Description
A 34 year-old man presented at a remote primary centre of our hospital and was attended by a junior surgeon under training. He complained of sudden onset loss of vision in his left eye, which was painless in nature. On examination the visual acuity was found to be 6/6 in the right eye, whereas it was 1/60 in left eye. The pupillary reflexes were found to be brisk in both eyes. On mydriatic fundus examination, a subretinal cyst was observed in the macular area of left eye. Undulating movements were noted in the cyst wall whenever its locale was illuminated. An Android operating system-based smartphone (OnePlus 6 T) was used to capture the image of the cyst (figure 1A), as well as a short video of its movements using an indirect ophthalmoscope and a 20D lens (video 1). The images and the video were then communicated to the base hospital, where subretinal cysticercosis (SRC) was diagnosed empirically and the patient was advised urgent surgery and head imaging. Later evaluation was completed at the base hospital, where ultrasonography of the lesion confirmed SRC with scolex (figure 1B) and optical coherence tomography (OCT) imaging too revealed features of SRC described earlier (figure 1C). A pars plana vitrectomy procedure with in vivo cyst lysis1 was done to remove the SRC.
Figure 1.
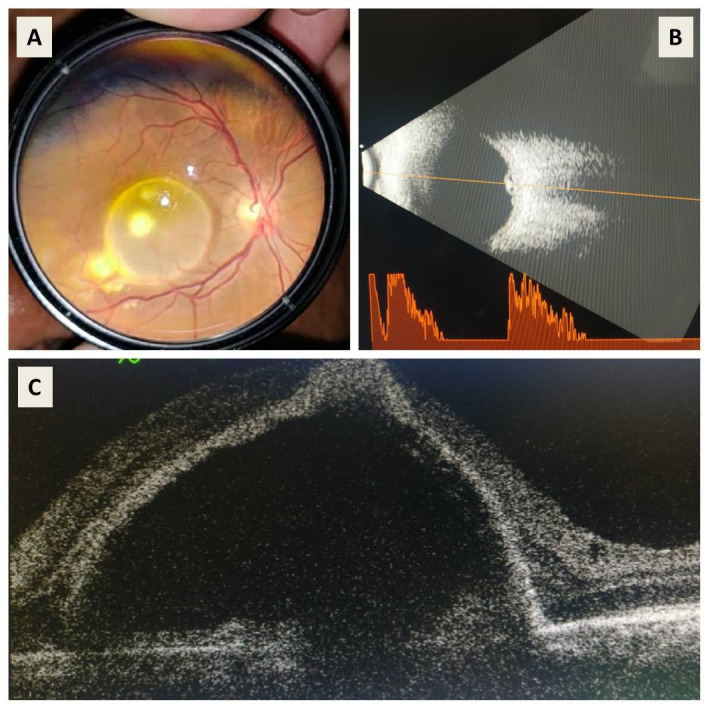
(A) Clinical photograph captured using smartphone and 20D lens by placing the 20D lens coaxial to the smartphone camera lens. A cyst is noticeable in the macular area. (B) Sonography image of the cyst with scolex. High spikes can be seen corresponding to the cyst on the accompanying vector scan. (C) Macular optical coherence tomography line scan taken through the cyst. The cyst is present in the subretinal space, and the scolex can be seen to cast an optical shadow on the underlying structures.
Video 1.
Cysticercosis is an infection with the larval stage of the parasite and is mainly seen in low-income countries. Human beings acquire cysticercosis through faecal–oral contamination. It is thus found in areas with poor sanitation and is endemic in Southeast Asia, Indian subcontinent, Mexico, South America and sub-Saharan Africa.2 The diagnosis is chiefly clinical but requires highly trained retinal surgeons as the disease is rare. Ultrasound, OCT and CT are assistive but are not easily available in remote areas, specifically where this zoonosis is endemic. Thus, diagnosis can be extremely challenging for an untrained ophthalmologist without access to these investigations. Untreated intraocular cysticercosis or a delay in its treatment incites severe ocular inflammation, more so when the cyst is dying due to antigenic release. Hence, urgent surgery is advocated after ruling out intracranial involvement.
In this era of technological advancements and innovations, the development of cheap tools can decrease dependency on expensive equipment. In this context, smartphones have shown promising results and may play a greater role as potential aid for future ophthalmic examination and monitoring purposes.3 The procedure of imaging employed by the primary ophthalmologist was very simple and involved placement of a 20D lens coaxial to the smartphone camera lens. The clinical photograph was then taken with flash on through the dilated pupil. The video was acquired similarly using illumination of the indirect ophthalmoscope. Such smartphone assisted imaging hastened the diagnosis and the management of the patient and proved to be a cheap way of telemedicine in this case. Telemedicine has assumed a very important role, and this is increasingly being realised in the current viral pandemic. Judicious use of teleophthalmology will go far in reducing undue exposures while also allowing timely referrals at the same time.
Learning points.
Intraocular cysticercus is a rare condition which should be kept as a differential in patients presenting with subretinal cystic lesions in endemic areas.
Smartphone-based telemedicine can be used as an affordable modality to aid in diagnosis and monitoring of various ophthalmic conditions in underserved populations.
The use of telemedicine should be encouraged especially during the COVID-19 pandemic as it can aid in providing valuable clinical information without increasing the risk of exposure to the virus.
Footnotes
Contributors: AS, BT, and NG contributed to diagnosis, workup, writing the manuscript. RD contributed to performing critical revision. NG holds the overall responsibility to the presentation and contributed to diagnosis and performing a critical revision of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Azad S, Takkar B, Roy S, et al. Pars plana vitrectomy with in vivo cyst lysis for intraocular cysticercosis. Ophthalmic Surg Lasers Imaging Retina 2016;47:665–9. 10.3928/23258160-20160707-09 [DOI] [PubMed] [Google Scholar]
- 2.Winkler AS. Neurocysticercosis in sub-Saharan Africa: a review of prevalence, clinical characteristics, diagnosis, and management. Pathog Glob Health 2012;106:261–74. 10.1179/2047773212Y.0000000047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lord RK, Shah VA, San Filippo AN, et al. Novel uses of smartphones in ophthalmology. Ophthalmology 2010;117:1274–1274.e3. 10.1016/j.ophtha.2010.01.001 [DOI] [PubMed] [Google Scholar]


