Abstract
Background
The impact of the coronavirus disease 19 (COVID-19) pandemic on health care workers has been substantial. However, the impact on vascular surgery (VS) trainees has not yet been determined. The goals of our study were to gauge the impact of COVID-19 on VS trainees’ personal and professional life and to assess stressors, coping, and support structures involved in these trainees' response to the COVID-19 pandemic.
Methods
This was an anonymous online survey administered in April 12–24, 2020 during the surge phase of the global COVID-19 pandemic. It is a subset analysis of the cross-sectional Society for Vascular Surgery Wellness Committee Pandemic Practice, Anxiety, Coping, and Support Survey. The cohort surveyed was VS trainees, integrated residents and fellows, in the United States of America. Assessment of the personal impact of the pandemic on VS trainees and the coping strategies used by them was based on the validated Generalized Anxiety Disorder 7-item (GAD-7) scale and the validated 28-time Brief Coping Orientation to Problems Experienced inventory.
Results
A total of 145 VS trainees responded to the survey, with a 23% response rate (145/638). Significant changes were made to the clinical responsibilities of VS trainees, with 111 (91%) reporting cancellation of elective procedures, 101 (82%) with call schedule changes, 34 (24%) with duties other than related to VS, and 29 (24%) participation in outpatient care delivery. Over one-third (52/144) reported they had performed a procedure on a patient with confirmed COVID-19; 37 (25.7%) reported they were unaware of the COVID-19 status at the time. The majority continued to work after exposure (29/34, 78%). Major stressors included concerns about professional development, infection risk to family/friends, and impact of care delay on patients. The median score for GAD-7 was 4 (interquartile range 1–8), which corresponds to no or low self-reported anxiety levels. VS trainees employed mostly active coping and rarely avoidant coping mechanisms, and the majority were aware and used social media and online support systems. No significant difference was observed between integrated residents and fellows, or by gender.
Conclusions
The pandemic has had significant impact on VS trainees. Trainees reported significant changes to clinical responsibilities, exposure to COVID-19, and pandemic-related stressors but demonstrated healthy coping mechanisms with low self-reported anxiety levels. The VS community should maintain awareness of the impact of the pandemic on the professional and personal development of surgeons in training. We recommend adaptive evolution in training to accommodate the changing learning environment for trainees.
Introduction
In early 2020, the rapid spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its associated clinical syndrome, coronavirus disease 2019 (COVID-19), placed a significant strain on health care systems around the world. An early international survey of 77 vascular surgeons demonstrated dramatic impacts on clinical practices, through cessation of elective procedures and redeployment of Vascular Surgery (VS) to support other clinical areas.1
Among VS trainees, burnout has been associated with higher levels of depression and perceived stress and lower levels of social support and self-efficacy.2 All these factors may be exacerbated by the COVID-19 pandemic. To date, epidemiologic data of the mental health impact of the COVID-19 pandemic on health care professionals, in particular VS trainees, are lacking.3 A 2019 Association of Program Directors in Vascular Surgery (APDVS) survey revealed that more than 60% of trainees experienced one or more symptoms of distress on a weekly basis.4 Based on these findings, trainees are a cohort of physicians that can be more at risk and more vulnerable to stressful situations at work than attending physicians. The global COVID-19 pandemic impact has the potential to exacerbate the challenges experienced by trainees. With this in mind, the objective of this study is to examine the specific impact of COVID-19 on VS trainees in the United States.
Materials and Methods
The cross-sectional Society for Vascular Surgery (SVS) Wellness Committee Pandemic Practice, Anxiety, Coping, and Support Survey was administered in April 12–24, 2020 during the surge phase of the global COVID-19 pandemic. This is a subset analysis of the main Global SVS Wellness Committee survey, which has been published elsewhere.5 The anonymous global survey was reviewed by the University of Washington Human Subjects Division and deemed exempt (#009926) because of the minimal risk and nonidentifiable nature of the survey. Personal and professional COVID-19–related stressors on VS trainees were evaluated by unique survey items (Appendix 1). Anxiety levels were assessed by the Generalized Anxiety Disorder 7-item (GAD-7) scale, and coping strategies were evaluated by the 28-item Brief Coping Orientation to Problems Experienced (Brief COPE) inventory.6 , 7
The impact on trainees' clinical responsibilities was assessed through changes to work schedules, team compliment, and the duties performed by the residents. Open-ended questions were offered for additional information to be shared by the respondents. A multimodality approach to dissemination was used through the SVS and APDVS electronic mailing lists and was amplified via social media.
Categorical data are presented as numbers and percentages. Continuous data are presented as means and standard deviation of the mean or median and ranges or interquartile range (IQR) where appropriate. Measures of central tendency of numerical data were compared using Student's t-test for normal parametric normally distributed data and the Wilcoxon rank-sum test for not normally distributed data. Categorical data were compared using the Pearson chi-squared test. Data were analyzed using SPSS 19.0 for Windows (SPSS, Inc., Chicago, IL). This report was compiled in accordance with the American Association for Public Opinion Research standard definitions.8
Results
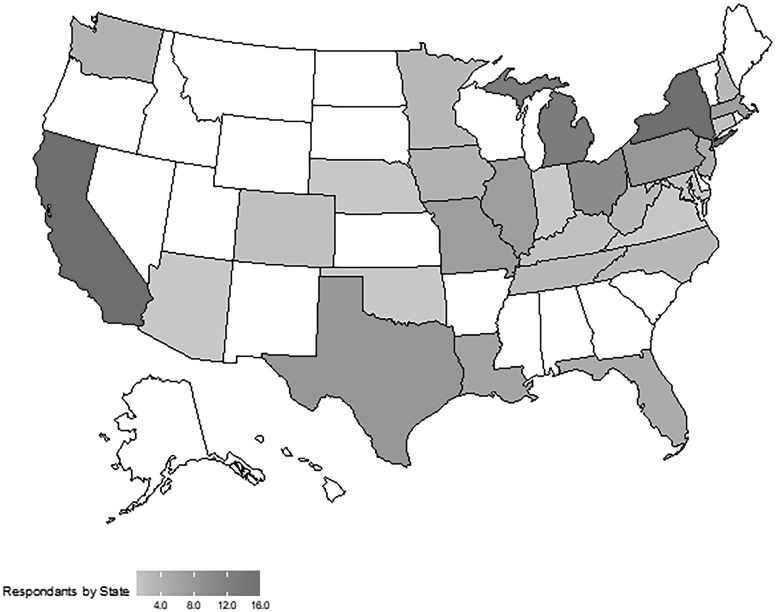
A total of 145 VS trainees responded to the survey from 29 states (Fig. 1 ). The current number of US VS trainees is 638, of which 30% identified as female on a recent survey from the APDVS. Therefore, the response rate was 23% (145/638). The majority of the respondents were male (60%) and white (57.2%) (Table I ). Most of the respondents completed the entire survey, and there was no significant difference in completion rates between integrated residents and fellows (88% vs. 82%, P = 0.315).
Fig. 1.
The US map of trainee respondents. The regions were classified as Northeast (Connecticut, Delaware, Maine, Maryland, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont), Midwest (Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, Ohio, South Dakota, and Wisconsin), Southeast (Alabama, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Virginia, and West Virginia), and West/Southwest (Arizona, California, Colorado, Hawaii, Idaho, Nevada, New Mexico, Oregon, Texas, Utah, and Washington).
Table I.
Descriptive statistics of trainee respondents
| Variable | n = 145 (%) |
|---|---|
| Training program | |
| Integrated vascular surgery residency | 83 (57.2) |
| Vascular surgery fellowship | 61 (42.1) |
| Prefer not to say | 1 (0.7) |
| Training level | |
| PGY 1–2 | 23 (15.9) |
| PGY 3–5 | 56 (38.6) |
| PGY 6–7 | 64 (44.1) |
| Prefer not to say | 2 (1.4) |
| Gender | |
| Male | 87 (60) |
| Female | 56 (38.6) |
| Prefer not to say | 2 (1.4) |
| Race | |
| White | 83 (57.2) |
| Asian | 30 (20.7) |
| African American | 4 (2.8) |
| American Indian/Alaska Native/Native Hawaiian/Pacific Islander | 2 (1.4) |
| Mixed | 5 (3.4) |
| Other | 12 (8.3) |
| Prefer not to say/unknown | 9 (6.2) |
| Size of the hospital | |
| 100–200 beds | 1 (0.7) |
| 201–300 beds | 7 (4.8) |
| 301–400 beds | 8 (5.5) |
| >400 beds | 105 (72.4) |
| Do not know or no response | 24 (16.6) |
| Region | |
| Northeast | 43 (29.7) |
| Southeast | 25 (17.2) |
| Midwest | 46 (31.7) |
| West/Southwest | 31 (21.4) |
| Completed the GAD-7 scale | 139 (95.9) |
| Completed the Brief COPE inventory | 130 (89.7) |
| Completed the entire survey | 123 (84.8) |
Impact of COVID-19 on the Clinical Responsibilities
Questions regarding the clinical responsibilities were answered by 123 trainees (73 integrated VS residents and 50 VS fellows). Most of the trainees reported that at the time of completing the survey, all elective surgical procedures were canceled (90.2%) and that, in most cases, the primary hospital where they work adhered to the American College of Surgeons and/or SVS guidelines for prioritizing surgeries during COVID-19 (85.4%).9 Overall, 83.1% stated there were intensive care unit (ICU) beds available and patients were not boarding on other units.
However, 44.4% of trainees in the Northeast noted they had no ICU beds available and were boarding patients in other parts of the hospital. Most trainees noted they were not participating in the delivery of any outpatient care for VS patients (76.4%). Among the 29 (23.6%) trainees still participating in the delivery of outpatient VS care, most reported they have reduced clinic/ambulatory center hours (23/29, 79.3%) and approximately half were incorporated into telemedicine visit (16/29, 55.2%).
Nearly a third of the trainees selected “residents removed form VS service” as applicable to them (n = 42, 34.1%). Call schedules were also changed for most of the trainees over the 2 weeks preceding the survey (82.1%). Nearly half reported the same overall number of on-call days, but the call schedule was reconfigured (46.3%). Call rotations were mostly on a weekly or biweekly rotation (36.6% and 22.8%, respectively). When not explicitly on call for VS, 44.7% of the trainees were available as backup for vascular emergencies, and 27.6% were available to assist with other necessary duties, such as cross-cover or line duties (Table II ).
Table II.
Impact of COVID-19 on clinical responsibilities of US trainees
| Variable | All n = 123 (%) | Integrated residents n = 73 (%) | Fellows n = 50 (%) | P |
|---|---|---|---|---|
| Elective surgeries cancelled | 111 (90.2) | 68 (93.2) | 43 (86.0) | 0.189 |
| Participating in the delivery of any outpatient care for vascular surgery patients | 29 (23.6) | 12 (16.4) | 17 (34) | 0.024 |
| Service changesa | ||||
| Residents removed from service | 42 (34.1) | 18 (24.7) | 24 (48) | 0.007 |
| One trainee covering vascular service alone | 75 (61) | 37 (50.7) | 38 (76) | 0.005 |
| One trainee cross covering multiple surgical services | 24 (19.5) | 16 (21.9) | 8 (16) | 0.416 |
| Covering other services | 13 (10.6) | 8 (11) | 5 (10) | 0.865 |
| Duties other than those as a vascular surgery traineeb | 34 (27.6) | 22 (30.1) | 12 (24) | 0.455 |
| Managing ICU patients | 18 (14.8) | 13 (18.1) | 5 (10) | 0.217 |
| Taking shifts to assist the ICU teams in placing lines | 18 (14.6) | 11 (15.1) | 7 (14) | 0.869 |
| Seeing patients in the emergency department | 4 (3.3) | 3 (4.1) | 1 (2) | 0.517 |
| Covering other surgery services | 10 (8.1) | 7 (9.6) | 3 (6) | 0.474 |
| Covering other medical services | 6 (4.9) | 6 (8.2) | 0 | 0.038 |
| Additional educational/research responsibilities | 13 (10.6) | 8 (11) | 5 (10) | 0.865 |
| Call schedule changes | 101 (82.1) | 62 (84.9) | 39 (78) | 0.324 |
| Less call | 26 (21.1) | 18 (24.7) | 8 (16) | 0.248 |
| More call | 19 (15.4) | 13 (17.8) | 6 (12) | 0.381 |
| Same call but changed distribution | 57 (46.3) | 31 (42.3) | 26 (52) | 0.298 |
| Duties while off of service | ||||
| No responsibilities—optimize social distancing | 49 (39.8) | 26 (35.6) | 23 (46) | 0.248 |
| Available to assist with vascular emergencies only | 55 (44.7) | 31 (42.5) | 24 (48) | 0.544 |
| Available to assist with any necessary duties (cross-cover, line team, etc.) | 34 (27.6) | 17 (23.3) | 17 (34) | 0.192 |
Trainees were asked “Which of the following apply to you? (Select all that apply)”; thus the categories are not mutually exclusive.
Trainees were asked “Have you been asked to assist in duties other than those as a vascular surgeon trainee?” If they replied “yes”, they were asked “Which other duties have you been asked to assist in? (Select all that apply)”. Categories are not mutually exclusive.
Some of the trainees included additional comments to explain the practice changes such as a) “one chief resident covering [the] entire vascular service, each week. We have also constructed a procedure/line team for COVID patients, staffed by one vascular resident and attending at a time”, b) “[we] split into teams of 4.1 week on, 3 weeks off in case of exposure. Backup team is the following week['s] team in case of illness/etc. When not on call, [we're] still performing duties as much as possible from [a] remote location and attending video educational conferences and increased research involvement”, and c) “Every other ‘respite’ week where the residents are responsible for at home learning”.
Exposure to COVID-19 and its Implications
A total of 52 of 144 respondents (36.1%) had operated on and/or placed a central venous catheter (CVC) in a patient with a confirmed COVID-19 infection: 15 (10.4%) had operated on a patient with COVID-19, 19 (13.1%) had placed a CVC, and 18 (12.5%) had performed both. Half (n = 27, 51.9%) of the trainees who have operated on or performed CVC placement in patients with COVID-19 were in the northeastern region of the United States.
One-quarter of respondents (n = 37, 25.7%) operated on or performed a procedure on a patient they later learned had a COVID-19 infection. In most of these circumstances, the trainees continued to work (n = 29, 78.4%), and very few underwent self-quarantine (n = 5, 13.5%) or were tested after the exposure (n = 4, 10.8%). Additional insight was gained from free-text comments: a) “… we were initially quarantined when exposed to a COVID-19 patient but given the number of patients that soon became impractical” and b) “[I] was told a patient was not suspected of having COVID-19 but needed a vascular catheter because of acute on chronic renal failure. The hospital was out of my size of N95 masks, so I performed the procedure without an N95. Later that day they tested the patient for COVID-19 and they came back positive. I no longer see any patient without an N95 first”. Four (2.8%) respondents reported testing positive for COVID-19, and 32 (22.2%) indicated they would consider themselves at “high” risk for COVID-19 infection.
Most trainees (93.5% of 124 respondents) indicated they had COVID-19 operating room protocols in place, and 63.7% had preoperative COVID-19 testing for their patients. A minority of respondents (23.4%) did not have adequate personal protective equipment at their hospital. Most (73.1%) noted that donning and doffing personal protective equipment was stressful.
COVID-19 Personal Impact, Stressors, Coping, and support Structures
Among the trainees who completed the GAD-7 survey (n = 139), the median anxiety score was 4 [IQR 1–8], which represents no anxiety. Overall, mild (GAD-7 score 5–9), moderate (GAD-7 score 10–14), and severe anxiety (GAD-7 score 15–21) was noted in 31.7%, 12.2%, and 5.8%, respectively, whereas 50.4% had no anxiety (GAD-7 score < 5). Among the small group of trainees with moderate/severe anxiety (18%), this was more common among fellows (n = 15, 25.9%) than residents (n = 10, 12.3%). The component breakdown of the GAD-7 survey stratified by training program can be seen in Figure 2 .
Fig. 2.
Responses to the Generalized Anxiety Disorder 7-item (GAD-7) scale by 139 vascular surgery trainees in the United States.
Most of the trainees (n = 112/145, 77.2%) noted they had implemented COVID-19–related modifications to their home routine after work, predominantly by having a separate changing area (73.1%) at their home. One hundred twenty-three (85%) of trainees responded to the series of questions regarding COVID-19–related stressors. Most were worried that their family and friends would get infected with COVID-19 (n = 116/123, 94.3%). The potential impact of COVID-19 on their career was noted to be stressful/very stressful by 44.4% of the trainees and exemplified by one of the free-text responses “[I am] worried about graduating experience given complete stoppage of elective vascular cases.” In addition, most were at least somewhat stressed by potential adverse patient outcomes due to care delay (88.6%, n = 109). Additional factors felt to be stressful/very stressful were working from home (n = 23, 18.8%), the burden of extra home cleaning (n = 25, 20.5%), and among those with children, the need for additional childcare (n = 26/67, 38.8%). There were no gender differences in the perception of COVID-19–related stressors.
A stressor captured in the free-text response focused on advocating for vulnerable patient populations. “A large part of the stress that I am experiencing as a result of the pandemic is in relation to the responsibility that I feel I have as a physician to advocate for the most vulnerable in our society, those who are being the most adversely affected by the medical and economic implications of this pandemic” and “I continue to be concerned … [by] the impacts [of COVID-19] on racial and ethnic minority patients affected by this virus. I would hope the SVS will have a response for these patients particularly low socioeconomic status, racial and ethnic minorities”.
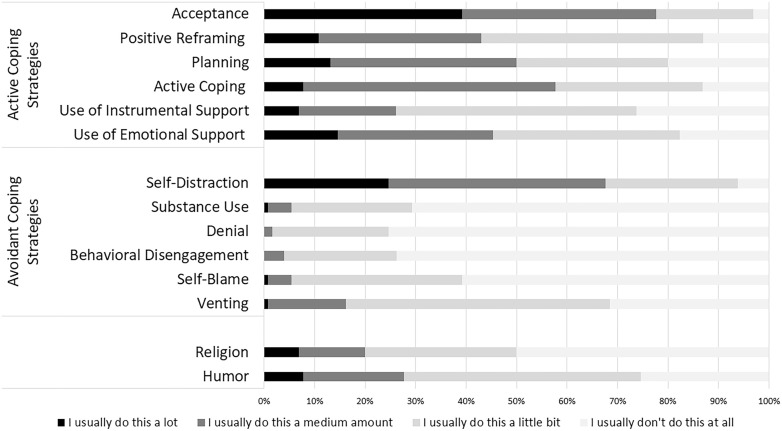
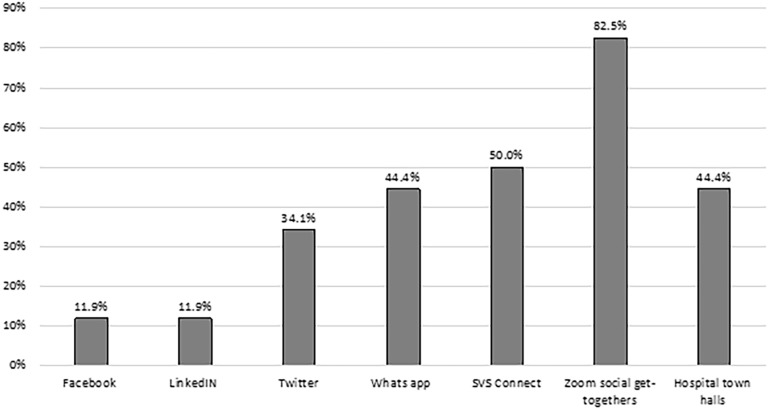
A total of 130 trainees completed the Brief COPE inventory. Most trainees used active strategies for coping, such as acceptance, planning, and use of support structures, and infrequently used avoidant strategies except for “self-distraction” which includes “I've been turning to work or other activities to take my mind off things” and “I've been doing something to think about it less, such as watching TV, reading, daydreaming, sleeping”. (Fig. 3 ). Among the 126 respondents who answered questions regarding support structures, Zoom social get-togethers were the most frequently used digital peer to peer support platform (82.5%) followed by SVS Connect (50%) (Fig. 4 ). Over half (54%) were aware of the SVS Physician Wellness Resources, but less than a third were aware of other physician wellness resources, such as ACS Surgeon Well-being (20.6%), AMA mental health (12.7%), Headspace discount (35.7%), and the suicide prevention line (31%).
Fig. 3.
Coping strategies used by 130 vascular surgery trainees in the United States as measured by the Brief Coping Orientation to Problems Experienced (Brief COPE) inventory.
Fig. 4.
Usefulness of social media systems and peer support systems for vascular surgery trainees in the United States.
Discussion
The impact of COVID-19 on the surgical practices in the United States is expected to have a significant impact on the training environments and unique stressors for trainees.10 This survey offers insight into the personal impact and changes to VS trainees' learning environment during April 2020 when COVID-19 cases surge in the United States. Multiple changes to the VS trainees's experience ranged from the type of work demands—ranging from redeployment to duties other than those of a VS trainee to additional independence on the VS service—or amount of work demands—ranging from additional clinical responsibilities to protected time for self-learning. In addition to these changes, most trainees identified major personal stressors, such as worrying about family and friends getting infected with COVID-19 and taking on additional home responsibilities.
Although trainees reported specific factors as stressful, overall self-reported anxiety levels were low, with half of the respondents stating they had no or minimal anxiety. Residents employed mostly active coping strategies and turned to a wide range of support structures across social media and professional societies. These findings suggest a high degree of resiliency among VS trainees.11 , 12
Lessons learned from previous outbreaks such as the 2003 severe acute respiratory distress syndrome (SARS) and 2015 Middle East respiratory syndrome coronavirus (MERS-CoV) demonstrated that the high rates of psychologic distress persisted after the immediate threat of the outbreak was over.13, 14, 15, 16 Factors associated with higher rates of stress included higher levels of exposure, health fear for self and colleagues, social isolation, job fear, an obligation to treat infected patients, previous psychiatric disorders, fewer years of health care experience, stigma and rejection from quarantine and their work in the health care field, and information overload.17, 18, 19, 20, 21, 22, 23 Mitigation strategies during these previous epidemics included clear communication, sensitivity to individual responses to stress, clinical autonomy, social support, strong management support, infection control guidance, and equipment.16 , 19 , 23, 24, 25, 26, 27, 28
Initial criticisms of mental health interventions to support those affected by the COVID-19 pandemic point out that there is no centralized organization responsible for planning and deploying evidence-based interventions to mitigate the psychological impact on health care workers.29 Taken together, these lessons emphasize the need for mitigation strategies that include multidisciplinary teams available to health care workers, regular and accurate updates, and secure platforms to provide these services.3
Because of the importance of resident well-being, The American Council of Graduate Medication Education has developed the Clinical Learning Environment Review (CLER).30 Before the current pandemic, investigations into the CLER have identified the key areas related to resident wellness and burnout to be workload, control, balance between effort and reward, community, fairness, and values.31 Crucial factors in maintaining personal well-being during vascular training include faculty entrustability, receptive leadership, celebrating small victories, and resiliency training—all which may be particularly crucial during times of crisis.32
Understanding the changes in VS training and mental health impact will help develop support programs unique to VS trainees and cultivate a set of best practices for training during a crisis to optimize surgeon well-being and resilience.33 In addition, the data identified potential additional educational opportunities for VS trainees. They include incorporating telemedicine into the training program as they are currently being underutilized, outlining the educational goals and objectives of the new duties during the pandemic response such as redeployment to the ICU or to dedicated line teams, demonstrating clear support for the VS trainees during these stressful times, and empowering them to take an active role in the COVID-19–related protocols designed specifically to support the trainees.
In our analysis of the larger cohort of vascular surgeons’ respondents to the survey, we found a strong association between lower self-reported anxiety levels among vascular surgeons who perceived that they had hospital support delivered through structured protocols, transparency from leadership, and opportunities to interact with the leadership.
Limitations
Our work is limited by the response rate that accounts for a fifth of the VS trainees. This may limit the generalizability of the findings to all VS trainees. In addition, the study is limited by the inherent design self-reported surveys such as recall bias, social desirability, and respondent selection bias. These were addressed by the short dissemination period of 10 days, the anonymous nature of the survey, and the dissemination of the survey through social media platforms and email lists.
Conclusions
VS trainees responding to the survey experienced significant changes to their clinical responsibilities and high rates of exposure related to the impact of COVID-19. The resulting stressors focused on their training and future career and worry about family, friends, and patients. They reported healthy active coping mechanisms and relatively low levels of anxiety, which suggests a high level of resiliency. Further study will be needed to understand the lasting effects of the COVID-19 pandemic on the personal and professional development of future vascular surgeons.
Footnotes
Competing Interests: The authors have no competing interests to declare.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.avsg.2020.09.045.
Supplementary Data
Vascular Surgeons in Training Version of Society for Vascular Surgery Wellness Task Force Pandemic Practice, Anxiety, Coping and Support Survey for Vascular Surgeons.
References
- 1.Ng J.J., Ho P., Dharmaraj R.B., et al. The global impact of COVID-19 on vascular surgical services. J Vasc Surg. 2020;71:2182–2183.e1. doi: 10.1016/j.jvs.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Janko M.R., Smeds M.R. Burnout, depression, perceived stress, and self-efficacy in vascular surgery trainees. J Vasc Surg. 2019;69:1233–1242. doi: 10.1016/j.jvs.2018.07.034. [DOI] [PubMed] [Google Scholar]
- 3.Xiang Y.-T., Yang Y., Li W., et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hekman K.E., Wohlauer M.V., Magee G.A., et al. Current issues and future directions for vascular surgery training from the results of the 2016-2017 and 2017-2018 Association of Program Directors in Vascular Surgery annual training survey. J Vasc Surg. 2019;70:2014–2020. doi: 10.1016/j.jvs.2019.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shalhub S., Mouawad N.J., Malgor R.D., et al. Global vascular surgeons experience, stressors, and coping during the COVID-19 pandemic. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spitzer R.L., Kroenke K., Williams J.B.W., et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 7.Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 8.The American Association for Public Opinion Research . 9th Edition. 2016. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. [DOI] [Google Scholar]
- 9.American College of Surgeons COVID-19 guidelines for triage of vascular surgery patients. ACS website. 2020. https://www.facs.org/covid-19/clinical-guidance/elective-case/vascular-surgery
- 10.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. doi: 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonanno G.A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 12.Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthop. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 13.Tam C.W.C., Pang E.P.F., Lam L.C.W., et al. Severe acute respiratory syndrome (SARS) in Hongkong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34:1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 14.Lee S.M., Kang W.S., Cho A.-R., et al. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang C.S., Du P.L., Huang I.C. Nurses’ perceptions of severe acute respiratory syndrome: relationship between commitment and intention to leave nursing. J Adv Nurs. 2006;54:171–179. doi: 10.1111/j.1365-2648.2006.03796.x. [DOI] [PubMed] [Google Scholar]
- 16.Chua S.E., Cheung V., Cheung C., et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can J Psychiatry. 2004;49:391–393. doi: 10.1177/070674370404900609. [DOI] [PubMed] [Google Scholar]
- 17.Maunder R.G., Lancee W.J., Rourke S., et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. 2004;66:938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 18.Abolfotouh M.A., AlQarni A.A., Al-Ghamdi S.M., et al. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017;17:1–10. doi: 10.1186/s12879-016-2096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khalid I., Khalid T.J., Qabajah M.R., et al. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin Med Res. 2016;14:7–14. doi: 10.3121/cmr.2016.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lancee W.J., Maunder R.G., Goldbloom D.S., et al. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McAlonan G.M., Lee A.M., Cheung V., et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 22.Bai Y., Lin C.-C., Lin C.-Y., et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55:1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 23.Matheson C., Robertson H.D., Elliott A.M., et al. Resilience of primary healthcare professionals working in challenging environments: a focus group study. Br J Gen Pract. 2016;66:e507–e515. doi: 10.3399/bjgp16X685285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Havermans B.M., Boot C.R.L., Houtman I.L.D., et al. The role of autonomy and social support in the relation between psychosocial safety climate and stress in health care workers. BMC Public Health. 2017;17:558. doi: 10.1186/s12889-017-4484-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amaratunga C.A., O’Sullivan T.L., Phillips K.P., et al. Ready, aye ready? Support mechanisms for healthcare workers in emergency planning: a critical gap analysis of three hospital emergency plans. Am J Disaster Med. 2007;2:195–210. [PubMed] [Google Scholar]
- 26.Murden F., Bailey D., Mackenzie F., et al. The impact and effect of emotional resilience on performance: an overview for surgeons and other healthcare professionals. Br J Oral Maxillofac Surg. 2018;56:786–790. doi: 10.1016/j.bjoms.2018.08.012. [DOI] [PubMed] [Google Scholar]
- 27.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci. 2004;359:1117–1125. doi: 10.1098/rstb.2004.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maunder R., Hunter J., Vincent L., et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 29.Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Long T.R., Doherty J.A., Frimannsdottir K.R., et al. An early assessment of the ACGME CLER program: a national survey of designated institutional officials. J Grad Med Educ. 2017;9:330–335. doi: 10.4300/JGME-D-16-00489.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jennings M.L., Slavin S.J. Resident wellness matters: optimizing resident education and wellness through the learning environment. Acad Med. 2015;90:1246–1250. doi: 10.1097/ACM.0000000000000842. [DOI] [PubMed] [Google Scholar]
- 32.Audu C.O., Coleman D.M. Prioritizing personal well-being during vascular surgery training. Semin Vasc Surg. 2019;32:23–26. doi: 10.1053/j.semvascsurg.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Wald H.S., Wald H.S. Optimizing resilience and wellbeing for healthcare professions trainees and healthcare professionals during public health crises - practical tips for an ‘ integrative resilience ’ approach ‘ integrative resilience ’ approach. Med Teach. 2020;0:1–12. doi: 10.1080/0142159X.2020.1768230. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Vascular Surgeons in Training Version of Society for Vascular Surgery Wellness Task Force Pandemic Practice, Anxiety, Coping and Support Survey for Vascular Surgeons.