Abstract
Objective
This study was performed to evaluate the position and morphology of the temporomandibular joint in female patients with skeletal class II malocclusion and to investigate the association between temporomandibular joint disorders and facial types using cone-beam computed tomography.
Methods
A lateral cephalogram was taken to determine the skeletal class of each participant. Sixty female patients aged 16 to 28 years were divided into high-angle, low-angle, and control groups. The shape of the condyle–fossa was measured and assessed on cone-beam computed tomography images of the 120 temporomandibular joints.
Results
Some condylar shape measurements displayed statistically significant differences among the groups. No significant differences were found in the length of the condyle, width of the glenoid fossa, or height of the articular eminence among the three groups. The posterior condylar position was more frequently observed in the low-angle group, whereas the anterior condylar position was more prevalent in the high-angle group.
Conclusion
The present study revealed differences in the condyle–fossa morphology and position in female patients with skeletal class II malocclusion with different vertical facial types.
Keywords: Cone-beam computed tomography, temporomandibular joint, osteoarthritis, vertical facial types, skeletal class II females, condylar position
Introduction
The temporomandibular joint (TMJ) is one of the most complex joints in the human body. This joint is a sophisticated articular system located between the mandibular condyle and the temporal bone.1,2 The continuous growth and stimulation of the condyle from childhood to adulthood leads to self-remodeling. As a part of the TMJ, the condyle can continually adapt to functional stimulation.
The clinical significance of the condyle–fossa relationship in the TMJ remains controversial.3 However, the shape of both the condyle and fossa may play a diagnostic role in the accurate prediction and clinical identification of TMJ osteoarthritis (OA), which requires treatment.4 The spectrum of clinical and pathologic presentations of TMJ OA ranges from structural and functional failure of the joint with disc displacement and degeneration to subchondral bone alterations (erosions), bone overgrowth (osteophytes), and loss of the articular fibrocartilage. Studies have shown an association of abnormal morphology and the position of the condyle with the development of TMJ OA.5
The condylar shape and position can be influenced by many dynamically variable factors, such as age, sex, functional matrix activities, increased or decreased masticatory force, occlusion changes, physiological adaptations, and the facial growth pattern.6,7
A previous study showed that the condylar position and fossa morphology varied according to the sagittal skeletal features.8 In addition, some researchers have stated that the condylar position has no association with the vertical skeletal pattern.9,10
In the present study, cone-beam computed tomography (CBCT) was employed to study the morphology and position of the condyle. Our aim was to evaluate the morphology and position of the condyle based on established vertical facial types and gain insight into the relationship between TMJ OA and vertical facial types.
Materials and methods
Data collection and patient grouping
This study was performed at the Orthodontic Department of the Stomatological Hospital of Xi'an Jiaotong University (Xi'an, Shaanxi, China). High-resolution CBCT imaging sets of the TMJ were collected from January 2015 to June 2019 at the College of Stomatology, Xi'an Jiaotong University. Female patients were equally divided into a high-angle, low-angle, and control group. Before the study began, we took a lateral cephalogram of each participant who required orthodontic treatment to obtain measurements for the inclusion criteria (ANB angle, Frankfurt horizontal–mandibular plane angle [FH-MP], and sella–nasion to gonion–gnathion angle [GoGn-SN]) before the study. Measurements were performed and assessed by an orthodontist, an arthrologist, and a radiologist.
The inclusion criteria in the control group were individual normal occlusion with a class I molar relationship, 0° < ANB < 5°, 22° < FH-MP < 32°, and 27.3° < GoGn-SN < 37.7°. The inclusion criteria in the high-angle group were a class II molar relationship, ANB > 5°, FH-MP > 32°, and GoGn-SN > 37.7°. The inclusion criteria in the low-angle group were a class II molar relationship, ANB > 5°, FH-MP < 22°, and GoGn-SN < 27.3°.
All three groups comprised female patients with no TMJ disorders (TMDs) (TMJ pain, limited opening, reciprocal clicking, and crepitus). The exclusion criteria in all three groups were a history of pregnancy, orthodontic treatment and maxillofacial trauma, evidence of TMDs in a clinical or imaging examination, history of TMJ treatment, obvious mandibular deviation, congenital craniofacial anomalies, visible facial asymmetry, and systemic diseases such as rheumatic arthritis and rheumatoid arthritis.
The study was approved by the Ethical Committee of Xi'an Jiaotong University (approval number xjkqll[2017] No. 022). After being informed about the nature of the experiment in detail, all participating individuals were willing to be enrolled in the trial and provided written informed consent. The statutory guardians of minors aged <18 years provided consent.
CBCT imaging
CBCT images of the bilateral TMJs were obtained by the same operator using a KaVo 3D eXam (KaVo Dental GmbH, Biberach, Germany). The image scanning protocol was as follows: field of view, 17 cm × 23 cm; 120 kV; 5 mA; exposure time, 7 seconds; and slice thickness, 0.1 mm. The scanner had sufficient image sharpness and contrast for visualization of the structures to be evaluated (articular eminence and mandibular fossa). The participants were positioned in a seated posture and bit their teeth into maximum intercuspal position. Their heads remained motionless with the Frankfort plane parallel with the ground. The scanner rotated 360° around the participant’s head. All images were obtained under the same conditions by the same experienced radiologist using the same device.
Measurements
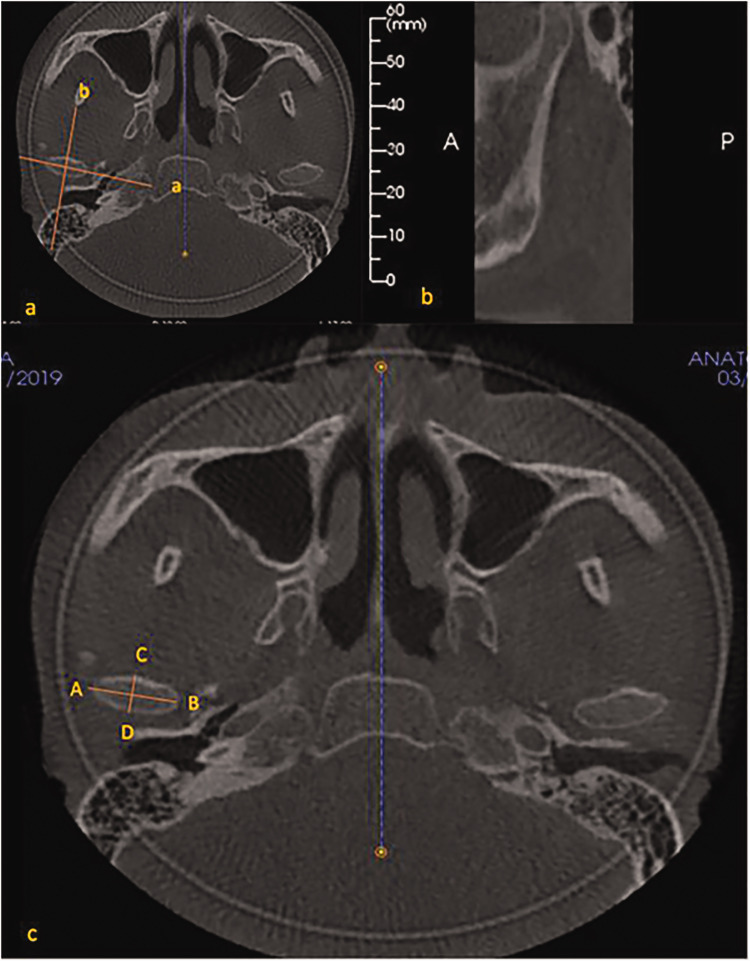
All patients underwent CBCT scans, and the images were three-dimensionally reconstructed using the third-party design software Invivo Dental 5.2 (KaVo Dental GmbH). Digital reconstruction was then conducted in the maxillofacial region. To correct the coronal and sagittal views, the view in which the bilateral condyles were symmetrical in size and exhibited the maximum area was chosen as the reference view for the secondary reconstruction (Figure 1a). On the corrected sagittal view (Figure 1b), the condylar process showed the maximal long axis, and the sagittal reference line was perpendicular to the long axis and passed through its midpoint. On the corrected coronal view, the condylar process had the maximum long axis, and the coronal reference line was parallel to the long axis and passed through its midpoint.
Figure 1.
(a) Axial view shows the maximum condylar area as the reference for the secondary reconstruction. a: Coronal reference line. b: Sagittal reference line. (b) Sagittal cross-sectional image corresponding to line b shown in (a). (c) AB: Mediolateral diameter of the condyle. CD: Anteroposterior diameter of the condyle.
The measurements were obtained according to the methods established by Yasa and Akgul11 and Ganugapanta et al.12 On the axial view, the mediolateral and anteroposterior diameters of the condyle could be measured (Figure 1c). On the standardized sagittal plane, we measured the depth and width of the glenoid fossa (Figure 2a), the width and height of the condylar head (Figure 2b), the length of the condyle (Figure 2c), the inclination (Figure 2d) and height of the articular eminence (Figure 2e), and the anterior, superior, and posterior joint spaces (Figure 2f). The definitions of these measurements are listed in Table 1.
Figure 2.
(a) GH: Depth of the glenoid fossa. EF: Width of the glenoid fossa. (b) ML: Height of the condylar head. JK: Width of the condylar head. (c) OP: Length of the condyle. (d) β: Inclination of the articular eminence. (e) q: Height of the articular eminence. (f) a: Anterior joint space. s: Superior joint space. p: Posterior joint space.
Table 1.
Definitions of measurements.
| Parameter | Definition |
|---|---|
| Mediolateral diameter of the condyle | Distance between the outermost point and innermost point of the condyle. |
| Anteroposterior diameter of the condyle | Distance between the foremost point and backmost point of the condyle. |
| Width of glenoid fossa | Distance between the lowermost point of the articular eminence and the lowermost point of the internal acoustic meatus. |
| Depth of glenoid fossa | A vertical line is drawn from the uppermost point of the glenoid fossa to the full width of the glenoid fossa. The distance between the uppermost point and the vertical point is the depth of the glenoid fossa. |
| Width of condylar head | Distance between the foremost point and backmost point of the condylar head. |
| Height of condylar head | A vertical line is drawn from the uppermost point of the condylar head to the full width of the condylar head. The distance between the uppermost point and the vertical point is the height of the condylar head. |
| Length of the condyle | A tangent line is drawn from the mandibular ramus to the sigmoid notch. The perpendicular distance between the uppermost point of the condyle and the tangent line is the length of the condyle. |
| Inclination of the articular eminence | A tangent line is drawn from the uppermost point of the glenoid fossa to the anterior inclination of the articular eminence. The angle between this line and a true horizontal line is the inclination of the articular eminence. |
| Height of the articular eminence | A tangent line is drawn from the uppermost point of the glenoid fossa. The perpendicular distance between the lowermost point of the articular eminence and the tangent line is the height of the articular eminence. |
| Superior joint space | Distance between the uppermost point of the condyle and the uppermost point of the glenoid fossa. |
| Anterior and posterior joint spaces | Two tangent lines are drawn from the most superior point of the articular cavity on the most prominent part of the anterior and posterior condylar surfaces. The shortest distances between these lines to the opposite glenoid fossa wall are the anterior and posterior joint spaces. |
Statistical analysis
All data were analyzed with SPSS ver. 18 (SPSS Inc., Chicago, IL, USA). The data of the left and right TMJs in the three groups were analyzed using the paired t-test. The statistical analysis was performed using the independent t-test to compare the differences among the three groups.
The condylar position was calculated by the following formula according to the method described by Pullinger et al.:13
where A is the anterior joint space and P is the posterior joint space.
At a ratio smaller than −12%, the condyle was considered to be in a posterior position. At a ratio greater than +12%, the condyle was considered to be in an anterior position. At a ratio within ±12%, the condylar position was considered concentric.
To avoid error, all images were remeasured by the same operator after 1 week. A P value of <0.05 was considered statistically significant.
Results
A total of 60 high-resolution CBCT imaging sets of the TMJ were collected from 60 female patients aged 16 to 28 years (mean age, 22.46 ± 3.57 years). The patients were equally divided into a high-angle, low-angle, and control group of 20 patients each. All TMJ measurements in the three groups are summarized in Tables 2 and 3. Among the measurements revealing the condylar morphology, the mediolateral and anteroposterior diameters of the condyle were longest in the low-angle group and shortest in the high-angle group (P < 0.05). The height of the condylar head was lowest in the low-angle group (P < 0.05), whereas no statistically significant difference was observed between the high-angle and control groups. The width of the condylar head was significantly different only between the high-angle and low-angle groups (P < 0.05). No significant differences were detected in the length of the condyle, the width of the glenoid fossa, or the height of the articular eminence among the three groups. The depth of the glenoid fossa was significantly smaller in the high-angle group than in the control and low-angle groups (P < 0.05). The inclination of the articular eminence was highest in the low-angle group and lowest in the high-angle group (P < 0.05). The posterior joint space was significantly different among the three groups (highest in the high-angle group and lowest in the low-angle group) (P < 0.05). The superior joint space was significantly lower in the high-angle group than in the control and low-angle groups (P < 0.05). The anterior joint space was significantly greater in the low-angle group than in the control and high-angle groups (P < 0.05).
Table 2.
Temporomandibular joint measurements in the three groups.
| Variable | Groups | n | Mean ± SD |
|---|---|---|---|
| Mediolateral diameter of condyle, mm | High-angle | 40 | 16.89 ± 0.79 |
| Control | 40 | 18.18 ± 1.12 | |
| Low-angle | 40 | 19.03 ± 0.73 | |
| Anteroposterior diameter of condyle, mm | High-angle | 40 | 7.18 ± 0.73 |
| Control | 40 | 8.13 ± 0.34 | |
| Low-angle | 40 | 8.97 ± 0.57 | |
| Width of glenoid fossa, mm | High-angle | 40 | 18.43 ± 0.98 |
| Control | 40 | 18.03 ± 1.18 | |
| Low-angle | 40 | 17.89 ± 1.23 | |
| Depth of glenoid fossa, mm | High-angle | 40 | 7.28 ± 0.88 |
| Control | 40 | 7.98 ± 1.13 | |
| Low-angle | 40 | 8.08 ± 0.93 | |
| Width of condylar head, mm | High-angle | 40 | 6.78 ± 1.01 |
| Control | 40 | 6.98 ± 0.93 | |
| Low-angle | 40 | 7.33 ± 0.78 | |
| Height of condylar head, mm | High-angle | 40 | 4.01 ± 0.47 |
| Control | 40 | 3.89 ± 0.74 | |
| Low-angle | 40 | 3.25 ± 0.66 | |
| Length of condyle, mm | High-angle | 40 | 25.58 ± 2.38 |
| Control | 40 | 25.45 ± 2.11 | |
| Low-angle | 40 | 25.66 ± 1.97 | |
| Height of articular eminence, mm | High-angle | 40 | 6.13 ± 1.00 |
| Control | 40 | 6.15 ± 0.59 | |
| Low-angle | 40 | 6.24 ± 0.69 | |
| Superior joint space, mm | High-angle | 40 | 2.38 ± 0.21 |
| Control | 40 | 2.97 ± 0.18 | |
| Low-angle | 40 | 2.91 ± 0.43 | |
| Anterior joint space, mm | High-angle | 40 | 1.88 ± 0.19 |
| Control | 40 | 1.84 ± 0.31 | |
| Low-angle | 40 | 2.51 ± 0.27 | |
| Posterior joint space, mm | High-angle | 40 | 2.45 ± 0.57 |
| Control | 40 | 2.07 ± 0.26 | |
| Low-angle | 40 | 1.73 ± 0.17 | |
| Inclination of the articular eminence, degrees | High-angle | 40 | 40.18 ± 6.51 |
| Control | 40 | 45.21 ± 5.77 | |
| Low-angle | 40 | 51.03 ± 7.01 |
SD, standard deviation.
Table 3.
Comparison of measurements among the three groups with independent t-test.
| Variable |
P value |
||
|---|---|---|---|
| High-angle vs. Control | High-angle vs. Low-angle | Control vs. Low-angle | |
| Mediolateral diameter of condyle | 0.000 | 0.000 | 0.000 |
| Anteroposterior diameter of condyle | 0.000 | 0.000 | 0.000 |
| Width of glenoid fossa | 0.260 | 0.089 | 0.846 |
| Depth of glenoid fossa | 0.005 | 0.001 | 0.893 |
| Width of condylar head | 0.590 | 0.022 | 0.203 |
| Height of condylar head | 0.675 | 0.000 | 0.000 |
| Length of condyle | 0.961 | 0.985 | 0.901 |
| Inclination of articular eminence | 0.002 | 0.000 | 0.000 |
| Height of articular eminence | 0.993 | 0.804 | 0.864 |
| Superior joint space | 0.000 | 0.000 | 0.634 |
| Anterior joint space | 0.773 | 0.000 | 0.000 |
| Posterior joint space | 0.000 | 0.000 | 0.000 |
The distribution of the condylar position in the high-angle, low-angle, and control groups is summarized in Table 4. As shown in the table, the anterior (42.5%) and concentric (45.0%) condylar positions were significantly more prevalent in the high-angle group, the concentric (75.0%) condylar position was significantly more prevalent in the control group, and the posterior (50.0%) and concentric (32.5%) condylar positions were significantly more prevalent in the low-angle group.
Table 4.
Distribution of condylar position in the three groups.
| Groups |
Condylar position |
||
|---|---|---|---|
| Posterior | Concentric | Anterior | |
| High-angle | 5 (12.5%) | 18 (45.0%) | 17 (42.5%) |
| Control | 3 (7.5%) | 30 (75.0%) | 7 (17.5%) |
| Low-angle | 20 (50.0%) | 13 (32.5%) | 7 (17.5%) |
Discussion
In the present study, CBCT images were collected to obtain measurements of the condyle–fossa. The anatomical structure of the TMJ is complex; thus, clinical examinations cannot precisely reveal its internal environment. Taking this obstacle into account, various radiographic methods have been used in previous studies to examine the TMJ morphology, such as CT magnetic resonance imaging (MRI), conventional/plain CT, plain film radiography, and CBCT. Conventional two-dimensional projections of the TMJ cannot show its three-dimensional shape accurately and thus have limited clinical utility. MRI is considered the gold standard diagnostic method for TMDs. Many cases of disc displacement without reduction develop from disc displacement with reduction. Such patients often have a history of joint clicking, limitation of mouth opening, and pain. All participants in the present study were investigated through a case history inquiry to exclude those with disc displacement without reduction. However, we were unable to use MRI for all participants in this study because of the limitations of the research conditions. CBCT is a new imaging method for the diagnosis of TMDs. Nakajima et al.14 found that CBCT can provide a three-dimensional image of the TMJ in which the bone structure can be clearly observed. Additionally, Lascala et al.15 evaluated the accuracy of TMJ measurements using CBCT and concluded that CBCT images have high reliability, repeatability, and accuracy. CBCT has obvious advantages in terms of its high space resolution, low radiation dose, and clear display of the bone trabecular structure of the condyle.
In some studies, age- and sex-related differences were found in the bone structure of TMJs.16 Ribeiro-Dasilva et al.17 suggested that female patients were at higher risk of developing TMDs than male patients. Thus, selection of female patients as study participants is very representative. Severt and Proffit18 and Haraguchi et al.19 found that some patients with malocclusion p had craniofacial asymmetry. However, the present study showed no significant differences in any TMJ measurements between the left and right sides among the three groups. Because the participants were females with facial symmetry and an age of 16 to 28 years, the effects of the facial form, sex, and age on the joint abnormalities were eliminated.
Kurita et al.20 found that both the mediolateral and anteroposterior diameters of the condyle were decreased mainly in patients with disc displacement. Gomes et al.21 reported that the size of the condyle in patients with OA was clearly decreased in the presence of pathological changes in the bone. Thus, the mediolateral and anteroposterior diameters of the condyle may be important factors in TMDs. In the present study, measurement of the mediolateral diameter of the condyle, anteroposterior diameter of the condyle, height of the condylar head, and width of the condylar head showed that the condylar head was narrow and long in the high-angle group but wide and short in the low-angle group. Such changes are associated with bone density, masticatory muscle strength, condylar stress, and adaptive remodeling. We assumed that the patients in the low-angle group had larger masticatory muscles and greater masticatory force that contributed to the adaptive reconstruction of the condyle. Arnett and Gunson22 suggested that a larger condyle is associated with more stable masticatory function. The degree of matching between the condyle and fossa would be better, contributing to greater stability of the condyle. Different concepts concerning the depth and width of the glenoid fossa have been proposed. For instance, Alkhader et al.23 speculated that the width of the glenoid fossa decreased because of changes in the bone. In another study, however, the opposite opinion was expressed (i.e., that the depth and width of the glenoid fossa were higher in patients with TMDs than in asymptomatic individuals) as established through comparison of the joint form between the TMD group and control group.24 In the present study, the depth of the glenoid fossa was significantly smaller in the high-angle group than in the control group and low-angle group. The risk of TMD is likely higher in the high-angle group than in the other groups because of the depth of the glenoid fossa. Earlier reports provided evidence that a high inclination of the articular eminence might be a pathogenic factor for TMD,25 which is contrary to the findings obtained by Sümbüllü et al.26 and Ren et al.27 The inclination of the articular eminence was highest in the low-angle group and lowest in the high-angle group. This indicates that the glenoid fossa was low and flat in the high-angle group but high and steep in the low-angle group. Some authors have reported that most patients with skeletal class II malocclusion with a low angle have a deep overbite and require a greater occlusal dimension when opening the mouth, which contributes to excessive development of the articular eminence.28 In addition, the glenoid fossa of patients with a low angle has undergone adaptive reconstruction because the masticatory force must match the more sturdy condyle. Paknahad and Shahidi29 reported that the condyles were more anteriorly positioned in patients with a high-angle vertical pattern than in those with a normal and low-angle vertical pattern. Moreover, Bjork30 found that the condyle of patients with a high angle often grew backward, which led to the occurrence of an anterior condylar position to some extent. The condyle often grew backward along with clockwise rotation of the mandible in patients with a high angle, which contributed to the tendency of the posterior condyle to rotate forward. The situation in patients with a low angle was the opposite, which is consistent with our results. In the control group, most condyles were in the concentric position, which is consistent with the findings reported by Madsen31 and Weinberg.32
Conclusions
In conclusion, the present study demonstrated some significant differences in the condyle–fossa morphology and position in female patients with skeletal class II malocclusion with different vertical facial types. We conclude that patients with skeletal class II malocclusion with a high angle have an unstable structure of the TMJ. We assume that the risk of TMDs in such patients is much higher than that in other people. The possible relationship between orthodontic treatment and TMDs is a topic of great research interest. Increasingly more investigations are being focused on this field. The present study will be helpful in the diagnosis of TMDs and provide orthodontic specialists with valuable clinical guidance.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The study was supported by the Nature Science Foundation of China (No. 81800944).
ORCID iD
References
- 1.Wu CK, Hsu JT, Shen YWet al. Assessments of inclinations of the mandibular fossa by computed tomography in an Asian population. Clin Oral Invest 2012; 16: 443–450. [DOI] [PubMed] [Google Scholar]
- 2.Lövblad KO, Essig M. Head and neck imaging. Eur Radio Suppl 2017; 35: 128. [Google Scholar]
- 3.Wang X, Zhang J, Gan Yet al. Current understanding of pathogenesis and treatment of TMJ osteoarthritis. J Dent Res 2015; 94: 666–673. [DOI] [PubMed] [Google Scholar]
- 4.Cevidanes LH, Hajati AK, Paniagua Bet al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 110: 110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinberg LA. Correlation of temporomandibular dysfunction with radiographic findings. J Prosthet Dent 1972; 28: 519–539. [DOI] [PubMed] [Google Scholar]
- 6.Kurusu A, Horiuchi M, Soma K. Relationship between occlusal force and mandibular condyle morphology. Angle Orthod 2009; 79: 1063–1069. [DOI] [PubMed] [Google Scholar]
- 7.Ishibashi H, Takenoshita Y, Ishibashi Ket al. Age-related changes in the human mandibular condyle: a morphologic, radiologic and histologic study. J Oral Maxillofac Surg 1995; 53: 1016–1023. [DOI] [PubMed] [Google Scholar]
- 8.Katsavrias EG, Halazonetis DJ. Condyle and fossa shape in Class II and Class III skeletal patterns: a morphometric tomographic study. Am J Orthod Dentofacial Orthop 2005; 128: 337–346. [DOI] [PubMed] [Google Scholar]
- 9.Park IY, Kim JH, Park YH. Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern. Korean J Orthod 2015; 45: 66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burke G, Major P, Glover Ket al. Correlations between condylar characteristics and facial morphology in Class II preadolescent patients. Am J Orthod Dentofacial Orthop 1998; 114: 328–336. [DOI] [PubMed] [Google Scholar]
- 11.Yasa Y, Akgul HM. Comparative cone-beam computed tomography evaluation of the osseous morphology of the temporomandibular joint in temporomandibular dysfunction patients and asymptomatic individuals. Oral Radiol 2018; 34: 31–39. [DOI] [PubMed] [Google Scholar]
- 12.Ganugapanta VR, Ponnada SR, Gaddam KPet al. Computed tomographic evaluation of condylar symmetry and condyle-fossa relationship of the temporomandibular joint in subjects with normal occlusion and malocclusion: a comparative study. J Clin Diagn Res 2017; 11: zc29–zc33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pullinger AG, Hollender L, Solberg WKet al. A tomographic study of mandibular condyle position in an asymptomatic population. J Prosthet Dent 1985; 53: 706–713. [DOI] [PubMed] [Google Scholar]
- 14.Nakajima A, Sameshima GT, Arai Yet al. Two and three-dimensional orthodontic imaging using limited cone beam computed tomography. Angle Orthod 2005; 75: 895–903. [DOI] [PubMed] [Google Scholar]
- 15.Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography. Dentomaxillofac Radiol 2004; 33: 291–294. [DOI] [PubMed] [Google Scholar]
- 16.Scheffler C. Variable and invariable proportions in the ontogenesis of the human face. J Craniofac Surg 2013; 24: 237–241. [DOI] [PubMed] [Google Scholar]
- 17.Ribeiro-Dasilva MC, Fillingim RB, Wallet SM. Estrogen-Induced monocytic response correlates with TMD Pain: a case control study. J Dent Res 2017; 96: 285–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Severt TR, Proffit WR. The prevalence of facial asymmetry asymmetry in the dentofacial deformities population at the University of North Carolina. Int J Adult Orthodon Orthognath Surg 1997; 12: 171–176. [PubMed] [Google Scholar]
- 19.Haraguchi S, Takada K, Yasuda Y. Facial asymmetry in subjects with skeletal class III deformity. Angle Orthod 2002; 72: 28–35. [DOI] [PubMed] [Google Scholar]
- 20.Kurita H, Ohtsuka A, Kobayashi Het al. Alteration of the horizontal mandibular condyle size associated with temporomandibular joint internal derangement in adult females. Dentomaxillofac Radiol 2002; 31: 373–378. [DOI] [PubMed] [Google Scholar]
- 21.Gomes LR, Gomes M, Jung Bet al. Diagnostic index of three-dimensional osteoarthritic changes in temporomandibular joint condylar morphology. J Med Imaging (Bellingham) 2015; 2: 034501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arnett GW, Gunson MJ. Facial planning for orthodontists and oral surgeons. Am J Orthod Dentofacial Orthop 2004; 126: 290–295. [DOI] [PubMed] [Google Scholar]
- 23.Alkhader M, Al-sadhan R, Al-shawaf R. Cone-beam computed tomography findings of temporomandibular joints with osseous abnormalities. Oral Radiol 2012; 28: 82–86. [Google Scholar]
- 24.Paknahad M, Shahidi S, Akhlaghian Met al. Is mandibular fossa morphology and articular eminence inclination associated with temporomandibular dysfunction? J Dent (Shiraz) 2016; 17: 134–141. [PMC free article] [PubMed] [Google Scholar]
- 25.Sülün T, Cemgil T, Duc JMet al. Morphology of the mandibular fossa and inclination of the articular eminence in patients with internal derangement and in symptom-free volunteers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 98–107. [DOI] [PubMed] [Google Scholar]
- 26.Sümbüllü MA, Cağlayan F, Akgül HMet al. Radiological examination of the articular eminence morphology using cone beam CT. Dentomaxillofac Radiol 2012; 41: 234–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ren YF, Isberg A, Westesson PL. Steep of the articular eminence in the temporomandibular joint. Tomographic comparison between asymptomatic volunteers with normal disk position and patients with disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 80: 258–266. [DOI] [PubMed] [Google Scholar]
- 28.Anders C, Harzer W, Eckardt L. Axiographic evaluation of mandibular mobility in children with angle Class II malocclusion (deep overbite). J Orofac Orthop 2000; 61: 45–53. [DOI] [PubMed] [Google Scholar]
- 29.Paknahad M, Shahidi S. Association between condylar position and vertical skeletal craniofacial morphology: a cone beam computed tomography study. Int Orthod 2017; 15: 740–751. [DOI] [PubMed] [Google Scholar]
- 30.Bjork A. Variations in the growth pattern of the human mandible: longitudinal radiographic study by the implant method. J Dent Res 1963; 42: 400–411. [DOI] [PubMed] [Google Scholar]
- 31.Madsen B. Normal variations in anatomy, condylar movements and arthrosis frequency of the temporomandibular joints. Acta Radiol Diagn (Stockh) 1966; 4: 273–288. [DOI] [PubMed] [Google Scholar]
- 32.Weinberg LA. Role of condylar position in TMJ dysfunction-pain syndrome. J Prosthet Dent 1979; 41: 636–643. [DOI] [PubMed] [Google Scholar]