Abstract
Extracorporeal shock wave therapy (ESWT) is a safe therapy and there are only a few side effects known (such as pain during ESWT and minor haematomata), but no severe complications are to be expected if it is performed as recommended.
Contraindications are severe coagulopathy for high-energy ESWT, and ESWT with focus on the foetus or embryo and focus on severe infection.
The effect mechanism of ESWT is still a component of diverse studies, but as far as we can summarize today, it is a similar process to a cascade triggered by mechano-transduction: mechanical energy causes changes in the cellular skeleton, which provokes a reaction of the cell core (for example release of mRNA) to influence diverse cell structures such as mitochondria, endoplasmic reticulum, intracellular vesicles, etc., so the enzymatic response leads to the improvement of the healing process.
The usage of ESWT should be taught, to improve the outcome. Courses should be organized by national societies, since the legal framework conditions are different from one country to another.
In this update the musculoskeletal indications are addressed (mainly bone and tendons): pseudoarthrosis, delayed fracture healing, bone marrow oedema and osteonecrosis in its early stages, insertional tendinopathies such as plantar fasciitis and Achilles tendon fasciitis, calcifying tendonitis of the rotator cuff, tennis elbow, and wound healing problems.
Cite this article: EFORT Open Rev 2020;5:584-592. DOI: 10.1302/2058-5241.5.190067
Keywords: shock wave, pressure, therapy, extracorporeal, indication
Introduction and history
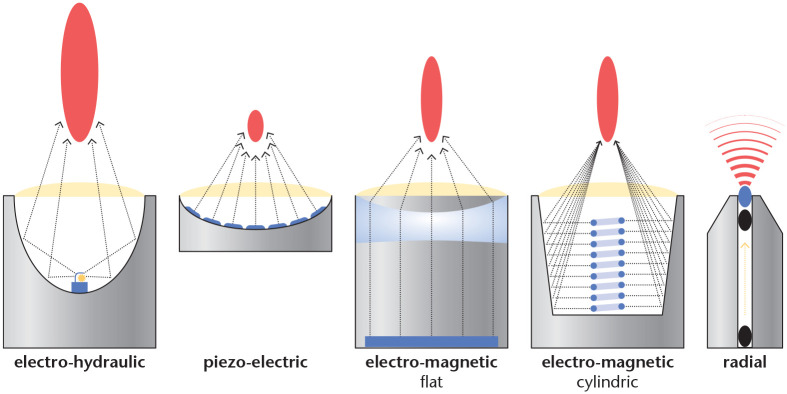
Extracorporeal shock wave therapy (ESWT) is a non-invasive form of treatment, that has been developed from ESWL (extracorporeal shock wave lithotripsy). The development of EWST, the physical theoretical basic knowledge and different devices for application, such as focusing devices (electro-hydraulic, piezo-electric, electro-magnetic flat, electro-magnetic cylindric) and radial devices, which are also called ballistic, started with first applications which were tested on bones by orthopaedic surgeons and traumatologists in Germany and in Bulgaria. Several researchers at different locations discovered and tried to use the effects of shock waves on bones relatively simultaneously.1,2 In orthopaedics, many other indications have emerged relatively quickly in addition to the application to bone, and ESWT has expanded rapidly.
In 1997, the uninhibited enthusiasm for ESWT as a form of therapy and the simultaneous lack of proven evidence led to the questioning of this kind of therapy especially in the country with the most frequent applications of ESWT. An exact survey of the evidence was initiated and, finally, the report of the ‘Medical Treatment’ working committee of the Federal Committee of Doctors and Health Insurance Funds on consultations of the year 1998 for the evaluation of extracorporeal shock wave therapy (ESWT) for orthopaedic, surgical and pain therapeutic indications according to §135 para.1 SGB V of 22.07.1999, resulted in the abolition of payment for this treatment by health insurance funds in Germany.
This was almost the end of ESWT, but an initiative of the German Society for Orthopaedics and Traumatology contributed to further development. Three multicentre studies were initiated the results of which put ESWT on a new footing scientifically. Although the work of the working groups around Michael Haake (Philipps-Universität-Marburg resp. Universität Regensburg) did not find any positive results of ESWT in the treatment of lateral epicondylitis,3,4 the multicentre study by Ludger Gerdesmeyer (Technische Universität München) showed significantly better results with ESWT than with a placebo.5
Extracorporeal shock wave therapy has been developed from extracorporeal shock wave lithotripsy (ESWL). Lithotripsy studies on the effects of shock waves on the different tissues of the body that come into direct or indirect contact with shock waves, have also focused on bones and other tissues of the musculoskeletal system, thus showing that shock waves can have a positive effect on a wide variety of tissues.6–11
Devices
The development of ESWT devices is closely linked to that of ESWL (Fig. 1). First the electro-hydraulic devices came onto the market, then the piezo-electric and the various electro-magnetic devices (with flat coil or cylindrical coil). All these devices produce focusing pressure pulses. There are considerable differences in the quality of the sound fields, mainly the focus zones are very different, but with all these devices shock waves can be generated within the highest energy settings. The radial devices use compressed air or electro-magnetic forces to accelerate a ‘projectile’ in the device, which transfers its energy on impact with an applicator and applies it to the tissue.
Fig. 1.
Different types of generating pressure waves and shock waves are produced by the diverse devices for ESWT. All these devices produce more or less focused pressure waves and shock waves except the radial devices, which produce pressure waves, which are not focused and have the highest energy in the area where the applicator delivers the mechanical energy into the body, superficially on the skin.
Physics
In order to be able to deal with the nature of shock waves, one has to deal with waves in general, then one can deal with the differences between more or less high-energy pressure waves and shock waves. According to Harten, an ‘oscillating structure’ has a well-defined resting position in which it can remain permanently.12 If it is deflected from this position, the driving forces try to bring it back into the resting position. The characteristic value of the oscillation is its natural frequency and its amplitude. The simplest oscillations, the so-called harmonic oscillations, are described mathematically by the angular functions of sine or cosine. More complicated oscillations can be understood as superpositions of such simple oscillations.11 Shock waves are mechanical waves, they propagate in a medium which also deforms or changes its density. The media we have to consider are water and human tissue; water due to the fact that all measurements are carried out in water, and human tissue because it is the target of ESWT in all orthopaedic indications. The deformation is reversible due to its restoring force.
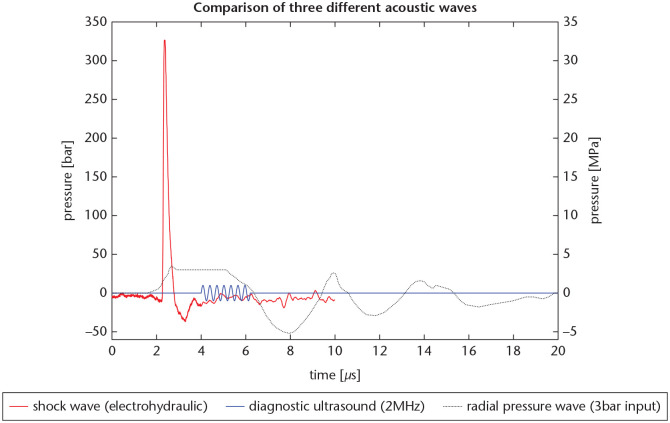
With the introduction of ballistic and radial devices, respectively, to the market, a conflict arose that has not yet been resolved, because these devices also claim to be suitable for extracorporeal shock wave therapy. In fact, these devices produce pressure pulses that appear to address similar or identical target organs as the focusing devices. The conflict is still part of heated discussions and will certainly continue to be so, especially as the users of both techniques have had clinical success, which is shown later in the ‘clinical indications’ section. The fact is, however, that radial devices do not produce pressure pulses that resemble the characteristic properties of the classic shock wave: the rising time and the maximal pressure of radial pressure waves are much lower (Fig. 2).
Fig. 2.
Comparison of three different acoustic waves: shock waves, diagnostic ultrasound and radial pressure waves.
Source. Electro-hydraulic shock wave: MTS Europe GmbH, measurement orthogold100, focused applicator. Diagnostic ultrasound: sine wave, calculated with 1 MPa peak pressure at 2MHz. Radial pressure wave: Cleveland RO, Chitnis PV, McClure SR. Acoustic field of a ballistic shock wave therapy device. Ultrasound Med Biol 2007;33:1327–1335, Figure 6a.
The description of the parameters for focusing devices goes back to ESWL, and is only of limited use to describe the pressure pulses for ESWT. The parameter set is written in the CE certification normative IEC 61846;13 this is the base for the description of shock waves and includes pressure (MPa) and time (s) in water. In this case the impedance is only dependent on the energy level. In human tissue, different tissue densities additionally influence the impedance (it is the product of the medium’s density and the wave’s velocity).
The measurements are carried out using hydrophones, they are presented in diagrams as graphs by time versus pressure, and the sound fields are measured at defined areas, the centres of the focus zones. Some parameters are calculations of the measurements, for example the energy flux density (ED, mJ/mm2). We will not discuss each parameter, since we want to focus on clinical indications, but we want to comment on the parameter energy. There are very prominent publications,5 where it is assumed that the product of ED and number of impulses is the total amount of energy, but this does not take into account that the focus size differs a lot with different energy levels and the pressure declines from the centre toward the margin, so one should consider the diverse pressure levels within the focus as isobars. At the moment, comparison of the devices is difficult, since the measurements are made under diverse circumstances. In the future it should be possible to define exactly described conditions for measurements and hydrophones, and the measurements should be made in defined focus areas.13 An additional parameter could be defined as momentum or impulse or impact (M; m * v (Ns)). All focusing devices have in common that they bring the highest energy together into the focus. Descriptions of the different generating mechanisms can be found in the literature.14 It should be emphasized that the quality of electro-hydraulically generated shock waves is obviously much different from that of shock waves produced by electro-magnetic and piezo-electric devices. For example, the jitter effect makes it difficult to measure each impulse correctly, which means that average values are given. Whether this is a reason for different effectiveness, cannot be said, but the sound fields of each pulse look much more different than with the other devices. Thus, from our point of view, there is an urgent need to introduce new parameters. Radial pressure waves, confusingly referred to as r-ESWT in the literature, are characterized by the fact that they have a sound field which becomes weaker and weaker as the process progresses. The impulses are oriented in one direction, but they run in all directions and they decrease in intensity the further they penetrate into the tissue. These devices generate the strongest energy directly at the point of entry at the treated region of the body. Of course, pressure gradients can also be measured, but compared to focusing devices, the rise times of the pressure pulses are much slower (between approximately 1 and 25 microseconds). The pressure intensity is also lower: the peak pressure in the focus can exceed 50 MPa for focusing devices, while the pressure peaks of approximately 15 MPa are significantly lower for radial devices. The rise times are even more clearly different: with focusing devices, the rise times are in the range of 5–10 ns at high energies, with radial devices, they are 5–1 ms. The rise times of the pressure peaks are considerably lower with radial devices. In particular, the penetration depth of the pressure pulses is very different for the two device types. With high energy settings, for example, a penetration depth of well over 10 cm can be achieved with focusing devices, whereas with radial devices the energy levels at approximately 1.5 cm have already dropped considerably, suggesting that superficial structures should be treated. Whether the superficial structures produce an effect in the depth, or only the pressure impulses of the devices, can perhaps sometimes be differentiated from further studies, but this does not exclude the possibility that with superficially effective devices positive effects can also be achieved in the depth.
The properties of shock waves and pressure waves that trigger an effect in the body are still not clear, and various physical effects can be observed: in addition to changes in pressure gradients, temperature changes and cavitation can also be observed.5,13 Which of these changes are necessary for the clinical effect is the subject of investigation; clear statements cannot yet be made, and therefore this topic is not explained in detail here. As published on the homepage of the International Society for Medical Shockwave Treatment (ISMST), it is recommended to record all possible parameters in the clinical documents which are available at the moment (type of machine, number of impulses, parameter of impulses as ED or comparable information), and it is recommended to cooperate with the manufacturer in case of designing and performing clinical studies and basic research publications (https://www.shockwavetherapy.org/about-eswt/ismst-recommendations/).
Biology
The transmission of a shock wave or of a pressure wave leads to effects on the tissue. The transformation of the physical energy into a biological response is similar to a cascade process. First the cell skeletal annexes are activated, which leads to the release of mRNA from the cell nuclei. This is followed by activation of cell organs such as the mitochondria and the endoplasmic reticulum and the cell vesicles, which release the specific proteins of the healing process. Wang’s research group showed several working mechanisms which fit into this idea of mechano-transduction, as the cascade is called by ESWT users.15 In animal models it is observed, that ESWT induces free radicals and oxygen radicals, which induce the production of a number of growth factors.16
The cellular effect of ESWT is increasingly better understood at the molecular level. Cell regeneration is a complex process including cell activation, migration and interaction of different cell types. This leads to the expression of cell surface proteins (receptors), which are stimulated by cytokines and thus activate the interactions.17,18 These processes are triggered, induced and amplified by ESWT.19 Initially, the mechanisms were not understood, and microfractures in the bone were shown and held responsible for the effects.20,21 Recent studies show the molecular mechanism of ESWT; it has been shown that osteogenesis is induced by inhibition of osteoclasts. In bone augmentation, ESWT activates osteogenesis by osteoblast differentiation and then by increased proliferation, which has been demonstrated in vivo and in vitro.16
ESWT improved symptoms in rats with OA and we have confirmed that it inhibits cartilage degeneration and promotes the rebuilding of subchondral bone. The mechanism may be that ESWT activates Wnt5a/Ca2+ signalling in bone marrow mesenchymal stem cells.22 The described results confirm the therapeutic effect of ESWT in rats with OA. Micro-CT findings included increased bone density, bone volume, trabecular count, and trabecular strength, suggesting that ESWT promotes subchondral bone formation.23 Additionally, proliferation of periosteal cells is induced.24 The fixed action of screws or implants in osteoporotic bone is a biomechanical problem. Different techniques such as bone impaction, angular stable plates, coatings or cement augmentation have been tried to avoid osteoporosis. Another possibility would be local bone induction. In a study in rats, local shock wave therapy was applied and it was shown that, not only in the area of the screws, but also far away from them an increase in bone density measured in micro-CT could be observed. Increased stability was also measured in the pull-out test (3000 unfocused shock waves with an energy density of 0.3 mJ/mm2 were administered).25,26
Indications/location/results
ESWT in daily life
Urologists have used ESWL to break up kidney stones. All other applications are regenerative. This must be explained to the patient accordingly and also affects the recommendations for the time following ESWT. If, for example, ESWT is used in the treatment of tendons or bones, one must take appropriate precautions to ensure that stress after treatment does not compromise the healing process. As can be seen from the mechanisms of action, ESWT can accelerate the healing of tissue, but basic principles must still be guaranteed, such as immobilization during bone healing, otherwise regenerative tissue would be destroyed during every movement of the fracture gap. It is very important to convey to the patient that healing takes time.
Side effects can be explained, for example, pain during the application of ESWT itself. At high energies or high contact pressure of the device on the tissue, petechial bleeding can occur in the skin in addition to a slight reddening of the skin.27 Rompe et al have shown that very high energy levels can cause damage of the tissue, as for example 0.6 mJ/mm2 energy flux density causes necrosis of tendons in rabbits.28
Comorbidities should be discussed with the patients, for example, those that may also have an effect on the healing process.29
Contraindications
Shock waves can destroy metals, as can be seen on boat propellers, so attention should be paid to the energy being applied. The higher the energy setting, the higher the destructive power, as applied to kidney stone shattering. Rompe et al have already impressively shown in 1997 that with the devices on the market, which are used for bone treatment, tendons can be permanently damaged.28 Since shock waves release their energy mostly to the environment where the media have a greater difference in impedance, all tissues which have very different impedances, i.e. particularly high or particularly low density, are endangered. It is therefore essential to ensure that the lungs are not in the sound field because it can lead to tears and bleeding or pneumothorax.
From the above it follows that ESWT should be used in an environment that is similar to the protective standard of accepted medical practice. In addition, it follows that only those people who have the appropriate competence should use ESWT. The indication can only be applied by someone who is authorized to make the diagnosis, which in many countries is reserved for physicians; in some countries also physiotherapists and/or podiatrists are authorized.
We regard the fact that the treatment itself is unpleasant or painful as a side effect, not a complication. ESWT can cause redness and superficial haematomata on the skin, due to the pain during ESWT. The patient might develop a vago-vasal reaction and become dizzy, and deeper injuries of the skin are not unknown.
Complications have been described, which occurred after ESWT, but it could not be proven that ESWT leads to such changes at the recommended energy levels. More likely, multiple cortisone infiltrations in the run-up to ESWT which are described, are much more likely to lead to necrosis of the humeral head.30
We recommend following the guidelines which are published on the homepage of the International Society for Medical Shockwave Treatment (ISMST), on how to perform ESWT (https://www.shockwavetherapy.org/about-eswt/ismst-guidelines/). Carrying out those instructions helps to avoid any complication as described here.
Bone indications: non-union, delayed healing
The oldest orthopaedic indication for ESWT is delayed bone fracture healing or pseudarthrosis. Valchanou published a series of bone treatments in 1991, which he carried out in Bulgaria at the end of the 1980s.1 At the same time, centres in Germany also made observations on the bones of animals treated with ESWT.6,7,31,32 However, the published studies were not fully characterized by their evidence levels, but several case series of different bony indications led to a spread of ESWT among orthopaedists and traumatologists.33 Despite the criticism of ESWT in the treatment of pseudarthrosis and delayed bone fracture healing, it has become accepted, not least due to the work of Cacchio and Furia, who have achieved a significantly higher level of evidence based medicine (EBM) standards than previous studies.34–37 Although there are also studies today that describe ESWT on bone with other than high-energy devices, one can only recommend high-energy treatment with focusing devices as applied in the publications with positive results, i.e. with electro-hydraulic and with electro-magnetic devices and energy levels from 0.35 mJ/mm2 to 0.70 mJ/mm2.
Osteochondrosis dissecans, osteonecrosis, bone marrow oedema
The treatment of femoral head necrosis has not been as successful as the treatment of delayed fracture healing and pseudarthrosis, but there are a few publications that describe a positive effect. Ludwig et al observed an improvement not only clinically, but also in the Association Research Circulation Osseous (ARCO) stage of femoral head necrosis.38 The data situation is not particularly overwhelming, but even in systematic reviews a positive effect appeared likely, even if it was pointed out that no double-blind studies are available.39,40 A later study also showed positive results, even though this work was also not a randomized controlled trial. Wang et al compared ESWT not to a placebo, but to core decompression, and found encouraging results.41 However, Wang et al also found in a comparative study with randomization of ESWT against alendronate comparable results in which ESWT was equivalent in both groups.42 d’Agostino et al found promising results in the early stage of femoral head necrosis.43 Not only osteonecrosis of the femoral head was studied, but also bone marrow oedema syndromes. A further study by d’Agostino et al, for example, showed a significant improvement with ESWT in Kienböck’s disease.44 In summary, there are reports of ESWT use in osteonecrosis: Perthes disease, Köhler I and II, femoral head necrosis and secondary osteonecrosis after trauma. The literature is poor, but there is a case report by Moretti et al concerning a successful treatment of bilateral osteochondrosis dissecans at the knee, and there is a published series from Berlin, which reported positive results.45,46
Plantar fasciitis, Achilles tendinopathy
ESWT has been most successful in routine treatment of heel complaints such as plantar fasciitis and in the insertion tendinopathy of the Achilles tendon and mid-portion Achillodynia. Here, the data situation is quite good, even though the literature has weaknesses for this indication. The Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen47 examined the evidence for use of ESWT in heel complaints most thoroughly, and this investigation led to the fact that health insurance companies in Germany have to bear the costs of ESWT at the heel because the examination produced sufficient evidence. Previous publications are much weaker; on the one hand no significant success was achieved compared with a placebo when local anaesthesia was used,4,48 or a very heterogeneous patient population was invited for therapy, which would not have facilitated randomization,49 even though there were studies that had shown good success of ESWT in plantar fasciitis.49–57 The list could be extended, but there are publications which have shown good results for focusing and radial devices. There are also studies comparing ESWT with other therapies, such as cortisone. Although ESWT does not have a damaging effect on tendon tissue, unlike cortisone, the results are not conclusive.
As with plantar fasciitis, there are many publications on Achilles tendinopathy that show that ESWT can produce a good effect. Very quickly it became established that one should not carry out this treatment without remedial gymnastics, especially in Achillodynia.58 Rompe et al dealt with remedial gymnastics and ESWT in further studies and emphasized their positive interaction, after he had investigated the two therapies and their effect in comparison with one another, and other colleagues also proved the positive effect of ESWT on pain relief in the Achilles tendon.59–64
Tendinitis calcarea, calcifying tendinitis
The use of ESWT on the calcified shoulder was developed because it was initially mistakenly assumed that the ‘lime’ could be blown out of the tendon, comparably to kidney stones, which are crushed and these fragments are then discharged via the ureter. But it became apparent that it was the effect on the tissue that induced healing and not the ‘destructive’ effect of shock waves.
Loew et al in Heidelberg were the first to publish a small series on ESWT for calcific shoulders. At the same time, Rompe et al published a series with good results.9,10,65 The different energy strengths and their different effects on the ‘lime’ deposit were also dealt with shortly afterwards.66 The breakthrough was achieved by Gerdesmeyer et al,5 who showed that high-energy (0.32 mJ/mm2) produced better results than low-energy (0.08 mJ/mm2) ESWT, but also that the low-energy ESWT was able to dissolve lime. Retrospectively this publication was probably very decisive for the overall success of ESWT, because the publication had a high degree of evidence and convinced the experts. Another article by Cacchio, who carried out a randomized controlled trial (RCT) comparing radial and focusing ESWT showed better results (for the visual analogue scale and the UCLA shoulder rating scale) for the radial device.67 This assessment is not shared by all shock wave users; rather, there is a predominant number of users who see advantages for focusing ESWT especially in tendinosis calcarean.68,69
Epicondylitis radialis (tennis elbow)
The first major article on ESWT in radial epicondylitis was published by Haake et al.3 who, however, included a bias in the study. Nevertheless, ESWT in radial epicondylitis quickly became established, but it certainly has the worst results of any of the recognized indications. It is disappointing that other forms of treatment such as cortisone infiltrations have no better evidence apart from short-term pain relief. ESWT at the elbow is often offered, but the evidence has to be proven by upcoming studies.
Trigger points
Extracorporeal shock wave therapy has established itself in trigger point therapy in recent years, with two types of application being used: the extensive treatment of muscles and fascia is usually performed with radial devices, the search for trigger points and the static treatment of these is more likely to be performed with focusing treatment with ESWT.70
Conclusions
Extracorporeal shock wave therapy has developed from extracorporeal shock wave lithotripsy and is a non-invasive form of treatment in musculoskeletal disorders. This review article covers the basics of ESWT, including its historical development, physical theoretical basic knowledge and different devices for application. A part of the article deals with the effect of ESWT on cells and its molecular mechanisms. Different indications such as bony indications: non-union, delayed healing, osteochondrosis dissecans, osteonecrosis, bone marrow oedema, plantar fasciitis, Achilles tendinopathy, epicondylitis radialis and trigger points are described. In our opinion, ESWT is a possible option in conservative therapy for the indications mentioned in this review. However, this option should be reserved for orthopaedic specialists familiar with this therapy and these indications. Nevertheless, further randomized trials are necessary to improve the evidence in some areas.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Valchanou VD, Michailov P. High energy shock waves in the treatment of delayed and nonunion of fractures. Int Orthop 1991;15:181–184. [DOI] [PubMed] [Google Scholar]
- 2. Schleberger R, Senge T. Non-invasive treatment of long-bone pseudarthrosis by shock waves (ESWL). Arch Orthop Trauma Surg 1992;111:224–227. [DOI] [PubMed] [Google Scholar]
- 3. Haake M, König IR, Decker T, Riedel C, Buch M, Müller HH. Extracorporeal shock wave therapy in the treatment of lateral epicondylitis: a randomized multicenter trial. J Bone Joint Surg Am 2002;84:1982–1991. [DOI] [PubMed] [Google Scholar]
- 4. Haake M, Buch M, Schoellner C, et al. Extracorporeal shock wave therapy for plantar fasciitis: randomised controlled multicentre trial. BMJ 2003;327:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gerdesmeyer L, Wagenpfeil S, Haake M, et al. Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA 2003;290:2573–2580. [DOI] [PubMed] [Google Scholar]
- 6. Johannes EJ, Kaulesar Sukul DM, Matura E. High-energy shock waves for the treatment of nonunions: an experiment on dogs. J Surg Res 1994;57:246–252. [DOI] [PubMed] [Google Scholar]
- 7. Graff J. Die Wirkung hochenergetischer Stosswellen auf Knochen und Weichteilgewebe. Bochum, Germany: Habilitationschrift Ruhr-Universitaet, 1989. [Google Scholar]
- 8. Haupt G, Haupt A, Ekkernkamp A, Gerety B, Chvapil M. Influence of shock waves on fracture healing. Urology 1992;39:529–532. [DOI] [PubMed] [Google Scholar]
- 9. Loew M, Jurgowski W. [Initial experiences with extracorporeal shockwave lithotripsy (ESWL) in treatment of tendinosis calcarea of the shoulder]. Z Orthop Ihre Grenzgeb 1993;131:470–473. [DOI] [PubMed] [Google Scholar]
- 10. Rompe JD, Rumler F, Hopf C, Nafe B, Heine J. Extracorporal shock wave therapy for calcifying tendinitis of the shoulder. Clin Orthop Relat Res 1995;321:196–201. [PubMed] [Google Scholar]
- 11. Chaussy C, Schmiedt E, Jocham D, Brendel W, Forssmann B, Walther V. The use of shock waves for the destruction of renal calculi without direct contact. Urol Res 1976;4:175. [Google Scholar]
- 12. Hans-Ulrich Harten. Mechanische Schwingungen und Wellen. Physik für Mediziner, Berlin, Heidelberg: Springer-Lehrbuch, 2007:101–123. [Google Scholar]
- 13. International Electrotechnical Commission. IEC 61846. Ultrasonics – Pressure pulse lithotripters – Characteristics of fields. Edition 1.0. Geneva, Switzerland: International Electrotechnical Commission, 1998. [Google Scholar]
- 14. Wess OJ, Mayer J. Fragmentation of brittle material by shock wave lithotripsy. Momentum transfer and inertia: a novel view on fragmentation mechanisms. Urolithiasis 2018. December 6. doi: 10.1007/s00240-018-1102-6 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang FS, Yang KD, Kuo YR, et al. Temporal and spatial expression of bone morphogenetic proteins in extracorporeal shock wave-promoted healing of segmental defect. Bone 2003;32:387–396. [DOI] [PubMed] [Google Scholar]
- 16. Wang FS, Wang CJ, Chen YJ, et al. Ras induction of superoxide activates ERK-dependent angiogenic transcription factor HIF-1 and VEGF-A expression in shock wave-stimulated osteoblasts. J Biol Chem 2004;279:10331–10337. [DOI] [PubMed] [Google Scholar]
- 17. Ogden JA, Tóth-Kischkat A, Schultheiss R. Principles of shock wave therapy. Clin Orthop Relat Res 2001;387:8–17. [DOI] [PubMed] [Google Scholar]
- 18. Cheng JH, Wang CJ. Biological mechanism of shockwave in bone. Int J Surg 2015;24(Pt B):143–146. [DOI] [PubMed] [Google Scholar]
- 19. Fu M, Sun CK, Lin YC, et al. Extracorporeal shock wave therapy reverses ischemia-related left ventricular dysfunction and remodeling: molecular-cellular and functional assessment. PLoS One 2011;6:e24342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wang CJ, Huang CY, Hsu SL, Chen JH, Cheng JH. Extracorporeal shockwave therapy in osteoporotic osteoarthritis of the knee in rats: an experiment in animals. Arthritis Res Ther 2014;16:R139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Da Costa Gómez TM, Radtke CL, Kalscheur VL, et al. Effect of focused and radial extracorporeal shock wave therapy on equine bone microdamage. Vet Surg 2004;33:49–55. [DOI] [PubMed] [Google Scholar]
- 22. Yu L, Liu S, Zhao Z, et al. Extracorporeal shock wave rebuilt subchondral bone in vivo and activated Wnt5a/Ca2+ signaling in vitro. Biomed Res Int 2017;2017:1404650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Császár NB, Angstman NB, Milz S, et al. Radial shock wave devices generate cavitation. PLoS One 2015;10:e0140541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kearney CJ, Lee JY, Padera RF, Hsu HP, Spector M. Extracorporeal shock wave-induced proliferation of periosteal cells. J Orthop Res 2011;29:1536–1543. [DOI] [PubMed] [Google Scholar]
- 25. van der Jagt OP, van der, Linden JC, Schaden W, et al. Unfocused extracorporeal shock wave therapy as potential treatment for osteoporosis. J Orthop Res 2009;27:1528–1533. [DOI] [PubMed] [Google Scholar]
- 26. Koolen MKE, Kruyt MC, Zadpoor AA, Öner FC, Weinans H, van der Jagt OP. Optimization of screw fixation in rat bone with extracorporeal shock waves. J Orthop Res 2018;36:76–84. [DOI] [PubMed] [Google Scholar]
- 27. Rompe J-D, Kirkpatrick CJ, Küllmer K, Schwitalle M, Krischek O. Dose-related effects of shock waves on rabbit tendon Achillis. J Bone Joint Surg Br 1998;80:546–552. [DOI] [PubMed] [Google Scholar]
- 28. Rompe JD, Küllmer K, Vogel J, et al. Extrakorporale Stoßwellentherapie. Orthopade 1997;26:215–228. [DOI] [PubMed] [Google Scholar]
- 29. Zwerver J, Hartgens F, Verhagen E, van der Worp H, van den Akker-Scheek I, Diercks RL. No effect of extracorporeal shockwave therapy on patellar tendinopathy in jumping athletes during the competitive season: a randomized clinical trial. Am J Sports Med 2011;39:1191–1199. [DOI] [PubMed] [Google Scholar]
- 30. Durst HB, Blatter G, Kuster MS. Osteonecrosis of the humeral head after extracorporeal shock-wave lithotripsy. J Bone Joint Surg Br 2002;84:744–746. [DOI] [PubMed] [Google Scholar]
- 31. Valchanou VD, Michailov P. High energy shock waves in the treatment of delayed and nonunion of fractures. Int Orthop 1991;15:181–184. [DOI] [PubMed] [Google Scholar]
- 32. Böddeker R, Schäfer H, Haake M. Extracorporeal shockwave therapy (ESWT) in the treatment of plantar fasciitis: a biometrical review. Clin Rheumatol 2001;20:324–330. [DOI] [PubMed] [Google Scholar]
- 33. Beutler S, Regel G, Pape HC, et al. Die extrakorporale Stosswellentherapie (ESWT) in der Behandlung von Pseudarthrosen des Röhrenknochens. Erste Ergebnisse einer prospektivenklinischen Untersuchung. Unfallchirurg 1999;102:839–847. [DOI] [PubMed] [Google Scholar]
- 34. Biedermann R, Martin A, Handle G, Auckenthaler T, Bach C, Krismer M. Extracorporeal shock waves in the treatment of nonunions. J Trauma 2003;54:936–942. [DOI] [PubMed] [Google Scholar]
- 35. Warmuth M, Schumacher I, Biedermann R, Wild C. Systematischer review. Decision support document Nr. 62; 2012. Wien: Ludwig Boltzmann Institute for Health Technology Assessment. [Google Scholar]
- 36. Cacchio A, Giordano L, Colafarina O, Rompe JD, Tavernese E, Ioppolo F, Flamini S, Spacca G, Santilli V. Extracorporeal shock-wave therapy compared with surgery for hypertrophic long-bone nonunions. J Bone Joint Surg Am 2009;91:2589–2597. [DOI] [PubMed] [Google Scholar]
- 37. Furia JP, Juliano PJ, Wade AM, Schaden W, Mittermayr R. Shock wave therapy compared with intramedullary screw fixation fractures for nonunion of proximal fifth metatarsal metaphyseal-diaphyseal. J Bone Joint Surg Am 2010;92:846–854. [DOI] [PubMed] [Google Scholar]
- 38. Ludwig J, Lauber S, Lauber HJ, Dreisilker U, Raedel R, Hotzinger H. High-energy shock wave treatment of femoral head necrosis in adults. Clin Orthop Relat Res 2001;387:119–126. [DOI] [PubMed] [Google Scholar]
- 39. Alves EM, Angrisani AT, Santiago MB. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol 2009;28:1247–1251. [DOI] [PubMed] [Google Scholar]
- 40. Kong FR, Liang YJ, Qin SG, Li JJ, Li XL. [Clinical application of extracorporeal shock wave to repair and reconstruct osseous tissue framework in the treatment of avascular necrosis of the femoral head (ANFH)]. Zhongguo Gu Shang 2010;23:12–15. [PubMed] [Google Scholar]
- 41. Wang CJ, Wang FS, Huang CC, Yang KD, Weng LH, Huang HY. Treatment for osteonecrosis of the femoral head: comparison of extracorporeal shock waves with core decompression and bone-grafting. J Bone Joint Surg Am 2005;87:2380–2387. [DOI] [PubMed] [Google Scholar]
- 42. Wang CJ, Wang FS, Yang KD, et al. Treatment of osteonecrosis of the hip: comparison of extracorporeal shockwave with shockwave and alendronate. Arch Orthop Trauma Surg 2008;128:901–908. [DOI] [PubMed] [Google Scholar]
- 43. d’Agostino C, Romeo P, Lavanga V, Pisani S, Sansone V. Effectiveness of extracorporeal shock wave therapy in bone marrow edema syndrome of the hip. Rheumatol Int 2014;34:1513–1518. [DOI] [PubMed] [Google Scholar]
- 44. D’Agostino C, Romeo P, Amelio E, Sansone V. Effectiveness of ESWT in the treatment of Kienböck’s disease. Ultrasound Med Biol 2011;37:1452–1456. [DOI] [PubMed] [Google Scholar]
- 45. Moretti B, Notarnicola A, Moretti L, Giordano P, Patella V. A volleyball player with bilateral knee osteochondritis dissecans treated with extracorporeal shock wave therapy. Chir Organi Mov 2009;93:37–41. [DOI] [PubMed] [Google Scholar]
- 46. Marx S, Thiele R. Fallvorstellung der arthroskopisch kontrollierten Therapie der Osteochondrosis dissecans mittels ESWT. Arthroskopie 2003;16:266–271. [Google Scholar]
- 47. Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen: IQWiG-Bericht – Nr. 499: Extrakorporale Stoßwellentherapie beim Fersenschmerz – Abschlussbericht vom 29.03.2017. https://www.iqwig.de/download/N15-06_Extrakorporale-Sto%C3%9Fwellentherapie-beim-Fersenschmerz_Abschlussbericht_V1-0.pdf
- 48. Rompe JD, Buch M, Gerdesmeyer L, et al. Musculoskeletal shock wave therapy—current database of clinical research. Z Orthop Ihre Grenzgeb. 2002;140:267-274. [DOI] [PubMed] [Google Scholar]
- 49. Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, Forbes A. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA 2002;288:1364–1372. [DOI] [PubMed] [Google Scholar]
- 50. Abt T, Hopfenmüller W, Mellerowicz H. [Shock wave therapy for recalcitrant plantar fasciitis with heel spur: a prospective randomized placebo-controlled double-blind study]. Z Orthop Ihre Grenzgeb 2002;140:548–554. [DOI] [PubMed] [Google Scholar]
- 51. Gollwitzer H, Diehl P, von Korff A, Rahlfs VW, Gerdesmeyer L. Extracorporeal shock wave therapy for chronic painful heel syndrome: a prospective, double blind, randomized trial assessing the efficacy of a new electromagnetic shock wave device. J Foot Ankle Surg 2007;46:348–357. [DOI] [PubMed] [Google Scholar]
- 52. Kudo P, Dainty K, Clarfield M, Coughlin L, Lavoie P, Lebrun C. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res 2006;24:115–123. [DOI] [PubMed] [Google Scholar]
- 53. Rompe JD, Decking J, Schoellner C, Nafe B. Shock wave application for chronic plantar fasciitis in running athletes: a prospective, randomized, placebo-controlled trial. Am J Sports Med 2003;31:268–275. [DOI] [PubMed] [Google Scholar]
- 54. Rompe JD, Hopf C, Nafe B, Bürger R. Low-energy extracorporeal shock wave therapy for painful heel: a prospective controlled single-blind study. Arch Orthop Trauma Surg 1996;115:75–79. [DOI] [PubMed] [Google Scholar]
- 55. Tornese D, Mattei E, Lucchesi G, Bandi M, Ricci G, Melegati G. Comparison of two extracorporeal shock wave therapy techniques for the treatment of painful subcalcaneal spur: a randomized controlled study. Clin Rehabil 2008;22:780–787. [DOI] [PubMed] [Google Scholar]
- 56. Gerdesmeyer L, Frey C, Vester J, et al. Radial extracorporeal shock wave therapy is safe and effective in the treatment of chronic recalcitrant plantar fasciitis: results of a confirmatory randomized placebo-controlled multicenter study. Am J Sports Med 2008;36:2100–2109. [DOI] [PubMed] [Google Scholar]
- 57. Malay DS, Pressman MM, Assili A, et al. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg 2006;45:196–210. [DOI] [PubMed] [Google Scholar]
- 58. Alfredson H, Pietilä T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med 1998;26:360–366. [DOI] [PubMed] [Google Scholar]
- 59. Rompe JD, Furia J, Maffulli N. Exccentric loading compared with shock wave treatment for chronic insertional achilles tendinopathy: a RCT. J Bone Joint Surg Am 2008;90:52–61. [DOI] [PubMed] [Google Scholar]
- 60. Rompe JD, Nafe B, Furia JP, Maffulli N. Eccentric loading, shock-wave treatment, or a wait-and-see policy for tendinopathy of the main body of tendo Achillis: a randomized controlled trial. Am J Sports Med 2007;35:374–383. [DOI] [PubMed] [Google Scholar]
- 61. Costa ML, Shepstone L, Donell ST, Thomas TL. Shock wave therapy for chronic Achilles tendon pain: a randomized placebo-controlled trial. Clin Orthop Relat Res 2005;440:199–204. [DOI] [PubMed] [Google Scholar]
- 62. Furia JP. High-energy extracorporeal shock wave therapy as a treatment for insertional Achilles tendinopathy. Am J Sports Med 2006;34:733–740. [DOI] [PubMed] [Google Scholar]
- 63. Rasmussen S, Christensen M, Mathiesen I, Simonson O. Shockwave therapy for chronic Achilles tendinopathy: a double-blind, randomized clinical trial of efficacy. Acta Orthop 2008;79:249–256. [DOI] [PubMed] [Google Scholar]
- 64. Furia JP. High-energy extracorporeal shock wave therapy as a treatment for chronic noninsertional Achilles tendinopathy. Am J Sports Med 2008;36:502–508. [DOI] [PubMed] [Google Scholar]
- 65. Loew M, Jurgowski W, Mau HC, Thomsen M. Treatment of calcifying tendinitis of rotator cuff by extracorporeal shock waves: a preliminary report. J Shoulder Elbow Surg 1995;4:101–106. [DOI] [PubMed] [Google Scholar]
- 66. Daecke W, Kusnierczak D, Loew M. Der Einfluss der Applikationsdosis auf die Wirksamkeit der ESWA bei der Tendinosis calcarea der Schulter. Orthop Prax 1997;33:119–123. [Google Scholar]
- 67. Cacchio A, Paoloni M, Barile A, et al. Effectiveness of radial shock-wave therapy for calcific tendinitis of the shoulder: single-blind, randomized clinical study. Phys Ther 2006;86:672–682. [PubMed] [Google Scholar]
- 68. Albert JD, Meadeb J, Guggenbuhl P, et al. High-energy extracorporeal shock-wave therapy for calcifying tendinitis of the rotator cuff: a randomised trial. J Bone Joint Surg Br 2007;89:335–341. [DOI] [PubMed] [Google Scholar]
- 69. Sabeti-Aschraf M, Dorotka R, Goll A, Trieb K. Extracorporeal shock wave therapy in the treatment of calcific tendinitis of the rotator cuff. Am J Sports Med 2005;33:1365–1368. [DOI] [PubMed] [Google Scholar]
- 70. Ramon S, Gleitz M, Hernandez L, Romero LD. Update on the efficacy of extracorporeal shockwave treatment for myofascial pain syndrome and fibromyalgia. Int J Surg 2015;24:201–206. [DOI] [PubMed] [Google Scholar]