Abstract
The ongoing worldwide COVID-19 pandemic has become a huge threat to global public health. Using CT image, 3389 COVID-19 patients, 1593 community-acquired pneumonia (CAP) patients, and 1707 nonpneumonia subjects were included to explore the different patterns of lung and lung infection. We found that COVID-19 patients have a significant reduced lung volume with increased density and mass, and the infections tend to present as bilateral lower lobes. The findings provide imaging evidence to improve our understanding of COVID-19.
Keywords: COVID-19, Community-Acquired pneumonia, Non-Pneumonia subjects, Lung, Big data
The current outbreak of coronavirus disease-2019 (COVID-19) has become a serious global health crisis. Chest CT imaging, as a direct assessment tool for lung infection, shows that ground-glass opacity, increased crazy-paving pattern, and consolidation are the main signs of COVID-19 infections (Li and Xia, 2020). Clinicians observed that COVID-19 patients’ lungs become smaller and stiffer (Anon), and have a 20–30% decrease in lung volume. However, there are limited studies that have used big data to explore the overall alterations of lung volume, density, and mass as well as the distribution of infections that caused by the coronavirus.
For this retrospective study, we identified 3389 CT scans from COVID-19 patients, 1593 scans from community-acquired pneumonia (CAP) nonviral patients, and 1707 scans from nonpneumonia subjects. The ages of the participants ranged from 12 to 98 years. All the CT images were acquired with slice thickness less than 2 mm and were anonymized before analysis. Preprocessing steps included the segmentation of lung lobes and infection lesions using a VB-Net toolkit (Shan et al., 2020), which combines V-Net (Milletari et al., 2016) with bottleneck layers to reduce and integrate feature map channels and achieves a Dice coefficient of 0.92 when compared with manual delineations.
First, we evaluated the overall characteristics of volume, density, and mass in the lung and 5 lung lobes in the three groups. Two-sample z-tests were adopted for comparing the mean difference of two groups. Second, for the infected regions, the volume, density, and mass were also obtained from 5 lung lobes to investigate their distinct inflammation distributions between COVID-19 and CAP patients.
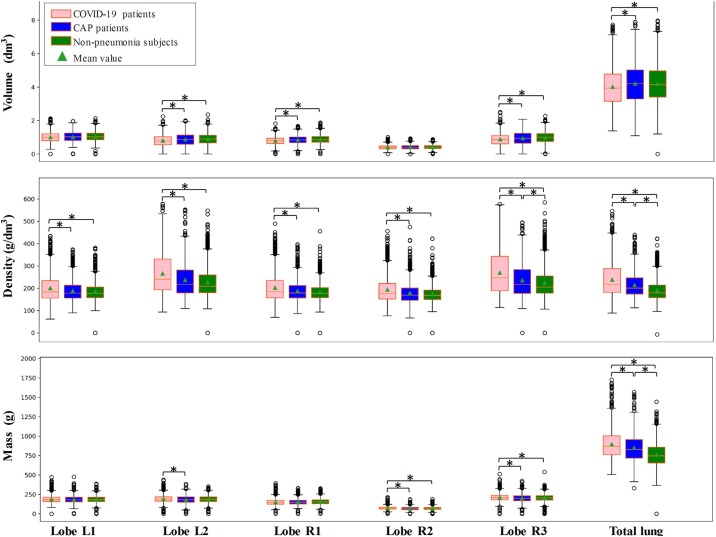
In the overall region analysis, lung volumes of COVID-19 patients are significantly smaller than those of CAP patients as well as nonpneumonia subjects. Lung densities of COVID-19 patients are larger than those of CAP patients, and those of nonpneumonia subjects are the smallest. The mass has a similar pattern with the density. In the lung lobe analysis, COVID-19 patients’ lung volumes are significantly smaller than the other two groups in L2, R1, and R3, while the lung densities are larger in all lung lobes. The mass of L2, R2, and R3 is higher in COVID-19. CAP patients are found with higher density of R3 (Figure 1). In line with a previous study where different degrees of alveolar collapse were found in 6 COVID-19 patients (Iwasawa et al., 2020), our findings indicate that COVID-19 is generally accompanied by reduced volume of the lung and lung lobes, with increased density and mass. The pattern of CAP is similar with nonpneumonia subjects, except that the density of CAP patients is relatively larger. This distinct distribution could be further utilized for differentiate diagnosis.
Figure 1.
Boxplot of volume, density, and mass of lung lobes and whole lung among coronavirus disease-2019 (COVID-19) (pink), community-acquired pneumonia (CAP) (blue), and nonpneumonia (green) subjects, respectively. Density is defined as the mean CT HU value of the region of interest plus an offset of 1000. Mass is calculated as the volume multiplied by density. *indicates that significant difference is found between the two groups (p < 0.05, corrected for multiple comparisons). L: left and R: right.
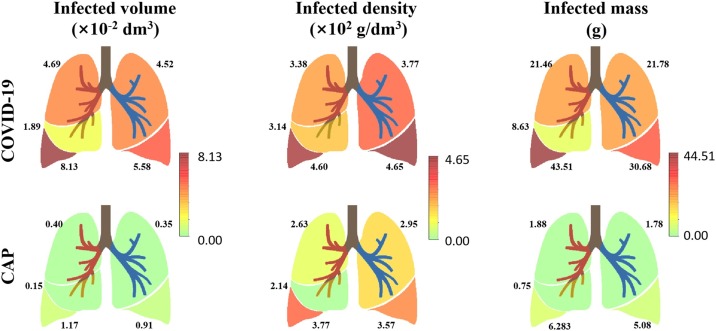
In the infected region analysis, the infection volumes of the lower lobes are more severe (COVID-19: right/left, 0.08/0.06 dm3 and CAP: right/left, 0.01/0.01 dm3), while the infection volume of the right middle lobe is relatively mild (COVID-19: 0.02 dm3 and CAP: 0.00 dm3). Regarding density, it appears that CAP patients also have increased density in the left and right lower lobes, while COVID-19 shows high density in all the five lobes. The pattern of mass is similar to that of the volume (Figure 2 ). These findings revealed that the typical pattern of infection in COVID-19 and CAP patients is bilateral and involves multiple lobes. Compared to the middle and upper lobes, lower lobes are more affected, with slight predominance in the right lower lobe. These findings might because that the cells targeted by the coronavirus are mainly located in the bilateral lower lobe bronchus. As the right bronchus is short and straight, the virus might tend to favor this location, which agrees with previous reports (Huang et al., 2020, Shi et al., 2020). Additionally, the volume, density, and mass patterns of COVID-19 are overall larger than those of CAP patients, which supports that COVID-19 patients have more severe pneumonia effects, and the relatively larger density distribution of COVID-19 might suggest that the manifestations of COVID-19 pneumonia could be more diverse.
Figure 2.
Illustration of infected distributions of the volume, density, and mass in lung lobes for coronavirus disease-2019 (COVID-19) and community-acquired pneumonia (CAP).
The present study has some limitations. Severity information and longitudinal follow-ups may allow the further exploration of the lung progresses in pneumonia patients. CAP can also be caused by different pathogens such as bacteria, fungi, parasites, or viruses. Viral infection was reported with more similar patterns as compared to COVID-19 pneumonia (Bai et al., 2020). Future studies could investigate the image patterns of CAP subtypes as well as with COVID-19.
In summary, by using a massive dataset, we observed reduced lung volume and increased density and mass in COVID-19 patients as compared to CAP patients and nonpneumonia subjects. In addition, pneumonia including COVID-19 tends to present as bilateral with a slight predominance in the right lower lobe, while there exists distinct infection distribution and severity between COVID-19 and CAP patients. We hope that our findings could provide imaging evidence in delineating lung abnormalities in pneumonia patients and would likely improve the understanding of the radiological underpinning of COVID-19.
Author contributions
F. Shi and D. Shen contributed to the study concept and design. L. Xia, F. Shan, Z. Mo and F. Yan contributed to the acquisition of data and statistical analysis. F. Shi and Y. Wei contributed to the analysis, interpretation of data, and drafting of the manuscript. All authors read and approved the final manuscript.
Conflict of interest
F.S., Y.W., and D.S. are employees of Shanghai United Imaging Intelligence, Shanghai, China. The company has no role in designing and performing the surveillances and analyzing and interpreting the data. All other authors report no conflicts of interest relevant to this article.
Funding source
This work was supported in part by the National Key Research and Development Program of China under Grant 2018YFC0116400.
Ethical approval
The study was approved by the Ethics Committee of Tongji Hospital of Huazhong University of Science and Technology, Shanghai Public Health Clinical Center of Fudan University, China-Japan Union Hospital of Jilin University, Ruijin Hospital of Shanghai Jiao Tong University School of Medicine.
Acknowledgments
None.
References
- People recovered from covid-19 can lose 20 to 30% of their lung function, doctors said. Available: https://www.novinite.com/articles/203609/.
- Bai H.X., Hsieh B., Xiong Z., Halsey K., Choi J.W., Tran T.M.L. Performance of Radiologists in Differentiating COVID-19 from Non-COVID-19 Viral Pneumonia at Chest CT. Radiology. 2020;296(2):E46–E54. doi: 10.1148/radiol.2020200823. Epub 2020/03/11. PubMed PMID: 32155105; PubMed Central PMCID: PMCPMC7233414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. PubMed PMID: 31986264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwasawa T., Sato M., Yamaya T., Sato Y., Uchida Y., Kitamura H. Ultra-high-resolution computed tomography can demonstrate alveolar collapse in novel coronavirus (COVID-19) pneumonia. Jpn J Radiol. 2020;38(5):394–398. doi: 10.1007/s11604-020-00956-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Xia L. Coronavirus disease 2019 (COVID-19): Role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020:1–7. doi: 10.2214/AJR.20.22954. PubMed PMID: 32130038. [DOI] [PubMed] [Google Scholar]
- Milletari F., Navab N., Ahmadi S.-A., editors. V-net: Fully convolutional neural networks for volumetric medical image segmentation. Fourth International Conference on 3D Vision (3DV); 2016: IEEE; 2016. [Google Scholar]
- Shan F., Gao Y., Wang J., Shi W., Shi N., Han M. Lung infection quantification of COVID-19 in CT images with deep learning. arXiv preprint arXiv: 200304655. 2020 [Google Scholar]
- Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]