Abstract
Although spinal arachnoid cysts are relatively common findings observed incidentally in adults, they are much rarely reported in children. They are usually asymptomatic and are mainly located in the middle and lower thoracic regions. However, in rare circumstances, these cysts can cause mass effects that lead to neurologic symptoms. We report the rare case of a spinal extradural arachnoid cyst in a 12-year-old boy who showed signs and symptoms of cauda equina syndrome. Magnetic resonance imaging of the lumbar spine revealed a huge extradural arachnoid cyst extending from L2 to L5. Emergent laminectomy and repair of dural defect was performed after total resection of the extradural arachnoid cyst. There were no postoperative complications. Total recovery was achieved 6 months after surgery. Here, we report this rare case with a review of the literature.
Keywords: Epidural, Lumbar spine, Arachnoid cysts
INTRODUCTION
Spinal arachnoid cysts are relatively rare expanding spinal diseases. When present, these are commonly located in the middle and thoracic spine and can displace the spinal cord anteriorly.7) They are believed to arise from small congenital defects in the dura mater. These cysts contain cerebrospinal fluid (CSF) and communicate with the spinal canal.12,13) They may also develop after to trauma, infection, inflammation, or lumbar puncture or postsurgical causes.4)
The clinical course of asymptomatic individuals with small cysts should be closely monitored. Surgical treatment is indicated in patients with significant neurologic findings such as cauda equina syndrome. Complete disconnection of the spinal communication is necessary for complete treatment.9)
We report this rare case of a 12-year-old boy with cauda equina syndrome caused by a huge extradural arachnoid cyst along with a review of the literature.
CASE REPORT
A 12-year old boy presented with the chief complaint of a 10-month history of progressive difficulty in voiding associated with gait ataxia and motor weakness of both lower extremities. He also had progressive difficulty in ambulating and an unusual pain sensation in both lower extremities. Furthermore, the patient had frequently experienced stumbling and falls. He had no history of any significant trauma, family history of spinal disease, or past history of lumbar puncture prior to the onset of symptoms. Physical examination revealed a weight of 80 kg, height of 168 cm, and body mass index of 28.3 kg/m2, indicative of morbid obesity for this boy.
The neurologic examination revealed bilateral weakness of the lower extremities, especially upon knee extension with a Medical Research Council (MRC) grade of 2/5. The patient did not have significant sensory deficits in the lower extremities. His perineal sensation and anal tone were normal.
Emergent magnetic resonance imaging (MRI) of the lumbar spine showed a large CSF-filled, cystic mass without contrast enhancement located at the level of L2 to L5 causing severe thecal sac compression. The imaging findings indicated an extradural arachnoid cyst (FIGURE 1). The thecal sac was severely flattened and displaced anteriorly.
FIGURE 1. Magnetic resonance images of the patient. Sagittal T2 and T1 weighted images show the cystic lesion from L2 to L5 (A & B). Axial T2 weighted images reveal a fluid-filled cyst situated dorsal to the thecal sac extending to foramen (C & D).
The patient underwent an emergent laminectomy of L2–L4 and removal of cyst with meticulous suture of the dural defect.
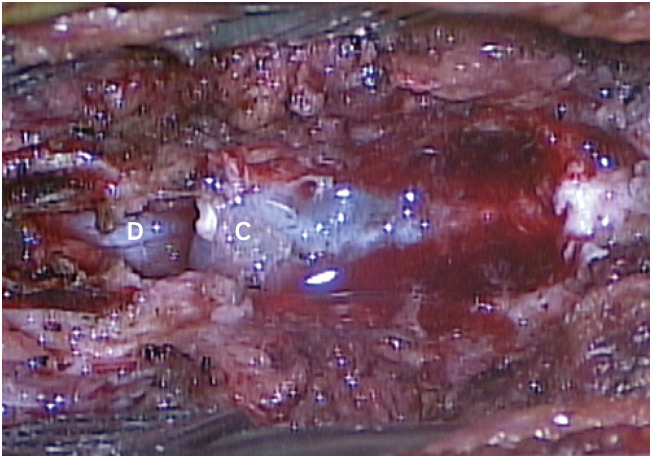
After laminectomy, removal of the yellow ligament permitted the visualization of a huge cyst in the epidural space (FIGURE 2). The cystic wall was thin and blue-colored with slight adhesions to the dura mater. During the careful dissection of the cystic membrane, a communicating tract and approximately 3 cm of dural defect with floating nerve rootlets were visualized. CSF leakage was also observed. Although the cyst was extended to the neural foramen, it was possible to remove the cystic membrane en bloc after fenestration of cyst. Microsurgical repair of the dural defect was performed, followed by the agglutination of a collagen fleece (Tachocomb®) and application of fibrin glue (Greenplast®) (FIGURE 3). Postoperatively, the patient had no neurologic aggravation and his symptoms improved. A biopsy of the cyst wall membrane revealed a fibrocollagenous tissue consistent with an arachnoid cyst.
FIGURE 2. Intraoperative finding of the patient. During the operation, normal dura can be seen in the L1 region. A CSF-filled extradural arachnoid cyst is observed.
CSF: cerebrospinal fluid, C: cyst, D: dura mater.
FIGURE 3. Intraoperative findings of the patient after cyst removal. A communicating tract and approximately 3 cm of dural defects with herniated nerve rootlets are observed (A). Microsurgical closure of the dural defect (communicating tract) is performed (B).
Six months after the surgery, the strength of the his lower extremities had near-normal recovery and his voiding difficulty had markedly improved.
DISCUSSION
Spinal meningeal cysts are categorized in 3 subgroups: type 1, extradural meningeal cyst that contains no neural tissue-extradural arachnoid cyst (type Ia) and sacral meningocele (type Ib); type 2, extradural meningeal cyst that contains neural tissue; and type 3, intradural meningeal cyst.10) Among them, extradural spinal arachnoid cysts are relatively uncommon lesions in adults.9) Moreover, extradural spinal arachnoid cysts are very uncommon causes of cauda equina syndrome in children. Some authors have reported that about 80% of spinal arachnoid cysts occur in the thoracic spine. It is inferred to be the most common in thoracic spine because of the narrow diameter and longest segment.3) These anatomic features possibly lead to rapid detection discovery of symptoms caused by the mass effect on the spinal cord.1) Although they are most commonly found in the thoracic spine, these cysts have also been reported to occur in the lumbar spine.11) However, the exact etiology and pathogenesis of spinal arachnoid cysts have not been well established.
Many spinal arachnoid cysts are idiopathic or congenital, whereas others may develop secondary to trauma, infection, or iatrogenic (lumbar puncture or surgery) causes.6,10,15) Idiopathic or congenital arachnoid cysts are characterized by distinctive features on imaging studies and they may present with neurological signs and symptoms.
The patient in this study denied any history of trivial injury, surgery, or lumbar puncture. There was no features of arachnoiditis on MRIs. Due to his young age and long history of prolonged gait disturbance, this event is mostly considered to be congenital. The hypothesis to explain the expansion of cysts are mainly two theories. First, osmotic gradient and fluid production by the cells forming its wall(non-communicating) and one-way valve like mechanism between the cyst and subarachonoid space.3,8,12)
An increase in the intraspinal pressure could stimulate the movement of CSF into the cyst.3,8) This ball valve mechanism might have been observed intraoperatively. Bony erosion of the spinal canal may suggest the presence of a valve like mechanism that is responsible for producing forces of CSF pressure within the cyst which are greater than normal hydrostatic forces.10)
MRI is a valuable diagnostic tool in determining the existence of spinal arachnoid cysts. Computed tomography (CT) myelography is also used to reveal communication between the cyst and the subarachnoid space. However, in our case, CT myelography was not performed due to the huge size of the cyst and its invasiveness.
Most asymptomatic and incidentally found spinal arachnoid cysts can be managed conservatively. On the contrary, symptomatic spinal arachnoid cysts require surgical intervention. For symptomatic spinal extradural cysts, total resection of the cyst including microsurgical suture of the dural connection to the cyst is an acceptable surgical strategy. For unmanageable refractory cases, placement of a cystoperitoneal shunt may be considered.5,14)
During the operation, we observed that the rootlets were floating through the communicating tract, microsurgical closure of the dural connection to the cyst was performed.2)
CONCLUSION
Although spinal arachnoid cysts are usually asymptomatic, in rare cases, these may cause severe mass effects and neurologic deficits that require emergent surgical intervention even in children. Early diagnosis should be emphasized. Whenever possible, total resection of the cyst and complete suture of the dural defect is essential to avoid refilling of the lesion.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Bond AE, Zada G, Bowen I, McComb JG, Krieger MD. Spinal arachnoid cysts in the pediatric population: report of 31 cases and a review of the literature. J Neurosurg Pediatr. 2012;9:432–441. doi: 10.3171/2012.1.PEDS11391. [DOI] [PubMed] [Google Scholar]
- 2.Carrillo R, Carrillo R. Lumbar cerebrospinal fluid drainage for symptomatic sacral nerve root cysts: an adjuvant diagnostic procedure and/or alternative treatment? Technical case report. Neurosurgery. 1998;42:952–953. doi: 10.1097/00006123-199804000-00162. [DOI] [PubMed] [Google Scholar]
- 3.Eroglu U, Bozkurt M, Kahilogullari G, Dogan I, Ozgural O, Shah KJ, et al. Surgical management of spinal arachnoid cysts in adults. World Neurosurg. 2019;122:e1146–e1152. doi: 10.1016/j.wneu.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Garg K, Borkar SA, Kale SS, Sharma BS. Spinal arachnoid cysts - our experience and review of literature. Br J Neurosurg. 2017;31:172–178. doi: 10.1080/02688697.2016.1229747. [DOI] [PubMed] [Google Scholar]
- 5.James HE, Postlethwait R. Spinal peritoneal shunts for conditions other than hydrocephalus and pseudotumor cerebri: a clinical report. Pediatr Neurosurg. 2007;43:456–460. doi: 10.1159/000108787. [DOI] [PubMed] [Google Scholar]
- 6.Kong WK, Cho KT, Hong SK. Spinal extradural arachnoid cyst: a case report. Korean J Spine. 2013;10:32–34. doi: 10.14245/kjs.2013.10.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu JK, Cole CD, Sherr GT, Kestle JR, Walker ML. Noncommunicating spinal extradural arachnoid cyst causing spinal cord compression in a child. J Neurosurg. 2005;103:266–269. doi: 10.3171/ped.2005.103.3.0266. [DOI] [PubMed] [Google Scholar]
- 8.McCrum C, Williams B. Spinal extradural arachnoid pouches. Report of two cases. J Neurosurg. 1982;57:849–852. doi: 10.3171/jns.1982.57.6.0849. [DOI] [PubMed] [Google Scholar]
- 9.Myles LM, Gupta N, Armstrong D, Rutka JT. Multiple extradural arachnoid cysts as a cause of spinal cord compression in a child. Case report. J Neurosurg. 1999;91:116–120. doi: 10.3171/spi.1999.91.1.0116. [DOI] [PubMed] [Google Scholar]
- 10.Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI, et al. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988;68:366–377. doi: 10.3171/jns.1988.68.3.0366. [DOI] [PubMed] [Google Scholar]
- 11.Sato K, Nagata K, Sugita Y. Spinal extradural meningeal cyst: correct radiological and histopathological diagnosis. Neurosurg Focus. 2002;13:ecp1. doi: 10.3171/foc.2002.13.4.8. [DOI] [PubMed] [Google Scholar]
- 12.Suryaningtyas W, Arifin M. Multiple spinal extradural arachnoid cysts occurring in a child. Case report. J Neurosurg. 2007;106:158–161. doi: 10.3171/ped.2007.106.2.158. [DOI] [PubMed] [Google Scholar]
- 13.Takagaki T, Nomura T, Toh E, Watanabe M, Mochida J. Multiple extradural arachnoid cysts at the spinal cord and cauda equina levels in the young. Spinal Cord. 2006;44:59–62. doi: 10.1038/sj.sc.3101799. [DOI] [PubMed] [Google Scholar]
- 14.Tarlov IM. Spinal perineurial and meningeal cysts. J Neurol Neurosurg Psychiatry. 1970;33:833–843. doi: 10.1136/jnnp.33.6.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woo JB, Son DW, Kang KT, Lee JS, Song GS, Sung SK, et al. Spinal extradural arachnoid cyst. Korean J Neurotrauma. 2016;12:185–190. doi: 10.13004/kjnt.2016.12.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]