 2020, 2015).
However, there is evidence to suggest that the emergence of fentanyl is once again shifting the distribution of opioid-related overdose deaths, bringing a new wave of opioid-related mortality to the urban Black communities still affected by the legacy of the late 20th century heroin epidemic. A National Vital Statistics Report indicates that although fentanyl-involved overdose death rates increased sharply across all demographic groups from 2013 to 2017, non-Hispanic Black Americans experienced the highest rate of increase (Spencer et al., 2019).
While heroin-involved overdose mortality decreased from 2017 to 2018 in major metropolitan areas (5.6 to 5.2 per 100,000 population) and suburban areas (5.8 to 5.5 per 100,000), synthetic opioid overdose mortality increased dramatically in major metropolitan areas (8.2 to 9.4 per 100,000) and suburban areas (11.6 to 12.7 per 100,000) (US Centers for Disease Control and Prevention, 2020a, 2020b). In rural areas, however, heroin-involved overdose mortality remained unchanged (2.4 per 100,000) and synthetic opioid-related mortality decreased (6.0 to 5.8 per 100,000) (US Centers for Disease Control and Prevention, 2020a, 2020b).
Differences in opioid-related and synthetic opioid mortality have been reported among residents of metropolitan areas in the US by age group within race and ethnicity groups, which were thought to be a reflection of differences among people who use drugs, the infiltration of fentanyl in urban drug markets, and risk factors for overdose (Lippold et al., 2019). The differences in opioid-related mortality among people in rural areas by age group within race and ethnicity groups has not be investigated. Nor have these investigations been stratified by sex, even though women have had overall lower opioid-related mortality rates than men from 1999 to 2018 with less steep increases since the emergence of fentanyl (Hedegaard et al., 2018).
With the long history of opioid-related overdose mortality in the US, from the heroin epidemic disproportionately impacting urban Black communities in the 1990s, to the more recent “deaths of despair” epidemic among rural white communities, we aimed to describe the trends in opioid-related overdose mortality rates in the US among white and Black Americans by age, sex, and urbanicity. We tracked trends in opioid-related overdose mortality from 2005 to 2017, focusing on changes occurring over the period when fentanyl became widespread in the drug market (2013 to 2017). Finally, we characterized the contributions of fentanyl, heroin, and other opioids to opioid-related mortality rates among white and Black Americans from 2013 to 2017 within strata of race, age, sex, and urbanicity. The findings can guide policy makers and program implementors in developing interventions to reduce opioid-related deaths and promote health equity.
2. Material and methods
2.1. Study population
We used death certificate data from the Centers for Disease Control and Prevention (CDC)’s WONDER online database to characterize trends in opioid-related overdose mortality from 2005–2017. CDC WONDER provides mortality counts for US counties based on death certificates for all US residents.
2.2. Study variables
From CDC WONDER, we extracted information stratified by five-year age groups, race (non-Hispanic [NH] Black and NH white), urbanicity (rural and urban/suburban), and cause of death (Ingram and Franco, 2014).
We identified opioid-related overdose deaths using the Substance Abuse and Mental Health Services Administration (SAMHSA)-recommended definition that includes the underlying causes corresponding to overdose (intentional [X60–64] and unintentional/accidental drug poisonings [X40–44], as well as poisonings due to assault [X85] and poisonings with undetermined intent [Y10–14]) and at least one relevant contributory cause code suggestive of opioid death (poisoning by opium [T40.0], heroin [T40.1], other opioids [T40.2], methadone [T40.3], other synthetic narcotics including fentanyl [T40.4], or other unspecified narcotics [T40.6]) (Prevention, 2018). We estimated the opioid-related deaths attributed to fentanyl, heroin, and other opioids as follows: 1) fentanyl-involved deaths were classified as deaths with a multiple cause code of T40.4 or “other synthetic narcotics;” 2) heroin-involved deaths were classified as deaths with the code of T40.1; 3) other opioid-involved deaths were classified as deaths with the codes T40.0, T40.2, T40.3, and/or T40.6. Given that many opioid-related overdoses involve polysubstance use, the three categories are not mutually exclusive.
The focus on NH white and NH Black Americans was motivated by the histories of opioid-related overdose in the US in these two groups (from 1990s to present), as well as suppression of the number of deaths (<10) among Hispanic Black, Hispanic white, NH American Indian/Alaska Natives, and NH Asian Americans, after stratifying by year, age, sex (male and female), and urbanicity; suppression is required to protect confidentiality.
After downloading stratified data, we dichotomized age at ≥55 years because adults aged 25–34, 35–44, and 45–54 had a higher drug overdose mortality rate from 1999 to 2017, with a steeper increase in the rate from 2013–2017, compared to adults 55–64 and ≥65 years (Hedegaard et al., 2018). We defined urbanicity by the National Center for Health Statistics 2013 dichotomization of their 6-category classification system for counties into urban/suburban (metropolitan areas ranging from small metro areas with less than counties with populations of <250,000 to large metro areas of >1 million) vs rural areas (nonmetropolitan areas ranging from micropolitan urban clusters with populations of <50,000 to areas that are less sparsely populated) (Ingram and Franco, 2014). The dichotomization of age and urbanicity was also motivated by suppression of the number of deaths (<10) among finer strata within NH white and NH Black Americans. Sex was defined as male and female.
2.3. Statistical analysis
We estimated trends (2005 to 2017 which was the most recent peak in the number of US deaths due to opioids) in crude and age-standardized (using the 2000 US standard population) opioid-related mortality rates for NH white and NH Black Americans by age and sex and urbanicity (Klein and Schoenborn, n.d.; Wilson et al., 2020). For both crude and age-standardized opioid-related overdose mortality rates, relative changes in the rates from 2013 (the emergence of fentanyl) to 2017 (the peak in opioid-related mortality rate in the US) were estimated.
We estimated the proportion of all opioid-related overdose deaths attributed to fentanyl, heroin, and other opioids. The proportion of all opioid-related overdose deaths attributed to each one of these three categories was estimated by dividing by the overall count of opioid-related overdose deaths (defined using the same SAMHSA definition). The absolute change in the proportion of opioid-related overdose deaths for each opioid type from 2013 to 2017 was estimated for each group.
The primary research question of our study was not pre-registered on a publicly available platform; results should be considered descriptive in nature and exploratory.
3. Results
Age-adjusted overdose-related mortality rates increased sharply in both NH white and NH Black Americans after 2013, the year that marked the emergence of fentanyl (Figure 1). From 2013 to 2017, the rate was consistently higher in NH white Americans; however, the relative age-standardized overdose-related mortality rate increased 174% among NH Black Americans (4.7 to 12.9 per 100,000 population) as compared to 85% among NH white Americans (10.5 to19.4 per 100,000 population). The number of overdose deaths were consistently higher in NH white Americans compared to NH Black Americans (reflective of US population proportions); however, from 2013 to 2017 deaths increased by 186% among NH Black Americans (1,926 to 5,513 deaths) compared with 80% among NH white Americans (20,605 to 37,113 deaths).
Figure 1:
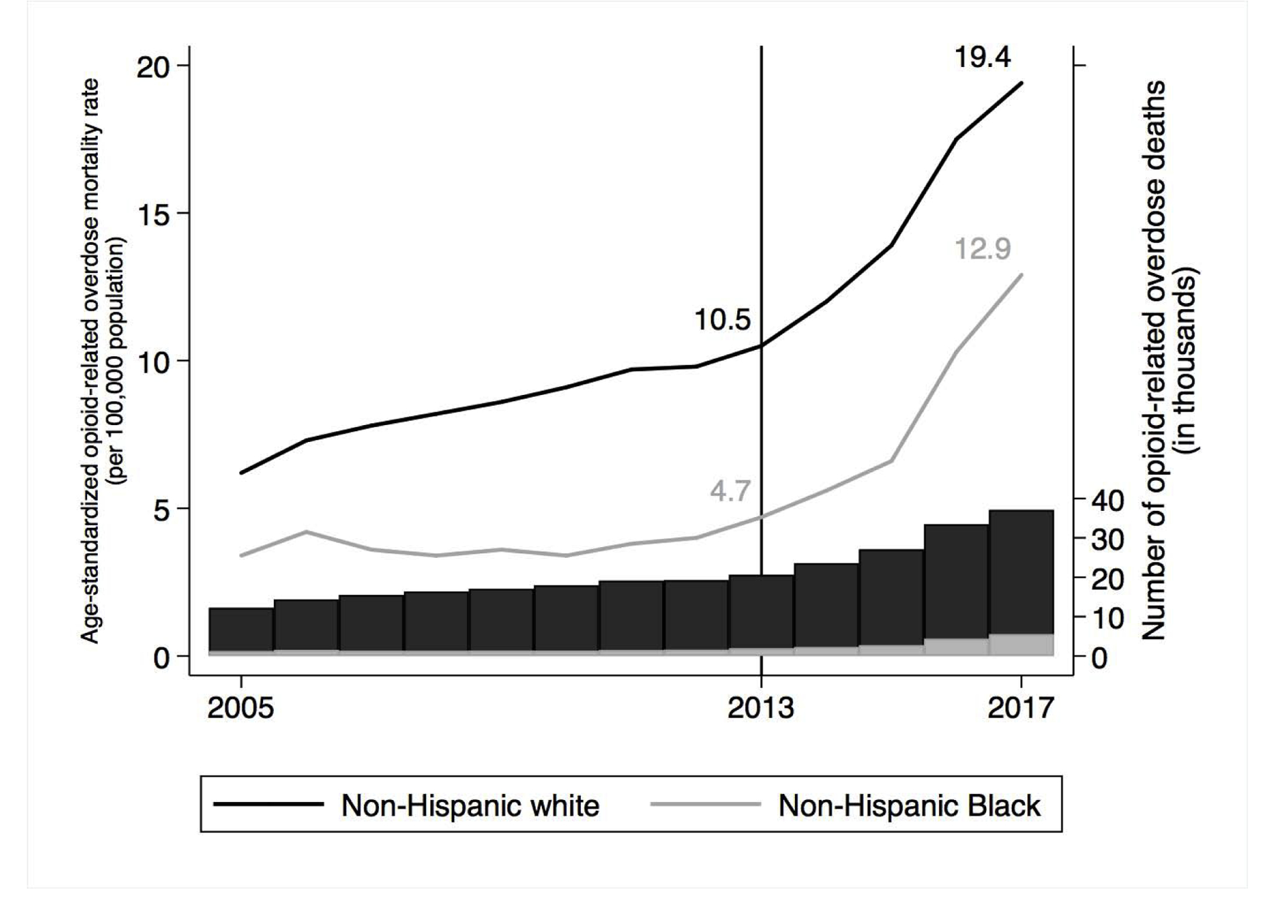
Trends in age-standardized opioid-related overdose mortality rates and number of opioid-related deaths, among non-Hispanic (NH) white and NH Black Americans 2005–2017
The black line and bars represent non-Hispanic white. The gray line and bars represent non-Hispanic Black.
Age-standardized opioid-related overdose mortality rate estimates are missing for certain years and subgroups because the number of deaths in the strata within this category was small, thus the data were suppressed in the CDC WONDER data to protect confidentiality.
Numbers show the 2013 and 2017 age-standardized opioid-related overdose mortality rate per 100,00 population.
The vertical line denoting the year 2013 within the plot is the visual reminder of the year illicitly-manufactured fentanyl emerged in the illicit opioid market.
3.1. Crude opioid-related overdose mortality rates, at the intersections of race, age, sex, and urbanicity
After stratifying by age (<55 and ≥55 years old), the highest crude overdose rate in 2017 was among younger urban NH white Americans (32.0 per 100,000 population) followed by younger rural NH white Americans (23.0 per 100,000 population), older urban NH Black Americans (21.1 per 100,000 population), and then younger urban NH Black Americans (17.1 per 100,000 population, Figure 2). Among older adults, NH Black Americans had the highest overdose rates throughout the study period (2005–2017). The steepest relative increase in the overdose rate from 2013–2017 was among younger urban NH Black Americans (178%), followed by younger rural NH Black Americans (98%), younger urban NH white Americans (93%), and older urban NH Black Americans (87%). Increases among younger rural NH white Americans (62%), older urban NH white Americans (66%), and older rural NH white Americans (16%) trailed behind. We further stratified the trends by sex, showing that the largest increases in overdose rates were among men. Among women, urban Black women had the greatest relative increases in opioid-related overdose mortality, regardless of age (age <55 years: 104%; age ≥55 years: 110%) (Figure 3).
Figure 2.
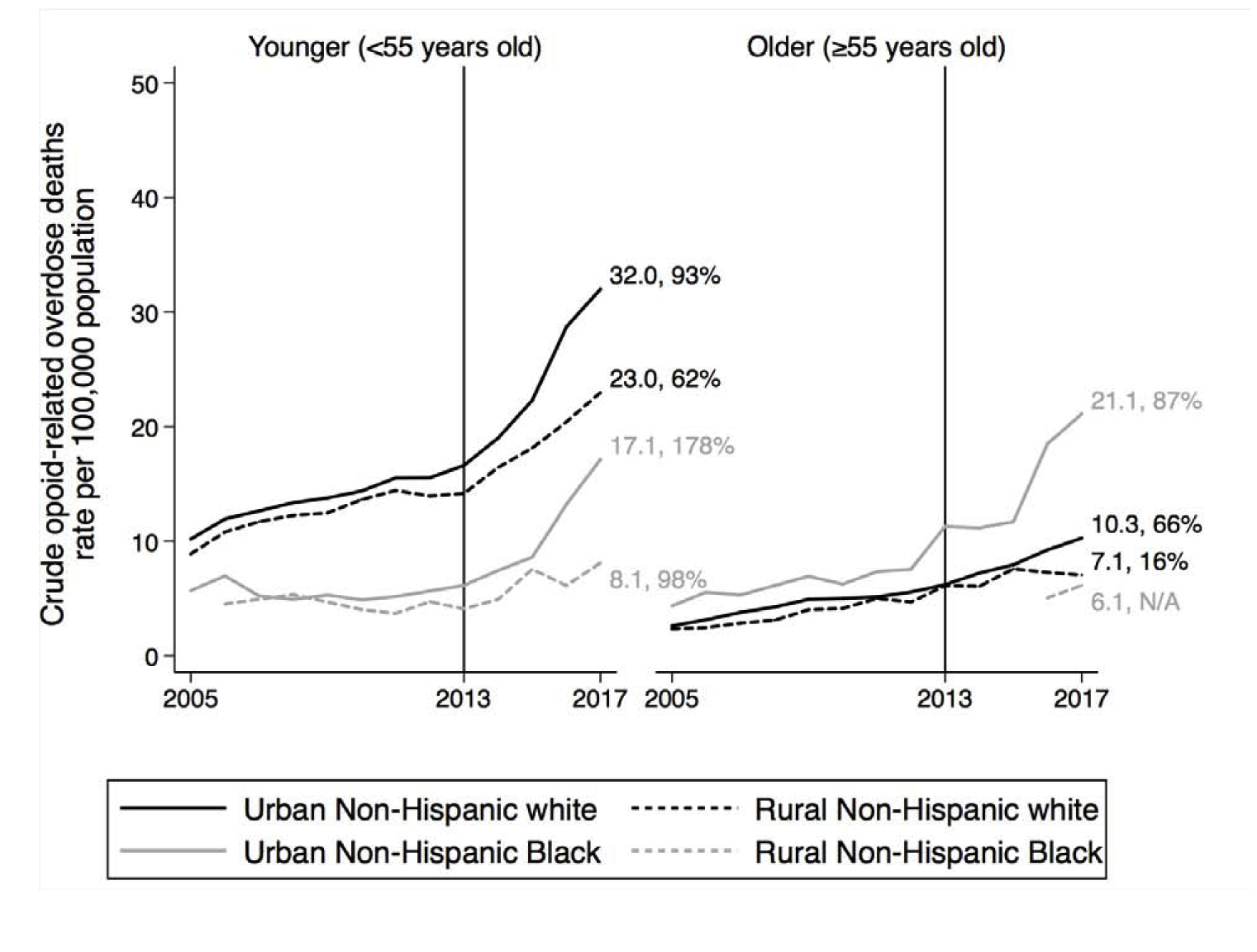
Crude opioid-related overdose mortality rates and the relative increase from 2013 to 2017, stratified by age, and by race and urbanicity
The solid black line represents urban non-Hispanic white. The dotted black line represents rural non-Hispanic white. The solid gray line represents urban non-Hispanic Black. The dotted gray line represents rural non-Hispanic Black.
Crude opioid-related overdose mortality rate estimates are missing for certain years and subgroups because the number of deaths in the strata within this category was small, thus the data were suppressed in the CDC WONDER data to protect confidentiality. Numbers show the 2013 and 2017 crude opioid-related overdose mortality rate per 100,00 population.
The vertical line denoting the year 2013 within the plot is the visual reminder of the year illicitly-manufactured fentanyl emerged in the illicit opioid market.
Figure 3:
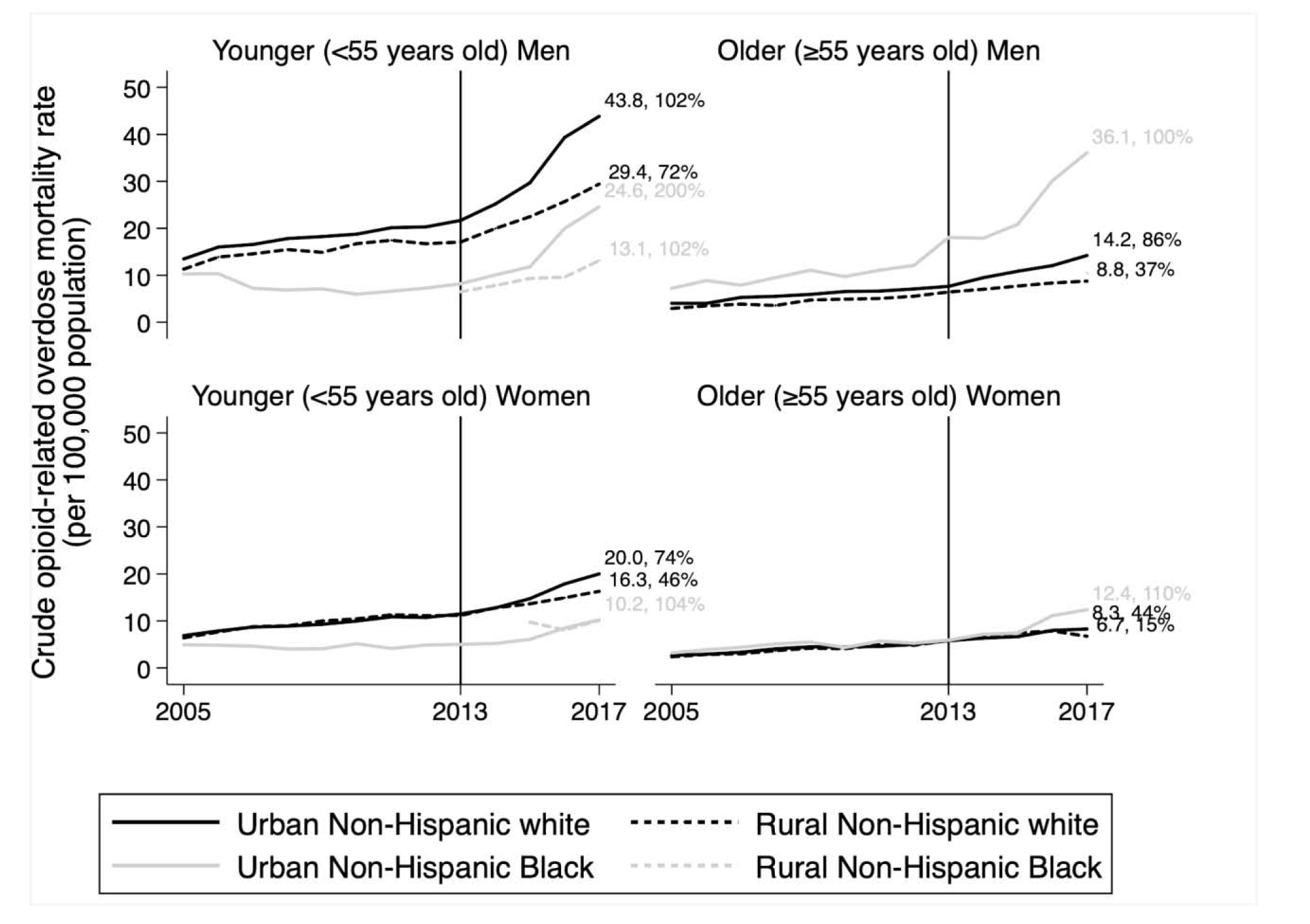
Crude opioid-related overdose mortality rates and the relative increase from 2013 to 2017, stratified by sex and age, and by race, and urbanicity
The solid black line represents urban non-Hispanic white. The dotted black line represents rural non-Hispanic white. The solid gray line represents urban non-Hispanic Black. The dotted gray line represents rural non-Hispanic Black.
Crude opioid-related overdose mortality rate estimates are missing for certain years and subgroups because the number of deaths in the strata within this category was small, thus the data were suppressed in the CDC WONDER data to protect confidentiality. Numbers show the 2013 and 2017 crude opioid-related overdose mortality rate per 100,00 population.
The vertical line denoting the year 2013 within the plot is the visual reminder of the year illicitly-manufactured fentanyl emerged in the illicit opioid market.
3.2. Changing contributions of fentanyl, heroin, and other opioid-involved deaths
The percent of total opioid-related deaths involving fentanyl increased in all strata of age, race, and urbanicity, while deaths involving heroin remained relatively stable and deaths due to other opioids, primarily prescription opioids, decreased (Figure 4). The largest increases in fentanyl-involved opioid deaths were among younger and older urban NH Black Americans, who experienced absolute increases of 61% and 65%, respectively. The next largest increases were among younger urban and rural NH white Americans, who experienced absolute increases of 53% and 39%, respectively. In 2017, 47% and 75% of total opioid-related deaths involved fentanyl among younger and older rural NH Black Americans; the numbers of fentanyl-involved deaths were suppressed by the CDC WONDER database in order to preserve confidentiality (Tiwari et al., 2014). Older urban and rural NH white experienced absolute increases of 27% and 21% in fentanyl-involved deaths.
Figure 4.
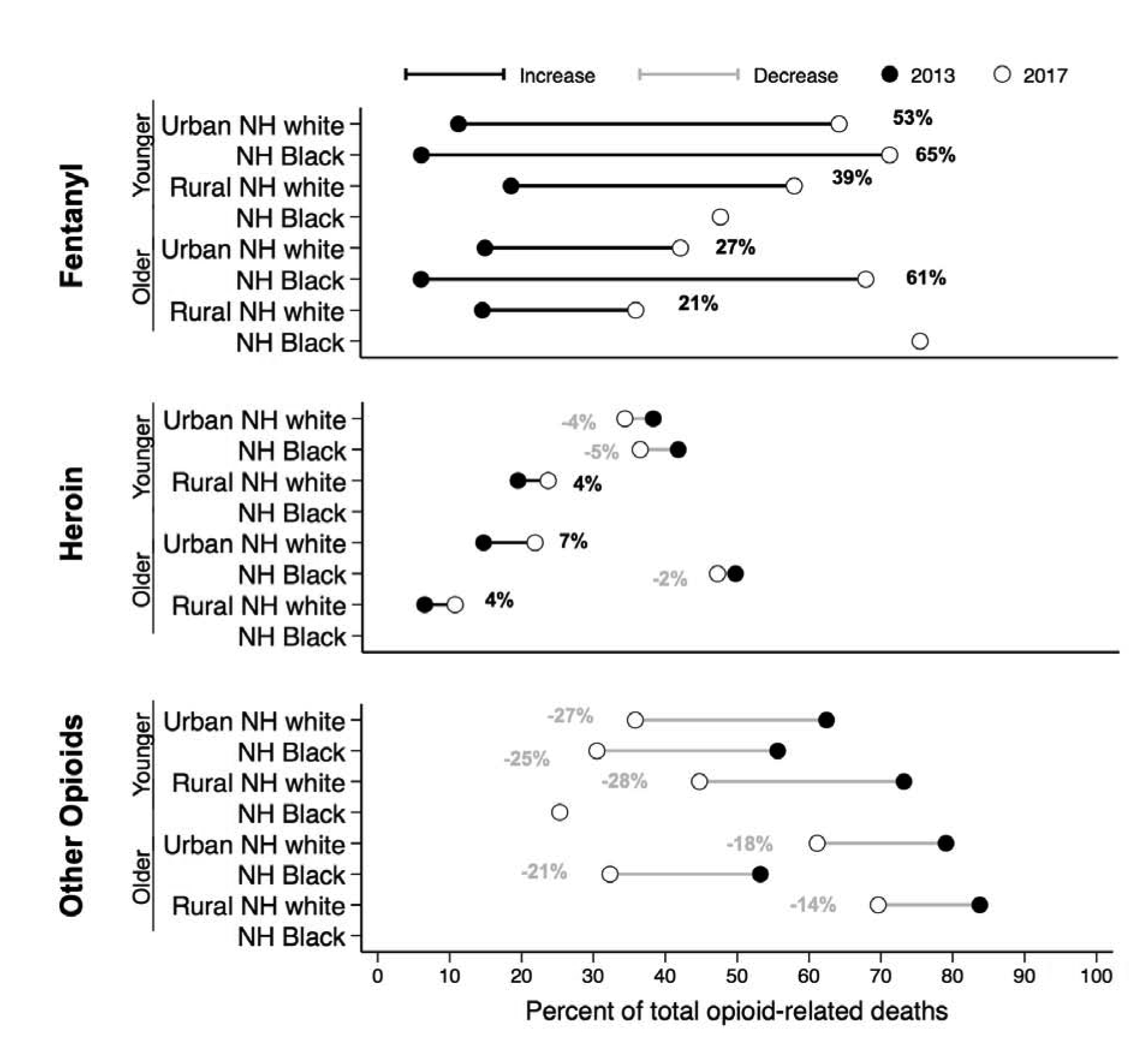
Changing percent contributions of type-specific opioids to the total opioid-related deaths from 2013 to 2017, by age, race, and urbanicity.
The black dot represents 2013. The white dot represents 2017. The red line represents an increase from 2013 to 2017. The blue line represents a decrease from 2013 to 2017.
NH=Non Hispanic
Younger refers to those <55 years. Older refers to those ≥55 years of age.
Fentanyl or synthetic narcotic-involved deaths were indicated with the multiple cause of death T40.4.
Heroin-involved deaths included the code T40.1.
Other opioids-involved deaths were indicated with the codes T40.0, T40.2, T40.3, and/or T40.6.
Percent contributions are missing for certain drugs, years, and subgroups because the number of deaths in the strata within this category was small, thus the data were suppressed in the CDC WONDER data to protect confidentiality
The contribution of heroin-involved opioid deaths was relatively stable over this time period, with the largest absolute decrease (−5%) seen in younger urban NH Blacks and the largest absolute increase (7%) seen in older urban NH whites. Heroin-involved deaths were greatest among older urban NH Black Americans (49% of total opioid-related deaths in 2013 and 47% in 2017). The percent of opioid-related deaths involving other opioids decreased the most among younger people: by 28% among younger rural NH whites, 27% among younger urban NH whites, and 25% among younger urban NH Blacks.
4. DISCUSSION
Our findings are consistent with previously published data showing higher opioid-related overdose mortality rates in NH white compared to NH Black Americans (Alexander et al., 2018). However, after stratifying by age and urbanicity, two important patterns emerged in the period from 2013–2017: 1) younger, urban NH Black Americans experienced the greatest relative increase in opioid-related overdose mortality rates of all sub-groups examined, and 2) among older adults, urban NH Black Americans had both a) the highest overall rates of opioid-related overdose mortality and b) the greatest relative increase in mortality. Although much of the discourse regarding the current opioid epidemic has focused on the rise of fatal overdoses among younger, rural white Americans, our data demonstrate that, in both age groups examined, urban NH Black Americans have experienced sharp increases in opioid-related overdose mortality rates since 2013. Our findings suggest fentanyl is the driving force behind rising opioid deaths in urban NH Black communities, as urban NH Black Americans (both those aged <55 and ≥55 years) experienced the largest increases in fentanyl-involved overdose death. Concurrently, we observed relatively stable contributions from heroin over time and substantial declines in contributions from other opioids, including prescription opioids among all sub-groups examined.
These data suggest that fentanyl may be shifting the burden of opioid deaths to exacerbate a decades-old epidemic among urban NH Black Americans. Urban centers have long been plagued by heroin epidemics, with older NH Black men impacted heavily by heroin overdose deaths. The response to earlier drug epidemics such as crack cocaine focused largely on punishment, with the ‘war on drugs’ disproportionately impacting urban NH Black men. When prescription opioids brought the opioid epidemic to white America in the late 1990s and early 2000s, media rhetoric changed entirely such that there was an outpouring of public and political support to address the opioid epidemic using a public health framework to address underlying drivers and risk factors rather than merely assigning moral blame (Alexander, 2012). Our data highlight an under-recognized phase of this epidemic, with fentanyl fueling a rapid increase in opioid-related overdose deaths among urban NH Blacks. National overdose mortality data for 2018 signaled an important 2% decline in the number of overdose deaths nationwide, providing hope that a decreasing trend is possible when 2019 data are available. But there was a worrisome 10% increase in the synthetic opioid mortality rate, which is driven by fentanyl and fentanyl analog-related deaths. Our study suggests urban NH Black Americans, particularly younger men, are at risk for being left behind in the decline of overdose deaths in the US. A health equity lens and appreciation of historical injustices are needed when examining drivers of, and interventions for, opioid-related overdose deaths among subgroups of Americans, so as to not further marginalize urban NH Black opioid users.
Observed differences in opioid-related overdose mortality rates by sub-group adds to the empirical evidence for racial equity in implementation of opioid-related mortality interventions and supports tailored public health interventions for urban, NH Black Americans (Barboza and Angulski, 2020; Hadland et al., 2017; Madden and Qeadan, 2020; Sherman et al., 2019). A recent study showed high interest among Black Americans in safe consumption sites, which are places for individuals to use previously purchased drugs under supervision (Sherman et al., 2019). Safe consumption sites may overcome important barriers to overdose prevention, including the rapid nature of fentanyl overdose and solitary drug use (Potier et al., 2014; US Centers for Disease Control and Prevention, 2015). Further, access to comprehensive drug checking programs which allow for the testing of fentanyl and other adulterants in real time could reduce racial disparities in overdose (Sherman et al., 2019). The rise in the opioid-related overdose mortality rate observed in older, urban Black Americans might be attributed to exposure to fentanyl without tools to reduce the probability of a fatal overdose (Jamison and Shefte, n.d.; Spencer et al., 2019). Access to comprehensive drug checking programs which allow for the testing of fentanyl and other adulterants in real time could reduce the probability of a fatal overdose (Sherman et al., 2019). A key difference, however, between younger and older adults observed in a recent study of urban adults in Baltimore, Providence, and Boston was that younger adults were less interested in overdose prevention sites or drug checking (Park et al., 2019; Sherman et al., 2019). A structural-level intervention to reduce opioid-related overdose mortality is drug treatment for all prison inmates (Green et al., 2018). Until criminal justice reform succeeds in narrowing the five-fold gap in incarceration rates between Black and white Americans, interventions within carceral systems may have an especially large population-level impact on overdose mortality in Black communities, and urban Black men in particular (National Association for the Advancement of Colored People (NAACP), n.d.).
Although rural areas continue to experience a significant burden of opioid misuse, our study underscores what others have recently shown in that the greatest relative increases in opioid-related overdose death rates have occurred among urban populations, both NH Black and NH white (Scholl et al., 2018). Both economic disadvantage as well as opioid supply factors are believed to be associated with higher overdose-related mortality rates (Monnat, 2019; Pear et al., 2019). Understanding how these and other contextual factors affect age and race subgroups in both urban and rural areas will be crucial in designing appropriately targeted prevention interventions.
Opioids are one of many substances that contribute to the drug overdose mortality rate in the US. For the first time in many years, the age-adjusted drug overdose mortality rate decreased (by 4.6%) from 2017 to 2018 despite the 10% increase in the synthetic opioid overdose mortality rate (Hedegaard et al., 2020). Overdose mortality rates involving cocaine and psychostimulants (such as methamphetamines) also increased 3-to-5 fold from 2012 to 2018 (Hedegaard et al., 2020). As drug use and overdose mortality continues to change over time in the US, understanding these changes within important sub-groups by race, sex, age, and urbanicity can ensure the appropriate treatment programs are available to people who need them in both urban and rural areas.
There are several limitations to our study, including our classifications of opioid-related overdose death and further classifying fentanyl-, heroin-, and other opioids-involved deaths. First, classification of opioid-related overdose death relies on the specification of a drug as a cause of death on the death certificate. Because this toxicology information is often incomplete, ascertainment of opioid-related deaths is almost certainly an underestimate (Buchanich et al., 2018; Paulozzi et al., 2012). Second, there is likely misclassification of fentanyl-, heroin-, and other opioids-involved deaths. Fentanyl-involved deaths were classified based on the code for “other synthetic narcotics,” which includes tramadol and other synthetic opioids in addition to fentanyl; however, we assume that fentanyl is the major contributing drug in the context of the current epidemic. We were not able to apply the Drugs Mentioned with Involvement methodology to identify fentanyl-involved deaths developed by the National Center for Health Statistics and the US Food and Drug Administration because we did not have access to the needed data, including text from death certificates (Spencer et al., 2019). Stratum-specific counts of overdose deaths among rural NH Black Americans were small and suppressed for confidentiality, which inhibited our ability estimating of mortality rates for this group in some calendar years. This also limited our ability to stratify our results into finer age groups, as well as into US states or regions, as prior evidence has shown differences in opioid-related and synthetic opioid mortality overdose mortality in the US by age, state, and region (Hedegaard et al., 2019; Lippold et al., 2019; US Centers for Disease Control and Prevention, 2020b, 2020a).
5. Conclusion
By describing trends in opioid-related mortality by age, race, urbanicity, and opioid type, a shift in the subgroups affected by the US opioid epidemic has occurred since the emergence of fentanyl in 2013. Among older adults, urban NH Blacks consistently experienced the highest mortality of any demographic group, throughout the study period (2005–2017). As synthetic opioid mortality continues to increase, we observed an emerging trend of increased opioid-related overdose mortality rates among urban, NH Blacks, particularly younger (<55 years) men (Hedegaard et al., 2020). Because the opioid epidemic has been characterized as a majority white epidemic in recent years, it is vital to call attention to this shift, culling resources to address the opioid epidemic as not only a public health emergency, but also an important issue of health equity. These findings should inform the scale-up of evidence-based harm reduction services and drug treatment targeting distinct groups of people who use drugs to ensure that the right interventions reach the right population(s) at the right time to reduce the impact of an epidemic killing more than 100 Americans every day (Hedegaard et al., 2018; Khoury et al., 2016).
Highlights.
In 2013, there was an increase in the availability of illicitly-manufactured fentanyl in the US
Non-Hispanic Black (vs. white) Americans had a greater increase in overdose rate
Urban non-Hispanic Black Americans had the greatest increases in overdose rate
Older urban non-Hispanic Black men had the greatest increase in fentanyl-induced overdose
Urban non-Hispanic Black Americans need of harm reduction and drug treatment services
Acknowledgements
We would like to thank those who submit death information to the state-level and the National Center for Health Statistics and those that manage the Centers for Disease Control and Prevention (CDC)’s WONDER online database. No compensation was provided to them for the data used in this study.
Funding This work was funded by a Catalyst Award to Dr. Keri Althoff from Johns Hopkins University. Kathryn M. Leifheit was supported by a National Institute of Child Health and Human Development Pre-Doctoral Fellowship (award number F31HD096767) and an Agency for Healthcare Research and Quality Post-Doctoral Fellowship (award number 2T32HS000046). Susan Sherman and Ju Nyeong Park received support from the Johns Hopkins University Center for AIDS Research (P30AI094189). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Role of Funding Sources Nothing declared
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
Althoff: no conflict declared
Leifheit: no conflict declared
Neyong: no conflict declared
Chandran: no conflict declared
Sherman: expert witness in opioid legislation on the side of the plaintiff.
REFERENCES
- Alexander M, 2012. The New Jim Crow: Mass Incarceration in the Age of Color-Blindness, The New Jim Crow: Mass incarceration in the age of colorblindness. The New Press. [Google Scholar]
- Alexander MJ, Kiang MV, Barbieri M, 2018. Trends in Black and White Opioid Mortality in the United States, 1979–2015. Epidemiology 29, 707–715. 10.1097/EDE.0000000000000858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barboza GE, Angulski K, 2020. A descriptive study of racial and ethnic differences of drug overdoses and naloxone administration in Pennsylvania. Int. J. Drug Policy 78 10.1016/j.drugpo.2020.102718 [DOI] [PubMed] [Google Scholar]
- Beletsky L, Davis CS, 2017. Today’s fentanyl crisis: Prohibition’s Iron Law, revisited. Int. J. Drug Policy 46, 156–159. 10.1016/j.drugpo.2017.05.050 [DOI] [PubMed] [Google Scholar]
- Buchanich JM, Balmert LC, Williams KE, Burke DS, 2018. The effect of incomplete death certificates on estimates of unintentional opioid-related overdose deaths in the united states, 1999–2015. Public Health Rep. 10.1177/0033354918774330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Deaton A, 2020. Deaths of Despair and the Future of Captialism. Princeton University Press, Princeton, NJ. [Google Scholar]
- Case A, Deaton A, 2015. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U. S. A 112, 15078–15083. 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Ondocsin J, Mars SG, 2017. Heroin uncertainties: Exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin.’ Int. J. Drug Policy 46, 146–155. 10.1016/j.drugpo.2017.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Clarke J, Brinkley-Rubinstein L, Marshall BDL, Alexander-Scott N, Boss R, Rich JD, 2018. Postincarceration fatal overdoses after implementing medications for addiction treatment in a statewide correctional system. JAMA Psychiatry. 10.1001/jamapsychiatry.2017.4614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadland SE, Frank Wharam JW, Schuster MA, Zhang F, Samet JH, Larochelle MR, 2017. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatr. 10.1001/jamapediatrics.2017.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Bastian BA, Trinidad JP, Spencer MR, Warner M, 2019. Regional differences in the drugs most frequently involved in drug overdose deaths: United states, 2017. Natl. Vital Stat. Reports 68, 1–15. [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Warner M, 2020. Drug Overdose Deaths in the United States, 1999–2018, NCHS Data Brief; Hyattsville, MD. [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Warner M, 2018. Drug Overdose Deaths in the United States, 1999–2017. HS Data Brief 1–8. 10.1016/j.neulet.2010.07.040 [DOI] [PubMed] [Google Scholar]
- Ingram D, FraNCnco S, 2014. 2013 NCHS Urban – Rural Classification Scheme for Counties Natl. Cent. Heal. Stat. Vital Heal. Stat 2 [PubMed] [Google Scholar]
- Jamison P, Shefte W, n.d. Falling Out [WWW Document]. Washington Post. URL https://www.washingtonpost.com/graphics/2018/local/opioid-epidemic-and-its-effect-on-african-americans/ (accessed 6.5.20). [Google Scholar]
- Jones CM, Einstein EB, Compton WM, 2018. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA - J. Am. Med. Assoc 10.1001/jama.2018.2844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury MJ, Iademarco MF, Riley WT, 2016. Precision Public Health for the Era of Precision Medicine. Am. J. Prev. Med 50, 398–401. 10.1016/j.amepre.2015.08.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein RJ, Schoenborn CA, n.d. Age Adjustment Using the 2000 Projected U.S. Population. [PubMed] [Google Scholar]
- Lippold KM, Jones CM, Olsen EO, Giroir BP, 2019. Racial/Ethnic and Age Group Differences in Opioid and Synthetic Opioid–Involved Overdose Deaths Among Adults Aged ≥18 Years in Metropolitan Areas — United States, 2015–2017. MMWR. Morb. Mortal. Wkly. Rep 68, 967–973. 10.15585/mmwr.mm6843a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden EF, Qeadan F, 2020. Racial inequities in U.S. naloxone prescriptions. Subst. Abus 41, 232–244. 10.1080/08897077.2019.1686721 [DOI] [PubMed] [Google Scholar]
- Monnat SM, 2019. The contributions of socioeconomic and opioid supply factors to U.S. drug mortality rates: Urban-rural and within-rural differences. J. Rural Stud 68, 319–335. 10.1016/j.jrurstud.2018.12.004 [DOI] [Google Scholar]
- National Association for the Advancement of Colored People (NAACP), n.d.. Criminal Justice Fact Sheet: Incarceration Trends in America [WWW Document]. URL https://www.naacp.org/criminal-justice-fact-sheet/ (accessed 6.5.20).
- Netherland J, Hansen HB, 2016. The War on Drugs That Wasn’t: Wasted Whiteness, “‘Dirty Doctors,’” and Race in Media Coverage of Prescription Opioid Misuse. Cult. Med. Psychiatry 40, 664–686. 10.1007/s11013-016-9496-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JN, Sherman SG, Rouhani S, Morales KB, McKenzie M, Allen ST, Marshall BDL, Green TC, 2019. Willingness to Use Safe Consumption Spaces among Opioid Users at High Risk of Fentanyl Overdose in Baltimore, Providence, and Boston. J. Urban Heal 96, 353–366. 10.1007/s11524-019-00365-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ, Ibrahimova A, Rudd RA, Goldberger BA, Thogmartin JR, Shelton K, 2012. A Comparison of Florida Medical Examiners’ Reports and Death Certificates for Specific Drug Related Overdose Deaths. Acad. Forensic Pathol 10.23907/2012.027 [DOI] [Google Scholar]
- Pear VA, Ponicki WR, Gaidus A, Keyes KM, Martins SS, Fink DS, Rivera-Aguirre A, Gruenewald PJ, Cerdá M, 2019. Urban-rural variation in the socioeconomic determinants of opioid overdose. Drug Alcohol Depend. 195, 66–73. 10.1016/j.drugalcdep.2018.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potier C, Laprévote V, Dubois-Arber F, Cottencin O, Rolland B, 2014. Supervised injection services: What has been demonstrated? A systematic literature review. Drug Alcohol Depend. 10.1016/j.drugalcdep.2014.10.012 [DOI] [PubMed] [Google Scholar]
- Prevention SA and M.H.S.A.C. for the A of, 2018. Using International Classification of Diseases (ICD) Codes to Assess Opioid-Related Overdose Deaths. [Google Scholar]
- Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G, 2018. Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017. MMWR. Morb. Mortal. Wkly. Rep 67 10.15585/mmwr.mm6751521e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman S, Morales K, Park J, McKenzie M, Marshall B, Green T, 2019. Acceptability of implementing community-based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. International Journal of Dr. Int. J. Drug Policy In press. [DOI] [PubMed] [Google Scholar]
- Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H, 2019. Drug overdose deaths involving fentanyl, 2011–2016. Natl. Vital Stat. Reports 68. [PubMed] [Google Scholar]
- Tiwari C, Beyer K, Rushton G, 2014. The impact of data suppression on local mortality rates: The case of cdc wonder. Am. J. Public Health 104, 1386–1388. 10.2105/AJPH.2014.301900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Centers for Disease Control and Prevention, 2020a. Synthetic opioid overdose data [WWW Document]. URL https://www.cdc.gov/drugoverdose/data/fentanyl.html (accessed 5.25.20).
- US Centers for Disease Control and Prevention, 2020b. Heroin Overdose Data [WWW Document]. URL https://www.cdc.gov/drugoverdose/data/heroin.html (accessed 5.25.20).
- US Centers for Disease Control and Prevention, 2015. Health alert: Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities [WWW Document]. URL https://emergency.cdc.gov/han/han00384.asp#_edn11 (accessed 6.5.20).
- Wilson N, Kariisa M, Seth P, Smith H, Davis NL, 2020. Drug and Opioid-Involved Overdose Deaths - United States, 2017–2018. MMWR. Morb. Mortal. Wkly. Rep 69, 290–297. 10.15585/mmwr.mm6911a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoorob M, 2019. Fentanyl shock: The changing geography of overdose in the United States. Int. J. Drug Policy 70, 40–46. 10.1016/j.drugpo.2019.04.010 [DOI] [PubMed] [Google Scholar]


