Abstract
Immune hemolytic disease of the fetus and newborn is a condition in which there is the premature destruction of fetal or neonatal red cells due to maternal alloantibody against red cell antigen inherited from father. We report the case of Hemolytic disease of fetus and newborn (HDFN) due to anti-E and anti-Fya antibody. Blood grouping was done using the conventional tube technique. Rh and Kell phenotyping of the patient and her husband performed by column agglutination and Duffy phenotyping were done by the conventional tube technique. Direct antiglobulin test was performed by column agglutination technique. Antibody screening and identification were done. Anti-E and Anti-Fya were identified with titer of Anti-E: 1:64 and Anti-Fya: 1:256. The patient's neonate developed jaundice. Phototherapy was given. Bilirubin stabilized and discharged on the 12th day.
Keywords: Alloimmunization in pregnancy, hemolytic disease of the fetus and newborn, multiple alloantibodies
Introduction
Immune hemolytic disease of the fetus and newborn is a condition in which there is premature destruction of fetal or neonatal red cells due to maternal alloantibody against red cell antigen inherited from father. Anti-D is implicated as a major cause of HDFN. Other antibodies such as anti-K, c, e, E, C, Fya, and JK are also implicated in HDFN which can range from subclinical to active hemolysis requiring exchange transfusion. We report the case of HDFN due to maternal anti-E and anti-Fya antibody.
Case Report
A 24-year-old female Gravida 2 Para 1 at 34 weeks 5 days was referred to our hospital with anemia with Hb of 6.5 g/dl requiring blood transfusion but with multiple incompatible crossmatch. The patient had a history of one blood transfusion 2 years ago.
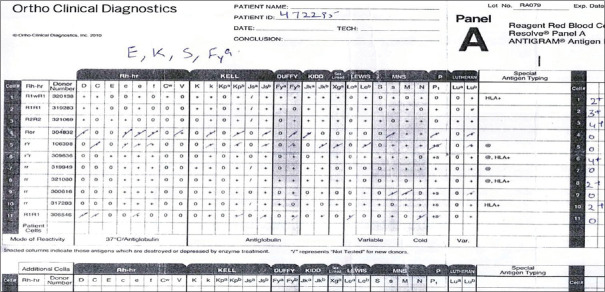
Blood grouping was done by conventional tube technique, and the patient was grouped as B Rh (D) Positive. The husband's blood group was O Rh (D). The direct antiglobulin test (DAT) was performed by column agglutination technique using a polyspecific orthoclinical diagnostic glass bead card and was negative. Antibody screening and identification were done using 0.8% ortho surgiscreen reagent red cells and 0.8% ortho resolve Panel A reagent red cells. The antibody screen showed positive reaction with cells 2 and 3 [Figures 1 and 2]. Antibody identification: eleven-cell identification panel resolve panel A (Ortho Clinical Diagnostics, Johnson and Johnson, USA) showed positive reactions with cells 1, 2, 3, 6, 8, and 10 which was suggestive of antibody against E, K, Fya, S antigens [Figures 3 and 4].
Figure 1.
Antigram showing antibody screen positive with 3 cell panel
Figure 2.

Showing antibody screen positive with 3 cell panel
Figure 3.

Showing antibody identification using 11 cell panel
Figure 4.
Antigram showing antibody identification using 11 cell panel
Four select cells(3, 5,6 7) from resolve Panel A (Ortho Clinical Diagnostics, Johnson and Johnson, USA) were used, confirming the presence of Anti-Fya and anti-E alloantibody and ruled out the presence of antibody against K and S antigens [Figure 5]. Antibody titer was found to be Anti-E: 1:64 and Anti-Fya: 1:256.
Figure 5.
Showing use of select cell for antibody identification
Rh and Kell phenotyping of the patient and her husband performed by column agglutination using ortho clinical diagnostic Rh/K cassette and Duffy phenotyping was done by the conventional tube technique.
Patient (DCe/DCe), K−, Fy (a−b+) [Figure 6]; husband (DCe/DEc), K-, Fy (a+b+) [Figure 7].
Figure 6.

Showing Rh/K phenotyping of the patient
Figure 7.
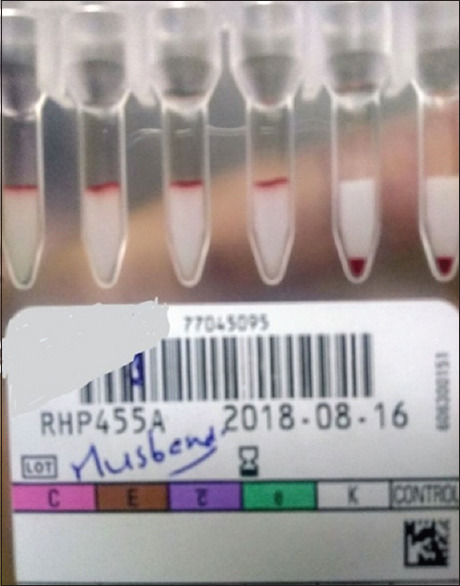
Showing Rh/K phenotyping of patient's husband
Twelve B Rh (D) positive red blood cell units were typed to find out E and Fya antigen negative unit, two units came to be E and Fya antigen negative. The patient was transfused with B Rh (D) positive E, K, Fya, c negative partial phenotype matched compatible donor unit.
Female neonate was delivered at 35 weeks by elective cesarean weighing 2.3 kg, Apgar score 10/10. The blood group of neonate was B Rh (D) positive. Direct Coombs test positive (4+) kept under observation. The child developed jaundice, with bilirubin of 11.4 mg/dl at 26 hrs, 13 mg/dl at 36 hrs, and 15 mg/dl at 48 hrs. Phototherapy was given. Bilirubin stabilized and discharged on the 12th day.
Antibody specificity causing hemolysis in the child could not be ascertained by elution due to the paucity of the sample received.
Discussion
With the availability of Rh immunoglobulin, the incidence of Rh D HDFN in Rh-negative females has decreased but maternal alloimmunization to other red cell antigens still remains a significant cause of HDFN as no prophylactic immunoglobulins are available to prevent these antibody formation. Sensitization to red cell antigens in females can occur during pregnancy or by blood transfusion.
Anti-E alloimmunization is frequently seen in pregnancy and associated with mild-to-moderate HDFN.
According to a study by Joy et al.,[1] a titer of 1:32 or greater was identified as critical titer of anti-E in the absence of previously affected fetus and warrants further evaluation. It predicted all cases of anemic fetus and newborns. However, a study by Moran et al.[2] in 62 infants with anti-E and positive DAT showed that anti-E can cause clinically significant HDFN but found no correlation between disease severity and antibody titers.
Chao et al.[3] reported a case of severe intrauterine hemolysis and neonatal death caused by anti-E alloimmunization with a titer of 1:1024 in the multiparous female with a history of previous perinatal loss. Strohm et al.[4] reported a case of severe HDFN with alloanti-E requiring multiple exchange transfusion with an antibody titer of 1:32.
Dávila et al.[5] reported a case of HDFN due to Fy incompatibility treated with phototherapy and exchange transfusion. Goodrick et al.[6] in a study of HDFN due to anti-Fya suggested that pregnancy in which anti-Fya is detected at significant titer (>64) should be closely monitored in a similar way to pregnancies where other significant antibodies are present.
In this case, the antibody titer of both alloantibodies was above the critical titer that is Anti-E: 1:64 and Anti-Fya: 1:256 and neonatal jaundice was managed with phototherapy alone.
To conclude, antibody screening should be done in all pregnant women and not restricted to RhD negative women or those with a past history of HDFN. Women of the reproductive age group should preferably be given transfusion with phenotypically matched blood, especially with blood group antigens capable of causing HDFN.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Joy SD, Rossi KQ, Krugh D, O'Shaughnessy RW. Management of pregnancies complicated by anti-E alloimmunization. Obstet Gynecol. 2005;105:24–8. doi: 10.1097/01.AOG.0000149153.93417.66. [DOI] [PubMed] [Google Scholar]
- 2.Moran P, Robson SC, Reid MM. Anti-E in pregnancy. BJOG. 2000;107:1436–8. doi: 10.1111/j.1471-0528.2000.tb11662.x. [DOI] [PubMed] [Google Scholar]
- 3.Chao AS, Chao A, Ho SY, Chang YL, Lien R. Anti-e alloimmunization: A rare cause of severe fetal hemolytic disease resulting in pregnancy loss. Case Rep Med. 2009;2009:471623. doi: 10.1155/2009/471623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strohm PL, Iams JD, Kennedy MS. Hemolytic disease of the newborn from anti-E. A case report. J Reprod Med. 1988;33:404–6. [PubMed] [Google Scholar]
- 5.Davila AA, Cruz DV, Roux M, Menendez RD, Rosales LC. Hemolytic disease of the newborn due to Duffy incompatibility: A case report. Revista Cubana de Pediatria. 2008:80. [Google Scholar]
- 6.Goodrick MJ, Hadley AG, Poole G. Haemolytic disease of the fetus and newborn due to anti-Fya and the potential value of Duffy genotyping in pregnancies at risk. Transfus Med. 1997;7:301–4. doi: 10.1046/j.1365-3148.1997.d01-38.x. [DOI] [PubMed] [Google Scholar]