Abstract
Background
The frequency of asymptomatic SARS-CoV-2 infection with viral spread is unclear. Asymptomatic SARS-CoV-2 infection development and progression was investigated in subjects undergoing mandatory quarantine on airport arrival.
Methods
2714 subjects were tested for SARS-CoV-2 and all were quarantined for 2 weeks. Viral retesting was undertaken on symptom development and routinely at 14 days if asymptomatic. Asymptomatic, positive patients underwent viral testing every 2 days to determine viral clearance.
Results
188/2714 (6.9%) patients became SARS-CoV-2 positive. On arrival, 136/188 tested positive, with 44/188 (23.4%) symptomatic and 92/188 (48.9%) asymptomatic. All 92 patients remained asymptomatic and were retested every 2 days until viral clearance. 2526 quarantined subjects remained virus free at 14 days. Viral clearance did not differ between symptomatic and asymptomatic patients (12.6 ± 1.0 days and 12.1 ± 0.4 days, respectively). Of the 52/188 (27.7%) testing negative on arrival, 27/52 subsequently became positive and developed symptoms 2–13 days after arrival. 25/188 (13.3%) remained asymptomatic and tested positive at day 14, with viral testing undertaken every 2 days in these subjects; of these, 24 remained asymptomatic, with viral clearance at 9.4 ± 0.7 days — less than for those who were asymptomatic on arrival (p < 0.002).
Conclusion
Asymptomatic patients with COVID-19 were more prevalent than those exhibiting symptoms, and are an infection reservoir.
Keywords: COVID-19, SARS-CoV-2, Symptoms, Screening
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the newly identified severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Rothan and Byrareddy, 2020). Whilst some patients may have mild symptoms, others develop a severe respiratory distress syndrome with features of a blood coagulopathy, requiring intensive support (Fogarty et al., 2020) and resulting in a severe healthcare burden (Carenzo et al., 2020). Mass testing helps to identify and isolate cases, and allows tracing of their contacts, which are all vital for limiting the spread of the coronavirus (Hellewell et al., 2020). The median COVID-19 incubation period is estimated at 5.1–6.4 days (Backer et al., 2020, Lauer et al., 2020). It has been estimated that 30–40% of all COVID-19 infections may be asymptomatic within a 14 day period (Oran and Topol, 2020), with higher estimates being suggested elsewhere (Nishiura et al., 2020). In one study of a cruise-ship outbreak (Mizumoto et al., 2020) it was estimated that 81% of those with COVID-19 may have been be asymptomatic. The Center for Disease Control and Prevention estimates that 35% of COVID-19 cases are asymptomatic, and that 40% of transmission occurs before symptom onset (CDC, 2020). Following the SARS-CoV-2 infection of a healthcare worker, contact screening identified that 56% of those testing positive for SARS-CoV-2 were asymptomatic (Arons et al., 2020). Clearly, these asymptomatic cases may act as a reservoir and are critical to the community spread of the virus.
All travelers arriving through Bahrain International Airport from highly endemic areas were tested on arrival by quantitative real-time reverse transcription polymerase chain reaction (RT-PCR), using extracted RNA. Those testing negative underwent mandatory quarantine for a 14-day period, allowing a prospective analysis of those who were initially asymptomatic and negative becoming subsequently positive, and their outcome, within a regulated environment.
Methods
The Kingdom of Bahrain implemented a policy that all travelers arriving through Bahrain International Airport undergo nasopharyngeal RT-PCR testing in the airport clinic. A total of 2714 travellers entered Bahrain within the defined period of 18 days from February 25 to March 14, 2020. Those who tested positive were transferred to hospital facilities, while those who were negative were quarantined for a 14-day period, with further testing on development of any symptoms of cough, fever, or sore throat. At the end of the 14-day period each subject was tested again by RT-PCR, and if negative was discharged from quarantine. Those who remained asymptomatic but tested positive at 14 days on routine testing were transferred to a dedicated isolation facility, and viral testing was undertaken every 2 days until viral clearance occurred, defined as two RT-PCR negative tests 24 h apart.
The real time RT-PCR diagnostic test used for SARS-CoV-2 followed a protocol from Charité Virology, Berlin, Germany. PCR was performed on nasopharyngeal samples. All samples were tested for the E gene and positive samples were confirmed after being tested for the N and RdRp genes (from TIB Molbiol) (Corman et al., 2020).
The study was approved by the National Covid-19 Taskforce Ethics Committee, number CRT−COVID2020−064.
Quarantine policy and facility
All travelers who arrived during the study period and tested negative on arrival were quarantined. Those who arrived from high-risk countries, based on the risk assessment (which included China, Iran, Iraq, and South Korea), were quarantined at a dedicated facility due to the high prevalence of COVID-19 noted within these groups. The quarantine facility is made up of eight large, multistorey buildings, a large outdoor area, and a medical clinic. The facility can hold up to 492 people, with adequate distancing. Buildings were assigned to males, females, and families.
The facility has separate, single-occupancy rooms with dedicated washing and toilet facilities, and was under the operation of a licensed and well-trained medical team, who were aware of the principal precautionary measures required for suspected COVID-19 cases. The medical team included physicians and nursing staff, who were available 24/7 via 8 -h shifts. Basic necessary medical equipment was provided at the facilities, including blood-pressure monitors, thermometers, swabs, medication, and a cardiopulmonary resuscitation cart. The facility had security staff for the supervision of subjects, who ensured that quarantined patients could not leave the facility and that they followed the facility’s visiting policies. Staff entered a dedicated cubicle to change and put on PPE, using a different cubicle to remove potentially contaminated PPE. All staff had access to the necessary resources, such as PPE, and regular, active monitoring of the medical team was undertaken for the absence/presence of symptoms.
On arrival, all quarantined individuals were informed and instructed about the aim and duration of quarantine. The medical team explained the necessity of compliance to the infection control measures. All admissions to the facilities were documented through electronic medical records, and medical rounds were conducted on daily basis to check for symptoms. If a person developed symptoms, following a medical assessment the patient was swabbed, isolated, and transferred out to a COVID-19 treatment facility.
The quarantined individuals were given the option to cohort as families within a building (using different rooms), or be segregated by gender. Children could stay with their mothers, with beds separated by 2 m. Food, snacks, face masks, and gloves were provided on a daily basis. Subjects were given colour-coded bracelets for identification. Frequent cleaning of the facility was undertaken, and all rooms were disinfected following the discharge of any person, as per national public health department instructions, using disposable equipment. Visiting by families was allowed in a dedicated outdoor area, with strict protective measures being implemented.
Statistical analysis
Data trends were visually and statistically evaluated for normality. Non-parametric tests (Mann–Whitney U and Kruskal–Wallis tests) were applied to data that contravened the assumptions of normality when tested using the Kolmogorov-Smirnov test. Statistical analysis was performed using the Stata statistical computer package (StataCorp, 2013).
Results
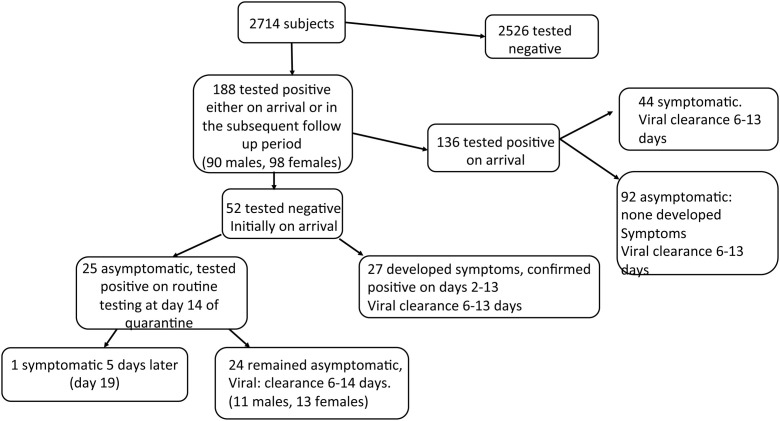
The progression of patients developing SAR-CoV-2 positivity is shown in Figure 1. No subject reported contact with a known positive COVID-19 case. Of the 2714 subjects returning to Bahrain by air from Iran or Egypt, a total of 188 (6.9%; 90 male and 98 female) eventually became SARS-CoV-2 positive, either on immediate testing in the airport or on subsequent testing in the quarantine facility. All of the other 2526 subjects quarantined produced a negative RT-PCR test at 14 days, indicating that they were not infected.
Figure 1.
SARS-CoV-2 detection and subsequent quarantine of 2714 travellers arriving in Bahrain Airport over an 18-day period, showing those who initially tested positive, and those who were subsequently found to be positive, with viral clearance for each group.
Of the 188 who tested positive, 44 (23.4%; 16 male and 28 female) were symptomatic on arrival, three of whom (2 females and 1 male) subsequently deteriorated and died on ventilatory support.
144/188 (76.6%; 41 male and 103 females) were asymptomatic on arrival. Of these, 92/188 (48.9%) tested positive on arrival and were transferred to hospital care: all 92 patients remained asymptomatic until viral clearance. All subjects who tested positive were retested every 2 days until viral clearance was achieved.
The 52/188 (27.7%) who tested negative on arrival were transferred to quarantine, as detailed; 27/52 subsequently developed symptoms and were confirmed positive by RT PCR (number of subjects and days to symptoms: six on day 2, four on day 3, two on day 4, one on day 5, five on day 6, one on day 7, five on day 12, and three on day 13). 25/188 (13.3%) remained asymptomatic but tested positive on day 14; viral testing was undertaken every 2 days in these subjects. 1/25 became symptomatic on day 5, while 24/25 (12.8% of the 188; 11 male and 13 female) remained asymptomatic with viral clearance (two negative tests 24 h apart) between 6 and 14 days after their initial positive testing (subjects and days to viral clearance: nine on day 6, one on day 7, two on day 8, three on day 9, one on day 11, five on day 12, and three on day 14). When divided into deciles, of the 24 asymptomatic patients, eight were 60 years and above, eight were aged 50–59 years, three 40–49 years, and five 20–29 years.
Time to viral clearance for those detected as positive on arrival was 12.6 ± 1.0 days for symptomatic and 12.1 ± 0.4 days for asymptomatic (p = ns). Those who remained asymptomatic, but who tested positive at 14 days had a shorter time to viral clearance (9.4 ± 0.7 days) compared with those who were asymptomatic on arrival (p < 0.002).
Discussion
These data show that in a large cohort of at-risk subjects for COVID-19, all of whom were monitored closely, the majority of those who were or subsequently became positive were asymptomatic and remained asymptomatic until viral clearance. Only a minority of subjects (23%) with SARS-CoV-2 infection were symptomatic, and would have likely been picked up by temperature scanning at the airport. Of those who were asymptomatic and infected, onsite RT-PCR screening picked up an additional 49% of the infections; however, 28% would not have been picked up even if tested after 48 h. Of particular concern are the 13% who remained asymptomatic and were only picked up with routine 14-day viral testing at the end of quarantine, and who remained asymptomatic until viral clearance up to 14 days later, a full 28 days post-arrival. There are few reports on how transmission can occur with these silent transmitters; there is evidence that asymptomatic patients are infectious (Zou et al., 2020), and therefore these subjects would be a reservoir of infectivity.
It remains possible, though unlikely, that some subjects picked up the infection from being at the facility itself, as it is difficult to expect complete compliance with self-isolation for 14 days. Even if that were the case, it is still clear that the infections were transmitted from asymptomatic subjects, because all symptomatic patients were isolated and transferred.
The proportion of asymptomatic COVID-19 patients reported here is greater than those estimated by other studies, where they range from 17.9% to 35% (Nishiura et al., 2020, Mizumoto et al., 2020, CDC, 2020), and not dissimilar to that reported in the cruise-ship outbreak (Mizumoto et al., 2020). However, this population was under direct observation throughout the quarantine period — in isolation facilities — and ours is therefore likely to be a more accurate determination than previous estimates.
A limitation of our study was that those who were asymptomatic for COVID-19 and were identified as positive for SARS-C0V-2 on day 14 may have become positive any time within that time frame, because regular testing was not carried out unless the individual became symptomatic. There was also the concern that individuals may have been infected whilst they were in quarantine, but this was unlikely in this closely monitored facility, as detailed above. While this study was carried out early in the pandemic, when test-based strategies (sequential PCR testing) were used to determine when infection control precautions could be lifted, it is important to acknowledge that approaches have now switched predominantly to non-test-based strategies.
In conclusion, asymptomatic patients with SARS-CoV-2 infection were found to be positive 14 days after initial testing, and remained asymptomatic until viral clearance. Asymptomatic patients with COVID-19 were more prevalent than those exhibiting symptoms, and are an infection risk requiring detection through multiple testing.
Conflicts of interest
The authors have declared that no conflicts of interest exist.
Ethical approval and consent to participate
The study was approved by the National Covid-19 Ethics Committee.
Consent for publication
All authors gave their consent for publication.
Availability of data and materials
All the data for this study will be made available upon reasonable request to the corresponding author.
Funding
No funding was received to perform this study.
Author contributions
AA and SLA analyzed the data and wrote the manuscript. AA and SAA performed data collection; ASA and SO interpreted data and edited the manuscript. MA supervised data collection and data analysis, and edited the manuscript. All authors reviewed and approved the final version of the manuscript.
Manaf Alqahtani is the guarantor of this work.
References
- Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020;382(22):2081–2090. doi: 10.1056/NEJMoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backer J.A., Klinkenberg D., Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Euro Surveill. 2020;25(5) doi: 10.2807/1560-7917.ES.2020.25.5.2000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carenzo L., Costantini E., Greco M., Barra F.L., Rendiniello V., Mainetti M. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020 doi: 10.1111/anae.15072. [DOI] [PubMed] [Google Scholar]
- CDC . 2020. Pandemic Planning Scenarios.https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html [23 June 2020]. Available from: [Google Scholar]
- Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogarty H., Townsend L., Ni Cheallaigh C., Bergin C., Martin-Loeches I., Browne P. COVID-19 coagulopathy in caucasian patients. Br Haematol. 2020 doi: 10.1111/bjh.16791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Global Health. 2020;8(4):e488–96. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172(9):577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10) doi: 10.2807/1560-7917.ES.2020.25.10.2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishiura H., Kobayashi T., Miyama T., Suzuki A., Jung S.M., Hayashi K. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oran D.P., Topol E.J. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020 doi: 10.7326/M20-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmunity. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data for this study will be made available upon reasonable request to the corresponding author.