Abstract
Background:
Several studies have examined the anterior cruciate ligament (ACL) injury history among relatives of patients undergoing ACL reconstruction (ACLR), but they have primarily analyzed adults with variable results.
Hypothesis:
We hypothesized that he rate of familial ACL injuries among pediatric patients with ACL tears would be greater than that among pediatric patients with uninjured knees.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Pediatric patients (≤18 years of age) who underwent ACLR between January 2009 and May 2016 were contacted to complete a questionnaire on subsequent complications and family history of ACL tears. A control cohort was recruited from children with uninjured knees seen in the concussion clinic of our institution. Binary logistic regression was used to determine the factors predictive of having a familial ACL tear history or complications.
Results:
Overall, 450 pediatric patients with primary ACL tears were included. Age at the time of surgery was 14.9 ± 2.2 years with a follow-up of 4.3 ± 2.1 years. When compared with 267 control patients, those with an ACL tear reported a higher rate of first-degree relatives with an ACL injury history (25.1% vs 12.0%; P < .001). In multivariate analysis, children with ACL injury had nearly 3 times (odds ratio [OR], 2.7) higher odds of having a first-degree relative with an ACL tear (95% CI, 1.7-4.2; P < .001). Patients were stratified by the number of first-degree relatives with ACL tears: no relatives, 1 relative, or ≥2 relatives. Children with ≥2 first-degree relatives were more likely to sustain a postoperative graft failure (OR, 5.1; 95% CI 1.7-15.2; P = .003) or a complication requiring surgical intervention (OR, 7.5; 95% CI, 2.6-22.0; P < .001).
Conclusion:
A family history of ACL injury is more likely in pediatric patients with ACL tears than in uninjured children. Further, patients undergoing primary ACLR as well as a strong family history of ACL tears are more likely to sustain a postoperative graft rupture or complication requiring surgery.
Keywords: knee, ligaments, ACL, epidemiology, family history, familial predisposition
The rate of anterior cruciate ligament (ACL) tears among pediatric patients has increased over the past 20 years, from 117 to 140 injuries per 100,000 patient-years in females over the years from 1994 to 2013.4 This is thought to be at least partly associated with increasing participation in sports among US children.1 Such injuries place a significant economic burden on the patients and their families, estimated at nearly US$3 billion annually for ACL reconstructions (ACLRs) and more than US$7.5 billion when including costs incurred during postoperative rehabilitation and other associated complications.21 Given these costs and the multitude of complications after ACL rupture including meniscal and cartilaginous damage, recurrent instability, and osteoarthritis, identification of predictive variables to identify those most at risk of ACL tears remains paramount.8–10,18,28 Prior studies5,12,29 have identified several extrinsic risk factors, including sport played, weather conditions, and landing patterns, that show some association with risk of ACL injury. Even more intrinsic risk factors have been identified, including sex, prior injury, ligamentous laxity, increased tibial slope, decreased notch width, and multiple genetic markers (ie, familial predisposition).7,16,17,19,20,24,25
Family history of ACL tear specifically is thought to be a risk factor for ACL injury, with previous studies11,13–15,22,30 demonstrating a 16%-38% rate of ACL tears in first-degree family members of index patients. These studies have focused primarily on adult populations with no separate analysis of pediatric patients and variable results. Only 1 small study14 of pediatric soccer athletes with ACL injury has examined familial predisposition to ACL injury, and few studies6,13 have examined postoperative complications. With the incidence of pediatric ACL injuries steadily increasing and a high rate of complications after surgery in this population, identification of related risk factors may provide opportunities for intervention.
Therefore, the primary objective of this study was to determine whether pediatric patients undergoing ACLR are more likely than uninjured children to have a first-degree relative who had previously suffered an ACL injury. Additionally, for patients undergoing ACLR, we sought to compare the rates of concomitant meniscal or ligamentous injuries and postoperative complications by the number of relatives with an ACL tear history. We hypothesized that when compared with controls, pediatric patients undergoing ACLR would have a significantly higher number of first-degree relatives with an ACL rupture history. We also hypothesized that there would be no difference in the rates of postoperative graft ruptures or complications requiring surgery when patients were categorized by the number of first-degree relatives with an ACL injury history.
Methods
This was an institutional review board–approved 2-part retrospective case-control and cohort study of 1009 pediatric patients (≤18 years of age) who underwent primary ACLR at our institution between January 2009 and May 2016. Surgeries were performed at an urban tertiary care children’s hospital by 3 fellowship-trained pediatric orthopaedic surgeons. Age at the time of surgery, sex, laterality, body mass index (BMI), sport at injury, and mechanism of injury as well as concomitant meniscal and ligamentous injuries were obtained from patient medical records. Sports were categorized according to the level of contact based on a classification system described by the American Academy of Pediatrics.27 Patients who underwent revision ACLRs or patients with an unknown history of familial ACL tear were excluded.
Patients (or a parent) were then contacted up to 3 times via email and/or telephone to complete a follow-up survey regarding subsequent complications. These included, but were not limited to, graft rupture, contralateral ACL injury, and meniscal tears. They were additionally questioned on a first-degree (parent or sibling) family history of ACL tear. In patients with a positive family history, the age and sport played at injury were recorded for afflicted relatives. Patients were then stratified into 3 cohorts by the number of first-degree relatives with an ACL rupture history: no relatives, 1 relative, or ≥2 relatives.
A control group of uninjured knees was recruited from children seen in the concussion clinic of our institution in order to compare the rates of familial ACL tears of patients undergoing ACLR with those in an unaffected population. Patients were selected from this clinic, as the majority were sports-playing children whom the authors believed would make suitable controls for the ACL cohort. Controls were ≤18 years of age and excluded if they had a history of ACL or meniscal injury or an unknown history of familial ACL tear. A power analysis revealed that we required a total of 316 patients (158 patients with ACL ruptures and 158 without ACL ruptures) to detect a 12% difference in familial ACL injury rates between the groups, based on the results of Flynn et al11 who reported an 11.7% difference in an adult study of first-degree relative ACL injury rates. A total of 2070 patients were ultimately contacted by telephone once. It was thought that an email survey would result in selection bias toward patients with a family history of ACL tear who might be more interested in participating, and therefore, control patients were contacted only by telephone.
Statistical analyses were performed using SPSS Statistics for Macintosh, Version 24.0 (IBM). Descriptive statistics were reported for characteristic variables. Categorical variables were analyzed using chi-square or Fisher exact tests. Continuous variables were analyzed using independent-sample t tests and 1-way analysis of variance tests for normally distributed data, while nonparametric variables were analyzed using Mann-Whitney U and Kruskal-Wallis tests. Binary logistic regressions were used to determine the factors predictive of (1) having a first-degree relative with an ACL tear history, (2) a postoperative graft rupture, or (3) complication requiring reoperation, with odds ratios (ORs) and 95% CIs calculated for each analysis. The threshold for significance was set at P < .05 for all statistical tests conducted.
Results
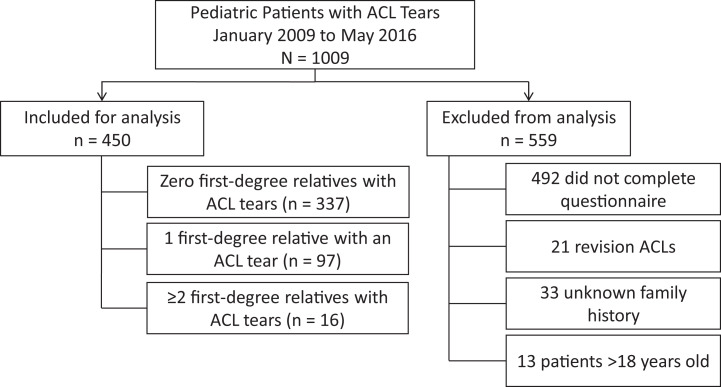
Of the 517 pediatric patients who had undergone ACLR surgery and completed our survey, 450 sustained a primary ACL injury and were included for analysis (Figure 1). The mean age at surgery was 14.9 ± 2.2 years with a mean follow-up of 4.3 ± 2.1 years (Table 1). A total of 237 (52.7%) patients were female, and 404 (89.8%) sustained an ACL injury while playing a sport. A total of 113 (25.1%) respondents had at least 1 first-degree family member with an ACL tear history. A total of 114 (25.3%) patients suffered a complication (Table 2). A total of 56 (12.4%) patients sustained a graft rupture during the follow-up period, and 97 (21.6%) required a return to the operating room for a complication or subsequent injury.
Figure 1.
Flowchart demonstrating the application of inclusion and exclusion criteria. ACL, anterior cruciate ligament.
Table 1.
Baseline Characteristics of Patients With ACL Injury (n = 450)a
| Characteristics | Mean ± SD or n (%) |
|---|---|
| Age, y | 14.9 ± 2.2 |
| Sex (female) | 237 (52.7) |
| BMI | 22.8 ± 4.6 |
| Laterality (left) | 208 (46.2) |
| Playing sport during injury | 404 (89.8) |
| Noncontact | 9 (2.2) |
| Limited contact | 30 (7.4) |
| Contact or collision | 365 (90.3) |
| Contact mechanism | 139 (35.5)b |
| Concomitant injury | 334 (74.2) |
| Meniscal injury | 330 (73.3) |
| Ligamentous injury | 25 (5.6) |
| First-degree relatives with ACL tears | 113 (25.1) |
| Follow-up length, y | 4.3 ± 2.1 |
aACL, anterior cruciate ligament; BMI, body mass index.
bMechanism of injury was available only for 391 patients.
Table 2.
Complication Typesa
| Complication (ipsilateral unless noted) | n |
|---|---|
| Patients with any complication | 114 |
| Graft rupture | 56 |
| Contralateral ACL tear | 33 |
| Meniscal tear | 38 |
| Other ligamentous (MCL, LCL, PCL) tear/sprain | 4 |
| Patellar dislocation/instability | 3 |
| Arthrofibrosis | 6 |
| Otherb | 5 |
| Required reoperation | 97 |
aACL, anterior cruciate ligament; LCL, lateral collateral ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament.
b1 each: loose body, chondral injury, meniscal transplant, cartilage removal, and ACL sprain.
A total of 267 patients with no history of knee injury were then used as controls for comparison with the 450 patients with an ACL tear (Table 3). Patients who had torn their ACL reported a significantly higher number of first-degree relatives with an ACL injury history when compared with controls (25.1% vs 12.0%; P < .001). When adjusting for age, sex, and sports participation in multivariate analysis, children with an ACL injury were at nearly 3 times (OR, 2.7) higher odds of having a first-degree relative with an ACL tear (95% CI, 1.7-4.2; P < .001). First-degree relatives of patients with ACL tears were also on average younger at injury (21.7 ± 8.6 vs 27.8 ± 12.4 years; P = .026) than relatives of patients without ACL injuries.
Table 3.
Comparison of Patients With and Without ACL Injurya
| ACL Injury (n = 450) | No ACL Injury (n = 267) | P | |
|---|---|---|---|
| Age, y | 14.9 ± 2.2 | 13.5 ± 2.7 | <.001 |
| Sex (female) | 237 (52.7) | 147 (55.1) | .535 |
| Playing sport during injury | 404 (89.8) | 222 (83.1) | .010 |
| Noncontact | 9 (2.2) | 37 (16.7) | <.001 |
| Limited contact | 30 (7.4) | 33 (14.9) | |
| Contact or collision | 365 (90.3) | 152 (68.5) | |
| First-degree relatives with ACL tears | 113 (25.1) | 32 (12.0) | <.001 |
| Age of youngest first-degree relative with ACL tears, yb | 21.7 ± 8.6 | 27.8 ± 12.4 | .019 |
| Sport played by first-degree relative with ACL tearsc | .399 | ||
| Noncontact | 2 (2.1) | 1 (5.3) | |
| Limited contact | 20 (21.1) | 5 (26.3) | |
| High contact | 73 (76.8) | 13 (68.4) |
aStatistics reported as either mean ± SD or n (%). For the group that did not suffer an ACL injury (controls), the sport played during injury reflects the sport played at the time that they suffered a concussion. Additionally, sport played at the time of injury for first-degree relatives was only available for 96 and 19 patients in the case and control groups, respectively. ACL, anterior cruciate ligament.
bMann-Whitney U test.
cFisher exact test.
Patients who had sustainedan ACL rupture (n = 450) were then categorized into 3 groups: 337 patients with no first-degree family history, 97 with 1 first-degree relative, and 16 with ≥2 first-degree relatives with an ACL tear history (Table 4). The number of concomitant meniscal and ligamentous injuries did not differ significantly across the 3 groups. Patients with ≥2 familial ACL tears had a significantly higher graft failure rate (37.5%) than patients with 0 or 1 familial ACL injury (11.9% and 10.3%, respectively; P = .008). This group also suffered significantly more complications that required reoperation (62.5% vs 19.6% and 21.6%; P < .001). When adjusting for age, sex, BMI, and sports participation in binary logistic regression, ≥2 familial ACL tears (OR, 5.1; 95% CI, 1.7-15.2; P = .003) and male sex (OR, 1.8; 95% CI, 1.0-3.3; P = .046) were predictive of suffering a postoperative graft rupture, while only ≥2 familial ACL tears was predictive of a requirement for reoperation (OR, 7.5; 95% CI, 2.6-22.0; P < .001).
Table 4.
Concomitant Injury and Postoperative Complications by Family Historya
| Number of First-Degree Relatives With ACL Tears | ||||
|---|---|---|---|---|
| Patient characteristics | 0 (n = 337) | 1 (n = 97) | ≥2 (n = 16) | P |
| Age, y | 14.9 ± 2.2 | 14.7 ± 2.1 | 15.1 ± 2.1 | .540 |
| Sex (female) | 170 (50.4) | 58 (59.8) | 9 (56.3) | .256 |
| BMIb | 22.9 ± 4.7 | 22.1 ± 4.3 | 24.0 ± 3.0 | .053 |
| Laterality (left) | 154 (45.7) | 47 (48.5) | 7 (43.8) | .873 |
| Playing sport during injuryc | 304 (90.2) | 86 (88.7) | 14 (87.5) | .737 |
| Noncontactc | 7 (2.3) | 2 (2.3) | 0 (0) | .422 |
| Limited contact | 19 (6.3) | 9 (10.5) | 2 (14.3) | |
| Contact or collision | 278 (91.4) | 75 (87.2) | 12 (85.7) | |
| Contact mechanism | 105 (35.8)d | 29 (34.1)e | 5 (38.5)f | .935 |
| Concomitant injuryc | 252 (74.8) | 70 (72.2) | 12 (75.0) | .875 |
| Meniscalc | 250 (74.2) | 68 (70.1) | 12 (75.0) | .685 |
| Ligamentousc | 19 (5.6) | 5 (5.2) | 1 (6.3) | ≥.999 |
| Complication | 81 (24.0) | 23 (23.7) | 10 (62.5) | .002 |
| Graft rupture | 40 (11.9) | 10 (10.3) | 6 (37.5) | .008 |
| Contralateral ACLc | 22 (6.5) | 10 (10.3) | 1 (6.3) | .371 |
| Meniscal tearc | 31 (9.2) | 6 (6.2) | 1 (6.3) | .468 |
| Required reoperation | 66 (19.6) | 21 (21.6) | 10 (62.5) | <.001 |
aStatistics reported as either mean ± SD or n (%). ACL, anterior cruciate ligament; BMI, body mass index.
bKruskal-Wallis 1-way analysis of variance.
cFisher exact test.
dn = 293.
en = 85.
fn = 13.
Discussion
Owing to the physical, financial, and psychosocial costs associated with complications after ACL injury, identifying predictive variables to determine those most at risk of ACL tears is of great interest. Previous studies in adult populations have shown a high rate of ACL rupture in first-degree family members, although none have examined pediatric patients or postoperative outcomes. Our population had a mean follow-up of 4.3 ± 2.1 years and was therefore able to analyze postoperative complications in patients with midterm follow-up. This study is the largest to show that pediatric patients undergoing primary ACLR have a significantly higher first-degree family history of ACL injury compared with control populations. Further, we show that patients with multiple familial ACL tears are at a higher risk of postoperative graft ruptures and complications requiring reoperation.
When comparing patients with ACL tears with controls, those with ACL injuries had more than twice the rate of first-degree familial ACL tears. After controlling for age, sex, sports participation, and family history of ACL tear, a patient with an ACL rupture was nearly 3 times as likely to have a first-degree family member with an ACL injury history. Such results—in both patients with and without ACL tears—are mostly consistent with previously reported rates (Table 5), although there are some discrepancies in the adult literature.13,15 Anderson et al2 were among the first to describe the potential contribution of family history to ACL tear incidence, although they did not report a higher incidence of ACL rupture in family members of patients with ACL tears. Another paper by Myer et al22 also showed no difference in the rate of familial ACL tears between patients with ACL injuries and those without (20% vs 15%).
Table 5.
Review of Prior Studies on the Familial Predisposition to ACL Injurya
| First Author | Study Population | Age of Patients With ACL | Relationships Assessed | FH in Patients With ACL Injury | FH in Patients Without ACL Injury | P |
|---|---|---|---|---|---|---|
| Goshima13 | ACLRs | 21b | First-degree relatives | 38/233 (16.3%) | — | — |
| Flynn11 | ACL tear vs no major knee injury | 23b | First-degree relatives | 40/171 (23.4%) | 20/171 (11.7%) | .004 |
| Hägglund14 | ACL injury vs no ACL injury | 15.0 ± 0.9 | First-degree relatives | 8/21 (38.1%) | 648/4280 (15.1%) | .004 |
| Harner15 | Bilateral ACL tears vs no knee injury history | 29.3 ± 6.8 | Immediate relatives | 11/31 (35.5%) | 1/23 (4.3%) | .008 |
| Westin30 | ACL tears vs without ACL tears | 20.5 ± 2.6 | Parents | 19/65 (29.2%) | 64/353 (18.1%) | .039 |
| Myer22 | ACLR vs meniscectomy only | 27.3 ± 0.7 | First-degree relatives | 24/120 (20.0%) | 16/107 (15.0%) | .319 |
aACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; FH, family history; —, no data available.
bSD and range not reported.
However, several other studies11,14,15,30 have found a higher incidence of ACL ruptures in family members of patients with ACL tears. Flynn et al11 reported that significantly more adult patients had a first-degree relative with an ACL tear history versus controls with no knee injury history (23% vs 12%). In a study of elite alpine skiers, Westin et al30 found that 29% of skiers with ACL tears had a parent with an ACL injury history versus only 18% in patients without ACL tears. In the only study of pediatric patients, Hägglund and Waldén14 described the highest known rate of familial ACL injuries in athletes with ACL tears versus uninjured players (38% vs 15%). However, this was in a small, homogeneous Scandinavian population of only soccer players with ACL injury (N = 21) from which it is difficult to generalize to other sports or draw broad conclusions.14 Harner et al15 (35% vs 4%) reported similarly high rates, although this was also a small study and all patients had suffered bilateral ruptures. While some may hypothesize that pediatric patients would have a lower rate of familial ACL tear because of the lower cumulative risk (exposure) of injury in presumably younger first-degree relatives, this was not observed. This is actually consistent with the epidemiology of ACL injuries, as the majority occur in sports-playing adolescents and young adults with a dramatic decline in the incidence of ACL tears at older ages.26 Therefore, in adult patients whose first-degree relatives are likely older on average, the majority of tears would have already occurred before the patient reached adulthood. With confirmation of our original hypothesis, this study demonstrates that even in a pediatric population—and the largest familial predisposition study to date—there likely is a familial predisposition to ACL tear.
Myer et al22 further showed risk differences between male and female patients, which was not seen in our cohort. A previous study23 has shown that polymorphisms of collagen genes (eg, COL1A1 and COL5A1) can predispose individuals to ACL injury, particularly in female patients, which may explain such findings. This is thought to be associated with increased ligamentous laxity as type I collagen is the most important structural component of ligaments. It is possible that these polymorphisms not only contribute to the higher rate of familial ACL injuries observed in patients with ACL tears but also to the higher rate of complications after ACLR seen in patients with a strong family history of ACL injury. Although factors such as ligamentous laxity, notch width, limb alignment, and tibial slope were not the focus of this investigation, familial predisposition to ACL rupture—aside from the aforementioned genetic markers—could manifest in children as similar anthropomorphic differences, ultimately making them more susceptible to ACL injury. Other similar, but perhaps not as quantifiable, inheritable factors such as neuromuscular skill (ie, coordination) could additionally contribute to a risk of ACL tear in first-degree relatives. Surgeons can use this information to provide additional counseling on the risks of postoperative complications and implement appropriate postoperative rehabilitation plans and neuromuscular prevention programs for patients with a strong family history of ACL tear.
Of the 450 patients who sustained a first-time ACL tear, 1 in 4 had an ACL injury history in a first-degree family member, with 1 in 25 having more than 1 affected first-degree family member. Although there were no characteristic or postoperative differences between patients when classified simply by the presence or absence of a history of ACL tear in a first-degree family member (data not shown), subsetting patients by the number of first-degree familial ACL injuries revealed increased postoperative complications for patients with an ACL tear history in ≥2 first-degree family members. Specifically, in contrast to our initial hypothesis, a higher number of first-degree relatives was associated with a 5-fold increase in the number of graft tears and an 8-fold increase in all-cause requirement for reoperation. While this relationship was previously postulated by Goshima et al,13 their study did not find a significant difference in the number of postoperative ACL injuries for adult patients with and without a family history of ACL tear.13 Bourke et al6 previously showed that a family history of ACL tear was associated with a higher rate of postoperative graft rupture (hazard ratio, 1.9) and contralateral ACL tear (hazard ratio, 1.6), but this was in a study of almost entirely adult patients as old as 62 years of age. Our work is therefore the first to show that there is likely not only a genetic predisposition toward ACL tear in this subset of children but also toward associated postoperative complications.
Several limitations should be noted. As is common in any study using telephone- and email-based enrollment, there was possible selection bias as patients with a familial history of ACL injury may have been more likely to respond to our survey. However, for both the email and telephone surveys, the project description provided to patients and families focused on postoperative outcomes after ACL tear and did not specifically mention family history until the relevant section of the questionnaire. It is also possible that there was some recall bias, as those with an ACL tear may have been more likely to identify a familial history of ACL injury than an unaffected patient. This likely did not play a role in the reported rates for first-degree relatives but may have influenced the incidence of familial tear in more distant family members. While we were unable to capture all patients undergoing ACLR during the study period, a response rate of 51.3% is in line with nationally reported rates for email- and telephone-based surveys in medicine.3 Additionally, although adequately powered for comparison of familial ACL injury rate in pediatric patients with and without ACL tears, we may have been underpowered to detect smaller differences in postoperative complications between patients based on the number of first-degree relatives with an ACL injury history. Last, although there were some baseline characteristic differences between patients with and without ACL tears, we performed multivariate regressions to control for these, which demonstrated that the only significant predictor of having a first-degree relative with an ACL injury history was an ACL tear in pediatric patients.
Conclusion
Pediatric patients with an ACL tear had significantly more first-degree relatives with a family history of ACL injury than patients without ACL injuries. Further, pediatric patients with a strong family history of ACL tears were more likely to suffer a postoperative graft rupture and had a higher rate of complications requiring surgery compared with patients with no family history of an ACL injury. This information should be used to better counsel the patients of their risk of injury and consideration of sport choice. Additionally, patients with a strong family history who undergo ACLR can be better counseled regarding their postoperative risk of complications.
Footnotes
Final revision submitted March 21, 2020; accepted April 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: N.M.P. has received educational support from Liberty Surgical. T.J.G. has received research support from AlloSource, Arthrex, and Vericel and educational support from Liberty Surgical and is a paid associate editor for The American Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Children’s Hospital of Philadelphia (ref. No. 16-013464).
References
- 1. 2017-18 High School Athletics Participation Survey: National Federation of State High School Associations; 2018.
- 2. Anderson AF, Lipscomb AB, Liudahl KJ, Addlestone RB. Analysis of the intercondylar notch by computed tomography. Am J Sports Med. 1987;15(6):547–552. [DOI] [PubMed] [Google Scholar]
- 3. Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. [DOI] [PubMed] [Google Scholar]
- 4. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3):e20161877. [DOI] [PubMed] [Google Scholar]
- 5. Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med. 2014;42(8):1806–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bourke HE, Salmon LJ, Waller A, Patterson V, Pinczewski LA. Survival of the anterior cruciate ligament graft and the contralateral ACL at a minimum of 15 years. Am J Sports Med. 2012;40(9):1985–1992. [DOI] [PubMed] [Google Scholar]
- 7. Brandon ML, Haynes PT, Bonamo JR, Flynn MI, Barrett GR, Sherman MF. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy. 2006;22(8):894–899. [DOI] [PubMed] [Google Scholar]
- 8. Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):1967–1976. [DOI] [PubMed] [Google Scholar]
- 9. Ekas GR, Laane MM, Larmo A, et al. Knee pathology in young adults after pediatric anterior cruciate ligament injury: a prospective case series of 47 patients with a mean 9.5-year follow-up. Am J Sports Med. 2019;47(7):1557–1566. [DOI] [PubMed] [Google Scholar]
- 10. Ekas GR, Moksnes H, Grindem H, Risberg MA, Engebretsen L. Coping with anterior cruciate ligament injury from childhood to maturation: a prospective case series of 44 patients with mean 8 years’ follow-up. Am J Sports Med. 2019;47(1):22–30. [DOI] [PubMed] [Google Scholar]
- 11. Flynn RK, Pedersen CL, Birmingham TB, Kirkley A, Jackowski D, Fowler PJ. The familial predisposition toward tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33(1):23–28. [DOI] [PubMed] [Google Scholar]
- 12. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44(10):2716–2723. [DOI] [PubMed] [Google Scholar]
- 13. Goshima K, Kitaoka K, Nakase J, Tsuchiya H. Familial predisposition to anterior cruciate ligament injury. AP-SMART. 2014;1(2):62–66. [Google Scholar]
- 14. Hägglund M, Waldén M. Risk factors for acute knee injury in female youth football. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):737–746. [DOI] [PubMed] [Google Scholar]
- 15. Harner CD, Paulos LE, Greenwald AE, Rosenberg TD, Cooley VC. Detailed analysis of patients with bilateral anterior cruciate ligament injuries. Am J Sports Med. 1994;22(1):37–43. [DOI] [PubMed] [Google Scholar]
- 16. Hewett TE, Lynch TR, Myer GD, Ford KR, Gwin RC, Heidt RS., Jr Multiple risk factors related to familial predisposition to anterior cruciate ligament injury: fraternal twin sisters with anterior cruciate ligament ruptures. Br J Sports Med. 2010;44(12):848–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. John R, Dhillon MS, Sharma S, Prabhakar S, Bhandari M. Is there a genetic predisposition to anterior cruciate ligament tear? A systematic review. Am J Sports Med. 2016;44(12):3262–3269. [DOI] [PubMed] [Google Scholar]
- 18. Johnson VL, Roe JP, Salmon LJ, Pinczewski LA, Hunter DJ. Does age influence the risk of incident knee osteoarthritis after a traumatic anterior cruciate ligament injury? Am J Sports Med. 2016;44(9):2399–2405. [DOI] [PubMed] [Google Scholar]
- 19. Kaynak M, Nijman F, van Meurs J, Reijman M, Meuffels DE. Genetic variants and anterior cruciate ligament rupture: a systematic review. Sports Med. 2017;47(8):1637–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Keays SL, Keays R, Newcombe PA. Femoral intercondylar notch width size: a comparison between siblings with and without anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):672–679. [DOI] [PubMed] [Google Scholar]
- 21. Mather RC, 3rd, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Myer GD, Heidt RS, Waits C, et al. Sex comparison of familial predisposition to anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2014;22(2):387–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Posthumus M, September AV, Keegan M, et al. Genetic risk factors for anterior cruciate ligament ruptures: COL1A1 gene variant. Br J Sports Med. 2009;43(5):352–356. [DOI] [PubMed] [Google Scholar]
- 24. Price MJ, Tuca M, Cordasco FA, Green DW. Nonmodifiable risk factors for anterior cruciate ligament injury. Curr Opin Pediatr. 2017;29(1):55–64. [DOI] [PubMed] [Google Scholar]
- 25. Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalised joint laxity. J Bone Joint Surg Br. 2005;87(6):800–803. [DOI] [PubMed] [Google Scholar]
- 26. Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42(6):394–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rice SG, American Academy of Pediatrics Council on Sports Medicine and Fitness. Medical conditions affecting sports participation. Pediatrics. 2008;121(4):841–848. [DOI] [PubMed] [Google Scholar]
- 28. Risberg MA, Oiestad BE, Gunderson R, et al. Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med. 2016;44(5):1215–1224. [DOI] [PubMed] [Google Scholar]
- 29. Smith HC, Vacek P, Johnson RJ, et al. Risk factors for anterior cruciate ligament injury: a review of the literature-part 2: hormonal, genetic, cognitive function, previous injury, and extrinsic risk factors. Sports Health. 2012;4(2):155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Westin M, Reeds-Lundqvist S, Werner S. The correlation between anterior cruciate ligament injury in elite alpine skiers and their parents. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):697–701. [DOI] [PubMed] [Google Scholar]