Abstract
Background
Substance use is common among youth experiencing homelessness (YEH). However, less is known about the use of multiple substances (polysubstance use), or factors associated with polysubstance use among YEH. The present study sought to identify subgroups of YEH based on their recent polysubstance use behavior, and investigate traumatic experiences, mental health and social network composition as predictors.
Methods
YEH (N = 1,032; Mage = 21.3) from three drop-in centers in Los Angeles completed an in-person survey and social network interview between October 2011 and June 2013. Latent class analysis (LCA) was used to identify subgroups of youth based on nine types of substance use in the past 30 days; latent class logistic regression was used to identify variables associated with class membership.
Results
Five polysubstance use classes were identified: heavy alcohol and marijuana (33.6%), illicit drug use (4.9%), high all polysubstance use (14.9%), primarily marijuana (18.1%), and low use (28.5%). Relative to the low use class, traumatic experiences were associated with membership in every polysubstance use class. Suicide attempts were associated with membership in the high all class (OR=9.41). Number of substance-using, homeless network members was associated with membership in the heavy alcohol and marijuana use class (OR=1.35). Number of non-substance-using network members (homeless [OR=0.29] and housed [OR=0.73]) was associated with lower odds of membership in the high all class.
Conclusions
Distinct groups of YEH can be identified by their recent polysubstance use patterns. Traumatic experiences, suicidality, and social network composition are important correlates of polysubstance use among YEH.
Keywords: polysubstance use, youth homelessness, social networks, trauma
1. Introduction
Over the past two decades, studies have documented high rates of substance use and substance use disorders among youth experiencing homelessness (YEH) (Hodgson, Shelton, van den Bree, & Los, 2013; Santa Maria, Narendorf, & Cross, 2018; Whitbeck, 2009). However, there have rarely been attempts to understand the use of multiple substances (polysubstance use) among YEH. A sizable body of literature has pointed to several factors associated with substance use among YEH, including traumatic experiences, poor mental health, and social network factors (Bender, Brown, Thompson, Ferguson, & Langenderfer, 2015; Rice, Milburn, Rotheram-Borus, Mallett, & Rosenthal, 2005a; Santa Maria et al., 2018; Whitbeck, Hoyt, & Yoder, 1999). The current study investigates how these factors may be associated with heterogeneity in polysubstance use among YEH.
1.1. Polysubstance use and associated risk factors
Similar to stably housed adolescents and young adults, tobacco, alcohol and marijuana are the most commonly used substances among YEH (Shadel, Tucker, & Golinelli, 2015; Whitbeck, 2009). Use of illicit (“hard”) drugs among YEH, such as cocaine and methamphetamines, has also been a cause for concern (Barman-Adhikari, Craddock, Bowen, Das, & Rice, 2018; Rice et al., 2005). Substance use severity is thought to vary depending on the type and number of substances used, and their associated consequences (Baer, Ginzler, & Peterson, 2003; Greene, Ennett, & Ringwalt, 1997). Previous research with YEH has tended to examine substance use independently, although in previous samples roughly half (48.5%) of YEH had engaged in polysubstance use (Rosenthal, Mallett, Milburn, & Rotheram-Borus, 2008) or were diagnosed with a polysubstance use disorder (Slesnick & Prestopnik, 2005). Polysubstance use has also been associated with being unsheltered (“sleeping rough”; Rhule-Louie, Bowen, Baer, & Peterson, 2008), inconsistent condom use (Heerde & Hemphill, 2016), injection drug use (Al-Tayyib, Rice, Rhoades, & Riggs, 2014), and, among the general population, increased risk of overdose (Gladden, O’Donnell, Mattson, & Seth, 2019).
The Risk Amplification Model (RAM) may help explain polysubstance use behaviors among YEH (Whitbeck & Hoyt, 1999). The RAM posits that caretaker abuse, family conflict, and deviant peer relationships place adolescents at greater risk for running away and experiencing homelessness. In turn, traumatic experiences and exposure to deviant peers while homeless amplify developmental risks. In addition, substance use appears to be highly comorbid with YEH’s mental health conditions, including depression (Whitbeck, Hoyt, & Bao, 2000), post-traumatic stress disorder (PTSD; Davis et al., 2019; Santa Maria et al., 2018; Thompson, McManus, & Voss, 2006), and suicidality (Salomonsen-Sautel et al., 2008; Yoder, Longley, Whitbeck, & Hoyt, 2008). However, relationships between traumatic experiences, poor mental health, and specific polysubstance use profiles have yet to be investigated.
Social network factors are also an important correlate of substance use among YEH. The RAM and a large body of subsequent research has shown that affiliation with social network members (alters) who engage in substance use or other antisocial behaviors (violence, theft, etc.) is associated with youths’ own substance use (Heinze, Toro, & Urberg, 2004; Rice, Milburn, & Monro, 2011; Whitbeck & Hoyt, 1999). The housing status of one’s network members may be important to consider well, as a greater proportion of homeless individuals within one’s network has been associated with greater substance use (Green Jr., de la Haye, Tucker, & Golinelli, 2013; Martino et al., 2011; Rice et al., 2005). Conversely, YEH who name parents, family members and home-based peers in their close personal networks tend to report fewer substance use risks (Milburn et al., 2009; Rice, Milburn, & Rotheram-Borus, 2007).
Similar substance use behaviors between social ties is an example of homophily, or the tendency for individuals to affiliate with others similar to themselves (Lazarsfeld & Merton, 1954). Homophily based on gender, race, and social class is pervasive (McPherson, Smith-Lovin, & Cook, 2001), and we argue that YEH’s relationships are homophilous in regards to substance use behaviors as well. Social network theory also acknowledges that individuals may have multiple, overlapping relationships with their respective network members (Wellman & Wortley, 1990). For YEH, this multiplexity is evident in terms of youths’ relationships with alters based on their housing status and substance use behaviors. While previous research suggests that affiliation with alters who are substance using and unhoused are independently predictive of greater risk (Rice et al., 2005), the multiplex nature of these relationships has not been fully explored.
1.2. The Current Study
The current study has two aims. First, we sought to understand the prevalence and heterogeneity in polysubstance use among YEH. Secondly, we sought to test complementary models of risk and protective factors for polysubstance use. Specifically, we tested whether (a) traumatic experiences and mental health problems, or (b) social network composition, are better predictors of heterogeneity in polysubstance use among YEH. By identifying specific polysubstance use profiles, and incorporating trauma, mental health, and social network characteristics into our predictive models, the current study will add greater specificity in predicting polysubstance use behaviors among YEH.
2. Materials and methods
2.1. Participants and procedures
Participants were 1,032 adolescents and young adults (Mage = 21.3, SD = 2.1) recruited from three drop-in centers in Los Angeles, California. The majority of the sample was male and racially diverse. Participant recruitment and data collection occurred in four waves from October 2011 to June 2013, allowing for sufficient recruitment of new individuals accessing drop-in services. Individuals aged 14 to 25 were approached to participate in the study. YEH aged 18 and older provided informed consent to participate, and YEH under the age of 18 provided informed assent. The University IRB waived the need to obtain consent from adolescents’ parents or guardians, since youth accessing drop-in centers were deemed unaccompanied minors. After providing informed consent/assent, participants completed an interviewer-administered social network interview, and a computerized survey assessing demographics, homelessness experiences, traumatic experiences and mental health. Participants received $20 as compensation for their time. All procedures were IRB approved.
2.2. Measures
2.2.1. Demographics and homelessness experiences
Demographic variables included age, male gender (reference: female), transgender (reference: cisgender male or female), Black/African American, Hispanic/Latino/a, and other race (reference: non-Hispanic White), and LGBQ identity (reference: heterosexual/straight). Participants were also asked whether they had ever been in the foster care (yes/no) and their age when they first experienced homelessness. Youths’ current living situation was assessed by asking them to choose from a list of possible accommodations. We used a definition of literal homelessness from Tsemberis, McHugo, Williams, Hanrahan and Stefancic (2007) as those who were currently staying in a shelter, a stranger’s home, hotel, motel, street, beach, tent or campsite, abandoned building, car, or bus. Youth who indicated other living arrangements, such as in a family member or relative’s home, a group home, transitional living program, or their own apartment, etc., were not considered literally homeless but rather, unstably housed.
2.2.2. Traumatic experiences and mental health
Traumatic experiences were assessed using the UCLA PTSD Reaction Index for DSM-IV (Pynoos, Rodriguez, Steinberg, Stuber, & Frederick, 1998). Participants responded yes or no to eight questions asking whether they had ever been the victim of physical abuse, sexual abuse, had ever witnessed physical abuse at home, been the victim of physical assault or sexual assault, witnessed physical violence or had seen a dead body in their neighborhood, or ever had a loved one become seriously injured or die by violence. Internal consistency was excellent (α = 0.90). Affirmative responses were summed to create a count of traumatic experiences (range: 0–8).
Post-traumatic Stress Disorder was assessed using the four-item Primary Care PTSD screen (PC-PTSD; Prins et al., 2003). The scale assessed PTSD symptoms in the past month related to an event in their lifetime that was “frightening, horrible, or upsetting” (α = 0.84). A dichotomous variable was created for participants who answered “yes” to three or more symptoms, indicating a positive screen.
The Center for Epidemiologic Studies Depression Scale (CES-D-10) was used to assess how often participants experienced depressive symptoms in the past week, from 1 “Less than 1 day or never” to 4 “5–7 days” (α = 0.79). Responses were summed and scores were dichotomized: those exceeding the clinical cutoff score (≥ 10) indicated a probable depression diagnosis.
Suicidality was assessed by asking participants, “During the past 12 months, how many times did you actually attempt suicide?” (Response options ranged from 0 to 6 or more times). Responses were dichotomized to reflect any suicide attempt in the past 12 months.
2.2.3. Social network composition
The social network interview was completed in-person with a trained research staff member (see Rice, Barman-Adhikari, Milburn, & Monro, 2012). Participants were asked to list people they interacted with in the past month: friends, family, people they “hang out/chill/have conversations with,” romantic/sexual partners, caseworkers/drop-in center staff, old friends from home, people they live/squat with, and other people they know from the street. After listing alters, participants were asked a series of questions about each alter: whether each alter had unstable housing, was homeless, or lived in a shelter, and each alter’s substance use behavior in the past 30 days. Four variables were created to describe the composition of participants’ egocentric networks: 1) number of homeless, substance-using alters, 2) number of homeless, non-substance-using alters, 3) number of housed, substance-using alters, and 4) number of housed, non-substance-using alters. Alters were categorized as substance-using if participants responded “yes” the alter “drank alcohol to the point of drunkenness”, “used marijuana”, or used other drugs (cocaine, heroin, methamphetamines, ecstasy, or prescription drug misuse) in the past 30 days. Non-substance-using alters were those whom the participant reported “no” to all of the above questions.1 The four categories are mutually exclusive and add up to the total number of alters nominated by each participant.
2.2.4. Substance use
Participants were asked how many times they had used alcohol, engaged in binge drinking (5 or more drinks in a row within a couple of hours), heavy alcohol use (binge alcohol use on six or more days), marijuana, cocaine, heroin, methamphetamines, ecstasy, or misused prescription drugs (without a doctor’s prescription or more than prescribed) in the past 30 days. Each type of substance use was dichotomized as any or no use in the past 30 days.
2.3. Data Analysis
Latent class analysis (LCA) in Mplus version 8 (Muthén & Muthén, 1998–2017) was used to classify individuals’ substance use in the past 30 days. All nine dichotomous substance use variables were treated as observed categorical variables, and a series of fit statistics were used to identify the best number of classes. Lower negative two log likelihood (−2LL), Akaike Information Criteria (AIC), Bayesian Information Criteria (BIC), sample-size adjusted BIC values indicate a better fitting model. In addition, non-significant test statistics for the Vuong Lo-Mendell-Rubin adjusted likelihood ratio test (VLRT) and the bootstrapped likelihood ratio test (BLRT) indicated that a model with k −1 classes was a better fitting model.
Latent class regression, a variant of multinomial logistic regression, was used to examine factors associated with emergent classes. We first ran a preliminary model using demographics and homelessness experiences as predictors to determine which of these variables to include in the final multivariate model. We also ran bivariate correlations to evaluate whether multicollinearity was present among the predictor variables. Next, we estimated a full model that included demographics, number of traumatic experiences, depression, PTSD, and social network variables together. Just over ten percent (10.2%) of the sample did not complete the social network interview, and there was a relatively high amount of missing for depression diagnosis (10.4%). Missing data were handled using full information maximum likelihood with robust standard errors in Mplus. This is a superior strategy to listwise deletion and equivalent to using multiple imputation techniques when data are assumed to be missing at random (Enders, 2011).
3. Results
3.1. Descriptive Statistics
Full descriptive statistics can be viewed in Table 1. On average, participants reported 2.8 (SD = 2.1) traumatic experiences in their lifetime, 41.0% met diagnostic criteria for depression, 27.7% met diagnostic criteria for PTSD, and 11.5% had attempted suicide in the past 12 months. Participants nominated an average of 10.5 alters (SD = 7.2). Marijuana (73.3%) was the most common substance used, followed by alcohol (68.5%), binge drinking (46.9%), methamphetamines (24.0%), prescription drug misuse (19.1%), heavy alcohol use (18.6%), cocaine (15.9%), ecstasy (14.6%), and heroin (9.9%).
Table 1.
Participant Characteristics (N = 1,032)
| Variable | M (SD) or n (%) |
|---|---|
| Demographics | |
| Age | |
| Gender | 21.3 (2.1) |
| Male | 723 (71.5%) |
| Female | 271 (26.8%) |
| Transgender (male to female) | 13 (1.3%) |
| Transgender (female to male) | 4 (0.4%) |
| Race/Ethnicity | |
| Black/African American | 241 (23.4%) |
| Hispanic/Latino/a | 138 (13.4%) |
| White | 493 (38.1%) |
| Asian | 6 (0.6%) |
| Native American | 30 (2.9%) |
| Native Hawaiian/Pacific Islander | 6 (0.6%) |
| Multiple races/ethnicities | 197 (19.1%) |
| LGBQ | 247 (23.9%) |
| Foster care / Homelessness Experiences | |
| Foster care placement | 348 (33.7%) |
| Age at first homelessness | 16.7 (3.9) |
| Literal homelessness | 568 (55.0%) |
| Mental Health / Trauma | |
| Num. traumatic experiences | 2.8 (2.1) |
| Depression | 423 (41.0%) |
| PTSD | 286 (27.7%) |
| Suicide attempt (past year) | 119 (11.5%) |
| Social Network (Alters) | |
| Network size (Total num.) | 10.5 (7.2) |
| Num. homeless, substance-using alters | 3.5 (4.6) |
| Num. homeless, non-substance-using alters | 0.6 (1.4) |
| Num. housed, substance-using alters | 2.9 (3.9) |
| Num. housed, non-substance using alters | 3.5 (4.3) |
| Substance use (Past 30-day) | |
| Alcohol (any) | 707 (68.5%) |
| Alcohol (binge use) | 484 (46.9%) |
| Alcohol (heavy use) | 192 (18.6%) |
| Marijuana | 756 (73.3%) |
| Cocaine | 164 (15.9%) |
| Heroin | 102 (9.9%) |
| Methamphetamine | 248 (24.0%) |
| Ecstasy | 151 (14.6%) |
| Prescription drug misuse | 197 (19.1%) |
3.2. Latent Class Analysis
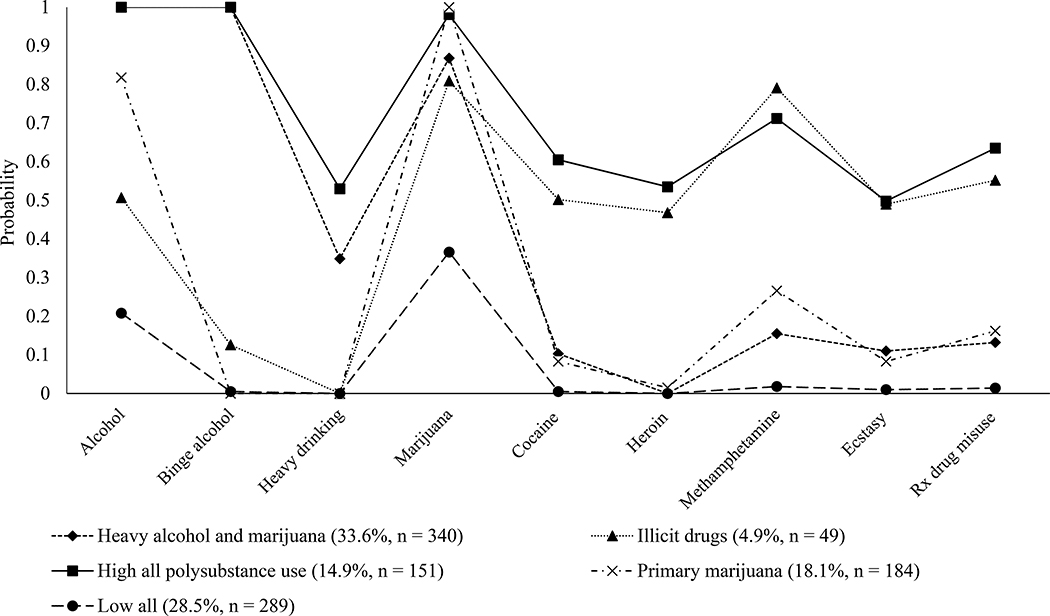
Results of our class enumeration indicated a five-class solution fit the data best (see supplemental Table 1 for fit statistics). Although VLRT and LRT tests indicated a six-class model, a five-class model was chosen for several reasons. First, plotted BIC and aBIC values point to an “elbow” when estimating five or more classes, indicating a plateau effect. Adjusted BIC is also a robust indicator of fit, while other measures often select the k+1 model (Nylund, Asparouhov, & Muthén, 2007). Secondly, in the six-class solution, several profiles contained less than 5% of the sample, indicating potential instability in class membership. Probabilities of endorsing each type of substance use within each class are displayed in Figure 1. Given these probabilities, we assigned the following labels to each class: high all polysubstance use (n = 151; 14.9%), primarily illicit drug use (i.e., marijuana2, cocaine, heroin, methamphetamine, ecstasy, and prescription drug misuse; n = 49; 4.9%), heavy alcohol and marijuana use (n = 340; 33.6%), primarily marijuana (n = 184; 18.1%), and low use (n = 289; 28.5%).
Figure 1.
Probabilities of substance use endorsement by emergent classes. Five latent classes emerged: a class with a high probability of heavy alcohol and marijuana use (Heavy alcohol and marijuana), a class with high probabilities of all substances (High all polysubstance use), a class with high probabilities of illicit drugs (i.e., marijuana, cocaine, heroin, methamphetamine, ecstasy, and prescription drug misuse), a class with a high probability of marijuana use (primary marijuana), and a class with relatively low substance use probabilities (Low all).
3.3. Predictors of polysubstance use class membership
In preliminary model building steps, demographic variables had significant associations with polysubstance use class membership. However, foster care involvement, age at first homelessness, and literal homelessness did not add predictive value, and were dropped from further analysis to conserve statistical power. As shown in Supplemental Table 2, the bivariate correlation between number of traumatic experiences and PTSD was moderately strong (rpb = 0.49), but did not exceed the 0.8 cutoff most commonly used to determine if multicollinearity is present (Vatcheva, Lee, McCormick, & Rahbar, 2016); therefore, both predictor variables were kept in subsequent models. Results of the full model are displayed in Table 2. All Odds Ratios (OR) are relative to the low all polysubstance use reference class. Number of traumatic experiences was associated with membership in all four polysubstance use classes (High all polysubstance use: OR=1.29 [1.10, 1.52]; Illicit drugs: OR=1.71 [1.24, 2.34]; Heavy alcohol and marijuana: OR=1.29 [1.14, 1.46]; Primarily marijuana: OR=1.32 [1.13, 1.54]). Past year suicide attempt was associated with membership in the high all polysubstance use class (OR=9.41 [3.13, 28.31]). Positive depression and PTSD screens were not significantly associated with polysubstance use class membership. For social network characteristics, the number of homeless, substance-using alters was positively related to membership in the heavy alcohol and marijuana use class (OR=1.35 [1.05, 1.74]); the number of non-substance-using alters (homeless: OR = 0.29; 95% CI: 0.13, 0.63, and housed: OR = 0.73 95% CI: 0.56, 0.93) were inversely related to membership in the high all polysubstance use class.
Table 2.
Predictors of polysubstance use classes among youth experiencing homelessness. Reference is Low all substance use class; n = 289.
| High all (n = 151) | Illicit drugs (n = 49) | Heavy alcohol & marijuana (n = 340) | Primary marijuana (n = 184) | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Demographics | ||||
| Age | 1.17 (0.98, 1.38) | 1.45 (1.07, 1.97) | 1.15 (1.02, 1.29) | 1.22 (1.05, 1.41) |
| Male gender | 3.12 (1.32, 7.39) | 12.54 (1.36, 80.72) | 2.32 (1.34, 4.02) | 1.64 (0.82, 3.32) |
| Trans/non-binary gender | 2.90 (0.02, 368.20) | 0.00 (0.00, 0.00) | 2.21 (0.15, 31.93) | 4.54 (0.40, 52.01 |
| African American (rel: White) | 0.47 (0.17, 1.30) | 0.40 (0.11, 1.50) | 1.03 (0.54, 1.97) | 1.07 (0.42, 2.73) |
| Hispanic/Latino/a (rel: White) | 1.21 (0.49, 3.01) | 0.10 (0.00, 13.73) | 1.48 (0.73, 3.00) | 0.78 (0.28, 2.14) |
| Other racea (rel: White) | 0.26 (0.09, 0.74) | 0.45 (0.13, 1.56) | 1.01 (0.52, 1.96) | 1.05 (0.44, 2.49) |
| LGBQ | 1.09 (0.40, 2.97) | 6.04 (1.43, 25.45) | 1.47 (0.81, 2.68) | 2.67 (1.29, 5.53) |
| Trauma / Mental Health | ||||
| Num. traumatic experiences | 1.29 (1.10, 1.52) | 1.71 (1.24, 2.34) | 1.29 (1.14, 1.46) | 1.32 (1.13, 1.54) |
| Depression | 1.03 (0.51, 2.10) | 2.21 (0.70, 6.98) | 1.00 (0.61, 1.62) | 1.53 (0.82, 2.87) |
| PTSD | 1.14 (0.47, 2.76) | 0.41 (0.11, 1.49) | 0.84 (0.44, 1.62) | 0.84 (0.40, 1.79) |
| Suicide attempt | 9.41 (3.13, 28.31) | 3.07 (0.58, 16.22) | 0.98 (0.35, 2.76) | 1.59 (0.51, 4.97) |
| Social Network (Alters) | ||||
| Network size (Total num.) | 1.15 (0.88, 1.49) | 4.22 (0.49, 36.32) | 0.96 (0.77, 1.21) | 1.06 (0.76, 1.46) |
| Num. homeless, substance-using | 1.19 (0.90, 1.58) | 0.33 (0.00, 2.78) | 1.35 (1.05, 1.74) | 1.27 (0.91, 1.77) |
| Num. homeless, non-substance-using | 0.29 (0.13, 0.63) | 0.08 (0.00, 2.09) | 0.97 (0.75, 1.26) | 0.78 (0.53, 1.13) |
| Num. housed, substance-using | 0.94 (0.72, 1.23) | 0.27 (0.03, 2.32) | 1.16 (0.92, 1.47) | 0.97 (0.70, 1.35) |
| Num. housed, non-substance-using | 0.73 (0.56, 0.93) | 0.26 (0.03, 2.09) | 0.99 (0.79, 1.24) | 0.91 (0.66, 1.27) |
Note: Bold indicates confidence interval does not include 1.
Other race includes Asian, American Indian, Native Hawaiian/Pacific Islander, and multiple races.
4. Discussion
Despite consistent evidence of higher substance use risks, this is the first known study to investigate heterogeneity in polysubstance use among YEH. Results showed a high probability of recent polysubstance use among most participants. The largest class was made up of youth with heavy alcohol and marijuana use. This was followed by a class of youth who primarily had a high probability of recently using marijuana. Consistent with previous research (Whitbeck, 2009), “hard” drug use was less common, but still concerning, as the illicit drug use and high all classes made up almost a fifth of the sample. Notably, the second largest class, comprising just over a quarter of youth, was made up of those with relatively low probabilities of substance use. Additionally, we identified important risk and protective factors related to polysubstance use class membership.
Among the trauma and mental health variables, number of traumatic experiences emerged as the most consistent predictor of polysubstance use class membership. It is possible that YEH may engage in polysubstance use as a means to cope with traumatic experiences such as physical and sexual abuse, or direct or indirect violence victimization on the streets or at home. This is in line with prior theoretical and empirical work investigating the Risk Amplification Model (RAM), which posits cyclical relationships between victimization, trauma, and street experiences, which often lead to maladaptive behavioral health outcomes (Whitbeck et al., 1999). In fact, recent research involving treatment-involved YEH supports a cyclical relationship in which trauma symptoms precede substance use, which then is associated with more trauma symptoms (Davis et al., 2019). Although our data are cross-sectional, most traumatic events recorded in these data precede current substance use and thus these results lend further support for theoretical models such as the RAM, and suggest that polysubstance use is yet another unfortunate consequence of victimization and other traumatic experiences.
Aside from trauma, suicidality emerged as a particularly strong predictor, but only for the high all polysubstance use class. This suggests that individuals with high probabilities of engaging in polysubstance use may include a group of youth who are at high risk for mental health comorbidities. However, this may be isolated to more severe mental health problems (e.g., suicidality) as probable depression and PTSD screens were not significantly related to membership in any polysubstance use class. Our results indicate that when screening for substance use among YEH, victimization and other traumatic experiences, as well as suicidality, may be more important severity indicators than depression or PTSD symptoms alone.
Although trauma emerged as a consistent correlate of polysubstance use, social network composition proved to offer additional specificity in exploring polysubstance use behaviors. Namely, affiliating with more homeless, substance-using individuals was associated with greater odds of membership in the heavy alcohol and marijuana use class. The fact that this network characteristic was associated with heavy alcohol and marijuana use (and not other polysubstance use behaviors) could indicate homophily (i.e. shared behaviors across network ties between peers), given that marijuana and alcohol use were the two most prevalent substance use behaviors among study participants. These substances may be more readily available amongst street-peers, leading to greater social pressures to use them.
Of course, social network influences can be beneficial for avoiding risky polysubstance use behaviors as well. In this study, youth with ties to individuals they believed to be non-substance users (e.g., individuals who did not drink alcohol to the point of drunkenness, or use marijuana or other drugs) were more likely to be in the low use class than the high all polysubstance use class. This was true whether youths’ network ties were homeless or housed. Interestingly, the difference in odds ratios suggests that ties to homeless, non-substance-using peers may be more strongly associated with being in the low all class than ties to housed, non-substance-using peers. This may suggest that homeless network members may have a stronger influence on homeless youths’ substance use behaviors than housed ones. Alternatively, substance use behaviors may play a role in who homeless youth choose to affiliate with (i.e., social selection). In sum, having non-substance using individuals in one’s personal network may be protective against a particularly risky pattern of polysubstance use. This supports prior work by Milburn and colleagues (2009), who identified a “protected cluster” of youth who tended to be younger, female, and more likely to have prosocial ties.
Results of this study have important implications for research and clinical practice with YEH. Namely, heterogeneity in youths’ substance use behaviors does not lend support for a “one size fits all” approach to screening, prevention, and treatment services (Greene et al., 1997; Narendorf, Bowen, Santa Maria, & Thibaudeau, 2018). When screening for substance use broadly, traumatic experiences may be a more useful risk factor than self-reported depression or PTSD symptomology. This study lends support for including suicide prevention efforts in screening procedures, as suicidality and multiple forms of polysubstance use likely co-occur. In addition, recent substance use may be more likely among YEH who are older, male, and LGBQ; age of first homelessness and experience of “literal” homelessness (i.e., unsheltered) status may be less important factors. Social network characteristics are also important to consider, as polysubstance use is related to the perceived substance use and housing status of youths’ network ties. Our unique findings lend some support for developing social network interventions to prevent and decrease harmful polysubstance use among YEH. Some guidance exists for developing such interventions (Dempsey, McAlaney, & Bewick, 2018; Nyamathi et al., 2007; Stewart, Reutter, Letourneau, & Makwarimba, 2009; Valente, 2012), yet they remain relatively untested among YEH populations.
This study is not without limitations. It relies on cross-sectional data; therefore, assertions about temporal ordering cannot be made. More longitudinal research is needed to identify and prevent adverse experiences before or after young people leave home (Whitbeck et al., 2000). Secondly, the data were collected from 2011 to 2013 in Los Angeles and may not generalize to YEH in other geographic or historical settings. Third, the sample size of the illicit drug class was relatively small, potentially resulting in an overfit of the model and imprecise estimates. We should also note that a limitations of self-report data include social desirability (possibly inflating the size of the low all class) and recall biases which could have yielded inaccuracies in recent polysubstance use behavior. Lastly, some of our substance use measures were limited, in that they did not assess for tobacco use or the frequency or quantity of marijuana use. This prevented us from making assumptions about the prevalence of marijuana use disorders in this sample.
4.1. Conclusions
Results of this study suggest that there is significant heterogeneity in polysubstance use behaviors among youth experiencing homelessness utilizing drop-in center services. In addition, risk and protective factors for specific polysubstance use profiles were identified. Given the consistent relationships between traumatic experiences and recent polysubstance use, such behaviors could be viewed as a coping mechanism or “self-medication” (Khantzian, 1997). Future research may consider how various moderators (e.g., gender, sexual orientation) influence the relationships between risk and protective factors and polysubstance use among YEH. In conclusion, previous traumatic experiences, suicidality, and social network composition are associated with emergent polysubstance use classes among YEH.
Supplementary Material
Highlights.
Five polysubstance use classes were found.
Traumatic experiences were associated with all polysubstance use classes.
Homeless, substance-using peers were associated with heavy alcohol and marijuana use.
Non-substance-using peers were negatively associated with being in the high all polysubstance use class.
Acknowledgements
We would like to thank the youth and drop-in center staff who volunteered their time to make this research possible.
Role of Funding Source: This work was supported by National Institute of Mental Health grant number R01 MH093336. The funding source did not have any role in the study design; in the collection, analysis and interpretation of data; writing the report; or the decision to submit the article for publication.
Footnotes
Conflict of Interest: No conflict declared
We attempted to create more alter categories based on the type of substance use participants perceived each alter to use (i.e., used alcohol and marijuana only, or used alcohol, marijuana, and illicit drugs). However, the number of alters in these categories was highly correlated (r > .80), and therefore we distinguished alters as those who were perceived to use any type of substance vs. no substance use
Note that recreational marijuana use became legal in the state of California in 2016, after study data were collected. Therefore, it is included in the “primary illicit drug use” class.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Al-Tayyib AA, Rice E, Rhoades H, & Riggs P (2014). Association between prescription drug misuse and injection among runaway and homeless youth. Drug and Alcohol Dependence, 134, 406–409. 10.1016/j.drugalcdep.2013.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS, Ginzler JA, & Peterson PL (2003). DSM-IV alcohol and substance abuse and dependence in homeless youth. Journal of Studies on Alcohol, 64(1), 5–14. [DOI] [PubMed] [Google Scholar]
- Barman-Adhikari A, Craddock J, Bowen E, Das R, & Rice E (2018). The Relative Influence of Injunctive and Descriptive Social Norms on Methamphetamine, Heroin, and Injection Drug Use Among Homeless Youths: The Impact of Different Referent Groups. Journal of Drug Issues, 48(1), 17–35. [Google Scholar]
- Bender K, Brown SM, Thompson SJ, Ferguson KM, & Langenderfer L (2015). Multiple Victimizations Before and After Leaving Home Associated With PTSD, Depression, and Substance Use Disorder Among Homeless Youth. Child Maltreatment, 20(2), 115–124. 10.1177/1077559514562859 [DOI] [PubMed] [Google Scholar]
- Davis JP, Diguiseppi G, De Leon J, Prindle J, Sedano A, Rivera D, … Rice E (2019). Understanding pathways between PTSD, homelessness, and substance use among adolescents. Psychology of Addictive Behaviors, 33(5), 467–476. 10.1037/adb0000488 [DOI] [PubMed] [Google Scholar]
- Dempsey RC, McAlaney J, & Bewick BM (2018). A critical appraisal of the social norms approach as an interventional strategy for health-related behavior and attitude change. Frontiers in Psychology, 9 10.3389/fpsyg.2018.02180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladden RM, O’Donnell J, Mattson CL, & Seth P (2019). Changes in Opioid-Involved Overdose Deaths by Opioid Type and Presence of Benzodiazepines, Cocaine, and Methamphetamine - 25 States, July-December 2017 to January-June 2018. MMWR. Morbidity and Mortality Weekly Report, 68(34), 737–744. 10.15585/mmwr.mm6834a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green HD Jr., de la Haye K, Tucker JS, & Golinelli D (2013). Shared risk: Who engages in substance use with American homeless youth? Addiction, 108(9), 1618–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene JM, Ennett ST, & Ringwalt CL (1997). Substance use among runaway and homeless youth in three national samples. American Journal of Public Health, 87(2), 229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heerde JA, & Hemphill SA (2016). Sexual Risk Behaviors, Sexual Offenses, and Sexual Victimization Among Homeless Youth: A Systematic Review of Associations With Substance Use. Trauma, Violence, and Abuse, 17(5), 468–489. 10.1177/1524838015584371 [DOI] [PubMed] [Google Scholar]
- Heinze HJ, Toro PA, & Urberg KA (2004). Antisocial behavior and affiliation with deviant peers. Journal of Clinical Child and Adolescent Psychology, 33(2), 336–346. 10.1207/s15374424jccp3302_15 [DOI] [PubMed] [Google Scholar]
- Hodgson KJ, Shelton KH, van den Bree MBM, & Los FJ (2013). Psychopathology in Young People Experiencing Homelessness: A Systematic Review. American Journal of Public Health, 103(6), e24–e37. 10.2105/AJPH.2013.301318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications Harvard Review of Psychiatry. Lippincott Williams and Wilkins; 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Lazarsfeld PF, & Merton RK (1954). Friendship as a social process: a substantive and methodological analysis In Berger M, Abel T, & Page CH (Eds.), Freedom and control in modern society (pp. 18–66). New York: Van Nostrand. [Google Scholar]
- Martino SC, Tucker JS, Ryan G, Wenzel SL, Golinelli D, & Munjas B (2011). Increased Substance Use and Risky Sexual Behavior Among Migratory Homeless Youth: Exploring the Role of Social Network Composition. Journal of Youth and Adolescence, 40(12), 1634–1648. 10.1007/s10964-011-9646-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, & Cook JM (2001). Birds of a Feather: Homophily in Social Networks. Annual Review of Sociology, 27(1), 415–444. 10.1146/annurev.soc.27.1.415 [DOI] [Google Scholar]
- Milburn NG, Rice E, Rotheram-Borus MJ, Mallett S, Rosenthal D, Batterham P, … Duan N (2009). Adolescents Exiting Homelessness Over Two Years: The Risk Amplification and Abatement Model. Journal of Research on Adolescence, 19(4), 762–785. 10.1111/j.1532-7795.2009.00610.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milburn N, Liang LJ, Lee SJ, Rotheram-Borus MJ, Rosenthal D, Mallett S, … Lester P (2009). Who is doing well? A typology of newly homeless adolescents. Journal of Community Psychology, 37(2), 135–147. 10.1002/jcop.20283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (n.d.). Mplus User’s Guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Narendorf SC, Bowen E, Santa Maria D, & Thibaudeau E (2018). Risk and resilience among young adults experiencing homelessness: A typology for service planning. Children and Youth Services Review, 86, 157–165. 10.1016/j.childyouth.2018.01.034 [DOI] [Google Scholar]
- Nyamathi A, Hudson A, Mutere M, Christiani A, Sweat J, Nyamathi K, & Broms T (2007). Drug use and barriers to and facilitators of drug treatment for homeless youth. Patient Preference and Adherence, 1, 1–8. [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- K. P. Vatcheva, Lee M, McCormick JB, & Rahbar MH (2016). Multicollinearity in Regression Analyses Conducted in Epidemiologic Studies. Epidemiology, 06(02). 10.4172/2161-1165.1000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, … Sheikh JI (2003). The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. 10.1185/135525703125002360 [DOI] [Google Scholar]
- Pynoos R, Rodriguez N, Steinberg A, Stuber M, & Frederick C (1998). The UCLA PTSD Reaction Index for DSM IV (Revision 1) Los Angeles, CA. [Google Scholar]
- Rhule-Louie DM, Bowen S, Baer JS, & Peterson PL (2008). Substance use and health and safety among homeless youth. Journal of Child and Family Studies, 17(3), 306–319. 10.1007/s10826-007-9142-5 [DOI] [Google Scholar]
- Rice E, Milburn NG, & Rotheram-Borus MJ (2007). Pro-social and problematic social network influences on HIV/AIDS risk behaviours among newly homeless youth in Los Angeles. AIDS Care, 19(5), 697–704. 10.1080/09540120601087038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice Eric, Barman-Adhikari A, Milburn NG, & Monro W (2012). Position-specific HIV risk in a large network of homeless youths. American Journal of Public Health, 102(1), 141–147. 10.2105/AJPH.2011.300295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice Eric, Milburn NG, & Monro W (2011). Social Networking Technology, Social Network Composition, and Reductions in Substance Use Among Homeless Adolescents. Prevention Science, 12(1), 80–88. 10.1007/s11121-010-0191-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice Eric, Milburn NG, Rotheram-Borus MJ, Mallett S, & Rosenthal D (2005). The Effects of Peer Group Network Properties on Drug Use Among Homeless Youth. The American Behavioral Scientist, 48(8), 1102–1123. 10.1177/0002764204274194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal D, Mallett S, Milburn N, & Rotheram-Borus MJ (2008). Drug Use Among Homeless Young People in Los Angeles and Melbourne. Journal of Adolescent Health, 43(3), 296–305. 10.1016/j.jadohealth.2008.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomonsen-Sautel S, Van Leeuwen JM, Gilroy C, Boyle S, Malberg D, & Hopfer C (2008). Correlates of Substance Use Among Homeless Youths in Eight Cities. American Journal on Addictions, 17(3), 224–234. 10.1080/10550490802019964 [DOI] [PubMed] [Google Scholar]
- Santa Maria DM, Narendorf SC, & Cross MB (2018). Prevalence and Correlates of Substance Use in Homeless Youth and Young Adults. Journal of Addictions Nursing, 29(1), 23–31. 10.1097/JAN.0000000000000206 [DOI] [PubMed] [Google Scholar]
- Shadel WG, Tucker JS, & Golinelli D (2015). Readjusting Our Priorities: Helping Homeless Youth Quit Smoking. American Journal of Preventive Medicine, 49(6), 970–973. 10.1016/J.AMEPRE.2015.05.029 [DOI] [PubMed] [Google Scholar]
- Slesnick N, & Prestopnik J (2005). Dual and multiple diagnosis among substance using runaway youth. American Journal of Drug and Alcohol Abuse, 31(1), 179–201. 10.1081/ADA-200047916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart M, Reutter L, Letourneau N, & Makwarimba E (2009). A support intervention to promote health and coping among homeless youths. The Canadian Journal of Nursing Research = Revue Canadienne de Recherche En Sciences Infirmieres, 41(2), 55–77. [PubMed] [Google Scholar]
- Thompson SJ, McManus H, & Voss T (2006). Posttraumatic stress disorder and substance abuse among youth who are homeless: Treatment issues and implications. Brief Treatment and Crisis Intervention, 6(3), 206–217. 10.1093/brief-treatment/mhl002 [DOI] [Google Scholar]
- Valente TW (2012). Network Interventions. Science, 337(6090), 49–53. 10.1126/science.1217330 [DOI] [PubMed] [Google Scholar]
- Wellman B, & Wortley S (1990). Different Strokes from Different Folks: Community Ties and Social Support. American Journal of Sociology, 96(3), 558–588. 10.1086/229572 [DOI] [Google Scholar]
- Whitbeck LB (2009). Mental health and emerging adulthood among homeless young people Mental health and emerging adulthood among homeless young people. New York, NY: Psychology Press. [Google Scholar]
- Whitbeck LB, & Hoyt DR (1999). Nowhere to grow: Homeless and runaway adolescents and their families Social institutions and social change. Hawthorne, NY: Aldine de Gruyter. [Google Scholar]
- Whitbeck LB, Hoyt DR, & Bao WN (2000). Depressive symptoms and co-occurring depressive symptoms, substance abuse, and conduct problems among runaway and homeless adolescents. Child Development, 71(3), 721–732. 10.1111/1467-8624.00181 [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Hoyt DR, & Yoder KA (1999). A Risk-Amplification Model of Victimization and Depressive Symptoms Among Runaway and Homeless Adolescents. American Journal of Community Psychology, 27(2), 273–296. 10.1023/A:1022891802943 [DOI] [PubMed] [Google Scholar]
- Yoder KA, Longley SL, Whitbeck LB, & Hoyt DR (2008). A Dimensional Model of Psychopathology Among Homeless Adolescents: Suicidality, Internalizing, and Externalizing Disorders. Journal of Abnormal Child Psychology, 36(1), 95–104. 10.1007/s10802-007-9163-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.