Abstract
Objective
We designed a method for inserting C1 pedicle screws using the direct visualization technique of the pedicle and serial dilatation technique to reduce complications and malposition of screw, and assessed the accuracy of this method.
Methods
Free-hand C1 pedicle screw insertion using the direct visualization technique of the pedicle and serial dilatation technique was performed on 5 consecutive patients with C1–2 instability at a single institute from March to December 2018. The method involved protecting the vertebral artery (VA) and C1 root using the Penfield No. 1, securing the entry point of the posterior arch screw and the pedicle was visible directly in Trendelenburg position. The hole at the entry point of the C1 posterior arch was serially dilated using a 2.5×3.0 mm drill bit, and the C1 pedicle screw was inserted with the free hand technique. We measured postoperative radiological parameters and recorded intraoperative complications, postoperative neurological deficits and the occurrence of occipital neuralgia. Postoperative computed tomography (CT) was performed to check screw malposition or construction failure.
Results
Of the 10 C1 pedicle screws on postoperative CT, 20% of screws (grade A) were in the ideal position while 80% of screws (grade B) occupied a safe position. Overall, 100% of screws were safe (grade A or B). There were no iatrogenic neurological deficits, VA injury.
Conclusion
Freehand placement of the C1 pedicle screw through the direct visualization technique of the pedicle and serial dilatation technique is safe and effective without intraoperative fluoroscopy guidance.
Keywords: Cervical atlas, Atlanto-Axial joint, Pedicle screws
INTRODUCTION
Posterior fixation of the cervical spine is commonly used to stabilize the atlantoaxial complex. Atlantoaxial problems can be caused by trauma, degenerative disorder, and malignancy.1,2,3,4,5) C1 lateral mass screw fixation is generally performed for C1–2 stabilization. The technique of insertion of the C1 lateral mass screw by Hams can damage structures anterior to C1, such as the hypoglossal nerve and internal carotid artery, because the screw must be bi-cortically inserted.7,9) The C1 pedicle screw fixation technique was introduced by Tan et al.25) in 2003 as an alternative to the C1 lateral mass screw.14) This method involves placing the screw into the lateral mass via the posterior arch, without invading the anterior cortex.16,23,25) In addition, in a biomechanical comparison study of the C1 pedicle and lateral mass screws, the C1 pedicle screw showed greater stiffness.2,17,27) Although the technique is frequently used for C1–2 instability, it requires fluoroscopic guidance, which is time-consuming and has the risks of accumulative radiation.8,11,12,13,18,20,21) It is occasionally difficult to interpret biplane X-ray scans acquired after C1–2 pedicle screw insertion. Therefore, we report a series of 5 patients who underwent freehand insertion of the C1 pedicle screw with the direct visualization technique of the pedicle and serial dilatation technique. The purpose of this study was to validate the safety and accuracy of freehand screw insertion of C1 pedicle screws.
MATERIALS AND METHODS
Patient population
This was a retrospective study of 5 consecutive patients who underwent free hand placement of the C1 pedicle screw with the direct visualization technique of the pedicle to treat C1–2 instability at a single institute from March to December 2018. All patients were treated by a single neurosurgeon specialized in spine surgery. The study included patients diagnosed with C1–2 instability because of degenerative, or congenital abnormalities. Patients who had an instability caused by an infection or rheumatoid arthritis or required occipital fixation were excluded from this study. The C1 vertebra with ponticulus posticus was not considered for pedicle screw use. The C2 vertebra with high-riding vertebral artery (VA) was also excluded for laminar or pars screw use. C1–2 instability can be determined using the atlantodental interval (ADI), which is the radiographic measurement of atlantoaxial joint articulation. In this article, we defined atlantoaxial dislocation as ADI greater than 3 mm in adults over the age of 18 years.
Surgical technique
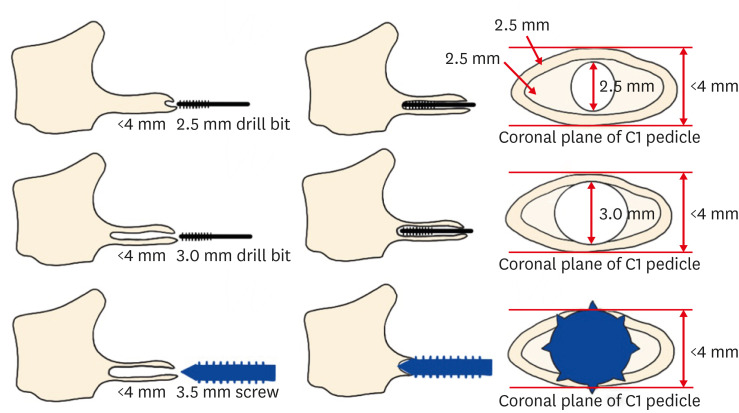
The patient was placed in the prone position. The craniocervical junction was exposed in the usual fashion. Dissection was performed approximately 2 cm lateral to the midline using bipolar cautery. The VA and C1 roots were exposed. Bleeding from the epidural venous plexus when exposed to the C1 lateral mass was controlled using compression with gelfoam-coagulation. Since only the upper part of the lateral mass was exposed, the bleeding was mild. Medial and lateral margins of the C1 lateral mass were identified with palpation using a Penfield No. 4 dissector. The VA and C1 roots were exposed from the C1 posterior arch and dissected away cranially using the root retractor and suction tip (FIGURE 1). The C1 pedicle was then visualized directly (FIGURE 2). The entry point of the C1 pedicle screw was the midpoint between the lateral and medial margins of the C1 pedicle in the posterior arch (FIGURE 3). The pilot hole was estimated by directly visualizing the course of the C1 pedicle as follows. Protecting the VA and C1 root, a high-speed drill with a 1.8-mm match head bur was used to make a hole at the entry point of the C1 posterior arch, which was expanded deep and wide with a 2.5-mm-diameter drill bit and further widened with 3.0-mm-diameter drill bit at a depth of 26–30 mm, as measured on preoperative computed tomography (CT). The screw length was finally determined during surgery by measuring the depth of the ball tip probe after tapping. Subsequently, a 28–34-mm-long screw of 3.5-mm diameter was inserted (FIGURE 4). Identical to the C1 pedicel screw, freehand insertion of the C2 pedicle screw was performed (FIGURE 5).
FIGURE 1. Exposure of the vertebral artery and C1 roots from the C1 posterior arch.
FIGURE 2. Direct visualization of the course in the C1 pedicle.
FIGURE 3. Entry point of the C1 pedicle screw.
FIGURE 4. Serial dilatation technique.
FIGURE 5. Entry point of the C2 pedicle screw.
This method of the serial dilatation technique allowed the insertion of the pedicle screw into the C1 pedicle with a diameter of less than 4 mm. If the pedicle was large enough, the pilot hole was tapped with a 3.0-mm tap without widening the hole using 2.5- and 3.0-mm-diameter drill bits, and subsequently, a 28–34-mm long screw with a diameter of 4.0 mm was inserted. This method of the serial dilatation technique allowed the trajectory to be gradually and safely expanded through the cancellous channel of the pedicle without damaging the cortical bone on the C1 pedicle with a diameter of less than 4 mm. The Vertex Reconstruction System (Medtronic Sofamor-Danek, Memphis, TN, USA) was used in all 5 patients. After inserting the screws and atlantoaxial facet joint fusion (FIGURE 6), 3.0-mm rods were applied and fastened using cap nuts.
FIGURE 6. Atlantoaxial facet joint fusion.
Radiographic and clinical evaluation
In all patients, preoperative CT and magnetic resonance imaging were performed to determine the ideal screw lengths and diameters of the C1 and, C2 pedicle screws. The patients also underwent CT angiography for evaluation of possible occult VA injury. Thin-cut CT was performed for the evaluation of screw malposition 1–3 days after surgery. The accuracies of the screws were rated as grades A, B, C, D, and E for perfectly insertion to the pedicle, 0–2 mm, 2–4 mm, 4–6 mm, and more than 6 mm of cortical breach, respectively. Grade A and B screws were considered well positioned.3) The 5 patients were examined clinically after 1 postoperative month. The electronic medical record review included patient demographics, diagnosis, and estimated blood loss as identified by anesthesiologists. Intraoperative injury of the nerve structure or VA and postoperative symptom of occipital neuralgia were also included. The Nurick grade was used to assess neurological outcomes before and after surgery.
RESULTS
Demographic data
A total of 10–C1 pedicle screws were implanted in 5 consecutive patients: one man and four women, aged 49–76 years (mean, 59 years) at the time of surgery. The mean follow-up period was 2.2 months (range, 1–3 months). Three patients had myelopathy due to os odontoideum while 2 had C1–2 subluxation. The preoperative Nurick grade was 1, 2, and 5 in one, three, and one patient, respectively. The mean operation time was 212.2 minutes (range, 180–249 minutes), and the mean intraoperative blood loss volume was 120 mL (range, 100–200 mL) (TABLE 1).
TABLE 1. Demographic characteristics of 5 patients who underwent free hand placement of a C1 pedicle screw with direct visualization of the pedicle and serial dilatation technique.
| Case | Sex | Age (years) | Diagnosis | Operative level | Operative time (min) | Blood loss (mL) |
|---|---|---|---|---|---|---|
| 1 | F | 49 | Os odontoideum | C1–2 | 249 | 100 |
| 2 | M | 54 | C1–2 subluxation | C1–2 | 200 | 100 |
| 3 | F | 54 | Os odontoideum | C1–2 | 180 | 200 |
| 4 | F | 76 | C1–2 subluxation | C1–2 | 241 | 100 |
| 5 | F | 62 | Os odontoideum | C1–2 | 191 | 100 |
F: female, M: male.
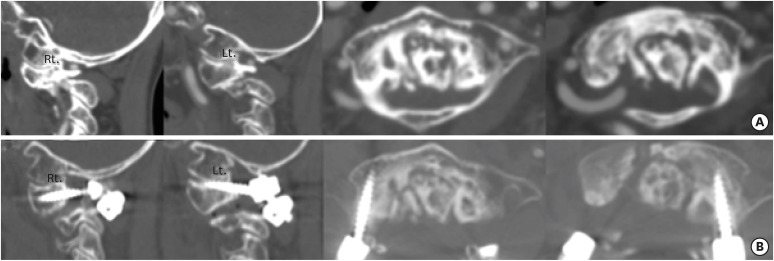
Radiological and clinical outcomes
On preoperative CT, the right and left mean diameters of the C1 posterior arch at the VA groove were 3.1 mm (range, 2.5–4.1 mm) and 3.0 mm (range, 2.7–3.9 mm), respectively. All screws inserted using a serial dilatation in the pedicle with a diameter of less than 4 mm were acceptable on postoperative CT (FIGURE 7). Of the 10 C1 pedicle screws imaged with postoperative CT, 20% of screws were grade A while 80% were grade B. Overall, 100% of screws were rated as safe (grade A or B). There were no known neurological or VA injuries. The 5 patients were free of neck pain after surgery, and all patients with preoperative myelopathy improved by more than one Nurick grade at the postoperative 1-month status (TABLE 2). After C1 pedicle screw insertion, none of the patients had iatrogenic neurological deficits, wound infections, VA injuries, cerebrospinal fluid leakage, or occipital neuralgia. There was no radiographic evidence of construct failure, and all screws were in excellent sagittal alignment.
FIGURE 7. Sagittal and axial CT images. (A) Preoperative CT image, (B) Postoperative CT image.
CT: computed tomography, Rt.: right, Lt.: left.
TABLE 2. Radiologic and clinical outcomes of 5 patients who underwent free hand placement of a C1 pedicle screw with direct visualization of the pedicle and serial dilatation technique.
| Case | Diameter of the C1 posterior arch | C1 pedicle wall violation grade | Nurick grade | Occipital neuralgia | ||||
|---|---|---|---|---|---|---|---|---|
| Rt. | Lt. | Rt. | Lt. | Pre-op | Post-op (1 month) | Rt. | Lt. | |
| 1 | 3.1 | 3.0 | B | B | 1 | 0 | x | x |
| 2 | 2.9 | 2.7 | B | B | 2 | 1 | x | x |
| 3 | 3.0 | 2.7 | B | B | 2 | 1 | x | x |
| 4 | 2.5 | 2.7 | B | B | 5 | 4 | x | x |
| 5 | 4.1 | 3.9 | A | A | 2 | 1 | x | x |
Rt.: right, Lt.: left, Pre-op: pre-operative, Post-op: post-operative.
DISCUSSION
The Cl level is a common anchor point for posterior approach to treat occipitocervical and atlantoaxial spinal pathology. The C1 lateral mass and C2 pedicle screws for atlantoaxial stabilization are generally used in patients with atlantoaxial instability owing to the safety of screw insertion.1,4,7) However, since the C1 lateral mass screw entry point is covered with the C1–2 venous plexus, C1–2 venous plexus injury can cause profuse bleeding, extending the operation time, when exposed to the C1 lateral mass. Pan et al.19) demonstrated blood loss of up to 1,000 mL. Furthermore, occipital neuralgia is a possible complication of C2 nerve root traction or irritation during C1 lateral mass fixation. Several studies showed that occipital neuralgia occurred in many cases after C1 lateral mass screw insertion.5,24) Although some studies suggested that C2 root sacrifice was not related with occipital neuralgia, further studies are required to identify the occurrence of occipital neuralgia after the sacrifice of the C2 nerve root.6,22)
As an alternative to the C1 lateral mass screw, Lee et al.10) introduced the notching technique of C1 screw insertion. In this method, the entry point is made on the notching of the inferior arch, where the inserted screw is placed partially out of the inferior wall of the posterior arch.10) The notching technique provides a higher entry point than the C1 lateral mass screw to reduce the injury of the C1–2 venous plexus and C2 nerve root. Several studies have provided a method to protect the surrounding tissue of the C1 posterior arch by placing the bone wax and gelatin sponge under the C1 posterior arch.14,19) However, the notching technique still carries a risk of the C1–2 venous plexus and C2 nerve root injury since the entry point of notching technique is close to the entry point of the lateral mass screw. The screw pull-out strength can be weakened from placing the screw out of the inferior wall of the posterior arch.
In the early 2000s, the use of the C1 posterior arch screw was reported independently in two studies.23,25) In the subaxial vertebra, the pedicle is anatomically located at the connection between the vertebral body and the posterior arch. The connection of the C1 posterior arch and the lateral mass in the atlas is anatomically and biomechanically similar to the pedicle of the subaxial vertebra. Therefore, previous studies considered this connection of C1 as a pedicle of C1.14,15) C1 pedicle screw insertion involves placing the screw into the lateral mass via the posterior arch without violating the anterior cortex. There are several advantages to C1 pedicle screw fixation compared to the C1 lateral mass screw and notching technique. First, C1 pedicle screw fixation provides a greater pull-out strength and minimizes the focus of the stress at the screw–bone junction. Second, this method results in less irritation to the C2 nerve root and venous plexus since there is no need to coagulate the C1–2 venous plexus or to retract the nerve caudally when placing the screw via the C1 posterior arch. Third, the C1 pedicle screw entry point is visible better directly. Therefore, C1 pedicle screw fixation is becoming a popular alternative for C1–2 stabilization. However, according to an anatomical study by Tan et al.,25) C1 pedicle screw fixation is not suitable for patients with a thickness of less than 4 mm in the thinnest part of the posterior arch groove.
In a later published study by Tan et al.,26) C1 pedicle screw fixation is feasible for a C1 posterior arch <4 mm or even 2.5 mm using the pedicle exposure technique. However, in the pedicle exposure technique, the outer bone at the posterior arch, inferior to the VA groove along the direction of the trajectory, is removed by Rongeur for exposing the feasible screw entry point in the C1 posterior arch <4 mm. The process of removing part of the cortex of the C1 posterior arch may influence the screw pull-out strength. In addition, the direction of the trajectory was confirmed with fluoroscopic guidance, which is time-consuming and has the risks of accumulative radiation. It is difficult to interpret biplane X-rays taken after C1 pedicle screw insertion. In our study, the C1 pedicle screw can safely inserted in patients with a posterior arch thickness less than 4 mm using direct visualization of the pedicle and serial dilatation technique without fluoroscopy guidance. With minimal exposure of the upper part of the lateral mass and Trendelenburg position change, the C1 pedicle is fully exposed and the C1 pedicle screw was inserted while looking directly at the C1 pedicle so that the screw could be inserted into the desired trajectory without fluoroscopy guidance. A screw of 3.5-mm size can be inserted in patients with less than 4 mm of posterior arch thickness because the pedicle is dilated with serial 2.5- or 3.0-mm drill bits. The pull-out strength does not also decrease from holding the cortical bone above or below or cancellous bone beside the coronal section of the pedicle. In the present study, although patients were only few, the accuracy of the screw was acceptable for grade A and B on postoperative CT in all inserted screws. All screws of grade B were inserted into the pedicle with a diameter less than 3.5 mm. There was no venous plexus bleeding and occipital neuralgia using direct visualization or the serial dilatation technique in our study. However, in pedicles with a diameters of less than 3.5 mm, a long-term follow-up is needed to evaluate the delayed VA injury because the thread of the screw is located beyond the cortical bone above or below the coronal section of pedicle. In addition, more studies should be performed to identify a reduced rate of bleeding of the venous plexus and occipital neuralgia as demonstrated in this study by using direct visualization and serial dilatation technique. Although this study provides only preliminary results and is subject to selection bias, we believe that the described technique is a useful addition to the surgical techniques available for the treatment of C1–C2 instability.
CONCLUSION
According to previous studies, pedicle with a diameter of 4 mm or less pose difficult in pedicle screw insertion. However, out study suggests that C1 pedicle screw insertion using direct visualization and serial dilatation technique is feasible for a C1 posterior arch <4 mm or even 2.5 mm. Freehand placement of the C1 pedicle screw technique is safe and effective even without fluoroscopy guidelines during surgery.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.Aryan HE, Newman CB, Nottmeier EW, Acosta FL, Jr, Wang VY, Ames CP. Stabilization of the atlantoaxial complex via C-1 lateral mass and C-2 pedicle screw fixation in a multicenter clinical experience in 102 patients: modification of the Harms and Goel techniques. J Neurosurg Spine. 2008;8:222–229. doi: 10.3171/SPI/2008/8/3/222. [DOI] [PubMed] [Google Scholar]
- 2.Fensky F, Kueny RA, Sellenschloh K, Püschel K, Morlock MM, Rueger JM, et al. Biomechanical advantage of C1 pedicle screws over C1 lateral mass screws: a cadaveric study. Eur Spine J. 2014;23:724–731. doi: 10.1007/s00586-013-3143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 5.Gunnarsson T, Massicotte EM, Govender PV, Raja Rampersaud Y, Fehlings MG. The use of C1 lateral mass screws in complex cervical spine surgery: indications, techniques, and outcome in a prospective consecutive series of 25 cases. J Spinal Disord Tech. 2007;20:308–316. doi: 10.1097/01.bsd.0000211291.21766.4d. [DOI] [PubMed] [Google Scholar]
- 6.Haque A, Price AV, Sklar FH, Swift DM, Weprin BE, Sacco DJ. Screw fixation of the upper cervical spine in the pediatric population. Clinical article. J Neurosurg Pediatr. 2009;3:529–533. doi: 10.3171/2009.2.PEDS08149. [DOI] [PubMed] [Google Scholar]
- 7.Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 8.Heo Y, Lee SB, Lee BJ, Jeong SK, Rhim SC, Roh SW, et al. The learning curve of subaxial cervical pedicle screw placement: How can we avoid neurovascular complications in the initial period? Oper Neurosurg (Hagerstown) 2019;17:603–607. doi: 10.1093/ons/opz070. [DOI] [PubMed] [Google Scholar]
- 9.Lee KH, Pyeon HJ, Nam H, Won JS, Hwang JY, Lee KA, et al. Significant therapeutic effects of adult human multipotent neural cells on spinal cord injury. Stem Cell Res. 2018;31:71–78. doi: 10.1016/j.scr.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 10.Lee MJ, Cassinelli E, Riew KD. The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine (Phila Pa 1976) 2006;31:2798–2801. doi: 10.1097/01.brs.0000245902.93084.12. [DOI] [PubMed] [Google Scholar]
- 11.Lee S, Seo J, Lee MK, Jeon SR, Roh SW, Rhim SC, et al. Widening of the safe trajectory range during subaxial cervical pedicle screw placement: advantages of a curved pedicle probe and laterally located starting point without creating a funnel-shaped hole. J Neurosurg Spine. 2017;27:150–157. doi: 10.3171/2016.12.SPINE16738. [DOI] [PubMed] [Google Scholar]
- 12.Lee S, Park JH. Minimally invasive cervical pedicle screw placement with a freehand technique through the posterolateral approach using a tubular retractor: a technical note. Oper Neurosurg (Hagerstown) 2019;17:E166–E172. doi: 10.1093/ons/opy375. [DOI] [PubMed] [Google Scholar]
- 13.Lee S, Jung SK, Keshen SG, Lewis SJ, Park JH. A distal start point facilitates safer insertion of s2-alar-iliac screws fixation. J Clin Neurosci. 2020;72:102–107. doi: 10.1016/j.jocn.2019.12.058. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Kim ES, Eoh W. Modified C1 lateral mass screw insertion using a high entry point to avoid postoperative occipital neuralgia. J Clin Neurosci. 2013;20:162–167. doi: 10.1016/j.jocn.2012.01.045. [DOI] [PubMed] [Google Scholar]
- 15.Lin B, Xu Y, Guo ZM, Liu H, Chen ZW, He MC. Feasibility of atlantoaxial pedicle screws' placement in children 6-8 years of age: a cadaveric and tomographic study. J Pediatr Orthop B. 2013;22:399–403. doi: 10.1097/BPB.0b013e32835f583e. [DOI] [PubMed] [Google Scholar]
- 16.Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ. Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine (Phila Pa 1976) 2005;30:1519–1523. doi: 10.1097/01.brs.0000168546.17788.49. [DOI] [PubMed] [Google Scholar]
- 17.Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Xiang M, et al. C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine (Phila Pa 1976) 2009;34:371–377. doi: 10.1097/BRS.0b013e318193a21b. [DOI] [PubMed] [Google Scholar]
- 18.Moon E, Lee S, Chong S, Park JH. Atlantoaxial instability treated with free-hand C1-C2 fusion in a child with Morquio syndrome. Childs Nerv Syst. 2020 doi: 10.1007/s00381-020-04561-2. [DOI] [PubMed] [Google Scholar]
- 19.Pan J, Li L, Qian L, Tan J, Sun G, Li X. C1 lateral mass screw insertion with protection of C1-C2 venous sinus: technical note and review of the literature. Spine (Phila Pa 1976) 2010;35:E1133–E1136. doi: 10.1097/BRS.0b013e3181e215ff. [DOI] [PubMed] [Google Scholar]
- 20.Park JH, Jeon SR, Roh SW, Kim JH, Rhim SC. The safety and accuracy of freehand pedicle screw placement in the subaxial cervical spine: a series of 45 consecutive patients. Spine (Phila Pa 1976) 2014;39:280–285. doi: 10.1097/BRS.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 21.Park JH, Roh SW, Rhim SC. A single-stage posterior approach with open reduction and pedicle screw fixation in subaxial cervical facet dislocations. J Neurosurg Spine. 2015;23:35–41. doi: 10.3171/2014.11.SPINE14805. [DOI] [PubMed] [Google Scholar]
- 22.Patel AJ, Gressot LV, Boatey J, Hwang SW, Brayton A, Jea A. Routine sectioning of the C2 nerve root and ganglion for C1 lateral mass screw placement in children: surgical and functional outcomes. Childs Nerv Syst. 2013;29:93–97. doi: 10.1007/s00381-012-1899-1. [DOI] [PubMed] [Google Scholar]
- 23.Resnick DK, Benzel EC. C1-C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery. 2002;50:426–428. doi: 10.1097/00006123-200202000-00039. [DOI] [PubMed] [Google Scholar]
- 24.Rhee WT, You SH, Kim SK, Lee SY. Troublesome occipital neuralgia developed by c1-c2 harms construct. J Korean Neurosurg Soc. 2008;43:111–113. doi: 10.3340/jkns.2008.43.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, et al. Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976) 2003;28:888–895. doi: 10.1097/01.BRS.0000058719.48596.CC. [DOI] [PubMed] [Google Scholar]
- 26.Tan M, Dong L, Wang W, Tang X, Yi P, Yang F, et al. Clinical application of the “pedicle exposure technique” for atlantoaxial instability patients with a narrow c1 posterior arch. J Spinal Disord Tech. 2015;28:25–30. doi: 10.1097/BSD.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 27.Zarro CM, Ludwig SC, Hsieh AH, Seal CN, Gelb DE. Biomechanical comparison of the pullout strengths of C1 lateral mass screws and C1 posterior arch screws. Spine J. 2013;13:1892–1896. doi: 10.1016/j.spinee.2013.06.015. [DOI] [PubMed] [Google Scholar]