Abstract
Introduction
Producing healthy physicians who act as a “healthy role-model” in their environment must be one of the concerns of medical schools today in response to the global movement of “health-promoting university” by the WHO (1995). However, no publications explained the “healthy role-model” in medical school. This study aimed to fill this gap by exploring the definition and characteristics of a “healthy role-model” for medical teachers.
Methods
We used a grounded theory approach with in-depth interviews and e-mail communications to 48 medical teachers from various backgrounds of “health professions education,” “health education and behavior”/’health education and promoter,’ “general practitioners/family medicine,” “adolescent health,” “internal medicine,” and “cardiology-vascular medicine.” The medical teachers were from Indonesia, one other developing country (Bangladesh), and five developed countries (United States of America, Canada, Netherlands, Australia, and United Kingdom). We also invited 19 medical students from Indonesia for three focus group discussions.
Results
We identified four categories to define a “healthy role-model” for medical schools as persons who are seen: 1) “physically,” “socially,” “mentally”, and “spiritually” healthy; 2) internalized healthy behaviors; 3) willing to promote healthy lifestyles; and, 4) a life-long learner. In each category, there are several characteristics discussed.
Conclusion
Our study provides some insights to define a “healthy role-model” of medical teachers by using the characteristics of healthy people and adult learners. The first category describes the characteristics of healthy people, but cultural issues influence the perspectives of medical teachers to define a “healthy role-model” for medical schools.
Keywords: healthy role-model, role-modeling, adult learner, grounded theory methodology
Introduction
The clause “I will attend to my own health, well-being, and abilities in order to provide care of the highest standard” in the modern-day physician’s pledge,1 emphasizes how medical schools have significant responsibilities to graduate professional physicians who are not only competent in the field of medicine but also are healthy people. Medical schools should provide an educational environment that guarantees the development of healthy physicians’ characteristics as optimally as possible. Medical teachers are the critical components of the educational environment.2 The first interaction when students arrive at medical school is with their teachers, and their relationship continues throughout the yearly collegial learning process. Therefore, the availability of medical teachers as a “healthy role-model” could be a practical approach to fulfill their responsibilities as medical professionals and educators.
Essentially, role-modeling is an effective learning method in medical education.3 The efficacy of role-modeling for the development of professional characters and behaviors has been proved in many publications.4–8 Medical teachers as a “healthy role-model” who should model healthy behavior might apply to the development of healthy physician characteristics in their medical students throughout the learning processes.6,9
However, based on the authors’ knowledge, publications in the area of “modeling healthy behavior” by medical teachers were not found. Most researches on healthy behavior are studied in the health education areas. Whereas, most studies in health professional education areas are focusing on “teaching and learning methods,” “assessment,” “curriculum development,” and “role-modeling,” but not “modeling healthy behavior.” The absence of theoretical concepts and limited standard criteria to define a “healthy role-model” and their characteristics have made identifying their availability difficult. Even though the term “healthy” was defined in the dictionary and the definition of health explained by the World Health Organization (WHO) in 1948, still, these are not enough to describe what characteristics a “healthy role-model” in medical schools should have. Accordingly, in this study, we explored the definition and characteristics of a “healthy role-model” for general medical schools using the grounded theory methodology.
Methods
Research Design
There is a lack of theoretical concepts about “healthy role-models in medical schools” and therefore, this study used the grounded theory approach by Corbin and Strauss.10 Our goal was to develop the definition and characteristics of a “healthy role model” in medical schools conceptually. We used semi-structured in-depth interviews, electronic mail (e-mail) communications in open-ended questions, and focus group discussions (FGDs) to support our data collection. We interviewed and communicated with 48 medical teachers (41 from Indonesia and 7 from other developed and developing countries) and FGDs with 19 medical students.
Setting and Participants
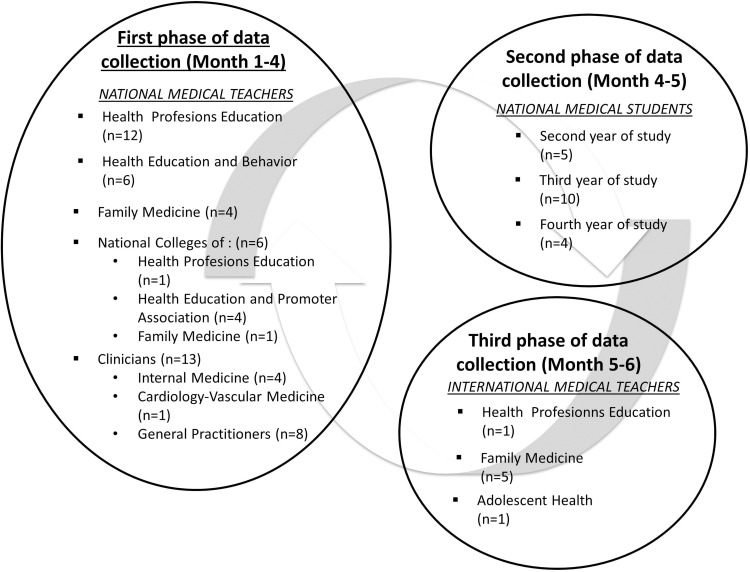
Originally, we recruited 41 medical teachers from different fields of medicine from Indonesia, and five developing (United States of America, Canada, Netherlands, Australia, and United Kingdom), and four from developed countries (India, Malaysia, Bangladesh, and Philippines). Medical teachers’ fields are: “health professions education,” “health education and behavior”/’ health education and promoter,’ “general practitioners/family medicine,” “adolescent health,” “internal medicine,” and “cardiology-vascular medicine,” were purposively invited in this study. We assumed that these field backgrounds are strongly related to “role-models” and the promoting healthy behavior by modeling that we were studying. The national medical teachers (Indonesia) are representatives of their departments or colleges and are recommended by their chairpersons. International medical teachers were coming from eight centers of excellence in primary care in five developed countries (United States of America, Canada, Netherlands, Australia, and United Kingdom) and one developing country (Bangladesh). Three medical teachers from other developing countries have not responded to our query. They were purposively invited in this study since they have similar background fields with our Indonesian participants. However, medical teachers’ recruitment from other countries outside of Indonesia was also done conveniently based on a close relationship with the authors’ institution. Figure 1 explains each representative sample of participants.
Figure 1.
Sample of participants of each data collection phases.
We selected medical students from the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada Yogyakarta. This medical school was the first in Indonesia that promoted itself as a “health-promoting campus.” Eligible medical students for the FGDs were in their second, third, and fourth years of study. We assumed that these students have enough knowledge to contribute comments on the definition and characteristics of a “healthy role model” in medical school that were defined by the national international medical teachers in this study. We added medical students for this study because they have been interacting with many medical teachers during their learning process, and thus can triangulate our data from the medical teachers. We excluded the first-year students because they were new entries to the medical schools when this study was conducted. We used a randomizer research software from the Social Psychology Network11 to randomly select medical students who were invited to participate.
Data Collection and Procedure
Data collection was conducted from September 2018 to February 2019. We used a list of guiding questions: 1) What is the definition of a “healthy role-model” in a medical school?; 2) Do medical schools need a “healthy role-model”?; 3) Who could be expected as a “healthy role-model” in medical schools?; 4) What characteristics must they have as a “healthy role-model” in a medical school?; and, 5) Should all of the characteristics described be visible in a “healthy role-model,” or is there one that must be more prominent than others? We used the positive doctor role modeling concept described by Passi et al12 and healthy person characteristics by Hoye et al13 to develop these questions. Each question was further probed by using “What,” “Why,” or “How” questions.
Data collection was done in three phases. First, in-depth interviews and e-mail communications in open-ended questions were conducted with medical teachers in different fields of medicine from Indonesia. Second, FGDs were conducted with medical students at the Faculty of Medicine, Public Health and Nursing, Gadjah Mada University Yogyakarta. Third, e-mail communications concerning the open-ended questions were conducted with international medical teachers.
A professional interviewer who works as an anthropologist, and had experience in conducting qualitative research, conducted the first two interviews in the first phase of data collection. The first author observed these interview sessions. At the end of each session, the first author was given a chance to lead the interview, while the professional interview observed the process. Feedback was given after each session. In the third interview session, the first author led the interview while a professional interviewer acted as an observer. The first author again got feedback after the session. The professional interviewer then allowed the first author to conduct the next interview session independently. Next, the first author conducted all FGDs with medical students. All participants were invited formally by the first author. The agreement of time and place to conduct the interviews or FGDs was communicated between the first author and participants.
In all of the interviews and FGDs sessions, because the term “healthy role-model” was new in medical school, the interviewer explained the term of a healthy person and role model in medical school before starting the interview. When no more questions about the term arose, the first author began the interviews and FGDs. All in-depth interviews lasted 25–60 minutes, while FGDs lasted approximately one hour. All of those were audio-recorded and transcribed verbatim. We anonymized all transcripts.
In e-mail communications, all participants were given 20 days to reply counting from the first-day the e-mail was sent. We reminded all participants who did not reply to the e-mail three days before the deadline. By sending their response, we assumed the medical teacher agreed to participate in this study.
Data Analysis
After each in-depth interview or focus group discussion session was conducted, the first author directly listened to the recording. A transcriber service agent transcribed all transcripts. The first author examined all transcripts by checking line by line to see the congruence between the transcripts and recordings. The recordings and transcripts were used to conduct reflections and guide the next sessions of the in-depth interviews and FGDs. We followed the steps of grounded theory by Straus and Corbin in analyzing our data.10,14
Open coding, in this first step of grounded theory methodology (GTM),10,14 the first author invited two independent coders. All transcripts, recordings, and e-mail communication responses of participants were sent via e-mail because all coders lived in different cities. Each coder conducted open coding independently, then discussed it via phone. The open coding was done with the following steps. First, the reading line by line of all statements of participants was conducted iteratively. Second, making “in vivo coding” from a line by line open coding which was conducted previously. Third, underlining the keywords of each statement that were chosen and writing this statement in short sentences without eliminating the main idea of what the participants want to inform. Fourth, comparing the coding, which was recently made with the coding list that was obtained from the previous coding consistently (constant comparation), and making a new coding if there was no suitable coding with the coding list. Fifth, writing the participant’s statement as a quotation for every coding to explain coding that was made. All coders wrote a memo during open coding that would be discussed with other coders in axial and selective coding sessions. This memo was also useful for reflection.
List of categories and subcategories from the participants in the first phase of data collection were compared with emerging categories and subcategories from the participants in the second phase. These categories and subcategories were used to enhance our list of categories and subcategories that emerged from the first phase. The categories and subcategories that emerged from FGDs might also be critical because it represents the characteristics that medical students want to model from their teachers who are’ “healthy role-models.” Finally, we used categories and subcategories from participants in the third data collection phase to complete our list.
Axial coding, in this second step of GTM, all coders discussed all categories and subcategories found in the open coding step. In the third step of GTM, selective coding, all coders tried to find the main category of definition and characteristics of a “healthy role-model” in medical schools. Theoretical sampling is the next step of data analysis of GTM, which was done by the recruitment of medical students in the second phase and international medical teachers from several developed and developing countries in the third phase of data collection.
All analysis processes were done iteratively, constantly collecting, coding, constantly comparing, and interpreting based on the GTM approach until there was not any new category, nor subcategory that emerged. The differences between coders were solved through discussion. No new categories and subcategories emerged after we analyzed 24 in-depth interviews, seven responses in e-mail communication, and two FGDs sessions. The remaining transcripts and responses in e-mail communication in open-ended questions were used to ensure data saturation.
The coding results were then discussed with the other authors. Differences in interpretation were discussed until consensus was reached. Memos and documents from the coding steps of all coders were kept by the first author and checked by the second and third authors. The quotations were also checked whether they describe completely the category and subcategory that were represented.
Trustworthiness
Triangulation of the study population (national and international medical teachers from different fields in medicine and medical students), triangulation of study methods (in-depth interviews, FGDs, and e-mail communication with open-ended questions), and triangulation of three data collection phases were used to increase the credibility of this study. Member-checking was also done by sending the analytic results back to all participants to get their feedback. We provided thick descriptions to allow readers to determine whether the findings were transferable to their context. The results of coding data by three coders were sent to the two Co-authors. They conducted an audit trail to ensure that the analysis was grounded in the data; thus, this study’s dependability could be maintained. To ensure this study’s conformability, the two Co-authors conducted an audit trail to check the primary researcher’s detailed procedural records. These records helped us to assess and ensure the accuracy of these findings based on the participants’ perspectives’ truthfulness.
Results
We conducted 35 semi-structured in-depth interviews, 13 e-mail communications with open-ended questions, and 3 FGDs sessions. Table 1 shows the participants’ characteristics in this study.
Table 1.
The Characteristics of Participants in This Study
| The Phase of Data Collection | Field of Medicine | n |
|---|---|---|
| First phase of data collection (national medical teachers) | Health Profession Education | 13 |
| Health Education and Behavior/Health Education and Promoter Association | 10 | |
| Family Medicine | 5 | |
| Internal Medicine | 4 | |
| Cardiology-Vascular Medicine | 1 | |
| General Practitioners | 8 | |
| Second phase of data collection (national medical students) | Session 1 (Third year medical student) | 10 |
| Session 2 (Fourth year medical student) | 4 | |
| Session 3 (Second year medical student) | 5 | |
| Third phase of data collection (international medical teachers) | Health Profession Education/Medical Education | 1 |
| Family Medicine | 5 | |
| Adolescent Health | 1 |
Four defining categories for “healthy role-model” in medical schools emerged. All participants stated that all members of medical schools, ie, teachers, students, and staff, should act as “healthy role-models.” Nevertheless, all participants agreed that medical teachers are the first and critical people to be a “healthy role-model” in medical schools.
A “healthy role-model” in a medical school is a person who is seen as: 1) physically, socially, mentally, and spiritually healthy; 2) internalized healthy behaviors in their life; 3) willing to promote healthy lifestyles; and 4) life-long learner. Furthermore, the characteristics of “healthy role-model” in medical schools were explained in terms of the physical, mental, social, and spiritual aspects of health. One category that is “spiritually healthy” did not emerge from overseas participants. All of these characteristics must be observable. We summarize these characteristics in Appendix 1 and explain them in more detail below with quotations.
Definition and Characteristics of “Healthy Role-Model” in Medical Education Institutions
Category 1: Physically, Socially, Mentally, and Spiritually Healthy
A “healthy role-model” in medical schools must have balance in showing four aspects of health in their life: physical, social, mental, and spiritual. These characteristics should be seen by other medical colleagues, students, and staff. All participants described these characteristics by using the WHO health definition. Participants from Indonesia added spiritually healthy as written in the definition of the Law of Republic of Indonesia No. 36 of 2009. The presence of cultural values, ie, norms, ethics, and religious values, also influences the characteristics of a “healthy role-model” in medical schools.
Subcategory 1: Physically Healthy
In physical aspects, a “healthy role-model” in medical schools are people who have: good physical appearance; ideal body weight and height; enthusiasm and healthy face; good stamina; ability to do their activity without limitation caused by disease; adopted healthy behaviors to maintain their physical health, ie, having routine physical exercise, no overeating, eat fruits and vegetable daily, drink water, not smoking, not addicted to alcohol nor drugs, routine medical checkup once every year, and are aware of any disease risk due to genetics or work environment.
For the ‘healthy role-model,’ we should demonstrate our healthy lifestyle: no smoking, no drugs, limited medication, limited use of alcohol, attention for our weight, daily activity/sports […] (IMT05)
As a healthy role model, he must know a healthy behavior, have a routine physical exercise, not smoking, not an alcoholic user, and other behavior that could harm his health […] (NMT11)
[…] when he was healthy, he was energetic, […] and during the teaching session, he seems with preparation and not lack of sleep […] (NMS02)
Subcategory 2: Mentally Healthy
In mental aspects, a “healthy role-model” in medical schools are people who are: happy, low profile person, productive, hard-worker, a fun person whom others feel comfortable around, positive thinkers, honest, and brave to remind others when they practice unhealthy behavior in a healthy environment. They also know their self-limitations, never feel excessive euphoria, do not become stressed or depressed, have excellent emotional management, make priorities, have specific goals to achieve, use excellent coping skills, have good time management skills, show respect and are satisfied with their life, practice a routine of self-reflection, have a proper sleep during rest time, and pleasant attitude and work ethic.
If we are finding it challenging to manage crises and consumed with just getting through each day, we can review our priorities. It takes time and sometimes courage to push back and say ‘no,’ but it is crucial to be somewhat ruthless in allocating time to what is most important to us at work and home. (IMT04)
[…] when you are healthy, you are happy and productive. (NMT16)
[…] if mentally healthy, it can be seen when they have a problem, they respond not excessively [.] they still can try to cover it up. (NMS03)
Subcategory 3: Socially Healthy
In social aspects, a “healthy role-model” in medical schools are people who: respect others, use technology to share only trusted information, make friends without discriminating, support others’ self-development, eg, by sharing tips on how to succeed in adopting healthy behavior, create safe environment for others, eg, by giving constructive feedback, obedient to norms, ethics, and policy in society and environment, work as a team, practice empathy, compassion, and altruism, and live a healthy and good relationship with their partner.
[…] We need to demonstrate empathy and a healthy outlook toward our jobs. You cannot do an excellent job if you are distracted by problems. If we are depressed, it is hard to care for other people compassionately. (IMT03)
[…] He can make a good relationship with people, do not like to be discriminative, not prejudiced […] respect others […] (NMT01)
[…] in a tutorial session, sometimes there were lecturers judged us with a statement like ‘how you came without learned anything’ […] that is making us uncomfortable. (NMS01)
Subcategory 4: Spiritually Healthy
In spiritual aspects, a “healthy role-model” in medical schools are people who: have an excellent vertical relationship with God in their beliefs, eg, having prayer time, entrusting their life to God, teaching life lessons to others based on their experiences, and implementing the right teachings in their religion by acting with kindness toward others.
Sometimes, when we got stressed […], we must believe that there is another power besides ourselves. For example, when someone suffers the final phase of cancer, if he did not believe that there is another power besides his power, it is easier to get stressed. (NMT15)
[…] some of the medical teachers give an example during their teaching on how we have a good relationship with God; instead, we were healthy. (NMS02)
Category 2: Internalized Healthy Behavior
To internalize healthy behavior in their life, a “healthy role-model” in medical schools should: 1) adopt healthy behaviors consistently and continuously in their life, not only follow a particular health trend; 2) make health a basic need of their life, so they have self-motivation to be healthy and always creative to conduct healthy behavior regardless of any limitations they have; and, 3) have self-regulation to prevent the adoption of unhealthy behavior.
No smoking, limited use of alcohol, and active life are the most important. Perseverance is essential to show the determination to try, as that will also be the same for patients. If they see and understand that their doctor also keeps trying, they will feel better understood. (IMT05)
[…] She adopts healthy behavior in her life, e.g., having physical exercise every day, eating healthy food[…]I remembered that I saw her walked from one building to another building for many times in that day[…]and when we met, she was smiling and said: Well, I could not take my physical activity session this morning!’ Wow, she pushed herself to fulfill her passion for being healthy […] (NMT07)
When I saw one teacher was smoking […], I did not see him as ‘a healthy role model’ because ‘a healthy role model’ in my mind is someone who can know that what he did is right or wrong. (NMS01)
Category 3: Willing to Promote Healthy Lifestyles
A “healthy role-model” in medical schools should: 1) commit to inviting other people in practicing healthy behavior, eg, by sharing their stories about conducting healthy behavior; 2) teach healthy behavior that is feasible to adopt by others; and 3) conduct health research which benefits their environment. Therefore, they are considered the right person to consult when people struggle to adopt healthy behavior.
Inspiring others to seek their mighty purposes[…] (IMT04)
A person who wants to promote it, e.g., tell people around him that he brings his drink bottle wherever he goes, he prefers to walk than to drive to go to another building around him. That has inspired us […] This person always invites people around him to try the same thing as he does. That is all we need. (NMT03)
[…]my physiological teacher did not only understand what they teach, but they also share their stories in detail and motivate me to have a physical exercise in maintaining my health. (NMS03)
Category 4: Life-Long Learner
As a “healthy role-model” in medical schools, they are knowledgeable about healthy behavior they adopt and what diseases are prevented by doing that behavior.
Q: What characteristics must they have as ‘healthy role-model’ in medical schools?
R: Intellectual curiosity, continuing self-education. (IMT01)
[…] they must have a knowledge of what healthy behavior they do and what disease they can prevent by doing such behavior (NMT11)
Discussion
Based on these findings, a “healthy role-model” for medical schools characterizes both of the characteristics of a “healthy person” and “adult learner.” The first characteristic of “healthy role-model” for medical schools found in this study described that they must be seen as a person who is physically, socially, mentally, and spiritually healthy. This characteristic is mostly similar to healthy people’s characteristics in the study done by Hoye et al.13 They conducted an exploratory study to investigate how nursing students in Indonesia and Scandinavia characterize a healthy person. Five categories emerged to characterize a healthy person, ie, having a strong and positive body image, feeling well and having inner harmony, following the rules of life, coping with challenges, and acting in unison with the environment, according to their study. The categories in their study were different from our findings. However, many codes in their study explained similar aspects with our findings. For example, strong body, perfect body image, coping with everyday life, being proactive, positive attitude to life, self-presentation in the environment, etc., which were also found in this study.
A spiritual aspect of health which emerged in this study was also similar to Hoye et al.13 In their study, Hoye et al13 found that only Indonesian students expressed anything about spirituality and religion in connection with health by describing “being obedient to God” (”a person who believes in God and always follows God’s law” and being “thankful to God”). We also found that overseas participants in this study did not mention about spiritually healthy. Therefore, these findings justified that cultural perspective could take into account all aspects of human experience, including health.15 The spiritual aspect was also not mentioned in health definition by WHO in 1948. Possibilities to explain the different views between our respondent from Indonesia and overseas is by understanding that Indonesian society is mainly religious. By using one of the six dimensions of Hofstede’s model,16,17 Indonesia has a high scoring of long-term orientation dimension, which explains that Indonesia has a pragmatic society. Hofstede’s model has six dimensions, ie, power distance, uncertainty avoidance, individualism versus collectivism, masculinity versus femininity, long-term versus short-term orientation, and indulgence versus restraint in order to distinguish different countries’ culture from each other. Societies that score high on long-term orientation dimension take a more pragmatic approach: they maintain some links with its past while dealing with the challenges of the present and future. Indonesians believe that important events in life will occur in the future; they believe in the next life after death and the need to have a good spiritual life. Therefore, they prepare for it while keeping balance with other health aspects. The spirituality of people has a positive effect on their health. Koenig18 conducted a systematic review of the relationship between religion/spirituality and both mental health and physical health. The term “religion” and “spirituality” in their study have a very similar definition, and there is overlap. Thus, they used term religion and spirituality interchangeably (ie, religion/spirituality). The majority of studies report significant relationships between religion/spirituality and better health. First, religion/spirituality involvement has a favorable impact on a host of physical diseases and the response of those diseases to treatment. Second, religion/spirituality is related to better mental health (less depression, lower stress, less anxiety, greater well-being, and more positive emotions). Third, religion/spirituality promotes better health behaviors (less alcohol and drug use, less cigarette smoking, more physical activity and exercise, better diet, and safer sexual practices). Fourth, religion/spirituality boosts supportive social interactions and increases community trust and involvement. The religion/spirituality beliefs and doctrines encourage the development of human virtues such as honesty, courage, dependability, altruism, generosity, forgiveness, self-discipline, patience, humility, and other characteristics that promote social relationships. Participation in a religion/spirituality community also increases the flow of health information by promoting healthy behavior.
The next three characteristics were related to the adult learner which is described by Knowles et al.19 Knowles postulates that adult learners differ from learning in child learners in six respects: the need to know (Why do I need to know this?); 2) the learners’ self-concept (I am responsible for my own decisions); 3) the role of the learners’ experiences (I have experiences which I value, and you should respect); 4) readiness to learn (I need to learn because my circumstances are changing); 5) orientation to learning (learning will help me deal with the situation in which I find myself); and 6) motivation (I learn because I want to). The second characteristic of a “healthy role-model” for medical schools as a person who internalized healthy behaviors in life is related to the learner’s self-concept (I am responsible for my own decision) and motivation (I learn because I want to) in adult learner characteristics. An adult person realizes that health matters are their responsibility.20,21 Therefore, they make health as their primary need and resources of everyday life by motivating themselves to adopt healthy behaviors consistently in their daily life.
Practicing healthy behaviors consistently is not only maintaining a “healthy role-model” health but also, they will then invite other’s attention to observe their behavior. Attention is an initial step in the modeling process. Their presence in the environment as a social prompt can increase others’ self-efficacy22 and lead to healthy behavior change through modeling. The modeling is a learning process where people need to put attention toward observing another’s behavior, then they store the information from their observation, reproduce that behavior, and finally motivate themselves to produce that behavior continuously. This process is explained by Bandura23 in his social cognitive theory.
The third characteristic of a “healthy role-model” for medical schools as a person who has willing to promote healthy lifestyles could also be related to the role of the learner experience (I have experience which I value or which I reflect) in adult learner characteristics.19 A “healthy role-model” should realize that health does not belong to themselves. Making an environment healthier is not a personal matter. Therefore, they need to share their experiences to help others become healthier in an attempt to achieve collective efficacy for creating the environment that can be healthier.20,21 As a medical teacher, they should realize their roles as an information provider23 not only for their patients but also for their students. Therefore, they should be aware of their characteristics and behaviors in formal and informal sessions of teaching and learning because it could influence their students’ characteristics.6,24,25 This argument was also explained by most of our participants in this study. They explained that the medical teacher is the main person for being a “healthy role-model” because they are learning centers for students and staff in a medical school. Therefore, being aware that their characteristics would be modeled by their students is an essential aspect that medical teachers have in their role as medical educators. They should only characterize the characteristics that they want their students to have as future physicians.
The fourth characteristic of a “healthy role-model” for medical schools is a life-long learner. This characteristic is related to readiness to learn (I need to learn because my circumstances are changing), orientation to learning (learning will help me deal with the situation to which I find myself), and motivation (I learn because I want to). As a critical person in the educational environment in medical school, medical teachers should be the right person for consultation when others meet a problem in doing some healthy behavior. By practicing healthy behavior, medical teachers accumulate a growing reservoir of experience on doing the healthy behaviors. A “healthy role-model” has real experience in doing some of the healthy behaviors. Then, there is a process of reflection and abstraction (separation of aspects that have value and those that do not), translating what is understood to be a principle and testing their understanding of a new situation in doing that healthy behavior. These processes are explained by Kolb25 in his theory about experiential learning.
All of these characteristics must be observable by others in order for the modeling process can occur. By using the social cognitive theory by Bandura,23 we can better understand this mechanism, which was explained above. All of these characteristics are not beneficial if these characteristics are unobservable in a medical teacher who acts as a “healthy role-model.”
We realized that finding these “ideal” medical teachers with all of these characteristics is challenging, primarily when it is expected must be characterized by all medical teachers in one medical school. Also, we realized that if we insist that all of those characteristics must be seen in all medical teachers, it will cause some undesired outcomes. The medical teachers who have a physical limitation caused by increasing age or chronic disease, for example, might have no chance of being healthy role models in medical school. To prevent this outcome from happening, most of our participants explained that those medical teachers can still be healthy role models in medical school. Because how they live with their limitation and having a regular activity by behaving in a healthy way makes them deserve to be categorized as healthy role models in medical school. Even though it is hard to find all of these characteristics in one medical teacher, it is possible. Therefore, we need further study to explore the minimum of these characteristics to categorize medical teachers as healthy role models in medical school.
However, a future study can also use characteristics in this study to find the ideal, or optimum, medium, or less healthy role models in medical schools and explore what the persons do for maintaining healthy behavior and role-modelling it. As a result, their “healthy behavior” can inspire the medical students and all “civitas academica” on campus.
By these findings, we suggested that these characteristics of a “healthy role-model” should complement the characteristics of “positive role-model” in a medical school, which was described by Passi et al.12 Our findings give a brief description about each aspect of health in the original definition according to the WHO. Therefore, by these findings, we could understand that to define a healthy person is not mainly focused on physical characteristics which are easy to observe but includes many intangibles.
Limitations
Although this study is the first grounded theory to explore the definition and characteristics of a “healthy role-model” for medical schools, it also has some limitations. First, “health” in spiritual aspects only emerged from Indonesian participants. Thus, readers must be careful to interpret this finding to another context that has a different culture from Indonesia. This difference emerged as an exciting issue about the influence of cultural dimensions, which should be investigated in the future. Second, FGDs were conducted with undergraduate medical students who have not had a clerkship experience. The difference in educational environment between medical students in undergraduate and clerkship program might be influencing their perceptions of a “healthy role-model” for medical school, which must be investigated in the future. Third, the recruitment of international medical teachers was done conveniently. However, they included world leaders in their fields and not just individual medical teachers. All of them have an essential position in their field background. Thus, they can represent worldwide perspectives of global health care.
Conclusions
Our study provides a detailed and complete picture of the definition and characteristics of a “healthy role-model” for medical schools—these characteristics are related to a healthy person and adult learners’ characteristics. Spirituality emerged in the definition and characteristics of a “healthy role model” for medical schools but might only be suitable for certain cultures. This finding may be useful as a theoretical concept to develop an instrument to assess healthy role models’ characteristics in our medical teachers today. More studies are needed to determine the minimal characteristics of a healthy role model in medical school to prevent any undesired outcomes, including the stigmatization of our medical teachers’ mental or physical limitations that could cause them not to be categorized as a healthy role model in medical school.
Acknowledgments
The authors wish to thank all participating medical teachers from Health Profession Education, Primary Care, Health Promotion and Behavior, and Clinician from Internal Medicine and Cardiology–Vascular Medicine in Indonesia. We wish to thank the medical students in the Faculty of Medicine, Public Health, and Nursing Universitas Gadjah Mada, Indonesia, for their time and opinions to provide us valuable insights on this topic. We also express our appreciation to all medical teachers in Primary Care, Medical Education, and Adolescent Health from developed and developing countries who participated in this study, ie, Professor Mark Graber at the Department of Family Medicine at The University of IOWA, USA, author of the Family Medicine book that has been translated into many languages; Professor Job Metsemakers at Department of Family Medicine Maastricht University, Netherlands, past President of WONCA Europe Association of Family Doctors; Professor Susan Sawyer at Department of the Pediatric/Adolescent Health University of Melbourne, Australia, President of the Lancet Commission of Adolescent Health; Professor Michael Kidd at Department of the Family Medicine University of Toronto, Canada, past President of WONCA World Association of Family Doctors; Professor Warren Rubeinsten, past Head of Department of Departement of Family and Community Medicine Univ. of Toronto Canada; Professor Amanda Howe at Department of General Practice Univ. of Eastern Anglia, Norwich, UK, past President of WONCA World Association of Family Doctors; and, Professor Humayun Takluder at SEARAME Council/Medical Education, Bangladesh. All authors also extend our thanks to Mrs. Onengan Caturanggani, S. Sos, who helped in conducting two in-depth interview sessions and helped the first author to conduct the next in-depth interview independently. We also thank Murti Mandawati, SKep, Ns, MMedEd, and drg. Cicih Bhakti Purnamasari, MMedEd, who helped as coders.
Funding Statement
The Ministry of Research, Technology, and Higher Education (Indonesia) funded this research.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
This study was approved by The Medical and Health Research Ethics Committee Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Indonesia, under their file number 0946. The aim and process of data collection were well explained to participants. The written informed consent was obtained from participants before they took part in this study, and the participants’ informed consent included the publication of anonymized responses. All procedures performed in this study were following the principles stated in the Declaration of Helsinki and the institutional research committee’s ethical standards.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflict of interest. The authors alone are responsible for the content and writing the article.
References
- 1.Online Archieve of WMA Declaration Of Geneva. 2017. World Medical Association; Available from: https://www.wma.net/policies-post/wma-declaration-of-geneva/&pdfName=wma-declaration-of-geneva. Accessed March27, 2019. [Google Scholar]
- 2.McAleer S, Roff S. Educational environment In: Dent JA, Harden RM, editors. A Practical Guide for Medical Teachers. 4th ed. London: Elsevier; 2013:392–399. [Google Scholar]
- 3.Ficklin FL, Browne VL, Powell RC, Carter JE. Faculty and house staff members as role-model. J Med Educ. 1988;63(5):392–396. [DOI] [PubMed] [Google Scholar]
- 4.Paice E, Heard S, Moos F. How important are role-model in making good doctors? BMJ. 2002;325(7366):707–710. doi: 10.1136/bmj.325.7366.707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kenny NP, Mann KV, MacLeod H. Role-modelling in physicians’ professional formation: reconsidering an essential but untapped educational strategy. Acad Med. 2003;78(12):1203–1210. doi: 10.1097/00001888-200312000-00002 [DOI] [PubMed] [Google Scholar]
- 6.Stern DT, Papadakis M. The developing physician-becoming a professional. N Engl J Med. 2006;355:1794–1799. [DOI] [PubMed] [Google Scholar]
- 7.Cruess SR, Cruess RL, Steinert Y. Role-modelling-making the most of a powerful teaching strategy. BMJ. 2008;336:718–721. doi: 10.1136/bmj.39503.757847.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kahn MW. Etiquette-based medicine. N Engl J Med. 2008;358(19):1988–1989. doi: 10.1056/NEJMp0801863 [DOI] [PubMed] [Google Scholar]
- 9.Coulehan J. Viewpoint: today’s professionalism: engaging the mind but not the heart. Acad Med. 2005;80(10):892–898. doi: 10.1097/00001888-200510000-00004 [DOI] [PubMed] [Google Scholar]
- 10.Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 3rd ed. USA: Sage Publication Inc; 2008. [Google Scholar]
- 11.Urbaniak GC, Plous S. Research randomizer [Computer software] Version 4.0. 2013. Available from: https://www.randomizer.org/. Accessed April1, 2018.
- 12.Passi V, Johnson S, Peile ED, Wright S, Hafferty F, Johnson N. Doctor role-modelling in medical education: BEME Guide No. 27. Med Teach. 2013;35(9):e1422–36. doi: 10.3109/0142159X.2013.806982 [DOI] [PubMed] [Google Scholar]
- 13.Hoye S, Kvigne K, Aiyub I, et al. A healthy person: the perceptions of Indonesian and Scandinavian nursing students. Glob Qual Nurs Res. 2016;3:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park (CA): SAGE; 1990. [Google Scholar]
- 15.Kleinman A, Benson P. Anthropology in the clinic: the problem of cultural competency and how to fix it. PLoS Med. 2006;3(10):e294. doi: 10.1371/journal.pmed.0030294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hofstede G. Dimensionalizing cultures: the Hofstede model in context. Online Readings Psychol Cult. 2011;2(1). doi: 10.9707/2307-0919.1014 [DOI] [Google Scholar]
- 17.Country comparison [Internet]. Helsinki, Finland: Itim International and The Hofstede Centre; 2017. Available from: https://www.hofstede-insights.com/country-comparison/australia,india,indonesia,the-usa/. Accessed March27, 2019. [Google Scholar]
- 18.Koenig HG. Religion, spirituality, and health: the research and clinical implications. ISRN Psychiatry. 2012;16:278730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knowles MS, Holton EF, Swanson RA. The Adult Learner: The Definitive Classic in Adult Education and Human Resource Development. 6th ed. Amsterdam: Elsiver; 2005. [Google Scholar]
- 20.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. doi: 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 21.Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Intern Assoc Appl Psychol. 2008;57(1):1–29. [Google Scholar]
- 22.Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13(4):623–649. doi: 10.1080/08870449808407422 [DOI] [Google Scholar]
- 23.Bandura A. Social Foundation of Thought and Action: A Social Cognitive Theory. New Jersey: Prentice-Hall Inc; 1986. [Google Scholar]
- 24.Squires G. Teaching as a Professional Discipline. London: Falmer Press; 1999:47. [Google Scholar]
- 25.Kolb D. Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, New Jersey: Prentice-Hall; 1984. [Google Scholar]