Abstract
Objectives
This study aims to investigate if tranexamic acid (TXA) reduces both visible and hidden blood loss in patients undergoing total knee arthroplasty (TKA).
Patients and methods
A total of 128 female patients (mean age 68.9±5.8 years; range, 55 to 80 years) who underwent TKA and were admitted between January 2010 and January 2020 were included in this retrospective study. Only patients who had primary unilateral knee arthroplasty with a cemented posterior cruciate ligament substituting implant were included. Patients were divided into two groups according to TXA administration in the perioperative period. Group 1 consisted of patients who did not receive TXA (n=69), while Group 2 consisted of patients who received TXA (n=59). The effect of TXA on visible and hidden blood loss, amount of erythrocyte suspension transfusions, postoperative early wound complications, and the relationship between the volume of hidden blood loss and drainage volume were detected.
Results
There was no statistically significant difference between the groups in terms of age, body mass index, operation side, preoperative hematocrit (HCT) values, and total blood volume. Postoperative HCT values were statistically higher in Group 2. Fifty-four units of erythrocyte suspension transfusion were required in Group 1, while six units were required in Group 2 (p<0.001). Early wound complication was determined in 10 patients in Group 1 and only in one patient in Group 2 (p=0.011). Intraoperative blood loss, postoperative drainage volume, hidden blood loss, and total blood loss values were significantly lower in Group 2 (p=0.001). In all patients, there was a significant positive correlation between the postoperative drainage volume and the hidden blood loss volume (r=0.532, p=0.001).
Conclusion
The use of TXA in patients undergoing TKA reduces postoperative bleeding (visible and hidden blood loss), blood transfusion needs, and early wound complications. In addition, drainage volume in postoperative 24 hours can be used to estimate the amount of hidden blood loss in early postoperative period.
Keywords: Hidden blood loss, total knee arthroplasty, tranexamic acid.
Introduction
Symptomatic knee osteoarthritis is common among old people. Total knee arthroplasty (TKA) is regarded as the most effective treatment in relieving pain and restoring range of motion for patients with end stage osteoarthritis of the knee.[1] Despite the advances in surgical techniques, one of the issues that worries the surgeons is the blood loss after TKA operation.[2]
Various techniques are introduced to reduce postoperative blood loss in patients undergoing TKA.[3] One of them is antifibrinolytic treatment. Tranexamic acid (TXA) is a synthetic derivative of amino acid lysine which inhibits fibrinolysis by reversible blockade of lysine binding sites on plasminogen. It also inhibits the activation of plasminogen by plasmin activator.[3] As a result of lower plasmin levels, fibrinolytic activity is diminished, fibrin is not broken down, and thereby bleeding is decreased. The drug has no effect on other blood coagulation parameters such as platelet count, activated partial thromboplastin time, and prothrombin time.[4,5]
Total blood loss (TBL) due to TKA is the sum of visible and hidden loss. Visible loss is composed of intraoperative blood loss and blood volume collected in the suction drains (drainage volume). Hidden blood loss is the volume of blood that diffuses into tissues, residual blood in the knee joint cavity.[5,6]
In the literature, although various studies have determined the reducing effect of TXA on the visible blood loss, there is some controversy about the effect of TXA on hidden blood loss.[5,7-9] In some studies, the use of TXA in knee replacement patients has been reported to decrease external blood loss but not hidden blood loss.[7,8] The administration route, timing, and optimal dose of TXA in TKA are still controversial issues. Clinical variables may affect the efficiency of the drug. In this study, we aimed to investigate if TXA reduces both visible and hidden blood loss in patients undergoing TKA.
Patients and Methods
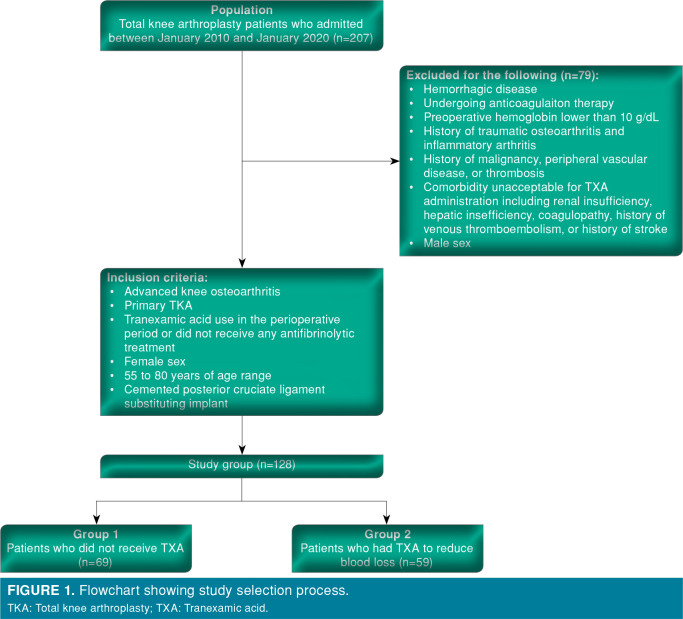
All TKA patients admitted between January 2010 and January 2020 at Ankara Numune Training and Research Hospital and Ankara City Hospital, Department of Orthopaedics and Traumatology were evaluated retrospectively. Inclusion and exclusion criteria were given in Figure 1. The study protocol was approved by the Ankara City Hospital Ethics Committee (No: E1-20-925, Date: July 16, 2020). A written informed consent was obtained from each patient. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Figure 1. Flowchart showing study selection process. TKA: Total knee arthroplasty; TXA: Tranexamic acid.
Tranexamic acid was not used due to clinical consensus in patients operated between January 2010 and September 2015; however, after September 2015, TXA was used in all TKA patients with a standard protocol.
Medical records of 207 patients were available for the study. Seventy-nine patients were excluded because they did not meet the inclusion criteria. A total of 128 patients (mean age 68.9±5.8 years; range, 55 to 80 years) were included. Patients were divided into two groups according to the use of TXA in the perioperative period. Group 1 consisted of patients who did not receive TXA (n=69), while Group 2 consisted of patients who received TXA to reduce blood loss (n=59).
All surgical procedures were performed by the same author team or one of the authors. In all patients, the following standard surgical technique was used:
First generation cephalosporin was used for prophylaxis which was administered intravenously 30 minute before inflation of the tourniquet and continued for 24 hours (1 g in every 8 hours). The operation was performed under spinal/epidural anesthesia. A tourniquet was used in all cases. The tourniquet was inflated 100 mmHg above the systolic blood pressure of the patients. Anterior midline skin incision and medial parapatellar arthrotomy were performed. Cemented posterior cruciate ligament substituting implant was used in all cases (Vanguard® complete knee system, Biomet Orthopaedics Inc., Warsaw, IN, USA). Patella was not changed but peripatellar osteophytes were removed and denervation was performed. The hole in the femur for intramedullary guide was occluded with an intramedullary bone plug to reduce bleeding from intramedullary canal after wound closure. The tourniquet was deflated after the prosthetic components were implanted and meticulous hemostasis was performed. A number 10-gauge drain was placed intraarticularly and connected to the drainage bottle. Intraoperative blood loss was measured by weighing the wet surgical gauzes. After wound closure, a compressive Robert Jones bandage was applied.[10] The drain was clamped for three hours after operation to provide hemostasis. After three hours, clamp was released and drainage started. Drains were removed 24 hours after the operation and the volume of blood collected in the drainage bottle was measured and recorded.
Tranexamic acid was administered 10 mg/kg intravenously before tourniquet deflation and then a second dose of 10 mg/kg was administered three hours after the operation.
For thrombosis prophylaxis, low molecular weight heparin 4000 IU was subcutaneously administered on operation evening and continued 4000 IU daily. Ambulation with partial weight bearing was permitted in the second postoperative day.
Age, operation side, early postoperative wound complications, amount of transfusion and body mass index (BMI) (kg/m2), preoperative, postoperative Day 1, Day 2, and Day 3 hematocrit (HCT) values, intraoperative blood loss, and postoperative drainage volume of the patients were collected from medical records retrospectively.
Total blood volume (TBV) was calculated by the Nadler[11] method as follows:
TBV=k1xH3+k2xW+k3
For females, k1=0.3561, k2=0.03308, and k3=0.1833; H=height (m) and W=weight (kg).
Total blood loss was calculated by Gross formula[6] method as follows:
TBL=TBVx(Preoperative HCT-Postoperative 3-day HCT)/Mean HCT
The volume of erythrocyte suspension (each one 200 mL) given to the patient was added to TBL separately.[6] Total hidden blood loss volume was calculated by subtracting visible blood loss volume from TBL volume.
Statistical analysis
Statistical analysis was carried out using the IBM SPSS for Windows 22.0 software (IBM Corp., Armonk, NY, USA). Descriptive statistics for numerical variables were expressed as mean and standard deviation. Parametric test procedures were used in the Kolmogorov-Smirnov test on normal distribution. Independent two-sample t-tests were used to determine the relationships between parameters. Chi-square analysis was also used to determine the relationship between categorical data. Mann-Whitney U test was used to evaluate the relationship between drainage volume and volume of hidden blood loss in patients using TXA. Correlation analysis between the volume of hidden blood loss and postoperative drainage volume was evaluated with Pearson correlation coefficient. The results were evaluated within the 95% confidence interval and p<0.05 was considered as statistically significant.
Results
The demographic data of the patients included in the study were shown in Table I. There was no statistically significant difference between the groups in terms of age, BMI, operation side, preoperative HCT and TBV (Table I).
Table 1. Demographic data of study patients.
| Group 1 (n=69) | Group 2 (n=59) | p | |||
| n | Mean±SD | n | Mean±SD | ||
| Age (year) | 68.7±5.9 | 69.3±5.6 | 0.544 | ||
| Body mass index (kg/m2) | 32.4± 3.9 | 31.9±3.8 | 0.457 | ||
| Side | |||||
| Right | 34 | 30 | |||
| Left | 35 | 29 | |||
| Preoperative hematocrit | 40.0±2.9 | 38.8±3.6 | 0.05 | ||
| Total blood volume (mL) | 3,938.0±311.5 | 3,821.8±367.7 | 0.055 | ||
| SD: Standard deviation. | |||||
Postoperative first day, second day, and third day HCT values were statistically higher in Group 2 (p=0.001, p=0.001, p=0.001, respectively) (Table II). Sixteen patients had one unit and 19 patients had two units of erythrocyte suspension transfusions in Group 1. However, in Group 2, four patients had one unit and one patient had two units of erythrocyte suspension transfusion. There was a statistically significant difference in transfusion amount between the study groups (p<0.001) (Table II). Early wound complication (edema, hematoma, serous drainage, and skin edge inflammation) was determined in 10 patients in Group 1 whereas only in one patient in Group 2 (p=0.011) (Table II).
Table 2. Comparison of groups according to hematocrit values, transfusion amount, and early complications.
| Group 1 (n=69) | Group 2 (n=59) | p* | |||
| n | Mean±SD | n | Mean±SD | ||
| Postoperative 1st Day HCT | 29.2±3.2 | 31.8±4.0 | 0.001* | ||
| Postoperative 2nd Day HCT | 26.7±2.8 | 30.0±3.6 | 0.001* | ||
| Postoperative 3rd Day HCT | 26.7±2.4 | 29.7±2.8 | 0.001* | ||
| Transfusion | <0.001* | ||||
| 1 unit | 16 | 4 | |||
| 2 unit | 19 | 1 | |||
| Early complication | 10 | 1 | 0.011* | ||
| HCT: Hematocrit; * p<0.05: statically significant difference. | |||||
When the groups were compared in terms of intraoperative blood loss, postoperative drainage volume, hidden blood loss, and TBL, the values of Group 2 were significantly lower (p=0.001) (Table III).
Table 3. Comparison of groups in terms of bleeding related parameters.
| Bleeding parameters | Group 1 (n=69) | Group 2 (n=59) | p* |
| Mean±SD | Mean±SD | ||
| Intraoperative blood loss (mL) | 222.9±87.4 | 132.6±41.6 | 0.001* |
| Postoperative drainage volume (mL) | 632.0±166.3 | 405.3±102.1 | 0.001* |
| Hidden blood loss (mL | 617.8±150.9 | 345.1±101.3 | 0.001* |
| Total blood loss (mL) | 1472.7±237.2 | 883.0±207.3 | 0.001* |
| * p<0.05: statically significant difference. | |||
Correlation analysis between postoperative drainage volume and the volume of hidden blood loss of all patients included in the study was evaluated. There was a significant positive correlation between the postoperative drainage volume and the hidden blood loss volume (r=0.532, p=0.001).
Discussion
The primary outcome of this study is that the use of TXA significantly reduces both visible and hidden blood loss in TKA patients. The transfusion amount and early wound complications were less in patients treated with TXA. The secondary outcome of the study is that the drainage volume in the first 24 hours after the operation has a statistically significant relationship with the volume of hidden blood loss.
Total blood loss for patients with osteoarthritis undergoing primary TKA ranges in between 1,300 to 1,500 mL.[6,7,12] Most of the patients are in old age with several co-morbidities. Their cardiovascular system may not tolerate such amount of blood loss and complications may arise.[6] Blood loss can be replaced by allogenic blood transfusions while this method has risks such as longer hospital stay, infection disease transmission, immunologic reaction, hemolytic and anaphylactic reactions, and increased mortality.[12]
In TKA, TBL is composed of visual loss and hidden loss. Visual loss is the intraoperative blood loss and the volume of drained blood. Hidden loss is the residual blood in the joint and the blood diffused into tissues. Sehat et al.[6] reported that the mean TBL in TKA patients was 1,474 mL. The mean visible loss was 739 mL, and mean hidden loss was 735 mL. Thus, the hidden loss was 50% of the TBL.[6] In their study which included 78 patients with primary osteoarthritis undergoing TKA, Iwai et al.[13] reported that the mean estimated TBL volume was 1,538 mL and the mean volume of hidden blood loss was 548 mL. Hu et al.[12] included 304 osteoarthritis patients undergoing unilateral primary TKA in their prospective study and indicated that TBL was 1,346±671 mL and hidden blood loss was 465±358 mL. As hidden blood loss is 35 to 50% of TBL, it has clinical importance and the volume of hidden blood loss needs to be estimated and strategies reducing hidden blood loss volume are required for postoperative blood management.
In major orthopedic surgical procedures, TXA is frequently used to reduce the amount of bleeding and the need for transfusion.[14-16] Authors have contrary opinions about the effect of the drug on hidden blood loss.[7,9,11] Good et al.[7] reported that 51 patients with osteoarthrosis who had unilateral cemented TKA received either placebo (n=24) or TXA 10 mg/kg (n=27) intravenously just before tourniquet release and three hours later. They reported that TXA decreased TBL by nearly 30% and drainage volume by 50%, while hidden blood loss was only marginally influenced and was at least as much as the drainage volume. In this case, TXA decreased external blood loss but not hidden blood loss in total knee replacement. Meta-analyses and prospective studies concluded that TXA significantly reduces hidden blood loss. Chen et al.[9] accomplished a meta- analysis including seven studies and 530 patients and concluded that TXA statistically significantly reduced hidden blood loss compared with the control group (patients without TXA). Furthermore, Huang et al.[14] included 108 patients who underwent TKA in their study. The patients were divided into two groups. In the experimental group, 15 mg/kg of TXA mixed in 100 mL normal saline was administered, while TXA was not used in control group. They concluded that both the measured and hidden blood losses were reduced in the experimental group compared with the control group (p<0.001). In the current study, mean TBL, visible blood loss, and hidden blood loss volume in patients without TXA (Group 1) were 1,472 mL, 854 mL, and 617 mL, respectively. However, mean TBL, visible blood loss, and hidden blood loss volume in patients with TXA (Group 2) were 883 mL, 537 mL, and 345 mL, respectively. The difference between the groups were statistically significant. Therefore, the use of TXA significantly reduced both visible and hidden blood loss in TKA patients. Hidden blood loss constitutes 41.91% of the TBL in patients without TXA and 39.07% in patients with TXA.
It has been reported that TXA reduces bleeding and the need for blood transfusion after TKA.[16,17] In addition, Liu et al.[17] reported that TXA improves recovery of knee function after TKA. Tranexamic acid is applied effectively and safely in topical, intravenous, and combined routes.[18] Although some studies have reported that there is no difference between methods in terms of safety and efficacy, some studies reported that the combined use is more effective.[18-20] In the current study, treatment with two doses of intravenous TXA provided decreased TBL, transfusion requirements, and early postoperative wound complications in patients with unilateral cemented knee arthroplasty. The results of the current study were compatible with the results published in the literature.[5,8,9,12]
Although visible blood loss in TKA patients can be easily detected clinically, there is no useful and easy method to predict hidden blood loss volume clinically in the literature. There are various methods for calculating hidden blood loss volume using postoperative third day HCT or Hb values.
However, postoperative first 24 hours is very important for the follow-up of TKA patients in terms of early postoperative bleeding. Hidden blood loss calculation made according to the blood values in the postoperative third day is not sufficient for early bleeding follow-up. Since hidden blood loss constitutes 39 to 42% of TBL, it is important to follow-up hidden blood loss postoperatively. For this reason, in this study, we evaluated the relationship between postoperative drainage volume and hidden blood loss and a positive correlation was found between postoperative drainage volume and hidden blood loss.
According to the significant positive correlation between the postoperative drainage volume and the hidden blood loss, drainage volume in postoperative 24 hours may be evaluated as a predictor of hidden blood loss volume. So, orthopedic surgeons may estimate the hidden blood loss volume and perform the postoperative blood management earlier.
The limitations of this study were its retrospective study design and being performed in a single center. However, early prediction of the amount of hidden blood loss in postoperative period may be a significant advantage. In addition, the standardization of patient sex and surgical method increases the strength of this study.
In conclusion, the use of TXA in patients with TKA reduces postoperative bleeding (visible and hidden blood loss), blood transfusion needs, and early wound complications. In addition, the amount of postoperative drain output in postoperative 24 hours can be used to estimate the amount of hidden blood loss in early postoperative period.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Choi YJ, Ra HJ. Patient Satisfaction after Total Knee Arthroplasty. Knee Surg Relat Res. 2016;28:1–15. doi: 10.5792/ksrr.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shen PF, Hou WL, Chen JB, Wang B, Qu YX. Effectiveness and safety of tranexamic acid for total knee arthroplasty: a prospective randomized controlled trial. Med Sci Monit. 2015;21:576–581. doi: 10.12659/MSM.892768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ido K, Neo M, Asada Y, Kondo K, Morita T, Sakamoto T, et al. Reduction of blood loss using tranexamic acid in total knee and hip arthroplasties. Arch Orthop Trauma Surg. 2000;120:518–520. doi: 10.1007/s004029900132. [DOI] [PubMed] [Google Scholar]
- 4.Boublik J, Atchabahian A. Tranexamic acid. In: Scott WN, editor. Insall & Scott Surgery of The Knee. Philadelphia: Elsevier; 2018. pp. 1071–1077. [Google Scholar]
- 5.Yang ZG, Chen WP, Wu LD. Effectiveness and safety of tranexamic acid in reducing blood loss in total knee arthroplasty: a meta-analysis. J Bone Joint Surg [Am] 2012;94:1153–1159. doi: 10.2106/JBJS.K.00873. [DOI] [PubMed] [Google Scholar]
- 6.Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty?. Correct blood loss management should take hidden loss into account. Knee. 2000;7:151–155. doi: 10.1016/s0968-0160(00)00047-8. [DOI] [PubMed] [Google Scholar]
- 7.Good L, Peterson E, Lisander B. Tranexamic acid decreases external blood loss but not hidden blood loss in total knee replacement. Br J Anaesth. 2003;90:596–599. doi: 10.1093/bja/aeg111. [DOI] [PubMed] [Google Scholar]
- 8.Chen X, Cao X, Yang C, Guo K, Zhu Q, Zhu J. Effectiveness and safety of fixed-dose tranexamic acid in simultaneous bilateral total knee arthroplasty: a randomized double- blind controlled trial. J Arthroplasty. 2016;31:2471–2475. doi: 10.1016/j.arth.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 9.Chen X, Zhu X, Yang S, Lin W, Wang L. Tranexamic Acid Treatment Decreases Hidden Blood Loss in Total Knee Arthroplasty. e1397-e405Am J Ther. 2016;23 doi: 10.1097/MJT.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 10.Brodell JD, Axon DL, Evarts CM. The Robert Jones bandage. J Bone Joint Surg [Br] 1986;68:776–779. doi: 10.1302/0301-620X.68B5.3782244. [DOI] [PubMed] [Google Scholar]
- 11.Li ZJ, Zhao MW, Zeng L. Additional dose of intravenous tranexamic acid after primary total knee arthroplasty further reduces hidden blood loss. Chin Med J (Engl) 2018;131:638–642. doi: 10.4103/0366-6999.226884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu Y, Li Q, Wei BG, Zhang XS, Torsha TT, Xiao J, et al. Blood loss of total knee arthroplasty in osteoarthritis: an analysis of influential factors. J Orthop Surg Res. 2018;13:325–325. doi: 10.1186/s13018-018-1038-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iwai T, Tsuji S, Tomita T, Sugamoto K, Hideki Y, Hamada M. Repeat-dose intravenous tranexamic acid further decreases blood loss in total knee arthroplasty. Int Orthop. 2013;37:441–445. doi: 10.1007/s00264-013-1787-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang PG, Jia XF, Xiang Z, Ji Y, Wu GY, Tang Y, et al. Tranexamic acid reduces hidden blood loss in patients undergoing total knee arthroplasty: A comparative study and meta-analysis. Med Sci Monit. 2016;22:797–802. doi: 10.12659/MSM.895571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sezgin EA, Atik OŞ. Are we scientifically ready to adopt tranexamic acid as a routine in arthroplasty. Eklem Hastalik Cerrahisi. 2019;30:338–339. doi: 10.5606/ehc.2019.19003. [DOI] [PubMed] [Google Scholar]
- 16.Atik OS. Does tranexamic acid reduce blood loss and blood transfusion requirement in knee arthroplasty. Eklem Hastalik Cerrahisi. 2012;23:166–167. [PubMed] [Google Scholar]
- 17.Liu W, Yang C, Huang X, Liu R. Tranexamic Acid Reduces Occult Blood Loss, Blood Transfusion, and Improves Recovery of Knee Function after Total Knee Arthroplasty: A Comparative Study. J Knee Surg. 2018;31:239–246. doi: 10.1055/s-0037-1602248. [DOI] [PubMed] [Google Scholar]
- 18.Çavuşoğlu AT, Ayanoğlu T, Esen E, Atalar H, Turanlı S. Is intraarticular administration of tranexamic acid efficient and safe as systemic administration in total knee arthroplasty. Single center, randomized, controlled trial. Eklem Hastalik Cerrahisi. 2015;26:164–167. doi: 10.5606/ehc.2015.33. [DOI] [PubMed] [Google Scholar]
- 19.Sun Q, Li J, Chen J, Zheng C, Liu C, Jia Y. Comparison of intravenous, topical or combined routes of tranexamic acid administration in patients undergoing total knee and hip arthroplasty: a meta-analysis of randomised controlled trials. e024350BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-024350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sridharan K, Sivaramakrishnan G. Tranexamic Acid in Total Knee Arthroplasty: Mixed Treatment Comparisons and Recursive Cumulative Meta-Analysis of Randomized, Controlled Trials and Cohort Studies. Basic Clin Pharmacol Toxicol. 2018;122:111–119. doi: 10.1111/bcpt.12847. [DOI] [PubMed] [Google Scholar]