Abstract
Objective
To compare the test-retest reliability and validity of three simple maximal isometric back extensor strength (BES) assessment protocols with different test postures, and to recommend an optimal clinical protocol to quantify BES.
Methods
Asymptomatic adults, aged over 45 years, were assessed for maximal isometric BES using external fixation of dynamometers, with the subject in standing, prone and sitting positions, respectively. Measurements were repeated at a one-week interval to examine test-retest reliability. Validation was performed by comparing with results obtained from isokinetic dynamometer assessments.
Results
Out of a total of 60 included participants, intra-class correlation coefficients (ICC) were 0.92, 0.93 and 0.90 in standing, prone and sitting positions, respectively. Correlation analyses revealed acceptable convergent validity in the standing and prone position (r = 0.50 and 0.54, respectively), whereas tests conducted in the sitting position showed a relatively low validity (r = 0.32). Among the three protocols, measurement error was lowest in the prone position.
Conclusions
Maximal isometric BES assessment in the prone position was shown to be the most reliable and valid protocol, and may be considered the preferred option for assessing BES in clinical practice.
Keywords: Back extensor, isometric strength, postures, dynamometer, reliability, validity
Introduction
Back extensor strength (BES) is an important determinant of physical function and has been identified as a primary predictor of frailty, poor quality of life and morbidity in older people.1 Thus, it is important that back muscle strength be assessed in high risk populations, and be included in goal-setting and treatment programs for those who have lumbar dysfunction.2
Conventional manual muscle testing in the clinic is inherently subjective, with poor validity and reliability.3 The current gold standard uses a large device called an isokinetic dynamometer, which can provide accurate evaluations of dynamic and static BES and is usually the first choice in clinical research.4 However, due to high cost, lack of portability, and space limitations, the isokinetic dynamometer is not practical in clinical and epidemiological settings. A hand-held dynamometer (HHD) is a relatively time-saving and inexpensive apparatus now commonly used in clinical practice. Use of external fixation, e.g. with a belt, can reduce measurement errors compared with assessments during which the tester manually fixes the HHD.5
Although previous studies have addressed HHD-test reliability issues, by devising methods to fix the HHD for BES measurements with subjects in standing and prone positions,6–8 an optimal and standardized BES assessment protocol in clinical settings remains absent, which may be partly due to a lack of adequate methodological research and comparisons based on reliability and validity. Different test postures are likely to lead to deviations in force assessment on the thoracic level.9 However, the performance of HHDs with subjects in different test positions has not been investigated well enough to determine whether this affects BES testing, and the present authors suggest that test posture is an important consideration for an accurate assessment of BES.
The purpose of the present study was to compare the test-retest reliability and validity of three isometric back extensor strength methods, using externally-fixed dynamometers with different subject positioning, and to identify an optimal clinical protocol that best predicts back extensor strength.
Subjects and methods
Study population
Volunteers included in this prospective study were recruited from Southwest Hospital, Third Military Medical University, Chongqing, China between March 2018 and March 2019. The inclusion criteria were: (1) aged over 45 years; (2) ambulatory and independent in daily living activities; and (3) no current back pain that could interfere with maximal effort during evaluations of strength.10 Exclusion criteria comprised: (1) severe back pain within the previous 3 months; (2) new onset of radiologically verified fractures or extremity injury; (3) a history of surgery; and (4) back strength training within the previous 6 months.
The study was approved by the Ethics Committee of the First Affiliated Hospital, Third Military Medical University, PLA (approval number KY201853). All study participants provided written informed consent prior to evaluation, and all research activities adhered to the tenets of the Declaration of Helsinki.
Study design
All subjects were examined during two testing sessions with a 1-week interval. During session 1, the demographic characteristics were recorded, and BES was measured in the standing, prone, and sitting positions, using an Excel 2016 random number generator (Microsoft, Redmond, WA, USA) to determine the order of testing. Session 2 followed the same test order and subjects were additionally assessed using an isokinetic dynamometer. The test procedures were standardized (Table 1), and on each test day, each method was applied with an intermission of 1 h to ensure complete recovery between tests.11 All three isometric tests required the participant to warm up before formal testing, followed by 3 × 5 s maximal efforts, separated by a 1 min pause to reduce potential fatigue. The maximum value of three trials was recorded for each test. To ensure the highest BES had been attained, an additional trial was performed when the last measurement value was >5% higher than the previous value.7 All assessments were performed by the same experienced tester (SY) and verbal instructions were provided to motivate the participant to exert maximal effort. The dynamometer was zeroed before each trial and was calibrated with known weights on a monthly basis, to ensure the consistency of linear responses.
Table 1.
Three isometric and one isokinetic measurement methods for back extensor strength.
| BES test | Exercise | Test position | Arm | Hip | Knee joint | Sensor pad location | Fixation location |
|---|---|---|---|---|---|---|---|
| Gauge | Back Extension | Standing | Cross on chest | Extension | Extension | Xipho-Sternal Junction†† | Pelvis (over bilateral anterior superior iliac spine) |
| HHD | Back Extension | Prone | Along the body† | Extension | Extension | Midline between the two anguli superior to scapulae | Over the dynamometer and around the underside of the table |
| HHD | Back Extension | Sitting | Cross on chest | 90° Flexion | 90° Flexion‡ | Midline between the two anguli superior to scapulae | Over both upper thighs and around the underside of the chair |
| IKD | Back Extension | Sitting | 60° Flexion | 90° Flexion | 90° Flexion | A line connecting the vertebral angle of the scapulae | Both knees and proximal thighs, lower lumbar spine |
BES, back extensor strength; HHD, handheld dynamometer; IKD, isokinetic dynamometer.
Palms facing upwards and lift arms from the couch; ‡Feet off the ground; ††Sensor pad was replaced by a hook which was attached horizontally to the gauge by rope.
Standing position test
In order to assess BES in the standing position, a frame based on the work of Davarian et al.,12 was developed, and an SF-500 diagram tension dynamometer (SUNDOO Inc, Wenzhou, Zhejiang, China) was attached to the bracket. Participants wore a collar with a hook placed at the level of the xiphoid process, and stood facing the frame, with their pelvis fixed to the bottom baffle by a strap and their arms crossed in front of their chest. An inextensible wire was connected from the fixed dynamometer to the hook on the participant’s collar (Figure 1a). The test procedures followed the recommendations of Jorgensen and Nicolaisen,11 with the trunk starting position at 30° of flexion, determined by a digital goniometer (Sanliang Inc, Jiangyin, Jiangsu, China). Participants were then asked to extend their trunk against the rope with maximum effort for 5 s and the monitor displayed their effort as force (N).
Figure 1.
Representative images showing examples of participant positioning for three isometric back extensor strength (BES) tests utilizing different postures: (a) standing BES with a tension dynamometer; (b) prone BES with tripod fixation of the handheld dynamometer; and (c) seated BES with a chair-box fixation system for the handheld dynamometer.
Prone position test
Prone position BES was measured with a microFET3 isometric dynamometer (Hoggan Scientific, Salt Lake City, UT, USA) that was externally fixed using a lightweight aluminium tripod and belt system, similar to that developed by Valentin and Maribo.8 The participant was positioned on the treatment table with their trunk straight, arms along their body, palms facing upwards, and feet over the edge of the table. Two belts were then secured over the dynamometer and around the underside of the table. Tests were conducted according to the recommendations of Limburg et al.7 After achieving the correct starting position, the participant was asked to raise their hands, lift their head, and push back against the tripod with maximal force (N) for 5 s (Figure 1b). The peak BES was recorded for each effective trial.
Sitting position test
Maximal BES in the sitting position was also measured using a microFET3 isometric dynamometer (Hoggan Scientific) and a chair-box system that was designed for external fixation. The chair without a backboard was fixed to the wall using four pipe clamps and the microFET3 dynamometer was fixed in an aluminium box suspended by a vertical and adjustable string along the wall. The test position and procedures were as previously described.13 The participants were asked to sit with their hips and knees flexed at 90°, arms crossed on their chest, and feet off the ground. A strap was then secured over the top of the thigh and around the underside of the chair. The transducer pad was aligned with the midline connecting two superior borders of the scapula (Figure 1c). From this position, the subject was asked to stretch their trunk backward against the wall with maximum effort. Direct contact between the upper trunk and the transducer head was maintained for 5 s. The maximal force (N) of three trials was recorded.
Isokinetic dynamometer test
To validate the three maximal isometric BES test results, participants were assessed using the IsoMed 2000 isokinetic dynamometer (D&R Ferstl GmbH, Hemau, Germany), an ideal piece of equipment to determine muscle force. The test position and procedures followed the recommendations of Dvir and Keating.14 The tested range of motion was set to cover 20°, based on motion of the lever arm, and based on this range of motion, test velocities were set at 60°/s.4 Once positioned, after one or two submaximal practices for familiarization, each participant completed five successive repetitions for the isokinetic mode, starting in an upright position and performing a subsequent trunk extension sweeping from 0° to 20°. Participants were instructed to perform the maximum extension and verbal encouragements were given to encourage maximum physical effort throughout the protocol. Peak torque was recorded in Newton metres (N⋅m) for each trial, and the highest torque achieved from 5 successful trails was used in validity analyses.
Statistical analyses
Data are presented as mean ± SD. The intra-class correlation coefficient (ICC) and limits of agreement (LOA) were used to define the quality and magnitude of reliability of the measurements plotted with a 95% confidence interval (CI) using the Bland–Altman method.15 To identify the absolute variability, the standard error of measurements (SEM) were quantified, as well as the smallest detectable change (SDC). The coefficient of variation (CV) was calculated as the SEM on a log scale.8 Peak force values from BES isometric tests were validated against peak torque values derived from the isokinetic dynamometer, using a two-tailed Pearson’s correlation coefficient (r) with 95% confidence intervals. The strength of correlations were interpreted as low (0.1–0.3), medium (0.3–0.5), or high (0.5–1.0).16 ICC values of <0.50, 0.50–0.75, or >0.75 indicated poor, moderate, or good to excellent reliability, respectively.17 A P value <0.05 was determined to be statistically significant and all statistical analyses were performed using SPSS for Windows, version 20.0 (SPSS Inc, Chicago, IL, USA).
Results
A total of 60 volunteers (50 female and 10 male) were recruited into the study and completed both sessions (mean ± SD age, 61.7 ± 7.6 years; height, 153.5 ± 7.3 cm; weight, 57.6 ± 7.4 kg; and body mass index, 24.5 ± 2.8 kg/m2). Three of the female participants were unable to attend the isokinetic test: two, due to osteoarthritis in the shoulder and one due to back pain after the second isometric test in the standing position. Therefore, a total of 60 subjects (50 female and 10 male) were included in the final reliability analysis, and 57 subjects (47 female and 10 male) were included in the validity analysis.
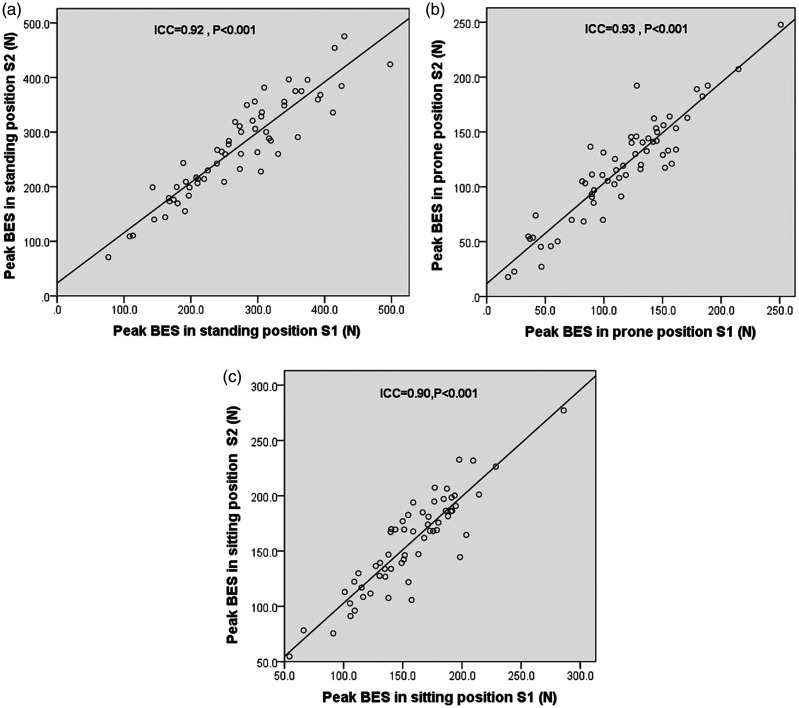
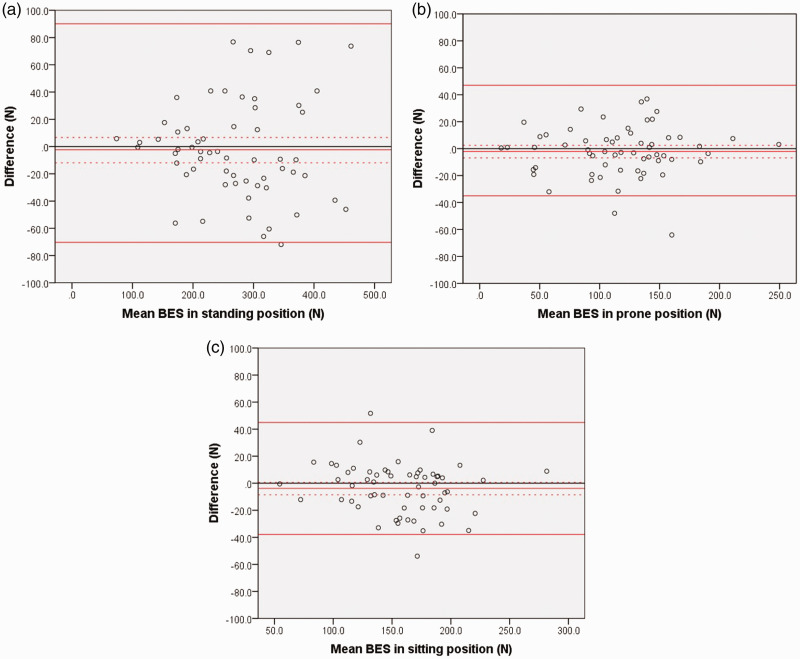
Test-retest reliability and measurement error for each test procedure are presented in Table 2. Between-session reliability of isometric BES measures, determined with external fixation of the HHD in standing (ICC 0.92, 95% CI 0.87, 0.95; P < 0.001), prone (ICC 0.93, 95% CI 0.88, 0.95; P < 0.001), and sitting (ICC 0.90, 95% CI 0.83, 0.94; P < 0.001) positions was excellent (Figure 2). The SEM value (representing random error) was highest in the standing position (25.5), followed by the sitting (13.2) and prone position (13.0). Similarly, the CV and SDC values were highest in the standing position and lowest in the prone position (Table 2). The Bland–Altman plots show the means and absolute differences of repeated isometric BES measures with external fixation of the HHD in different positions (Figure 3). The LOA values were –70.35 to 90.15 N with a mean bias of –2.3 N in the standing position, –35.01 to 47.10 N with a mean bias of –2.1 N in the prone position, and –37.83 to 44.94 N with a mean bias of –3.8 N in the sitting position (Table 2). All three test procedures showed higher peak back extensor strength in session 2 compared with session 1, suggesting a mild learning effect.
Table 2.
Measurement error and reliability of three maximal isometric back extensor strength assessments with different subject positioning.
| Test position | Session 1 Peak (N)a | Session 2 Peak (N)a | Diffa,b | Statistical significance | SEM | CV (%) | SDC | ICC (95% CI) | LOA |
|---|---|---|---|---|---|---|---|---|---|
| Standing | 269.6 ± 89.1 | 271.9 ± 89.3 | –2.3 ± 36.0 | P = 0.63 | 25.5 | 20.3 | 70.7 | 0.92 (0.87, 0.95) | –70.35, 90.15 |
| Prone | 115.2 ± 47.4 | 117.3 ± 47.0 | –2.1 ± 18.4 | P = 0.37 | 13.0 | 5.7 | 36.0 | 0.93 (0.88, 0.95) | –35.01, 47.10 |
| Sitting | 155.1 ± 39.8 | 158.9 ± 43.0 | –3.8 ± 18.7 | P = 0.71 | 13.2 | 6.0 | 36.6 | 0.90 (0.83, 0.94) | –37.83, 44.94 |
Data presented as mean (SD); bSession 1–session 2.
Diff, between-session difference; SEM, standard error of measurements; CV, coefficient of variation; SDC, Smallest detectable change; ICC, intraclass correlation coefficient; CI, confidence interval; LOA, limits of agreement.
Figure 2.
Scatter plots of test-retest reliability of the three back extensor strength (BES) procedures in healthy adults (n = 60), showing: (a) standing; (b) prone; and (c) sitting positions. An overall excellent reliability was found in all protocols. N, Newtons; S1, session 1; S2, session 2; ICC, intra-class correlation. P < 0.001 (Pearson’s correlation coefficient analyses).
Figure 3.
Bland–Altman plots of back extensor strength (BES) data in healthy adults (n = 60), tested in: (a) standing; (b) prone; and (c) sitting positions. Plots illustrate mean bias (middle solid red line), the upper and lower limits of 95% confidence interval for measurement errors (red upper and lower dashed lines), and limits of agreement (red upper and lower solid lines) between two separate measurement sessions.
Analyses of the correlation between the absolute differences and mean BES value in the two-stage assessments are presented in Table 3. In the standing position, there was a statistically significant positive correlation between the values (P < 0.001), whereas homoscedasticity in the prone and sitting positions was validated by the lack of a significant difference between the absolute differences and the mean values.
Table 3.
Relationship between absolute differences in back extensor strength and the mean of paired measures.
| Test position | r | 95% CI | Statistical significance |
|---|---|---|---|
| Standing | 0.50 | 0.31, 0.66 | P < 0.001 |
| Prone | 0.01 | −0.23, 0.24 | P = 0.955 |
| Sitting | 0.09 | −0.11, 0.30 | P = 0.515 |
CI, confidence interval; r, Pearson’s correlation coefficient.
A total of 57 participants underwent evaluations of BES using the IsoMed-2000 isokinetic dynamometer, and the mean peak torque was 80.9 ± 38.5 N·m. Peak isometric BES was strongly associated with isokinetic dynamometer-derived peak torque in the standing position (r = 0.50, P < 0.01 in session 1 and r = 0.60, P < 0.01 in session 2) and prone position (r = 0.54, P < 0.01 in both session 1 and session 2). However, it was only moderately correlated with BES in the sitting position (r = 0.32, P < 0.05 in both session 1 and session 2; Table 4).
Table 4.
Validity of isometric methods shown by correlation between back extensor strength values from three hand-held dynamometer isometric methods and isokinetic dynamometer-derived torque.
| Test position | Session 1 |
Session 2 |
||
|---|---|---|---|---|
| R | 95% CI | r | 95% CI | |
| Standing | 0.50** | 0.28, 0.67 | 0.60** | 0.42, 0.73 |
| Prone | 0.54** | 0.31, 0.74 | 0.54** | 0.31, 0.74 |
| Sitting | 0.32* | 0.07, 0.52 | 0.32* | 0.04, 0.57 |
r, Pearson’s correlation coefficient; CI, confidence interval.
*P <0.05; **P <0.01.
The correlations among the three isometric measurements are presented in Table 5. In addition to a high consistency of internal paired measurement values, a good agreement was observed between the standing and prone position (r = 0.50–0.61, P < 0.01), and a high correlation was observed between the prone and sitting position (r = 0.56–0.60, P < 0.01). The correlation between the standing and sitting position was relatively poor (r = 0.25–0.35, P < 0.05).
Table 5.
Correlations among three maximal isometric back extensor strength measurements with different subject positioning.
| Test position | Standing S1 | Standing S2 | Prone S1 | Prone S2 | Sitting S1 | Sitting S2 |
|---|---|---|---|---|---|---|
| Standing S1 | 1 | 0.92** | 0.50** | 0.50** | 0.25* | 0.29* |
| Standing S2 | 1 | 0.58** | 0.61** | 0.31* | 0.35** | |
| Prone S1 | 1 | 0.92** | 0.59** | 0.60** | ||
| Prone S2 | 1 | 0.56** | 0.59** | |||
| Sitting S1 | 1 | 0.90** | ||||
| Sitting S2 | 1 |
S1, session 1; S2, session 2.
*P <0.05; **P <0.01 (Pearson’s correlation coefficient analyses).
Discussion
The present study was primarily an investigation and comparison of the reliability and validity of three maximal isometric back extensor strength measurements with different subject positioning in the same study population. All three protocols produced excellent test-retest reliability in terms of ICC, and showed that an external fixed dynamometer is a highly reliable tool to quantify back extensor strength in different postures. When using an HHD fixed with a tripod with the subject in a prone position, an acceptable degree of measurement error and reliability was achieved. A higher level of measurement error was observed when using a tension dynamometer with the subject in a standing position.
Using a Bland–Altman plot, differences between the paired tests in the standing position were found to increase as mean BES increased, whereas between-test differences within the prone and sitting positions were maintained at a relatively low level. This phenomenon may be related to the different levels of posture maintenance during these tests, since the effort made by the subject generates an intrinsic measurement error that is difficult to completely control when maximal contractions are requested.18 The subject made maximal voluntary exertion in the standing position, moving the trunk beyond the ‘cone of economy’, thus requiring more energy to maintain an upright position, leading to muscle fatigue and discomfort.19 Conversely, the anticipation of pain and the fear of possible impairment of movement may also lead to an inability or unwillingness to stretch as hard as possible in the standing position, thereby interfering with the maximal isometric strength test of the back extensor muscles.20 In the present study, compared with the pulling test in a standing position, tests in the prone and sitting positions were more stable, since the trunk movement was limited with external fixation of HHDs. Counter pressure was provided directly by the tripod and the wall, respectively, thereby eliminating measurement variations. However, upper body weight may have influenced performance during the prone position test, which was based on a modified Biering-Sørensen test, and may have resulted in a source of inter-individual variation.21 Nonetheless, in the present study, results of tests in the prone position had the lowest random error and systematic error among the three protocols. In addition, fixation of the HHD with a tripod to assess BES, with the participant in a prone position, allows accurate evaluation of BES without discomfort, and poses minimal risk of injury to even the severely disfigured spine.10
A comparison of average force measurements in the present study showed that BES measured in the standing position was highest among the three methods, at almost 154.5 N higher than results from the prone position and 113.8 N higher than values from the sitting position, and this order was consistent with the ranking of CV, SDC, and LOA. To the best of the authors’ knowledge, no reference values for between-position comparisons of back extensor strength assessments have been provided by previous studies.
The present study results showed good validity for BES measurements in the standing and prone position. This may be because all subjects had a fully extended trunk aligning with the hips and knees in the neutral position, which was beneficial to the back-extensor muscle specifically tested. In the standing position, participants stood on a frame with their pelvis fixed to the bottom bracket by a strap, which strictly limited the involvement of other muscle groups in the maximal back extension. However, restraining straps are not required with the appropriate placement of the participant in the prone position, the natural, relaxed prone posture curbs any movement at the level of the pelvis.7 Although the excellent test-retest reliability favours the chair-box system for the clinical assessment of BES in the sitting position, participants cannot be strictly stabilized when performing maximal trunk extension, therefore other muscle groups, such as the thigh musculature, rather than just the back extensors, may be involved in the test.22 This problem was shown by the relatively low validity found in the present study.
Harding et al.6 introduced a BES assessment protocol for the standing position, involving a pair of vertically oriented anchor rails on the wall, which was tested on 52 healthy adults aged 46.4 ± 20.4 years. The validity was 0.82, and was above the validity of 0.60 in the present study. The figures in the Harding study appear to show that the isokinetic dynamometer testing (to validate the novel test) was performed in the standing position,6 while the isokinetic dynamometer measures were conducted seated in the present study, which may have limited the ability to validate the isometric tests in the standing position. Another study, involving 50 healthy female participants aged 30–79 years, examined reliability using an isometric dynamometer (BID-2000) with the subject in prone position, and showed a CV of 2.33% and a correlation of 0.38 with isokinetic-dynamometer torque.7 Valentin et al.8 introduced a tripod to fix the HHD in assessing BES in a prone position, and verified the method with a study population of 48 female patients diagnosed osteopenia, with an ICC results of 0.90 and CV of 17%. The present result of 5.7% for CV and ICC of 0.93 in the prone position test, suggest a more stable and highly reliable test than previously reported.8 The present CV results could not be compared with the study by Limburg et al.,7 as they did not describe their method of CV calculation. Nonetheless, the better correlation with isokinetic-dynamometer torque in the present study (0.54 versus 0.38), suggests that the external belt system to fix the HHD improved validity compared with the Limburg study.
The correlation between muscle strength values measured in different positions were also analysed in order to compare the methodologies. The results indicated a good agreement between the standing and prone positions, and a high correlation between the prone and sitting positions. The correlations among the three tests suggested that the prone position test is most likely to minimize postural heterogeneity in BES testing, and better reflects BES measured in different positions than the other protocols.
The results of the present study may be limited by several factors. First, the gender imbalance due to the high proportion of female participants in this study population may have resulted in the measured values of BES not objectively reflecting the actual average value of the wider community population of the same age-group. Secondly, isokinetic dynamometer measures were seated values, which may limit comparisons with prone and standing measures to determine validity. Lastly, since the subjects were a healthy and ambulatory population, it is not clear whether the study findings apply to other groups of people, such as individuals with musculoskeletal injury. Therefore, further research is needed to validate the present results.
In conclusion, the present study describes and tests three simple maximal isometric BES assessment protocols in asymptomatic adults using externally-fixed dynamometers with different subject positioning. In light of acceptable reliability, validity and measurement errors, maximal isometric back extensor strength assessment, with the subject in a prone posture, can be applied to individuals with different back strength levels and may be the most useful for ranking back extensor strength in clinical and epidemiological studies.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The research was supported by funds from the Health Bureau of the Logistics Support Department of the CMC, China (grant No. AWS17J004); the Clinical Medical Research Program of the Third Military Medical University (grant No. 2018XLC3010); and the Chongqing Graduate Research and Innovation project (grant No. CYS19369).
References
- 1.Gomes MJ, Martinez PF, Pagan LU, et al. Skeletal muscle aging: influence of oxidative stress and physical exercise. Oncotarget 2017; 8: 20428–20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Granacher U, Gollhofer A, Hortobagyi T, et al. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review. Sports Med 2013; 43: 627–641. [DOI] [PubMed] [Google Scholar]
- 3.Nadler SF, DePrince ML, Hauesien N, et al. Portable dynamometer anchoring station for measuring strength of the hip extensors and abductors. Arch Phys Med Rehabil 2000; 81: 1072–1076. [DOI] [PubMed] [Google Scholar]
- 4.Roth R, Donath L, Kurz E, et al. Absolute and relative reliability of isokinetic and isometric trunk strength testing using the IsoMed-2000 dynamometer. Phys Ther Sport 2017; 24: 26–31. [DOI] [PubMed] [Google Scholar]
- 5.Thorborg K, Bandholm T, Holmich P. Hip- and knee-strength assessments using a hand-held dynamometer with external belt-fixation are inter-tester reliable. Knee Surg Sports Traumatol Arthrosc 2013; 21: 550–555. [DOI] [PubMed] [Google Scholar]
- 6.Harding AT, Weeks BK, Horan SA, et al. Validity and test-retest reliability of a novel simple back extensor muscle strength test. SAGE Open Med 2017; 5: 2050312116688842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Limburg PJ, Sinaki M, Rogers JW, et al. A useful technique for measurement of back strength in osteoporotic and elderly patients. Mayo Clin Proc 1991; 66: 39–44. [DOI] [PubMed] [Google Scholar]
- 8.Valentin G, Maribo T. Hand-held dynamometry fixated with a tripod is reliable for assessment of back extensor strength in women with osteoporosis. Osteoporos Int 2014; 25: 2143–2149. [DOI] [PubMed] [Google Scholar]
- 9.Kocjan A, Sarabon N: Assessment of isometric trunk strength - the relevance of body position and relationship between planes of movement. J Sports Sci Med 2014; 13: 365–370. [PMC free article] [PubMed] [Google Scholar]
- 10.Sinaki M, Khosla S, Limburg PJ, et al. Muscle strength in osteoporotic versus normal women. Osteoporos Int 1993; 3: 8–12. [DOI] [PubMed] [Google Scholar]
- 11.Jorgensen K, Nicolaisen T. Trunk extensor endurance: determination and relation to low-back trouble. Ergonomics 1987; 30: 259–267. [DOI] [PubMed] [Google Scholar]
- 12.Davarian S, Maroufi N, Ebrahimi I, et al. Trunk muscles strength and endurance in chronic low back pain patients with and without clinical instability. J Back Musculoskelet Rehabil 2012; 25: 123–129. [DOI] [PubMed] [Google Scholar]
- 13.Mika A, Unnithan VB, Mika P. Differences in thoracic kyphosis and in back muscle strength in women with bone loss due to osteoporosis. Spine (Phila Pa 1976) 2005; 30: 241–246. [DOI] [PubMed] [Google Scholar]
- 14.Dvir Z, Keating J. Reproducibility and validity of a new test protocol for measuring isokinetic trunk extension strength. Clin Biomech (Bristol, Avon) 2001; 16: 627–630. [DOI] [PubMed] [Google Scholar]
- 15.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310. [PubMed] [Google Scholar]
- 16.Stark T, Walker B, Phillips JK, et al. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R 2011; 3: 472–479. [DOI] [PubMed] [Google Scholar]
- 17.Kolber MJ, Cleland JA. Strength testing using hand-held dynamometry. Phys Ther Rev 2005; 10: 99–112. [Google Scholar]
- 18.Wang CY, Olson SL, Protas EJ. Test-retest strength reliability: hand-held dynamometry in community-dwelling elderly fallers. Arch Phys Med Rehabil 2002; 83: 811–815. [DOI] [PubMed] [Google Scholar]
- 19.Schwab F, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010; 35: 2224–2231. [DOI] [PubMed] [Google Scholar]
- 20.Al-Obaidi SM, Nelson RM, Al-Awadhi S, et al. The role of anticipation and fear of pain in the persistence of avoidance behavior in patients with chronic low back pain. Spine (Phila Pa 1976) 2000; 25: 1126–1131. [DOI] [PubMed] [Google Scholar]
- 21.Gruther W, Wick F, Paul B, et al. Diagnostic accuracy and reliability of muscle strength and endurance measurements in patients with chronic low back pain. J Rehabil Med 2009; 41: 613–619. [DOI] [PubMed] [Google Scholar]
- 22.Burnham RS, Bell G, Olenik L, et al. Shoulder abduction strength measurement in football players: reliability and validity of two field tests. Clin J Sport Med 1995; 5: 90–94. [DOI] [PubMed] [Google Scholar]