Abstract
Background:
It is unknown whether the treatment effects of partial meniscectomy and physical therapy differ when focusing on activities most valued by patients with degenerative meniscal tears.
Purpose:
To compare partial meniscectomy with physical therapy in patients with a degenerative meniscal tear, focusing on patients’ most important functional limitations as the outcome.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
This study is part of the Cost-effectiveness of Early Surgery versus Conservative Treatment with Optional Delayed Meniscectomy for Patients over 45 years with non-obstructive meniscal tears (ESCAPE) trial, a multicenter noninferiority randomized controlled trial conducted in 9 orthopaedic hospital departments in the Netherlands. The ESCAPE trial included 321 patients aged between 45 and 70 years with a symptomatic, magnetic resonance imaging–confirmed meniscal tear. Exclusion criteria were severe osteoarthritis, body mass index >35 kg/m2, locking of the knee, and prior knee surgery or knee instability due to an anterior or posterior cruciate ligament rupture. This study compared partial meniscectomy with physical therapy consisting of a supervised incremental exercise protocol of 16 sessions over 8 weeks. The main outcome measure was the Dutch-language equivalent of the Patient-Specific Functional Scale (PSFS), a secondary outcome measure of the ESCAPE trial. We used crude and adjusted linear mixed-model analyses to reveal the between-group differences over 24 months. We calculated the minimal important change for the PSFS using an anchor-based method.
Results:
After 24 months, 286 patients completed the follow-up. The partial meniscectomy group (n = 139) improved on the PSFS by a mean of 4.8 ± 2.6 points (from 6.8 ± 1.9 to 2.0 ± 2.2), and the physical therapy group (n = 147) improved by a mean of 4.0 ± 3.1 points (from 6.7 ± 2.0 to 2.7 ± 2.5). The crude overall between-group difference showed a –0.6-point difference (95% CI, –1.0 to –0.2; P = .004) in favor of the partial meniscectomy group. This improvement was statistically significant but not clinically meaningful, as the calculated minimal important change was 2.5 points on an 11-point scale.
Conclusion:
Both interventions were associated with a clinically meaningful improvement regarding patients’ most important functional limitations. Although partial meniscectomy was associated with a statistically larger improvement at some follow-up time points, the difference compared with physical therapy was small and clinically not meaningful at any follow-up time point.
Registration:
NCT01850719 (ClinicalTrials.gov identifier) and NTR3908 (the Netherlands Trial Register).
Keywords: Knee, Patient-Specific Functional Scale, meniscus, arthroscopic surgery, physical therapy
For patients middle-aged and older with degenerative meniscal tears, previous randomized controlled trials have revealed no clinically relevant benefit of partial meniscectomy over nonoperative treatment such as physical therapy and sham surgery.9,11,12,14,16,22,26,31 When deciding on the best treatment for individual patients, their specific needs during activities of daily living should be taken into account. Additionally, the patient’s perspective is important in treatment outcomes and is gaining attention in health care evaluation studies.17
Past trials have investigated treatment effects using general, fixed-item patient-reported outcome measures (PROMs).9,11,12,14,16,22,26,31 The results of these studies were based on scores from the International Knee Documentation Committee (IKDC) subjective knee form, Knee injury and Osteoarthritis Outcome Score, and Western Ontario and McMaster Universities Osteoarthritis Index.9,11,12,14,16,22,26,31 These PROMs are validated for various patient populations, such as patients with anterior cruciate ligament (ACL) injuries, cartilage damage, and meniscal tears.4,13,20 Although these fixed-item PROMs are adequate measures for health care evaluation studies, the items that are embedded in these PROMs do not take the variety of important daily life activities for individual patients into account.2,30 When using such fixed-item outcome measures, one assumes that all items are equally relevant for all patients.30 Therefore, the scores of items that are less or not relevant for a patient can influence the overall results.30 Additionally, these PROMs may not take into account an individual patient's rehabilitation goals.
The patient’s specific needs in daily life should be taken into account when evaluating treatment from a patient’s perspective. A patient-specific instrument can be used in addition to the more generic, fixed-item PROMs. An instrument such as the Patient-Specific Functional Scale (PSFS; https://www.physio-pedia.com/Patient_Specific_Functional_Scale) allows patients to select or propose those activities that are most relevant to them (ie, patient-specific activities) and quantify the experienced difficulty in performing those activities because of their condition.2,5,6 Middle-aged and older patients with a meniscal tear seem to overestimate the effectiveness of surgery in terms of participation in daily life activities such as walking and sports activities.18 Research shows that 59% of these patients were too optimistic about their return to daily life and leisure activities after surgery.19 The patient’s overestimation of a surgical intervention could partly explain why meniscal surgery is still so frequently performed.
Patient-specific activities have not yet been considered as part of the evaluation of treatment effects in those with a meniscal tear. Furthermore, assessing treatment effects using patient-specific activities can enhance treatment involvement, satisfaction, and perceived recovery.23 This study compared the effectiveness of partial meniscectomy versus physical therapy on patient-specific activities over 24 months for middle-aged and older patients with degenerative meniscal tears. We used the PSFS in addition to the fixed-item IKDC form, as previously published,26,28 to assess differences between these treatments.
Methods
Study Design
For this study, we analyzed data of early surgery versus nonoperative treatment with optional delayed meniscectomy for patients aged ≥45 years with nonobstructive meniscal tears as part of the Cost-effectiveness of Early Surgery versus Conservative Treatment with Optional Delayed Meniscectomy for Patients over 45 years with non-obstructive meniscal tears (ESCAPE) trial, a multicenter randomized controlled trial comparing partial meniscectomy with physical therapy.27 A medical ethics committee approved the ESCAPE trial in 2013, and the trial was registered at ClinicalTrials.gov (NCT01850719) and the Netherlands Trial Register (NTR3908).
Enrollment and Randomization
Patients for the ESCAPE trial were recruited from 9 participating hospitals in the Netherlands. Details on the inclusion/exclusion criteria and participant enrollment are described in the published study protocol.27 In short, patients aged between 45 and 70 years with knee pain related to a meniscal tear (ie, pain experienced on the same side, medial or lateral, or both) were recruited for the trial. Meniscal tears were diagnosed by magnetic resonance imaging (MRI; 3.0 T) according to the ISAKOS grading system. If a participating surgeon considered a tear suitable for repair, the patient could not participate in the trial. Exclusion criteria were severe osteoarthritis (Kellgren-Lawrence grade of 4, significant osteophytes, joint-space narrowing, sclerosis, and abnormalities of bone ends),15 body mass index >35 kg/m2, locking of the knee,3 prior surgery to the index knee (with the exception of diagnostic arthroscopic surgery), and knee instability due to an MRI-confirmed ACL or posterior cruciate ligament rupture. Patients were randomly allocated by computer to receive either partial meniscectomy or physical therapy in a 1:1 ratio with varying block sizes up to a maximum of 6. The randomization scheme was stratified by hospital and age (45-57 and 58-70 years). Participants, clinicians, and research staff were not blinded for treatment allocation during data collection. However, the researchers did perform statistical analyses on a blinded database. The database was unblinded for the interpretation of the results.
Interventions
Partial Meniscectomy
Patients assigned to the partial meniscectomy group underwent surgery within 4 weeks after randomization at the hospital of inclusion. Partial meniscectomy consisted of an intra-articular inspection of the knee joint according to standardized surgery protocols, including an assessment of the lateral and medial menisci, the ACL, and the chondropathy as well as a general classification of the level of degeneration. The surgeon partially removed the affected meniscal portion until a stable and solid meniscus was reached. Meniscal repair was not performed in this population. All patients received written perioperative instructions. Rehabilitation after discharge from the hospital consisted of a home exercise program. The patient received a consultation in the outpatient orthopaedic clinic 8 weeks after surgery. In agreement with Dutch Orthopaedic Association guidelines, patients were only referred to physical therapy when signs of abnormal recovery were present.25
Physical Therapy
Physical therapy started within 2 weeks after randomization. Patients were referred to preselected physical therapy clinics that participated in the trial. The treatment protocol consisted of a progressive exercise program of 16 sessions, each 30 minutes long, over a period of 8 weeks. Additionally, patients underwent the same home exercise program as the partial meniscectomy group. Patients with persistent symptoms either continued the physical therapy treatment beyond the prescribed 16 weeks or were referred for delayed surgery by their orthopaedic physician. A detailed description of the physical therapy protocol can be found in Appendix 1.
Data Collection
Our data were collected within the ESCAPE trial, as described in the trial study protocol.27 We collected the data between July 2013 and October 2017. Patients completed self-administered questionnaires at baseline and at 3, 6, 12, and 24 months after enrollment, either online or on paper according to the preference of the patient. The baseline data for this study included patient characteristics, the level of osteoarthritis, and 3 PROM scores: the Dutch-language equivalent of the PSFS, the IKDC form, and a visual analog scale (VAS) for pain during weightbearing. The IKDC is a PROM for knee-specific symptoms, function, and sports activity. This PROM was developed for patients with knee ligament or meniscal injuries.13 The IKDC is a reliable and valid measurement instrument for patients with meniscal tears.29 In this questionnaire, the minimum score of 0 points represents the worst knee function, and the maximum score of 100 points indicates no limitations in function. We assessed the patient’s self-reported pain during weightbearing during the previous week at baseline. The pain intensity was scored using a VAS of 100 mm, with 0 indicating no pain and 100 indicating very severe pain. The VAS is the most reliable measure for degenerative knee pain.1 This study assessed the baseline scores for the IKDC and VAS for potential confounding effects on the main outcome.
The online questionnaires required completion of an item before continuing to the next item. For the paper questionnaires, the researcher obtained missing items by telephone. To enhance the response rate, the patient received up to 3 reminders. In case a patient was not able or willing to complete a questionnaire at a specific time point, efforts were made to collect data for the following time point(s).
Outcome
This study also focused on a secondary outcome measure of the ESCAPE trial: the Dutch-language equivalent of the PSFS. This Dutch-language questionnaire is also known as the Patient-Specific Complaint questionnaire, which is the term that we used in the ESCAPE trial protocol.27 The Dutch-language equivalent of the PSFS assesses subjective functional status by measuring patients’ perceived difficulty in performing activities that they value most in daily life and would like to improve. All patients selected a maximum of 3 activities. Patients could either choose from a predefined list of 28 activities or suggest their own. The perceived difficulty was quantified on an 11-point (0-10) numeric rating scale (NRS; online version) or on a 100-mm VAS (paper version). The VAS was subsequently converted into an NRS to match the measurement scale of the online questionnaire, with 0 indicating no difficulty and 10 indicating impossibility in performing that activity.1 A mean score was calculated per patient by adding the difficulty scores for each activity and dividing this by the number of selected activities. The PSFS is an efficient and easy-to-administer measurement tool. The time to complete the PSFS is about 4 minutes. In addition, the PSFS is a reliable measurement tool in patients with knee dysfunction.6
Before statistical analyses, we calculated the minimal important change (MIC) of the PSFS in our population, using an anchor-based method, to provide a context of clinical relevance.7 The anchor question was the following: “How did your function in daily activities change since the surgery/treatment of your knee?” A detailed description of the methods and results for the MIC calculation can be found in Appendix 2.
Statistical Analysis
Specific activities that were listed by patients were evaluated in terms of frequencies using descriptive statistics. The overall PSFS difficulty score was analyzed by linear mixed-model analysis using both intention-to-treat and as-treated approaches. In the intention-to-treat analysis, patients were divided into 2 groups according to treatment allocation: partial meniscectomy and physical therapy. For the as-treated analysis, patients were divided into 3 groups: patients allocated to partial meniscectomy who underwent surgery, patients allocated to physical therapy who completed at least 16 physical therapy sessions, and patients allocated to physical therapy who underwent surgery during the study period. Patients allocated to partial meniscectomy who did not undergo surgery and patients allocated to physical therapy who did not complete the physical therapy protocol or undergo surgery were discarded from the as-treated analysis.
In the linear mixed-model analysis with random intercepts, PSFS scores at all follow-up time points were included as dependent variables. The crude overall intervention effects were defined by a model with only the treatment group and the baseline score of the PSFS as independent variables. Time and time × treatment interaction terms were added to specify crude intervention effects for each follow-up time point. Adjusted intervention effects were calculated using similar models and expanded with the following potential confounders as independent variables: level of osteoarthritis according to Kellgren-Lawrence classification,15 baseline IKDC score, affected meniscus (medial, lateral, or both), body mass index (<25, 25-30, or 31-35 kg/m2), age in years, affected leg, sex, and baseline VAS pain score.
In all models, physical therapy was defined as the reference treatment. Adverse events from the ESCAPE trial were reported descriptively. All analyses were performed using SPSS Version 22 (IBM), and statistical significance was assessed at the .05 level.
Patient Involvement
A patient representative from the medical ethics committee (M.E.C.-U.) assessed the burden of the trial and patient information before the start of the ESCAPE trial. Furthermore, a representative of the Netherlands Patients Federation (J.K.) was added to the ESCAPE research group for this study and provided the authors with feedback on the study. Also, the representative advised us on an implementation strategy to translate the results to daily practice in orthopaedic and general health care.
Results
Patients
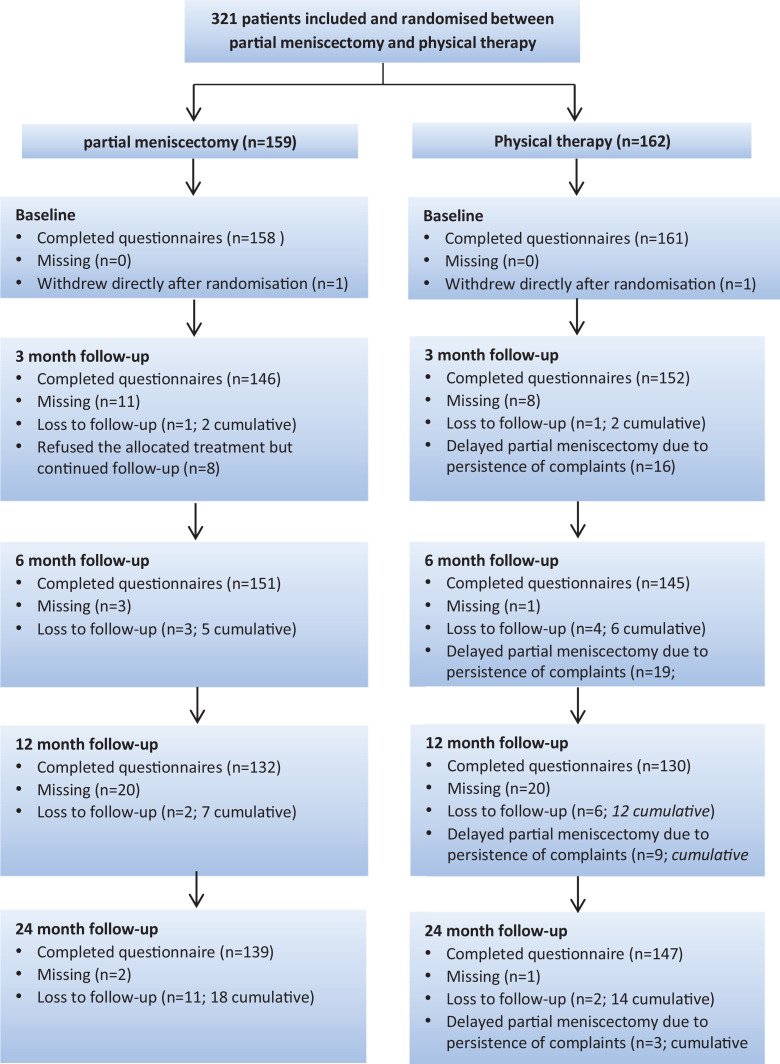
Figure 1 shows a flowchart of the treatment allocation and patient follow-up. We included 321 patients in the ESCAPE trial, who were randomly assigned to either the partial meniscectomy (n = 159) or the physical therapy (n = 162) group. The PSFS was completed by 319 patients (99.4%) at baseline, 298 patients (92.8%) at 3 months, 296 (92.2%) at 6 months, 262 (81.6%) at 1 year, and 286 (89.1%) at 2 years, which was the primary time point.
Figure 1.
Flow of patients. The flowchart shows the follow-up data of all patients allocated to a treatment group. The number of missing patients refers to the patients who were missing for a specific follow-up time point. These patients continued participating in the remaining follow-up time points. Patients who dropped out from the trial were referred to as “loss to follow-up.” Data of patients screened for eligibility were not available.
Baseline characteristics were similar in both treatment groups and are presented in Table 1. Patients selected a maximum of 3 (mean, 2.9 ± 0.4) activities that they experienced difficulty with and were most relevant to their daily life. The most frequently chosen activities in both groups were sports (12.4%), walking (10.3%), running (9.8%), standing for a long time (8.4%), and rising from a chair (7.4%). An overview of the frequencies and percentages of all activities for both groups is presented in Appendix 3.
TABLE 1.
Baseline Characteristics of Study Populationa
| Partial Meniscectomy (n = 158) | Physical Therapy (n = 161) | |
|---|---|---|
| Demographics | ||
| Age, y | 57.6 ± 6.5 | 57.3 ± 6.8 |
| Male sex, n (%) | 78 (49.4) | 80 (49.7) |
| Right knee, n (%) | 88 (55.7) | 81 (50.3) |
| Body mass index, kg/m2 | 26.7 ± 3.8 | 27.2 ± 4.0 |
| 18.5-25, n (%) | 56 (35.4) | 53 (32.9) |
| 26-30, n (%) | 72 (45.6) | 67 (41.6) |
| 31-35, n (%) | 30 (19.0) | 41 (25.5) |
| Mechanical complaints,b n (%) | 56 (35.4) | 67 (41.6) |
| Imaging c | ||
| Affected meniscus, n (%) | ||
| Medial | 126 (79.7) | 136 (84.5) |
| Lateral | 30 (19.0) | 25 (15.5) |
| Both | 2 (1.3) | 0 (0.0) |
| Osteoarthritis grade (Kellgren-Lawrence classification),d n (%) | n = 150 | n = 149 |
| 0 (none) | 18 (12.0) | 15 (10.1) |
| 1 (doubtful) | 81 (54.0) | 74 (49.7) |
| 2 (minimal) | 45 (30.0) | 55 (36.9) |
| 3 (moderate) | 6 (4.0) | 5 (3.4) |
| 4 (severe)e | 0 (0.0) | 0 (0.0) |
| Patient-reported outcomes | ||
| Knee function | ||
| PSFS score (0-10; best to worst) | 6.8 ± 1.9 | 6.6 ± 2.0 |
| IKDC score (0-100; worst to best) | 44.8 ± 16.6 | 46.5 ± 14.6 |
| Pain | n = 145 | n = 151 |
| VAS score during activities (0-100; best to worst) | 61.1 ± 24.5 | 59.3 ± 22.6 |
aData are shown as mean ± SD unless otherwise indicated. IKDC, International Knee Documentation Committee; PSFS, Patient-Specific Functional Scale; VAS, visual analog scale.
bIn contrast to locking of the knee joint, which was an exclusion criterion, mechanical complaints were allowed for inclusion.
cMeniscal tears were assessed on magnetic resonance imaging.
dOsteoarthritis was assessed using standing radiographs of the knee in the anterior-posterior direction.
ePatients with a Kellgren-Lawrence grade of 4 on baseline radiographs were excluded from the trial.
Minimal Important Change of the PSFS
The anchor-based calculation resulted in an MIC of 2.5 points for our study population. A more detailed description of these results can be found in Appendix 2.
Intention-to-Treat Analysis
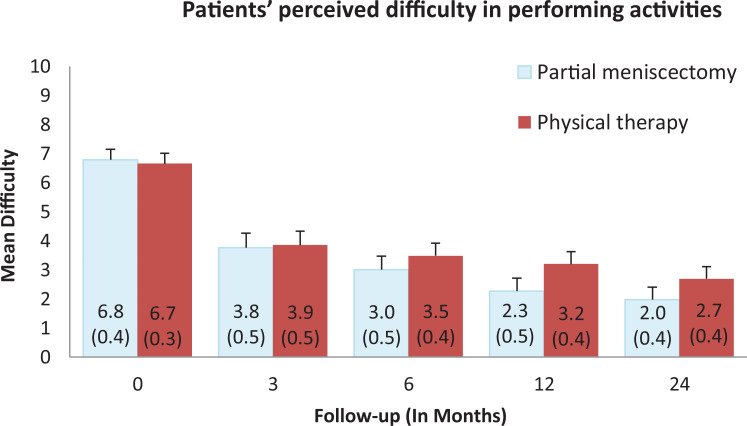
A total of 319 patients were included in the intention-to-treat analysis: 158 patients in the partial meniscectomy group and 161 patients in the physical therapy group. Group distributions per follow-up time point are reported in Table 2. From baseline to 24 months, the partial meniscectomy group improved a mean of 4.8 ± 2.6 points (from 6.8 ± 1.9 to 2.0 ± 2.2). The physical therapy group improved a mean of 4.0 ± 3.1 points (from 6.7 ± 2.0 to 2.7 ± 2.5) (Figure 2).
TABLE 2.
Intention-to-Treat Results of Mixed-Model Analysis
| n | Between-Group Differencea (95% CI) | P Value | |
|---|---|---|---|
| Partial Meniscectomy vs Physical Therapy | |||
| Crudeb | |||
| 3 mo | 146 vs 152 | –0.2 (–0.7 to 0.4) | .596 |
| 6 mo | 151 vs 145 | –0.6 (–1.2 to –0.1) | .034 |
| 12 mo | 132 vs 130 | –1.0 (–1.6 to –0.5) | <.001 |
| 24 mo | 139 vs 147 | –0.8 (–1.4 to –0.2) | .006 |
| Overall | 568 vs 574 | –0.6 (–1.0 to –0.2) | .004 |
| Adjustedc | |||
| 3 mo | 146 vs 152 | –0.4 (–1.0 to 0.2) | .184 |
| 6 mo | 151 vs 145 | –0.9 (–1.5 to –0.3) | .004 |
| 12 mo | 132 vs 130 | –1.2 (–1.8 to –0.6) | <.001 |
| 24 mo | 139 vs 147 | –0.8 (–1.3 to –0.2) | .006 |
| Overall | 568 vs 574 | –0.8 (–1.3 to –0.4) | <.001 |
aNegative values indicate that the difference is in favor of partial meniscectomy.
bCrude analyses, only corrected for the baseline Patient-Specific Functional Scale score.
cAdjusted analyses, with additional correction for potential confounders.
Figure 2.
Mean Patient-Specific Functional Scale (PSFS) scores for each group at baseline and at 3, 6, 12, and 24 months. The mean difficulty scores per group were calculated as the mean of the overall PSFS score per patient, adding the scores for each activity and dividing this by the number of selected activities per patient. Data in parentheses and error bars indicate the 95% CIs.
The mixed-model analysis revealed a significant crude overall treatment effect on the PSFS score between partial meniscectomy and physical therapy of –0.6 points in favor of partial meniscectomy (95% CI, –1.0 to –0.2; P = .004). At the different follow-up time points, the between-group difference was also significant, except at 3 months (Table 2). Adjusting for confounders increased the intervention effect to –0.8 points in favor of partial meniscectomy (95% CI, –1.3 to –0.4; P < .001). The adjusted between-group difference was also statistically significant at all follow-up time points, except at 3 months (Table 2).
As-Treated Analysis
A total of 294 patients were included in the as-treated analysis: 150 patients in the partial meniscectomy group, 97 patients in the physical therapy group, and 47 patients in the delayed partial meniscectomy group. Patients who had not undergone partial meniscectomy (n = 8) or who had not completed the physical therapy protocol (n = 17) were excluded from the as-treated analysis. Group distributions per follow-up time point are reported in Table 3.
TABLE 3.
As-Treated Results of Mixed Model Analysis
| Partial Meniscectomy vs Physical Therapy | Delayed Partial Meniscectomy vs Physical Therapy | |||||
|---|---|---|---|---|---|---|
| n | Between-Group Differencea (95% CI) | P Value | n | Between-Group Differencea (95% CI) | P Value | |
| Crude b | ||||||
| 3 mo | 133 vs 91 | 0.3 (–0.3 to 1.0) | .31 | 43 vs 91 | 2.0 (1.1 to 2.8) | <.001 |
| 6 mo | 144 vs 91 | –0.3 (–0.9 to 0.4) | .386 | 40 vs 91 | 1.3 (0.4 to 2.2) | .005 |
| 12 mo | 123 vs 81 | –0.7 (–1.4 to –0.1) | .033 | 32 vs 81 | 1.1 (0.1 to 2.0) | .026 |
| 24 mo | 133 vs 90 | –0.6 (–1.3 to 0.0) | .049 | 40 vs 90 | 0.6 (–0.3 to 1.5) | .193 |
| Overall | 533 vs 353 | –0.2 (–0.8 to 0.2) | .209 | 155 vs 353 | 1.3 (0.6 to 1.9) | <.001 |
| Adjusted c | ||||||
| 3 mo | 133 vs 91 | –0.1 (–0.7 to 0.6) | .843 | 43 vs 91 | 1.7 (0.8 to 2.6) | <.001 |
| 6 mo | 144 vs 91 | –0.7 (–1.3 to 0.0) | .05 | 40 vs 91 | 1.1 (0.2 to 2.1) | .024 |
| 12 mo | 123 vs 81 | –1.0 (–1.7 to –0.3) | .007 | 32 vs 81 | 1.0 (–0.01 to 2.0) | .053 |
| 24 mo | 133 vs 90 | –0.7 (–1.3 to 0.02) | .059 | 40 vs 90 | 0.8 (–0.1 to 1.8) | .094 |
| Overall | 533 vs 353 | –0.6 (–1.1 to –0.1) | .025 | 155 vs 353 | 1.2 (0.5 to 1.9) | .001 |
aNegative values indicate that the difference is in favor of partial meniscectomy.
bCrude analyses, only corrected for the baseline Patient-Specific Functional Scale score.
cAdjusted analyses, with additional correction for potential confounders.
The crude overall difference on the PSFS score between partial meniscectomy and physical therapy was –0.2 points in favor of partial meniscectomy (95% CI, –0.8 to 0.2; P = .209). The crude effect was significant at the 12-month and 24-month follow-up (Table 3).
After adjusting for potential confounders, the overall difference increased to –0.6 in favor of partial meniscectomy (95% CI, –1.1 to –0.1; P = .025) (Table 3). The adjusted effect was also significant at the 12-month follow-up but not at 24 months (Table 3).
We also observed a significant crude overall difference between the delayed partial meniscectomy group and the physical therapy group of 1.3 points (95% CI, 0.6-1.9; P < .001) in favor of the physical therapy group. Analyses of the separate follow-up time points showed that this difference was significant at all follow-up time points except at 24 months (Table 3). After adjusting for potential confounders, the effect remained significant only at 3 and 6 months (Table 3).
Adverse Events and Other Outcomes of the ESCAPE Trial
There were 17 participants (5.3%) who experienced a serious adverse event (partial meniscectomy: n = 9; physical therapy: n = 8). These serious adverse events included cardiovascular events (partial meniscectomy: n = 0; physical therapy: n = 2), neurological problems (partial meniscectomy: n = 1; physical therapy: n = 1), internal medicine conditions (partial meniscectomy: n = 2; physical therapy: n = 1), (re)surgery on the affected knee (partial meniscectomy: n = 4; physical therapy: n = 1), and total knee replacement (partial meniscectomy: n = 2; physical therapy: n = 3). Other nonserious adverse events occurred in 13 patients (partial meniscectomy: n = 9; physical therapy: n = 4) including reactive arthritis (partial meniscectomy: n = 1; physical therapy: n = 0); extra consultations because of consistent knee pain (partial meniscectomy: n = 6; physical therapy: n = 2); pain in the back, hip, or foot (partial meniscectomy: n = 2; physical therapy: n = 0); and nonspecified adverse events (partial meniscectomy: n = 0; physical therapy: n = 2).26
The primary outcomes of the ESCAPE trial were published in separate articles. These outcomes included patient-reported knee function, pain, and general health as well as the cost-effectiveness of both treatments.26,28
Discussion
In this study evaluating the treatment effect of degenerative meniscal tears focusing on activities most valued by individual patients, we found that patients with degenerative meniscal tears were mostly interested in improving in sports, walking, running, standing for a long time, and rising from a chair. Both partial meniscectomy and physical therapy resulted in a clinically relevant improvement over time on the individual patient’s most important activities. Differences between partial meniscectomy and physical therapy were statistically significant but not clinically relevant.
To our knowledge, only 1 previous study has reported on patients’ expectations after knee surgery.19 In that study, patients undergoing partial meniscectomy were asked, before surgery, what their expectations were on return to leisure activities. This was compared with the actual outcome at 3 months after surgery. Less than half of the patients participated at the level that they expected, which resulted in a high proportion of patients who were unsatisfied with their knee function and level of participation. Patients were mainly overoptimistic about their return to light and recreational sports activities, which are categories that match the 3 most frequently selected activities (sports, walking, running) in our study population. Together, these studies provide clinicians and patients with a more realistic prognosis on recovery expectations for activities most valued by the patient.
When comparing partial meniscectomy with nonoperative treatment (ie, physical therapy) for patients with a meniscal tear, previous trials have mainly focused on generic, fixed-item outcomes such as knee pain and function.9,11,12,14,16,26,31 The results of this study support the findings from previous studies that there is no clinically relevant difference between partial meniscectomy and physical therapy for middle-aged and older patients with a meniscal tear.9,11,12,14,16,21,26,31 An important benefit of using patient-specific outcomes instead of generic outcomes is that the outcome reflects the relevant daily life and leisure activities for individual patients.5 Therefore, this study strengthens the current guidelines on degenerative meniscal tears.9,11,12,14,16,21,26,31
Strengths and Limitations
This study compared partial meniscectomy with physical therapy for symptomatic meniscal tears from a patient’s perspective. The outcome measure focused on activities that were most valued by the patient, enhancing a patient-centered approach. We included a large sample of patients with symptomatic meniscal tears who were randomized between partial meniscectomy and physical therapy. The participation rate at 2-year follow-up was 89.1%. In addition, we found that, of the list of 28 activities, 4 of the 5 most selected activities were equal in both intervention groups. The similarity in selected activities between both groups reduced the likelihood that the type of chosen activities influenced our results.
This study has several limitations to report. First, participants, clinicians, and research staff were not blinded to the allocated treatment during data collection, and the patients’ preferred treatment before randomization was not recorded. This increases the chance of observer and participant bias. However, statistical analyses were performed with a blinded database. Second, the sample size was determined by the power calculation of the ESCAPE trial. We determined the calculation on the primary outcome of the ESCAPE trial, namely, the IKDC form, and not specifically based on the PSFS. Third, patients were recruited if they experienced knee pain related to MRI-confirmed meniscal tears. However, we cannot guarantee that their knee pain was solely caused by the meniscal tear. Mild to moderate degenerative changes of the knee can also play a role in experienced knee pain.8 Fourth, the PSFS is not validated in this specific population or in a similar population.
Fifth, the physical therapy protocol that we used in the ESCAPE trial consisted of general incremental exercises for cardiovascular conditioning, coordination, balance, and closed–kinetic chain strength of the lower extremities rather than exercises that focused on the relevant activities selected by our patients. Tailoring physical therapy to the individual patient, by including specific exercises that target the specific activities that patients selected on the PSFS, may have further increased the efficacy of physical therapy. Last, the scoring of the activities differed between the online (NRS; 94% at baseline) and paper-based (VAS; 6% at baseline) questionnaires. The VAS scores were converted to NRS scores before data analysis. Although the VAS and NRS show high correlations in pain measurements for osteoarthritic knee pain, the correlation for the PSFS is unknown.1
Implications
While our results show a statistically significant difference in favor of partial meniscectomy, the difference between the partial meniscectomy and physical therapy groups was small.10 In large samples, even very small differences between 2 groups can be statistically significant. However, statistical methods for significant differences do not account for clinical relevance.10 When translating research results to clinical practice, we must consider clinical relevance instead of relying on statistical differences alone. However, research on clinically relevant differences between groups is lacking,10 let alone for group differences on the PSFS in patients with meniscal tears. The upper limit of the 95% CI of both the crude and adjusted between-group differences did not exceed the calculated MIC of 2.5 points. Also, regardless of the exact MIC value, it seems highly unlikely that the between-group difference of less than 1 point can be considered clinically relevant.10 Although the calculated MIC of 2.5 points is in line with the 2.2 points on the PSFS reported in patients with cervical radiculopathy,32 more research is necessary on the clinical relevance of the PSFS for quantifying treatment effects within patients and for comparing treatment effects between intervention groups.
Based on an MIC of 2.5 points on an 11-point scale, the PSFS might not be the recommended tool to detect small treatment effects at the group level. Nevertheless, the PSFS could potentially be valuable for physicians and physical therapists to evaluate treatment effects from the patient’s point of view.32
Interestingly, our study results suggest that patients apparently only perceive relevant improvement when they experience substantially less difficulty during selected activities that matter most to them. In addition, we found a large variety in the specific activities that patients selected, as shown in Appendix 3. This indicates that a physical therapy program tailored to the individual patient’s needs and wishes may be even more beneficial than the one-size-fits-all strategy with general exercises used in our study.
A focus on patient-specific activities and realistic expectations when discussing treatment options with the patient may support the shared decision-making process and enhance treatment engagement in patients. Additional goal setting for each activity will further enhance treatment involvement, satisfaction, and perceived recovery.23,24
Conclusion
This study found a statistically significant difference but no clinically relevant difference between physical therapy and partial meniscectomy in middle-aged and older patients with a meniscal tear, with outcomes focused on activities that the individual patients valued most. We therefore conclude that physical therapy should be suggested as a first-line treatment for middle-aged and older patients with a meniscal tear to improve specific daily life and leisure activities. Targeting physical therapy exercises to the specific activities that a patient values the most may even further enhance the physical therapy treatment effect.
Acknowledgment
The authors thank all participants of the ESCAPE trial for their contribution to the study and the participating centers for their help in this study.
Appendix 1
Exercise Program Consisting of 16 Supervised Sessions for 8 Weeks
The exercise protocol is detailed in Table A1. For all exercises, it was important to keep the patient’s individual needs and limitations focused by using the International Classification of Functioning, Disability and Health. The uninjured side is also less trained as usual, and therefore, both sides should be trained.
TABLE A1.
Physical Therapy Exercise Program
| Time Point, wk | Exercises | Repetitions or Duration |
|---|---|---|
| 0-8 | Stationary cycling for warming up and cooling down or cardiovascular training, gradually increasing in intensity | ≥15 min |
| 0-8 | Pulley or DynaBand strapped around ankle on uninjured side; standing on injured side and keeping balance; and stepping with uninjured side forward, backward, and sideways | 3 × 12 repetitions each direction |
| 0-4 | Calf raises on leg press machine | 3 × 12 repetitions |
| 0-8 | Hamstrings: standing hip extension in “multi-hip” training device | 3 × 12 repetitions |
| 0-4 | Keeping balance on balance board using both feet | 30-60 s |
| 0-8 | Climbing stairs, walking, acceleration, running, and jumping according to patient’s activity level | 10 min |
| 5-8 | Calf raises while standing on 1 leg | 3 × 12 repetitions |
| 1-8 | Leg press, placing feet high enough for shinbones to become level in horizontal plane with knee, starting at 110° of flexion unilaterally | 3 × 12 repetitions |
| 5-8 | Squats (according to needs of patient) in which knee flexion >90° is not allowed | 3 × 12 repetitions |
| 5-8 | Balance board on 1 foot and challenge with throwing ball | 3 min |
| 5-8 | Elliptical machine for warming up and cooling down or cardiovascular training | ≥10 min |
In addition to training of the lower extremity, “core stability” training is of importance for good posture positioning and moving. An active rehabilitation program is designed around cardiovascular health (circulation), coordination and balance, and closed-chain strength exercises. Closed-chain exercises activate both agonists and antagonists around the knee joint, resulting in direct rotatory movement and preventing shearing forces seen when performing open-chain exercises.
Home Exercise Program
Additionally, a home exercise program was provided to all participants. It consisted of 1-leg standing for 60 seconds and a step-down exercise comprising 3, 9, and 10 repetitions, twice a week.
Appendix 2
Minimal Important Change (MIC) of the Patient-Specific Functional Scale (PSFS)
Methods
The MIC is defined as the smallest change in the PSFS score that patients perceive as a beneficial change. We determined the MIC value using an anchor-based method, as it uses an external criterion to determine what patients consider important. The external anchor question that we used was as follows: “How did your function in daily activities change since the surgery/treatment of your knee?” Patients answered the question on a 7-point Likert scale: very much improved, much improved, slightly improved, neutral, slightly deteriorated, much deteriorated, and very much deteriorated.
Before calculating the MIC, we first analyzed the correlation between the changes in the PSFS score and the external anchor question. Next, if this correlation was above 0.5, the study population was divided into changed and unchanged groups based on the external anchor question. The changed group comprised patients who reported to be very much, much, and slightly improved. The unchanged group comprised patients who self-reported as unchanged. We excluded patients who reported very much, much, or slight deterioration in daily functioning because we were comparing patients with important improvement versus patients without important improvement.
We used the receiver operating characteristic (ROC) curve method because it searches for the optimal cutoff points, irrespective of how much misclassification occurs. A graphic display of the ROC curve was plotted. We then determined the sensitivity and specificity for all potential cutoff points and determined the MIC value by the most optimal cutoff point, that is, with the smallest value of the sum of the proportions of misclassifications {[1 – sensitivity] + [1 – specificity]}. In other words, the MIC was quantified by the PSFS score that best discriminated between patients with and without clinically relevant improvement.
Results
The correlation between the changed PSFS score and the anchor question was 0.5. We then divided the population between changed (n = 216) and unchanged (n = 48) groups. The ROC curve had an area under the curve of 0.744; the graph is displayed in Figure A1 below.
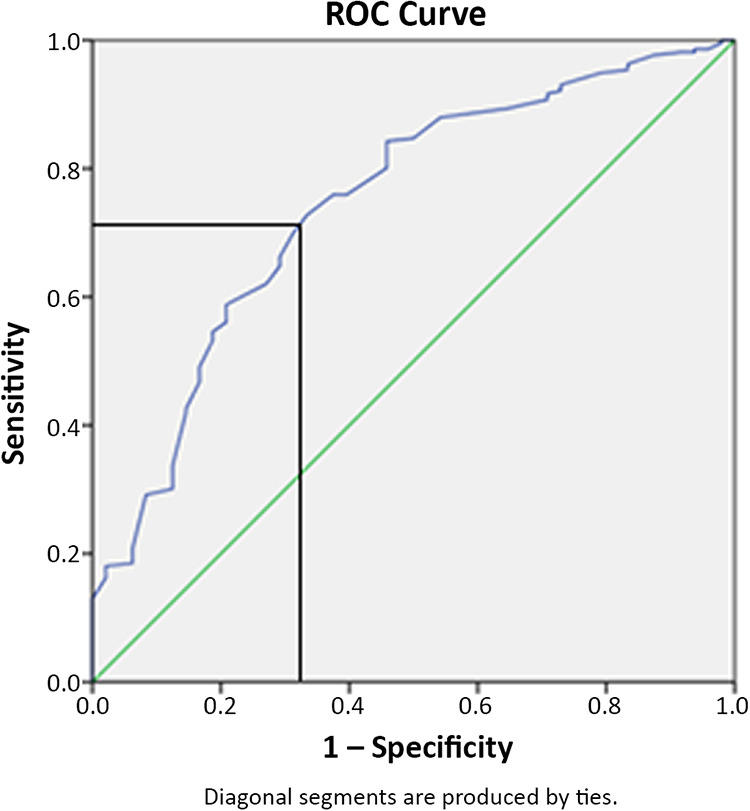
We determined the optimal cutoff at a sensitivity of 72.7% and a specificity of 66.7%, resulting in an MIC of 2.5 points on the PSFS (range, 0-10 points).
Appendix 3
Incidence of All Activitiesa
| Activity | Total | Partial Meniscectomy | Physical Therapy |
|---|---|---|---|
| Sports | 114 (12.4) | 60 (12.9) | 54 (11.9) |
| Walking | 95 (10.3) | 49 (10.6) | 46 (10.1) |
| Running | 90 (9.8) | 50 (10.8) | 40 (8.8) |
| Standing for a long time | 77 (8.4) | 37 (8.0) | 40 (8.8) |
| Rising up from a chair | 68 (7.4) | 37 (8.0) | 31 (6.8) |
| Turning over in bed | 55 (6.0) | 23 (5.0) | 32 (7.0) |
| Getting in/out of a car | 53 (5.8) | 23 (5.0) | 30 (6.6) |
| Lying in bed | 51 (5.5) | 32 (6.9) | 19 (4.2) |
| Cycling | 45 (4.9) | 26 (5.6) | 19 (4.2) |
| Heavy labor in and outside one’s home | 45 (4.9) | 21 (4.5) | 24 (5.3) |
| Sitting for long periods | 28 (3.0) | 15 (3.2) | 13 (2.9) |
| Carrying out one’s job | 28 (3.0) | 18 (3.9) | 10 (2.2) |
| Picking up an object from the floor | 27 (2.9) | 11 (2.4) | 16 (3.5) |
| Rising up from bed | 26 (2.8) | 10 (2.2) | 16 (3.5) |
| Driving a car or bus | 25 (2.7) | 12 (2.6) | 13 (2.9) |
| Carrying out hobbies | 18 (2.0) | 9 (1.9) | 9 (2.0) |
| Caring out household labor | 14 (1.5) | 5 (1.1) | 9 (2.0) |
| Other activities | 13 (1.4) | 7 (1.5) | 6 (1.3) |
| Traveling | 11 (1.2) | 3 (0.6) | 8 (1.8) |
| Standing | 10 (1.1) | 2 (0.4) | 8 (1.8) |
| Light labor in and outside one’s home | 8 (0.9) | 4 (0.9) | 4 (0.9) |
| Lifting | 6 (0.7) | 1 (0.2) | 5 (1.1) |
| Sexual activities | 3 (0.3) | 3 (0.6) | 0 (0.0) |
| Sitting on a chair | 2 (0.2) | 1 (0.2) | 1 (0.2) |
| Walking around the house | 2 (0.2) | 1 (0.2) | 1 (0.2) |
| Carrying an object | 2 (0.2) | 2 (0.4) | 0 (0.0) |
| Going out | 2 (0.2) | 1 (0.2) | 1 (0.2) |
| Visiting friends and family | 1 (0.1) | 1 (0.2) | 0 (0.0) |
aData are shown as n (%).
Authors: Julia C.A. Noorduyn, MSc, Tess Glastra van Loon, MSc, Victor A. van de Graaf, MD, PhD, Nienke W. Willigenburg, PhD, Ise K. Butter, MSc (Department of Orthopaedic Surgery, OLVG, Amsterdam, the Netherlands); Gwendolyne G.M. Scholten-Peeters, PhD (Amsterdam Movement Sciences, Faculty of Behavioural and Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands); Michel W. Coppieters, PhD (Amsterdam Movement Sciences, Faculty of Behavioural and Movement Sciences, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands; Menzies Health Institute Queensland, Griffith University, Gold Coast, Australia); Rudolf W. Poolman, MD, PhD (Department of Orthopaedic Surgery, OLVG, Amsterdam, the Netherlands; Department of Orthopaedic Surgery, Leiden University Medical Center, Leiden, the Netherlands); and the ESCAPE Research Group: Vanessa A.B. Scholtes, PhD, Eduard L.A.R. Mutsaerts, MD, PhD, Matthijs R. Krijnen, MD, PhD, Dirk Jan F. Moojen, MD, PhD, Derek F.P. van Deurzen, MD, Coen H. Bloembergen, MD (Department of Orthopaedic Surgery, OLVG, Amsterdam, the Netherlands); Julius Wolkenfelt, MD (Department of Orthopaedic Surgery, Bergman Clinics, Rijswijk, the Netherlands); Arthur de Gast, MD, PhD, Thom Snijders, MD (Department of Orthopaedic Surgery, Clinical Orthopaedic Research Center, Diakonessenhuis, Utrecht, the Netherlands); Daniel B.F. Saris, MD, PhD (Department of Orthopaedic Surgery, University Medical Center Utrecht, Utrecht, the Netherlands; Department of Orthopedic Surgery and Sports Medicine, Mayo Clinic, Rochester, Minnesota, USA); Nienke Wolterbeek, PhD (Department of Orthopaedic Surgery, St Antonius Ziekenhuis, Utrecht, the Netherlands); Camille Neeter, PhD (Fysiken Physical Therapy, Amsterdam, the Netherlands); Gino M.M.J. Kerkhoffs, MD, PhD (Department of Orthopaedic Surgery, Academic Medical Center, Amsterdam, the Netherlands); Rolf W. Peters, MD (Department of Trauma Surgery, Academic Medical Center, Amsterdam, the Netherlands); Igor C.J.B. van den Brand, MD, Suzanne de Vos-Jakobs, MD, Andy B. Spoor, MD, Taco Gosens, MD, PhD, Wahid Rezaie, MD (Department of Orthopaedic Surgery, Elisabeth-TweeSteden Ziekenhuis, Tilburg, the Netherlands; Department of Orthopaedic Surgery, Onze Lieve Vrouwziekenhuis, Aalst, Belgium); Dirk Jan Hofstee, MD, Bart J. Burger, MD, PhD (Department of Orthopaedic Surgery, Noordwest Ziekenhuisgroep, Alkmaar, the Netherlands); Daniel Haverkamp, MD, PhD (Department of Orthopaedic Surgery, Xpert Orthopedie, Amsterdam, the Netherlands); Anton M.J.S. Vervest, MD, PhD, Thijs A. van Rheenen, MD, Anne E. Wijsbek, MD (Department of Orthopaedic Surgery, Tergooi Hospital, Hilversum, the Netherlands); Ewoud R.A. van Arkel, MD, PhD, Bregje J.W. Thomassen, PhD (Department of Human Kinetics Technology, The Hague University of Applied Sciences, The Hague, the Netherlands); Sheila Sprague, PhD (Division of Orthopaedic Surgery, Department of Surgery, McMaster University, Hamilton, Ontario, Canada; Department of Health Research Methods, Evidence, and Impact, McMaster University, Hamilton, Ontario, Canada); Maurits W. van Tulder, PhD (Department of Health Sciences and EMGO Institute for Health and Care Research, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands); Mirjam Schavemaker, MD (Department of Radiology, Dijklander Ziekenhuis, Hoorn, the Netherlands); Rogier van Dijk, MD (Department of Radiology, Isala, Zwolle, the Netherlands); and J. van der Kraan, MsC (Netherlands Patients Federation, Utrecht, the Netherlands).
Final revision submitted July 1, 2020; accepted July 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for the ESCAPE trial was provided by the Netherlands Organization for Health Research and Development (ZonMw; grant 837002009), Zilveren Kruis (grant Z436), and the foundation of medical research of OLVG (grant 15u.025). The funders had no role in designing and conducting this study; the collection, management, analysis, and interpretation of the data; the preparation, review, and approval of the manuscript; or the decision to submit the manuscript for publication. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Medical Research Ethics Committees United (MEC-U).
References
- 1. Alghadir AH, Anwer S, Iqbal A, Iqbal ZA. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res. 2018;11:851–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barten JA, Pisters MF, Huisman PA, Takken T, Veenhof C. Measurement properties of patient-specific instruments measuring physical function. J Clin Epidemiol. 2012;65(6):590–601. [DOI] [PubMed] [Google Scholar]
- 3. Beaufils P, Becker R, Kopf S, Mattheiu O, Pujol N. The knee meniscus: management of traumatic tears and degenerative lesions. EFORT Open Rev. 2017;2(5):195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bellamy N. The WOMAC knee and hip osteoarthritis indices: development, validation, globalization and influence on the development of the AUSCAN hand osteoarthritis indices. Clin Exp Rheumatol. 2005;23(5)(suppl 39):S148–S153. [PubMed] [Google Scholar]
- 5. Beurskens AJ, de Vet HC, Kökeb AJ, et al. A patient-specific approach for measuring functional status in low back pain. J Manipulative Physiol Ther. 1999;22(3):144–148. [DOI] [PubMed] [Google Scholar]
- 6. Chatman AB, Hyams SP, Neel JM, et al. The Patient-Specific Functional Scale: measurement properties in patients with knee dysfunction. Phys Ther. 1997;77(8):820–829. [DOI] [PubMed] [Google Scholar]
- 7. Devji T, Carrasco-Labra A, Qasim A, et al. Evaluating the credibility of anchor based estimates of minimal important differences for patient reported outcomes: instrument development and reliability study. BMJ. 2020;369:M1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359(11):1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gauffin H, Tagesson S, Meunier A, Magnusson H, Kvist J. Knee arthroscopic surgery is beneficial to middle-aged patients with meniscal symptoms: a prospective, randomised, single-blinded study. Osteoarthritis Cartilage. 2014;22(11):1808–1816. [DOI] [PubMed] [Google Scholar]
- 10. Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A. Research Pearls. The significance of statistics and perils of pooling, part 1: clinical versus statistical significance. Arthroscopy. 2017;33(6):1102–1112. [DOI] [PubMed] [Google Scholar]
- 11. Herrlin SV, Hallander M, Wange PO, Weidenhielm L, Werner S. Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):393–401. [DOI] [PubMed] [Google Scholar]
- 12. Herrlin SV, Wange PO, Lapidus G, Hallander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):358–364. [DOI] [PubMed] [Google Scholar]
- 13. Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 14. Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kellgren J, Lawrence J. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ. 2016;354:i3740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Knottnerus AJ, Tugwell P. The patients’ perspective is key, also in research. J Clin Epidemiol. 2012;65(6):581–583. [DOI] [PubMed] [Google Scholar]
- 18. Manusco CA, Sculco TP, Wickiewicz TL, et al. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83(7):1005–1012. [DOI] [PubMed] [Google Scholar]
- 19. Pihl K, Roos EM, Nissen N, JøRgensen U, Schjerning J, Thorlund JB. Over-optimistic patient expectations of recovery and leisure activities after arthroscopic meniscus surgery. Acta Orthop. 2016;87(6):615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Roos EM, Roos HP, Ekdahl C, Lohmander LS. Knee injury and Osteoarthritis Outcome Score (KOOS): validation of a Swedish version. Scand J Med Sci Sports. 1998;8(6):439–448. [DOI] [PubMed] [Google Scholar]
- 21. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:J1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515–2524. [DOI] [PubMed] [Google Scholar]
- 23. Stevens A, Koke A, van der Weijden T, Beurskens A. Ready for goal setting? Process evaluation of a patient-specific goal-setting method in physiotherapy. BMC Health Serv Res. 2017;17(1):618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stevens A, Koke A, van der Weijden T, Beurskens A. The development of a patient-specific method for physiotherapy goal setting: a user-centered design. Disabil Rehabil. 2018;40(17):2048–2055. [DOI] [PubMed] [Google Scholar]
- 25. van Arkel ERA, van Essen A, Koëter S, et al. Artroscopie van de knie: indicatie en behandeling. Dutch Orthopaedic Association. Accessed September 1, 2018 http://www.orthopeden.org/
- 26. van de Graaf VA, Noorduyn JCA, Willigenburg NW, et al. Effect of early surgery vs physical therapy on knee function among patients with non-obstructive meniscal tears: the ESCAPE randomized clinical trial. JAMA. 2018;320(13):1328–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van de Graaf VA, Scholtes VA, Wolterbeek N, et al. Cost-effectiveness of early surgery versus conservative treatment with optional delayed meniscectomy for patients over 45 years with non-obstructive meniscal tears (ESCAPE study): protocol of a randomised controlled trial. BMJ Open. 2016;6(12):e014381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. van de Graaf VA, van Dongen JM, Willigenburg NW, et al. How do the costs of physical therapy and arthroscopic partial meniscectomy compare? A trial-based economic evaluation of two treatments in patients with meniscal tears alongside the ESCAPE study. Br J Sports Med. 2020;54(9):538–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. van de Graaf VA, Wolterbeek N, Scholtes VA, Mutsaerts EL, Poolman RW. Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am J Sports Med. 2014;42(6):1408–1416. [DOI] [PubMed] [Google Scholar]
- 30. Wright JG, Young NL. The patient-specific index: asking patients what they want. J Bone Joint Surg Am. 1997;79(7):974–983. [DOI] [PubMed] [Google Scholar]
- 31. Yim JH, Seon JK, Song EK, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41:1565–1570. [DOI] [PubMed] [Google Scholar]
- 32. Young IA, Cleland JA, Michener LA, Brown C. Reliability, construct validity, and responsiveness of the neck disability index, Patient-Specific Functional Scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil. 2010;89(10):831–839. [DOI] [PubMed] [Google Scholar]