Adolescent and young adult (AYA) reproductive healthcare needs are not diminished during pandemics. Indeed, needs for family planning services may be heightened due to a variety of environmental changes in response to the pandemic, including amount of parental supervision, daily structure, and usual ways of accessing contraception and condoms. Healthcare professionals (HCPs) caring for AYA patients need to acknowledge that contraception is an essential need and rapidly adopt new approaches to providing this crucial care.
In response to the COVID-19 pandemic HCPs are exploring novel ways to assure delivery of essential healthcare services and minimize exposure risks to personnel and patients, including virtual care. Fortunately, both phone and video platforms are well-suited to providing contraceptive care. While an in-person encounter may be ideal, many reproductive healthcare services can be performed virtually including contraception counseling, provision and maintenance of regular and emergency contraception, and sexual risk-reduction counseling. We propose the following approach for provision of contraception to adolescents during COVID-19, leveraging virtual care and minimizing the need for in-person visits (Figure 1). This approach can be used by a variety of HCPs from triage nurses to advanced care practitioners and across telehealth and in-person settings.
Figure 1: Algorithm for Providing Contraception for Young People During a Pandemic.
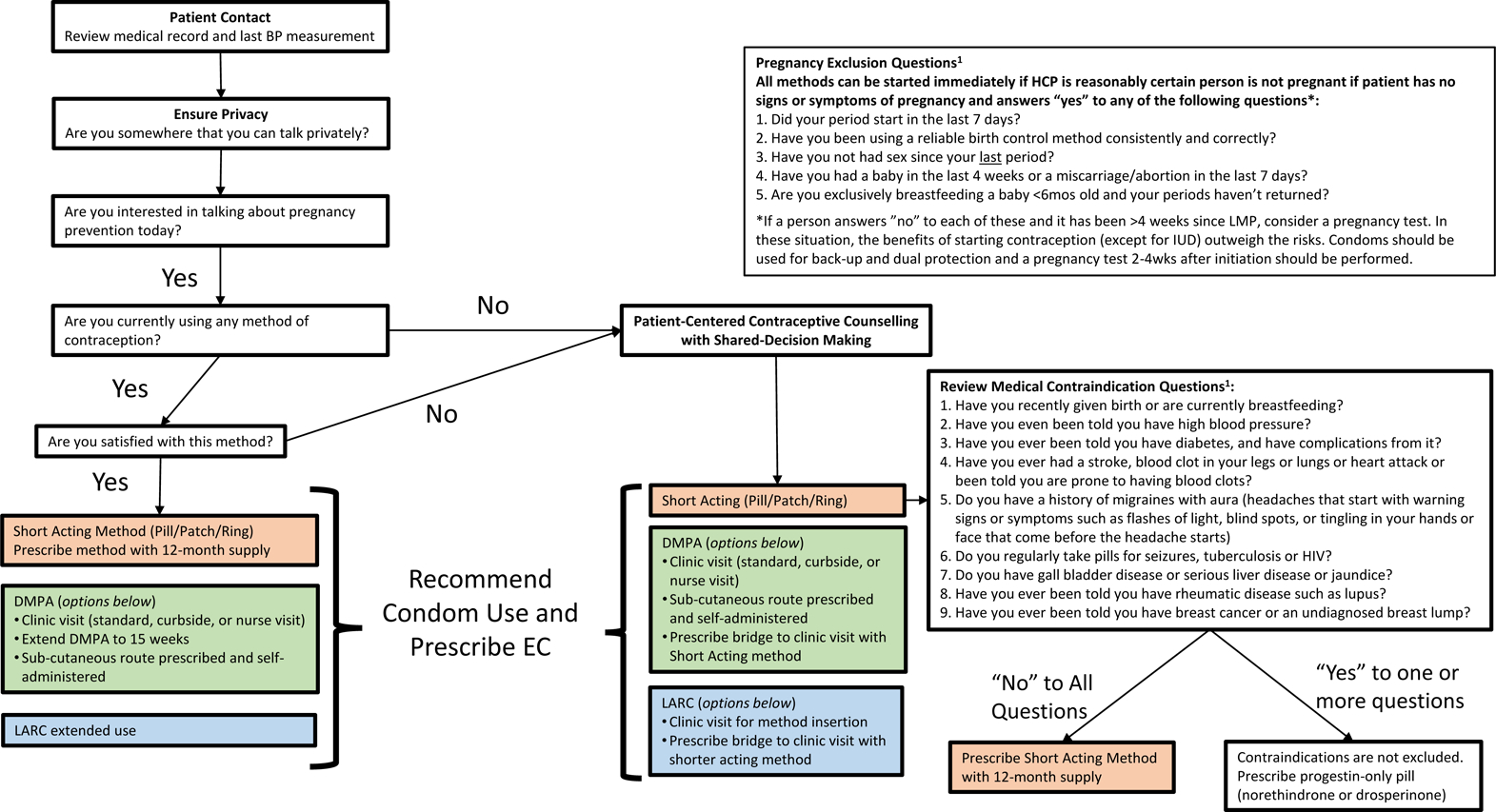
Abbreviations: AYA=Adolescents and Young Adults, HCP=Health Care Professional, US MEC= US Medical Eligibility Criteria for Contraceptive Use, BP=Blood Pressure, DMPA: Depot Medroxyprogesterone Acetate, LARC=Long-Acting Reversible Contraception, EC=Emergency Contraception
Safe provision of contraception relies largely on history and rarely requires a physical exam, pelvic or breast exams, sexually transmitted infection or cervical cancer screenings.1 Much of the information needed to provide contraceptives can be obtained from the patient history, including patient-reported or previously recorded blood pressure. The US Medical Eligibility Criteria for Contraceptive Use (US MEC) provides guidance on contraindications to contraceptives based on the patient history and is available in many forms, including a smartphone app.1
A challenge in conducting telehealth with adolescents is patient privacy: adolescents may not have a private space and HCPs may not be able to reliably assess whether an adolescent’s verbal communication is actually private. It is important to explore who is in the room and if the patient can speak freely. We recommend using clinical judgement to guide whether you can safely ask about sensitive content and how much you need to obtain. It is not necessary to obtain a complete sexual history to prescribe contraceptives. Consider the use of yes/no questions for sensitive topics, such as interest in contraception, sexual history, and pregnancy screening.
Fortunately, a healthy young person with no active or previous medical conditions who takes no medications or supplements can safely use any reversible contraceptive method. Using contraception is very safe and is safer than pregnancy. In addition to uncovering medical contraindications from patient history, HCPs can ask a series of questions to be reasonably certain a person is not pregnant. If there are no signs or symptoms of pregnancy and the patient meets additional criteria as identified in the US MEC (see Figure 1), contraception other than intrauterine contraception can be started immediately.1 Even in situations where a HCP is not reasonably certain a person isn’t pregnant, the benefits of starting contraception that day (except intrauterine devices) generally outweigh the risks, as none of the contraceptive methods are known to be teratogenic or abortifacient.1 HCPs can encourage patients to take a home pregnancy test, which are highly reliable, in 2–4 weeks in these situations.
Contraception counseling can be performed virtually using shared decision making to incorporate patients’ preferences and priorities, which may include efficacy. Clinicians may consider incorporating high quality resources, including videos and images, such as those available at bedsider.org, prior to, during (screen-sharing), or after their virtual patient encounter.2 Pills, transdermal patch, and vaginal rings can be refilled or initiated on the day of the telehealth encounter and a 12-month supply should be provided.3 After initiation, use of a back-up method for 7 days is recommended. Progestin-only contraceptive pills (norethindrone and drosperinone) are an option for those with a contraindication to estrogen.1
Depot medroxyprogesterone acetate (DMPA) is a progestin-only method available as a 150mg intramuscular (IM) or 104mg subcutaneous (SC) injection. Traditionally, DMPA is administered every 3 months in a clinical setting. However, in pandemic times, HCPs can consider extending the dosing interval to 15 weeks and exploring creative approaches to IM delivery (e.g. curbside).1 Alternately, the SC form may be prescribed along with alcohol swabs for self-administration at home. Medication teaching can be provided verbally, by video and/or via a patient information sheet, such as this one made by Reproductive Health Access Project https://www.reproductiveaccess.org/resource/depo-subq-user-guide/.4
For the patient who is interested in a long-acting reversible contraceptive method (LARC, i.e. an intrauterine device (IUD) or implant), a shorter acting contraceptive should be offered to provide contraception while awaiting in-person placement. People currently using a LARC nearing the end of their FDA-approved length of use can be reassured that these devices have contraceptive benefit far beyond the approved window.5
Counseling patients about the use of emergency contraception (EC) pills (i.e. levonorgestrel 1.5mg and ulipristal acetate 30mg) and offering an advanced prescription may be particularly beneficial now to reduce patient cost and access barriers. Ulipristal acetate is more effective than levonorgestrel, particularly in those who have a BMI >30 or who had sex more than 72 hours ago. Patients who take ulipristal acetate for EC should wait 5 days to start a hormonal contraceptive and use condoms until their next menses. It is also important to encourage consistent condom use for STI prevention, back-up for birth control and dual protection. For any contraceptive method prescribed, clinicians should review options for obtaining the product. This may include purchasing or filling a prescription at a pharmacy and online/phone ordering with home delivery. After a method is chosen, HCPs should inform patient to contact them if there are additional and unforeseen cost or insurance coverage barriers during the pandemic.
In addition to these approaches, 11 states and the District of Columbia allow for pharmacist-prescribed contraception. Further, some private companies provide telehealth options for home-delivery of contraceptives.6,7 However, we believe it is possible and imperative for HCPs to prioritize contraception access for young people throughout this pandemic and beyond as essential healthcare.
Footnotes
Conflicts of Interest: Drs. Wilkinson and Kottke have no conflicts of interest to disclose. Dr. Berlan is a consultant to Merck and Bayer and is a Nexplanon Clinical Trainer.
References
- 1.Curtis KM TN, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. 2016. [DOI] [PubMed]
- 2.www.bedsider.org. Accessed April 4, 2020.
- 3.Quick Start Algorithm-Patient requests a new birth control method. 2019; https://www.reproductiveaccess.org/wp-content/uploads/2014/12/QuickstartAlgorithm.pdf.
- 4.Depo-Provera Sub-Q User Guide. 2017; https://www.reproductiveaccess.org/resource/depo-subq-user-guide/. Accessed April 2, 2020.
- 5.McNicholas C, Swor E, Wan L, Peipert JF. Prolonged use of the etonogestrel implant and levonorgestrel intrauterine device: 2 years beyond Food and Drug Administration-approved duration. Am J Obstet Gynecol. 2017;216(6):586.e581–586.e586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams RL, Meredith AH, Ott MA. Expanding adolescent access to hormonal contraception: an update on over-the-counter, pharmacist prescribing, and web-based telehealth approaches. Curr Opin Obstet Gynecol. 2018;30(6):458–464. [DOI] [PubMed] [Google Scholar]
- 7.Who Prescribes the Pill Online? 2020; http://freethepill.org/online-pill-prescribing-resources/. Accessed April 4, 2020.


