Abstract
Background:
Emerging data indicate a resurgence of availability and harms of amphetamine-type stimulant (ATS) use. This study examined ATS overdose-involved emergency department (ED) visit trends and visit characteristics associated with ATS overdose.
Methods:
Data from the Healthcare Cost and Utilization Project’s (HCUP) 2010–2017 Nationwide Emergency Department Sample identified ATS overdose-involved visits. Predicted trend lines from 2010–2015 were fit using weighted logistic regression for any or only ATS-involved overdose using ICD-9-CM discharge diagnosis codes; percentage change from 2016 to 2017 used ICD-10-CM. Multivariable logistic regression examined characteristics in 2017 associated with only ATS-involved overdoses compared to drug overdoses not involving ATS.
Results:
Every year from 2010 to 2015 the odds of any ATS overdose-involved ED visits increased 11% (odds ratio [OR]: 1.11, 95% CI: 1.09, 1.14) and 7% for only ATS overdose-involved visits (OR: 1.07, 95% CI: 1.04, 1.10). From 2016 to 2017, any and only ATS overdose-involved visit rates increased 19.1% and 20.5%, respectively (P<.05). In 2017, ATS overdose-involved visits (N=42,428) accounted for 4.4% of all drug overdose visits (N=956,266). In adjusted regression models, characteristics more prevalent among patients with only ATS overdose included Western region; micropolitan and noncore urbanization levels; unintentional, undetermined, and assault intents; and cardiovascular effects.
Conclusions:
Our findings, coupled with the rising availability of ATS and related harms, underscore the expansion of current substance use and overdose prevention and response efforts to address stimulant use, particularly among groups at risk. Research to identify additional individual and community-level risk factors for increasing ATS overdose is warranted.
Keywords: methamphetamine, amphetamines, emergency department visits, overdose risk factors
1. Introduction
In recent years, there have been substantial increases in drug overdoses involving psychostimulants with abuse potential, including amphetamine-type stimulants (ATS) such as methamphetamine. From 2012 to 2018, ATS-involved overdose death rates increased, on average, 30% per year in the U.S. (Hedegaard et al., 2020), and from 2015 to 2016, emergency department (ED) visits and inpatient hospitalizations for ATS-involved nonfatal overdose increased approximately 11% (Hoots et al., 2018; Roehler et al., 2019). There is limited information on the specific stimulants driving this increase; however, methamphetamine appears to be a primary contributor, accounting for approximately 64% of amphetamine-involved ED visits in 2011 (Substance Abuse and Mental Health Services Administration [SAMSHA], 2013). Further, methamphetamine-involved deaths increased from 1,887 in 2011 to 9,356 in 2017, and, in 2017, methamphetamine was involved in 13.3% of overdose deaths compared to 2.3% for amphetamine (Hedegaard, Bastian, Trinidad, Spencer, & Warner, 2018, 2019).
Coincident with rising nonfatal and fatal ATS-involved overdoses, the availability and use of ATS have been increasing. In 2016, approximately 16 million U.S. adults (6.6%) reported past-year use of prescription stimulants (Compton, Han, Blank, Johnson, & Jones, 2018). By 2018, for persons 12 years and older more than 5 million Americans reported past-year misuse of prescription stimulants, and past-year methamphetamine use increased from 1.4 million in 2016 to 1.9 million in 2018 (SAMHSA, 2019). Additionally, reporting methamphetamine use at treatment admission for substance use increased more than 50% from 2008 to 2017 (Jones et al., 2020a). Finally, methamphetamine drug submissions – a marker of methamphetamine supply and availability – have also increased consistently between 2011 and the first half of 2019, with methamphetamine now being the most frequently reported drug among submissions in the U.S. (Drug Enforcement Administration [DEA], 2020a).
This study aims to further elucidate recent trends in ED visits for ATS-involved overdose and to identify visit characteristics associated with ATS-involved overdose in the U.S.
2. Methods
2.1. Study design
We conducted a secondary data analysis of ATS-involved overdose ED visits from a nationally representative sample of ED facilities in the U.S.
2.2. Data source
Data were obtained from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project’s (HCUP) Nationwide Emergency Department Sample (NEDS) from 2010 to 2017. The NEDS uses a stratified random sampling procedure from two files (i.e., the State Inpatient Databases and State Emergency Department Databases) to produce nationally representative estimates of ED visits in the U.S. (HCUP, 2020). From 2010 to 2017, a range of facilities (i.e., 945 to 984) and states (i.e., 28 to 37 states and Washington D.C.) participated in NEDS (HCUP, 2020). In 2017, 984 facilities in 37 states and Washington D.C. were included (N=33,506,645 total ED visits), representing a 20% sample of U.S. hospital-based EDs (HCUP, 2020).
2.3. Outcome
The primary outcome - ATS-involved overdose ED visits - was determined using principal and secondary diagnosis codes from the International Classification of Diseases, 9th Revision, Clinical Modification (i.e., ICD–9–CM, code 969.72) for data from 2010 to the third quarter of 2015 and diagnosis codes from the 10th Revision (i.e., ICD–10–CM, codes T43.621x–T43.624x) for data for the fourth quarter of 2015 to 2017. These diagnosis codes include poisonings by illicit amphetamines (e.g., methamphetamine, ecstasy) and prescription amphetamines, including dextroamphetamine and Adderall. ICD–10–CM codes included all encounters (i.e., initial, subsequent, sequelae) and only unintentional, intentional, assault, and undetermined intent codes; adverse effect and underdosing were excluded.
2.4. Data Analysis
First, we examined annual trends for 2010–2015 for any overdose involving ATS (see eTable 1 for a breakdown of other poisoning codes in this category) and overdoses involving only ATS (i.e., ED visit where there was a diagnosis code for ATS and no other drug poisoning codes). Age-adjusted rates were calculated for each year by applying age-specific rates to the 2000 U.S. Census standard population age distribution. Potential joins in the trend from 2010 to 2015 were identified using JoinPoint software (https://surveillance.cancer.gov/joinpoint/). Predicted trend lines were fit using weighted logistic regression in SAS-callable SUDAAN around any identified joins with year as the independent variable and any or only ATS overdose as the dependent variable. Sample weights were adjusted to reflect the age adjustment in the rates (Ingram et al., 2018). Because of the shift from ICD-9-CM to ICD-10-CM in the fourth quarter of 2015, we only examined the trend through 2015. To calculate an annual rate for 2015, we applied the visit counts and weights from third quarter of 2015 to fourth quarter of 2015. Percent change was also calculated between rates in 2016 and 2017 for ED visits with ICD-10-CM diagnosis codes.
Using 2017 data, we estimated weighted percentages and 95% CIs for any and only ATS-involved overdose ED visits by sex, age group, Census region, county urbanization level, overdose intent, admission to the hospital, and death. Central nervous system effects and cardiovascular effects were also examined because prior research has demonstrated that use of methamphetamine and other ATS is associated with both acute and chronic mental health and cardiovascular adverse events (Radfar & Rawson, 2014). We felt it was important to assess whether these types of events were found more commonly among ED visits for overdoses involving ATS compared to overdoses not involving these drugs as these findings would be informative from a clinical management perspective. See table footnotes for definitions.
Finally, we compared only ATS-involved overdose ED visits to overdose ED visits that did not involve ATS (i.e., poisoning codes for drugs other than ATS) by calculating weighted percentages and 95% CIs by the above covariables. Predicted marginals from bivariable logistic regression were used to generate prevalence ratios. Separate multivariable logistic regression models were developed to examine the relationship between each covariable and only ATS-involved overdose compared to overdoses not involving ATS, adjusted for potential confounders. Models were reduced with backwards elimination using a 10% change-in-estimate approach (Maldonado, 1993). All analyses accounted for the NEDS complex sample design and weights. Analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, NC) and SUDAAN version 11 (Research Triangle Institute, Research Triangle Park, NC) using predicted marginals from proc rlogist to calculate weighted prevalence ratios.
3. Results
3.1. Trend analysis
From 2010 to 2015, no joins were identified in JoinPoint, indicating a consistent linear trend; each year the odds of any and only ATS-involved overdose ED visits increased 11% (odds ratio [OR]: 1.11, 95% CI: 1.09, 1.14) and 7% (OR: 1.07, 95% CI: 1.04, 1.10), respectively.
The any ATS-involved overdose rate increased 19.1% from 2016 (11.4) to 2017 (13.6) (P<.05), and the only ATS-involved overdose rate increased 20.5% from 2016 (7.2) to 2017 (8.7) (P<.05). Figure 1 presents a graphical depiction of these trends.
Figure 1: Trendsa in amphetamine-type stimulant overdoseb emergency department visits, 2010–2017c.
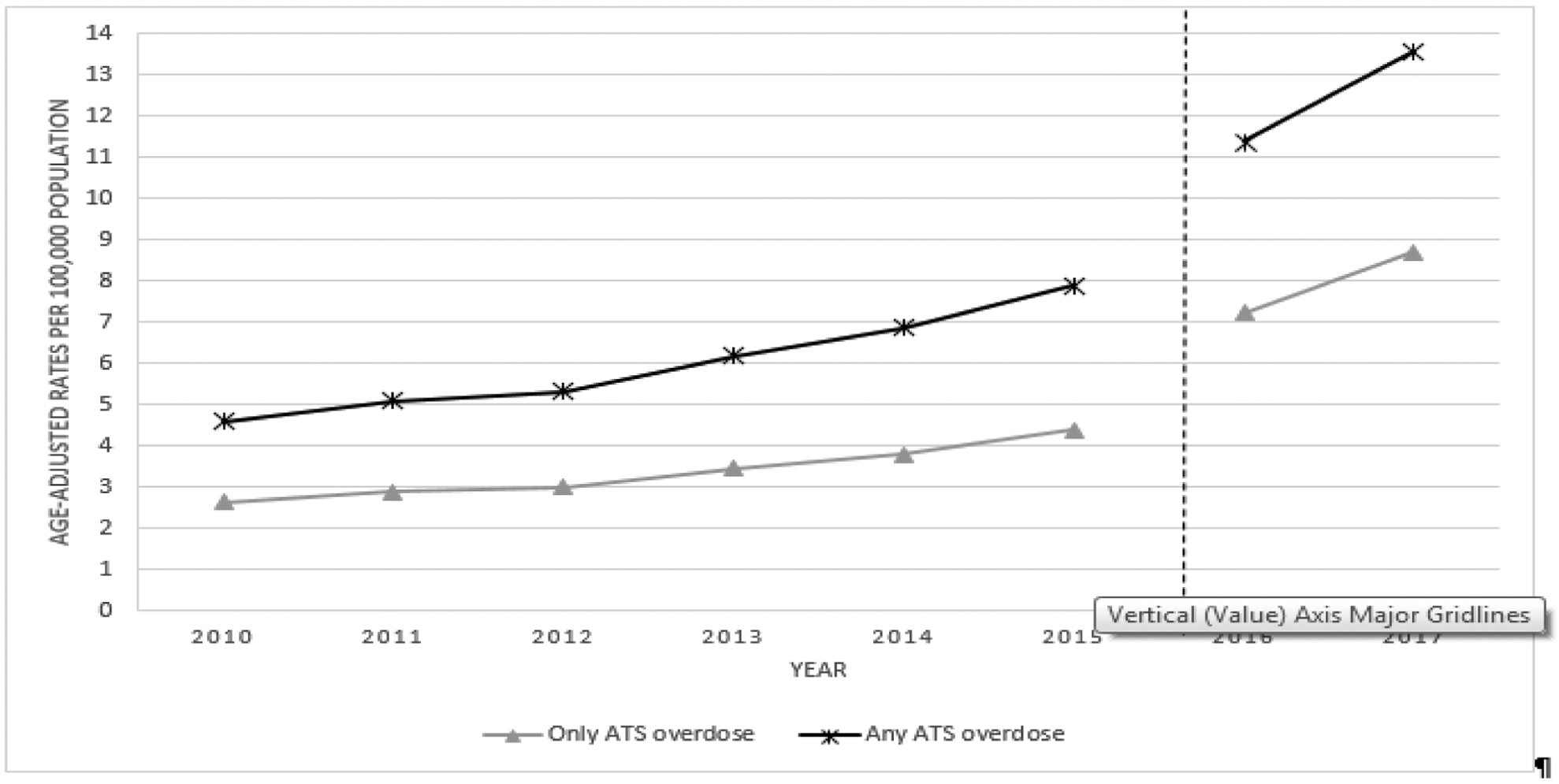
Source: Nationwide Emergency Department Sample
a Emergency department visit rates were calculated by applying age-specific emergency department visit rates to the 2000 U.S. standard population age distribution. All rates are per 100,000 population.
b International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes included 969.72; International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) included T43.621A, T43.621D, T43.621S, T43.622A, T43.622D, T43.622S, T43.623A, T43.623D, T43.623S, T43.624A, T43.624D, T43.624S.
c The vertical line between 2015 and 2016 on the graph of emergency department visit rates denotes the transition in the Nationwide Emergency Department Sample from using ICD-9-CM diagnosis codes to ICD-10-CM on October 1, 2015. ICD-10-CM coded injury data are not comparable to ICD-9-CM coded injury data.
3.2. Sample characteristics
In 2017, ATS-involved ED visits (N=42,428) accounted for 4.4% of all drug overdose ED visits (N=956,266). Of the 42,428 ATS-involved ED visits, 27,226 (64.2%) only included ATS. Table 1 provides a breakdown for all demographic and other characteristics. Persons visiting an ED for any ATS-involved overdose or only ATS-involved were mostly male (64.4% and 67.4%, respectively), aged 35–54 years (35.0% and 35.7%, respectively), from the West (38.2% and 42.6%, respectively), and from large central metropolitan areas (32.5% and 34.2%, respectively). A large majority of any ATS-involved and only ATS-involved overdoses were categorized as unintentional intent (74.8% and 79.6%, respectively), and a small percentage of patients died in the ED or were admitted to the hospital (1.6% and 1.2%, respectively). Approximately 36% (N=15,202) of any ATS-involved overdose ED visits were polydrug overdoses (i.e., presence of a poisoning code for another drug in addition to ATS).
Table 1:
Visit characteristics for emergency department visits estimating any and only amphetamine-type stimulantsa and comparing only amphetamine-type stimulants to all other drug overdosesb, 2017
| Any amphetamine-type stimulant overdose | Only amphetamine-type stimulant overdose | Drug overdose not including amphetamine-type stimulants | Unadjusted PRc (95%CI) | Adjusted PRc (95%CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Visit characteristic | n | (%) | 95% CI of % | n | (%) | 95% CI of % | n | (%) | 95% CI of % | ||
| All | 42,428 | 27,226 | 929,040 | ||||||||
| Sex | |||||||||||
| Male | 27,316 | (64.4) | (63.0–65.9) | 18,336 | (67.4) | (65.6–69.2) | 444,219 | (47.8) | (47.0–48.6) | 1.41 (1.37–1.45) | d |
| Female | 15,092 | (35.6) | (34.1–37.1) | 8,871 | (32.6) | (30.8–34.4) | 484,715 | (52.2) | (51.4–53.0) | 0.63 (0.59–0.66) | d |
| Age group | |||||||||||
| ≤ 24 | 9,880 | (23.3) | (21.4–25.4) | 6,534 | (24.0) | (21.7–26.3) | 279,025 | (30.0) | (28.9–31.2) | 0.80 (0.73–0.88) | d |
| 25–34 | 13,208 | (31.1) | (29.8–32.5) | 8,037 | (29.5) | (27.9–31.1) | 190,630 | (20.5) | (19.8–21.2) | 1.44 (1.36–1.53) | d |
| 35–54 | 14,859 | (35.0) | (33.7–36.4) | 9,715 | (35.7) | (34.0–37.4) | 255,267 | (27.5) | (26.8–28.1) | 1.30 (1.24–1.36) | d |
| ≥ 55 | 4,482 | (10.6) | (9.2–11.9) | 2,939 | (10.8) | (9.0–12.6) | 204,117 | (22.0) | (21.3–22.6) | 0.49 (0.42–0.58) | d |
| Census regione | |||||||||||
| Northeast | 2,499 | (5.9) | (4.8–7.0) | 1,467 | (5.4) | (4.3–6.4) | 161,810 | (17.4) | (15.0–19.8) | 0.31 (0.26–0.37) | 0.34 (0.29–0.40) |
| Midwest | 8,726 | (20.6) | (17.0–24.1) | 5,066 | (18.6) | (15.2–22.0) | 242,262 | (26.1) | (23.4–28.7) | 0.71 (0.61–0.83) | 0.74 (0.65–0.85) |
| South | 14,988 | (35.3) | (30.7–40.0) | 9,097 | (33.4) | (28.5–38.3) | 344,513 | (37.1) | (33.9–40.2) | 0.90 (0.79–1.03) | 0.94 (0.84–1.06) |
| West | 16,215 | (38.2) | (32.5–43.9) | 11,596 | (42.6) | (36.0–49.2) | 180,454 | (19.4) | (17.6–21.3) | 2.19 (1.89–2.54) | 2.02 (1.78–2.30) |
| County urbanization levelf | |||||||||||
| Large central metro | 13,143 | (32.5) | (27.6–37.5) | 8,821 | (34.2) | (28.5–39.9) | 272,442 | (29.6) | (26.5–32.7) | 1.15 (0.99–1.34) | 1.05 (0.92–1.20) |
| Large fringe metro | 6,240 | (15.4) | (12.8–18.1) | 3,736 | (14.5) | (11.7–17.3) | 193,880 | (21.1) | (18.3–23.8) | 0.69 (0.59–0.81) | 0.82 (0.71–0.93) |
| Medium metro | 9,423 | (23.3) | (19.1–27.5) | 5,828 | (22.6) | (18.2–27.0) | 220,258 | (24.0) | (20.7–27.2) | 0.94 (0.81–1.10) | 0.92 (0.80–1.06) |
| Small metro | 4,107 | (10.2) | (7.7–12.6) | 2,723 | (10.6) | (7.8–13.3) | 89,274 | (9.7) | (7.7–11.7) | 1.09 (0.89–1.33) | 1.06 (0.871.29) |
| Micropolitan (nonmetro) | 4,597 | (11.4) | (9.7–13.1) | 2,860 | (11.1) | (9.4–12.8) | 90,408 | (9.8) | (8.8–10.9) | 1.13 (0.98–1.30) | 1.16 (1.01–1.33) |
| Noncore (nonmetro) | 2,912 | (7.2) | (6.2–8.3) | 1,810 | (7.0) | (5.9–8.1) | 53,101 | (5.8) | (5.2–6.4) | 1.22 (1.05–1.42) | 1.28 (1.12–1.48) |
| Overdose intentg | |||||||||||
| Unintentional | 31,730 | (74.8) | (72.5–77.0) | 21,683 | (79.6) | (77.3–81.9) | 594,259 | (63.9) | (62.5–65.5) | 1.24 (1.20–1.29) | 1.20 (1.16–1.25) |
| Intentional self-harm | 7,540 | (17.8) | (16.0–19.5) | 3,340 | (12.3) | (10.8–13.8) | 295,761 | (31.8) | (30.4–33.3) | 0.39 (0.34–0.44) | 0.45 (0.40–0.50) |
| Assault | 152 | (0.4) | (0.2–0.5) | 119 | (0.4) | (0.3–0.6) | 2,018 | (0.2) | (0.19–0.24) | 2.02 (1.31–3.11) | 2.16 (1.40–3.34) |
| Undetermined | 3,005 | (7.1) | (5.9–8.3) | 2,084 | (7.7) | (6.3–9.0) | 37,003 | (4.0) | (3.6–4.3) | 1.92 (1.64–2.25) | 1.84 (1.58–2.16) |
| Admission to hospital | |||||||||||
| Yes | 23,328 | (55.0) | (41.0–49.1) | 13,306 | (48.9) | (43.8–53.9) | 335,867 | (36.2) | (35.0–37.3) | 1.35 (1.22–1.50) | d |
| No | 19,100 | (45.0) | (50.9–59.0) | 13,920 | (51.1) | (46.1–56.2) | 593,174 | (63.8) | (62.7–65.0) | 0.80 (0.73–0.88) | d |
| Diedh | |||||||||||
| Yes | 673 | (1.6) | (1.3–1.9) | 336 | (1.2) | (0.9–1.5) | 7,574 | (0.8) | (0.77–0.87) | 1.51 (1.16–1.96) | 0.91 (0.71–1.16) |
| No | 41,621 | (98.4) | (98.1–98.7) | 26,813 | (98.8) | (98.5–99.1) | 917,967 | (99.2) | (99.1–99.2) | 1.00 (0.99–1.00) | 1.00 (1.00–1.00) |
| Cardiovascular effectsi | |||||||||||
| Yes | 10,157 | (23.9) | (22.7–25.2) | 7,056 | (25.9) | (24.4–27.5) | 126,567 | (13.6) | (13.1–14.1) | 1.90 (1.79–2.03) | 1.69 (1.59–1.80) |
| No | 32,271 | (76.1) | (74.8–77.3) | 20,170 | (74.1) | (72.5–75.6) | 802,473 | (86.4) | (85.9–86.9) | 0.86 (0.84–0.88) | 0.89 (0.87–0.91) |
| Central nervous system (seizure) effectsj | |||||||||||
| Yes | 1,510 | (3.6) | (3.1–4.0) | 872 | (3.2) | (2.7–3.7) | 31,105 | (3.3) | (3.2–3.5) | 0.96 (0.82–1.11) | 0.80 (0.69–0.93) |
| No | 40,910 | (96.4) | (96.0–96.9) | 26,354 | (96.8) | (96.3–97.3) | 897,935 | (96.7) | (96.5–96.8) | 1.00 (1.00–1.01) | 1.01 (1.00–1.01) |
Source: Nationwide Emergency Department Sample
International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) included T43.621A, T43.621D, T43.621S, T43.622A, T43.622D, T43.622S, T43.623A, T43.623D, T43.623S, T43.624A, T43.624D, T43.624S.
International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) included T36-T50 diagnosis codes for all encounters (i.e., initial, subsequent, and sequelae) excluding adverse effects and underdosing and excluding amphetamine-type stimulant overdose codes (i.e., T43.621A, T43.621D, T43.621S, T43.622A, T43.622D, T43.622S, T43.623A, T43.623D, T43.623S, T43.624A, T43.624D, T43.624S).
Referent group for prevalence ratios is drug overdose not including amphetamine-type stimulants. Separate bivariable (Unadjusted PR) and multivariable (Adjusted PR) logistic regression models were developed to examine the relationship between each covariable (row) and only ATS-involved overdose compared to overdoses not involving ATS. Predicted marginals from logistic regression models were used to calculate prevalence ratios.
Only bivariable models for sex, age, and admission to the hospital are presented because no covariates remained in adjusted models after model reduction.
Adjusted for county urbanization level.
Determined based on NCHS 2013 Urban-Rural classification scheme (https://www.cdc.gov/nchs/data/series/sr_02/sr02_166.pdf); Adjusted for census region.
Intent is determined based on 5th or 6th character is the ICD–10–CM drug poisoning code; Adjusted for sex.
Adjusted for intent and admission to hospital.
International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) included I15.8, I15.9, I16, I20, I21, I24.8, I24.9, I46, I47, I48, I49, I60, I61, I62, I63, I71, I72, R00, R03.0; Adjusted for admission to hospital.
International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) included G40; Adjusted for age.
3.3. Multivariable logistic regression
In adjusted regression models (Table 1), characteristics more prevalent among patients with only ATS-involved overdose compared to overdoses not involving ATS included living in the Western region (aPR=2.02, 95% CI=1.78, 2.30); living in a micropolitan (nonmetro) or noncore (nonmetro) county (aPR=1.16, 95% CI=1.01, 1.33; aPR=1.28, 95% CI = 1.12, 1.48, respectively); being treated for an unintentional (aPR=1.20, 95% CI=1.16, 1.25), assault (aPR=2.16, 95% CI=1.40, 3.34) or undetermined intent poisoning (aPR=1.84, 95% CI=1.58, 2.16); and experiencing cardiovascular effects (aPR=1.69; 95% CI=1.59, 1.80). Characteristics less prevalent among patients with only ATS-involved overdose compared to overdoses not involving ATS included living in the Northeast (aPR=0.34, 95% CI=0.29, 0.40) or Midwest region (aPR=0.74, 95% CI=0.65, 0.85), living in a large fringe metro county (aPR=0.82, 95% CI=0.71, 0.93), being treated for an intentional self-harm poisoning (aPR=0.45, 95% CI=0.40, 0.50), and experiencing central nervous system effects (aPR=0.80; 95% CI=0.69, 0.93).
4. Discussion
Rising availability and use of ATS, including methamphetamine, have focused attention on the threat of a resurgent stimulant crisis in the U.S. Findings indicate that ATS-involved overdose ED visits have been increasing since 2010. This is consistent with recent increases in substance use treatment admissions involving methamphetamine (Jones et al., 2020a) and deaths involving psychostimulants with abuse potential during the same time period (Hedegaard et al., 2020; Hoots, et al., 2018; Kariisa et al., 2019). Taken together, these findings underscore the need to expand current substance use and overdose prevention, treatment, and response efforts to address rising methamphetamine and other ATS use.
Several factors may be contributing to the increase in ATS-involved overdoses. The first is an increase in supply and availability of stimulants. According to the DEA, methamphetamine is now readily available throughout the U.S, particularly in the West and Midwest, and supply is increasing in areas that historically have not been major markets for methamphetamine, such as in the Northeast (DEA, 2020b). Submissions for amphetamine and MDMA to the National Forensic Laboratory Information System also have increased in recent years in most U.S. regions (DEA, 2020a). Second, methamphetamine use has been increasing (Roehler et al., 2019), further supporting that more persons are using methamphetamine. Third, although the mixing of heroin or fentanyl with methamphetamine in the illicit drug supply remains minimal (DEA, 2020b), polysubstance use is increasing, particularly with illicit opioids. Methamphetamine use among persons using opioids has increased during the past several years because of the potential availability, cost, and “euphoric” feeling (Cicero et al., 2020; Ellis et al., 2018; Jones et al., 2020b), further complicating prevention efforts. Finally, a recent study indicated that some persons may be transitioning from illicit opioid use to methamphetamine use (Jones, 2019).
This study carries important policy and programmatic implications, including insights into at-risk populations and patient factors to prioritize for prevention, treatment, and response efforts. These include males, middle aged adults, persons living in the Western region, and persons in rural/nonmetro areas. Notably, findings are consistent with recent research identifying these populations as higher risk for past-year methamphetamine use (Jones et al., 2020c).
Prevention strategies include implementation of universal preventive interventions, such as Promoting School-Community-University Partnerships to Enhance Resilience (PROSPER), which has demonstrated long-term protective effects for preventing methamphetamine and other substance use (Spoth et al., 2017). Treatment for stimulant use disorders includes evidence-based non-pharmacological approaches, such as cognitive behavioral therapy or community-reinforcement approach, coupled with contingency management (De Cresenzo et al., 2018). Importantly, less than one-third of persons with methamphetamine use disorder receive substance use treatment (Jones et al., 2020c); thus, innovative strategies to link persons to care, including through the ED, and providing sustained follow-up and wrap-around services to strengthen treatment effectiveness are needed. Given increasing evidence of combined opioid and stimulant use and mixing of synthetic opioids into the illicit stimulant supply, comprehensive harm reduction strategies, including naloxone provision and overdose prevention training, should be expanded to persons using stimulants. Finally, future research should identify additional individual and community-level risk factors for rising stimulant use and overdose and be incorporated in prevention and response initiatives.
4.1. Limitations
The transition from ICD–9–CM to ICD–10-CM coding impacts accurately monitoring trends. Additionally, the poisoning by amphetamine discharge codes include both illicit and prescribed stimulants; thus, we are unable to parse out the extent to which these trends are being driven by illicit or prescribed stimulants. Analysis included all diagnoses codes, not just primary, which may overestimate overdose visits. Also, ED visits included are from unique overdose visits, not unique persons, making repeat ED visits by the same person possible. Finally, results may not represent current overdose trends due to the data time lag and the rapidly evolving drug market.
4.2. Conclusions
Rising availability of ATS and related harms coupled with increasing rates of ATS-involved overdoses presenting to the ED underscore the need to expand current substance use and overdose prevention and response efforts to incorporate stimulant use in the U.S. Efforts should be tailored to population groups particularly at-risk.
Supplementary Material
Highlights.
Amphetamine-type stimulant (ATS) overdose ED visits increased between 2010–2017.
Compared to non-ATS overdoses, ATS overdoses were more prevalent among males.
ATS overdoses were also more prevalent in the West and rural areas.
Actions to expand prevention and treatment of stimulant use disorder are needed.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this paper of those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of Interest: No conflicts declared.
References
- Cicero TJ, Ellis MS, Kasper ZA 2020. Polysubstance use: A broader understanding of substance use during the opioid crisis. Am J Public Health. 110(2), 244–250. doi: 10.2105/AJPH.2019.305412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Han B, Blanco C, Johnson K, Jones CM 2018. Prevalence and correlates of prescription stimulant use, misuse, use disorders, and motivations for misuse among adults in the United States. Am J Psychiatry. 175(8), 741–755. doi: 10.1176/appi.ajp.2018.17091048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Crescenzo F, Ciabattini M, D’Alo GL, De Giorgi R, Del Giovane C, Cassar C, et al. 2018. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: A systematic review and network meta-analysis. PLoS Med. 15(12), e1002715. doi: 10.1371/journal.pmed.1002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drug Enforcement Administration. 2019. National Forensic Laboratory Information System: NFLIS-drug midyear report 2018. Springfield, VA: US Department of Justice, Drug Enforcement Administration; Retrieved from https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/NFLISDrug2018MY.pdf. [Google Scholar]
- Drug Enforcement Administration. 2020a. National Forensic Laboratory Information System: NFLIS-drug midyear report 2019. Springfield, VA: US Department of Justice, Drug Enforcement Administration; Retrieved from https://www.nflis.deadiversion.usdoj.gov/DesktopModules/ReportDownloads/Reports/13408NFLISDrugMidYear2019.pdf [Google Scholar]
- Drug Enforcement Administration. 2020b. 2019 National drug threat assessment Annual drug report; 2019. Springfield, Virginia: US Department of Justice, Drug Enforcement Administration; 2019. https://www.dea.gov/sites/default/files/2020-01/2019-NDTA-final-01-14-2020_Low_Web-DIR-007-20_2019.pdf [Google Scholar]
- Ellis MS, Kasper ZA, Cicero TJ 2018. Twin epidemics: The surging rise of methamphetamine use in chronic opioid users. Drug Alcohol Depend. 193, 14–20. doi: 10.1016/j.drugalcdep.2018.08.029 [DOI] [PubMed] [Google Scholar]
- Healthcare Cost and Utilization Project. 2020. Introduction to the HCUP Nationwide Emergency Department Sample (NEDS) 2017. Retrieved from https://www.hcup-us.ahrq.gov/db/nation/neds/NEDS2017Introduction.pdf. [Google Scholar]
- Hedegaard H, Bastian BA, Trinidad JP, Spencer M, Warner M 2018. Drugs most frequently involved in drug overdose deaths: United States, 2011–2016 National Vital Statistics Reports; vol 67 no 9. Hyattsville, MD: National Center for Health Statistics; Retrieved from https://stacks.cdc.gov/view/cdc/61381. [PubMed] [Google Scholar]
- Hedegaard H, Bastian BA, Trinidad JP, Spencer MR, Warner M 2019. Regional differences in the drugs most frequently involved in drug overdose deaths: United States, 2017 National Vital Statistics Reports; vol 68 no 12. Hyattsville, MD: National Center for Health Statistics; Retrieved from https://stacks.cdc.gov/view/cdc/82186. [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Warner M 2020. Drug overdose deaths in the United States, 1999–2018 NCHS Data Brief, no 356. Hyattsville, MD: National Center for Health Statistics; Retrieved from https://www.cdc.gov/nchs/data/databriefs/db356-h.pdf. [Google Scholar]
- Hoots BE, Xu L, Kariisa M, Wilson NO, Rudd RA, Scholl L, et al. 2018. Annual surveillance report of drug-related risks and outcomes — United States, 2018 Surveillance Special Report. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Retrieved from https://www.cdc.gov/drugoverdose/pdf/pubs/2018-cdc-drug-surveillancereport.pdf. [Google Scholar]
- Ingram DD, Malec DJ, Makuc DM, Kruszon-Moran D, Gindi RM, Albert M, et al. 2018. National Center for Health Statistics Guidelines for Analysis of Trends. National Center for Health Statistics. Vital Health Stat 2(179), 1–71. Retrieved from https://www.cdc.gov/nchs/data/series/sr_02/sr02_179.pdf [PubMed] [Google Scholar]
- Jones CM 2019. Syringe services programs: An examination of legal, policy, and funding barriers in the midst of the evolving opioid crisis in the U.S. Int J Drug Policy. 70, 22–32. doi: 10.1016/j.drugpo.2019.04.006. [DOI] [PubMed] [Google Scholar]
- Jones CM, Olsen EO, O’Donnell J, Mustaquim D 2020a. Resurgent methamphetamine use at treatment admission in the United States, 2008–2017. Am J Public Health. 110(4), 509–516. doi: 10.2105/AJPH.2019.305527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Underwood N, Compton WM 2020b. Increases in methamphetamine use among heroin treatment admissions in the United States, 2008–2017. Addiction. 115(2), 347–353. doi: 10.1111/add.14812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Compton WM, Mustaquim D 2020c. Patterns and Characteristics of Methamphetamine Use Among Adults - United States, 2015–2018. MMWR Morb Mortal Wkly Rep. 69(12), 317–323. doi: 10.15585/mmwr.mm6912a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kariisa M, Scholl L, Wilson N, Seth P, Hoots B 2019. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. MMWR Morb Mortal Wkly Rep. 68(17), 388–395. doi: 10.15585/mmwr.mm6817a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado G, Greenland S 1993. Simulation study of confounder-selection strategies. Am J Epidemiol. 138, 923–936. doi: 10.1093/oxfordjournals.aje.a116813 [DOI] [PubMed] [Google Scholar]
- Radfar SR, Rawson RA 2014. Current research on methamphetamine: Epidemiology, medical and psychiatric effects, treatment, and harm reduction efforts. Addict Health. 6(3–4), 146–154. [PMC free article] [PubMed] [Google Scholar]
- Roehler DR, Hoots BE, Olsen EO, Kariisa M, Wilson NO, Rudd RA, et al. 2019. Annual surveillance report of drug-related risks and outcomes — United States, 2019 Surveillance Special Report. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Retrieved from https://www.cdc.gov/drugoverdose/pdf/pubs/2019-cdc-drug-surveillance-report.pdf. [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg MT, Feinberg ME, Trudeau L 2018. PROSPER delivery of universal preventive interventions with young adolescents: Long-term effects on emerging adult substance misuse and associated risk behaviors. Psychol Med. 47(13), 2246–2259. doi: 10.1017/S0033291717000691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMSHA). 2013. Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits HHS Publication No. (SMA) 13–4760, DAWN Series D-39 Rockville, MD: Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMSHA). 2019. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19–5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from https://www.samhsa.gov/data/. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


