Abstract
Total knee arthroplasty (TKA) is a satisfactory procedure for end-stage knee joint pathology. However, there is a significant incidence of unsatisfied patients.
In recent years conventional total knee arthroplasty surgical technique has been challenged and a modern trend to respect individual anatomy, alignment and soft tissue laxities has been developed.
The indications, limits and outcomes of these modern techniques in selected patients are not well-defined.
Modern technology (navigation, patient-specific instrumentation and robotics) has improved accuracy of the osteotomies but their effect on long-term outcomes is still unclear.
A technique which respects individual anatomy, laxities and alignment in combination with an implant which is designed to incorporate contemporary knee kinematics, without the use of modern technology, is presented.
Cite this article: EFORT Open Rev 2020;5:663-671. DOI: 10.1302/2058-5241.5.190085
Keywords: alignment, anatomy, individualized surgical technique, laxities, total knee arthroplasty
Introduction
It is widely accepted that total knee arthroplasty (TKA) is a well-established reconstructive procedure for end-stage knee joint disorders and satisfactory survival rates have been reported at 15 years follow up.1–4 However, it has recently been reported that functional outcomes are inferior when compared with total hip arthroplasty and a significant incidence (up to 30%) of patients with objectively sound joints are dissatisfied with the procedure.5,6
The long-term outcome of TKA depends on several factors (Fig. 1). Conventional surgical techniques have recently been challenged due to patient dissatisfaction rates and several specialist surgeons have addressed modifications and improvements of techniques, often using experimental or expensive modern technology. Surprisingly, improvements are often introduced separately, and there is a lack of a unified system of an improved TKA technique for everyday practice which would take into consideration individual knee and patient characteristics.
Fig. 1.
Factors affecting long-term outcomes of total knee arthroplasty.
Knee laxity
The normal knee is a relative unstable joint which relies on both static and dynamic stabilizers for stability. Appropriate soft tissue tension in TKA is of paramount importance since incorrect tensioning can lead to either stiffness or instability.2,7
A normal knee has seven laxities. In simple practical terms, the medial compartment is stable in extension and flexion, the lateral compartment is looser in both extension (2–3 mm) and flexion (3–4 mm) when compared to the medial compartment, and the flexion gap is greater than the extension gap by 2–3 mm. However, there is a significant individual and gender variability.8–10 During TKA we do not really know whether the native knee balance is a reliable guide for TKA balance and normal contralateral knees are seldom available. One can argue that all the various tissues in an arthritic knee (cartilage, ligaments, bone and osteophytes) have sustained degenerative changes and restoration to pre-arthritic conditions is difficult. On the other hand, we understand the consequences of not restoring native knee balance.11 There are two scenarios: over-tightening of soft tissue restraints causing asymmetric gaps and abnormal knee kinematics, and increasing multiple knee laxities due to uncontrolled soft tissue releases leading to knee instability. Furthermore, non-native ligament tensions can be perceived by the patient as abnormal (due to proprioception) causing pain, stiffness and/or limited flexion and this may explain why abnormal pain pathways are commonly seen after TKA.10,12
The definition of the balanced knee and the optimal soft tissue balancing technique are still controversial.13 Babazadeh et al14 attempted to define a balanced TKA, but their estimation has so far proved far from what has been found in cadaveric studies.15 Soft tissue balancing can be achieved with the use of spacer blocks, laminar spreaders, tensioning devices and trial components. In order to improve accuracy, contemporary sensor technology has been developed.15–18 It has also recently been understood that optimal soft tissue balancing perhaps depends on the choice of the different existing alignment techniques and the kinematic design principle of the implant used.10,11,19,20
Knee alignment
Alignment is critical for the long-term survival of TKA and is relevant to the method of osteotomy.21,22 Alignment should be considered in three different planes (frontal, sagittal and transverse) and a surgeon should be able to recognize the lower limb mechanical axis, femoral and tibia bone anatomical and mechanical axes and the differences between dynamic and static loading conditions.19,21,22
In mechanical alignment, osteotomy in the frontal plane is designed in such a way that the mechanical axis falls upon the centre of the knee joint in order to reduce polyethylene wear and loosening.23 Mild varus is acceptable, valgus should be avoided and ankle alignment should be considered. This technique was introduced in the mid-1980s in order to create a biomechanically friendly artificial joint in line with the technical and mechanical features of the existing TKA designs of this period.23 However, it has been proven that this is a mechanical compromise and it is not natural due to the fact that there is great individual alignment variability. Axial alignment (transverse plane) of both components affects the extensor mechanism and range of motion. Since femoral component rotation is closely related to the medio-lateral gap in flexion, the concept of 3° of femoral component external rotation was introduced when osteotomies are performed following the measured resection technique in order to create rectangular extension and flexion gaps. In the sagittal plane, femoral component alignment is determined by implant-specific issues and there is no uniform technique. By contrast, tibial component alignment affects range of movement (especially flexion) and in most TKA systems is set to 3°. Hungerford et al24 presented the anatomical method (a mechanical alignment variant) in an attempt to establish a knee joint line parallel to the ground (frontal plane) while performing a varus osteotomy cut to the tibial plateau (2–3°) combined with an additional valgus osteotomy cut to the femur (3°). This technique has proven to be less reproducible due to the insufficient instrumentation of the mid-1980s.
The modern argument is that not all patients have the same lower limb mechanical axis and that there is a high individual variability in femoral external rotation and tibial posterior slope.25–32 The clinical relevance of this argument relies on the assumption that if you systematically align TKA to given degrees and angles in the three different planes, at least in theory, you can produce abnormal alignment and possibly a kinematic conflict in given individuals. Clinically, it has been shown that there are individuals with ‘constitutional varus’ limb alignment.25,26 During surgery, the restoration of their alignment to neutral is unnatural and results in greater strain in both collateral ligaments.25,26 Moreover, mild constitutional varus knees left in varus show better mid-term clinical and functional outcomes.11,19,25,30,33
A contemporary alternative to mechanical alignment is kinematic alignment.19,30-32,34 The goal is to restore the relative relationship of the femur, the patella and the tibia at any flexion angle without the application of force to the knee joint. If you achieve this, at least in principle, there is a reduction of the incidence of stiffness and instability, which results in early recovery and increased range of movement. The three principles of kinematic alignment are: restoration of the native tibial and femoral articular surfaces; restoration of the native knee and limb alignment; and restoration of the native laxities. An understanding of the three kinematic axes of the knee (flexion axis of the tibia, flexion axis of the patella and the longitudinal rotational axis of the knee) is crucial. These kinematic axes are closely parallel or perpendicular to the native tibial and femoral articular surfaces. In order to restore the native articular surfaces, the surgeon should co-align both components’ axes to the three kinematic axes of the knee. The technique is often performed using generic instrumentation. Possible component malalignment results in changes to the native femoral and tibial surfaces, which changes the native resting length of the collateral ligaments, retinacula and posterior cruciate ligament. This unnatural tightening or loosening of ligaments produces abnormal kinematics and the patient experiences pain, binding, stiffness or instability.11,19,30–32,34
On clinical grounds, based on quality level I and II studies, comparing early and mid-term outcomes of mechanical and kinematic alignment, no significant differences were found in terms of objective and subjective scores, complications or failures.35–38 On the other hand, earlier recovery and fewer unhappy patients were recorded in the kinematic alignment groups.35–38
It seems that kinematic alignment is not applicable to all patients (due to high individual anatomy and alignment variability); the indications and limits of this technique are unclear and several surgeons practice variants of these techniques in more severe cases. Rivière et al 32,34 reviewed existing alignment techniques and classified them into patient-specific, hybrid and systematic. Their differences rely on the degree of both femoral and tibial osteotomy angle, the use of computer-assisted techniques (navigation)39 or patient-specific instruments40,41 for performing the osteotomies and the amount of soft tissue releases. With the exception of kinematic alignment, all other techniques require a varying degree of soft tissue releases.
Osteotomies
Measured resection technique1,42
This technique is based on the anatomical concept (normal anatomy is preserved, the implant is similar to the anatomy and the bone resections have the same thickness as the implant). The majority of cruciate-retaining implants are implanted using this technique. Osteotomies are performed first, followed by soft tissue release and minor discrepancies in soft tissue balancing are tolerated. Osteotomies are performed based on three different femoral landmarks: the posterior condylar axis (PCA), the transepicondylar axis (TEA), and Whiteside’s line (Anteroposterior axis of the knee). TEA is traditionally thought to be the most reliable landmark for assessing femoral rotation, but this can be difficult to identify intra-operatively. All three landmarks should be identified when using a measured resection technique in TKA. Measured resection guides can be either anterior or posterior referencing. In anterior referencing systems, the anterior point is fixed to ensure that femoral component size changes will not take any additional bone anteriorly (avoiding notching) but when additional bone is removed from the posterior femoral condyles it may result in flexion instability. In posterior referencing systems, posterior femoral cuts are set when the jig is pinned into place and if a decrease in femoral component size is needed it will endanger anterior cortical notching. The use of the measured resection technique is restricted by wide individual anatomical variation.
Gap-balancing technique1,42
This technique is based on the functional concept (preservation of the kinematics of the implant, accurate soft tissue balancing, often sacrificing the anatomy). The majority of cruciate-sacrificing or substituting implants are implanted using this or a combination technique. Femoral osteotomies are performed after accurate soft tissue balancing, and discrepancies in soft tissue tension are not well tolerated. It requires the femoral component to be positioned parallel to the resected tibia, with both collateral ligaments tensioned. The surgeon balances either the flexion or extension gap first. The technique starts with a precise tibial cut and any deviation from the perpendicular will affect femoral component rotation. The gaps are balanced before posterior and anterior femoral resection, which includes removal of all osteophytes and soft tissue tensioning with a variety of distraction devices (the integrity of the collateral ligaments is important). Improved flexion stability has been demonstrated using this technique and less femoral condylar lift-off in flexion is produced compared with the measured resection technique. However, cutting the tibia into excessive varus or valgus will result in femoral component malrotation, and over resection of the distal femur will affect the level of the joint line and will lead to flexion gap balance discrepancies. Gap balancing has recently been criticized for not reproducing close-to-normal knee kinematics, especially with the use of TKA implants which incorporate contemporary knee kinematic principles.10,14,43–48
The recent use of navigation, robotics and patient-specific instrumentation has statistically significantly improved the accuracy of bone osteotomies as shown in high-quality randomized studies.41,49–53 However, the long-term effect on both objective and subjective outcomes is unclear. This is indicative of the multi-factorial nature of the surgical technique and other factors, such as individual alignment, soft tissue balancing and implant kinematics, may be equally important.
Kinematic implant design
Modern patients who undergo TKA are younger and more active. It has recently been recognized that more demanding activities require closer-to-normal kinematics in the artificial joint and sagittal stability which directly affects quadriceps efficiency.20,54–56 Moreover, one can argue that contemporary alignment techniques and restoring individual laxity, should be combined with the use of implants which incorporate contemporary knee kinematics.
Recent work on normal knee kinematics, including kinematics of cadaveric unloaded knees and unloaded and loaded knees in living subjects, has shown that the knee does not work as a crossed four-bar link as previously thought. Rather, the normal knee moves with the medial side staying very nearly stable like a ball-and-socket joint while the lateral side moves front to back, rotating around the centre of the medial side.57–59 Implants designed according to the four-bar link kinematic model had asymmetric multi-radius femoral components (80–90°’). These designs (either cruciate retaining or posterior cruciate sacrificing), although designed to exhibit a normal posterior roll-back in flexion, often slide anteriorly (paradoxical movement – sagittal buckling) due to loss of stabilizing structures and inadequate tibiofemoral congruity.57 The combination of contemporary knee kinematics with our modern understanding of the anatomy of the posterior femoral condyles60 and the axis of knee rotation61 led to the development of single radius femoral components (1980’) and constant radius (late 1990’) medial pivot designs with medially congruent polyethylene liners.20,56 Medial pivot designs from different manufacturers have shown sagittal stability and satisfactory long-term objective and subjective outcomes.3,62–66 A recent trend to use customized TKAs for selected patients has not yet gained support, mainly due to the premium cost of these implants.67
Individualized surgical technique
During pre-operative planning, in longstanding AP radiographs, individual alignment is recorded. Following the removal of osteophytes, minimal medial release is performed around the medial tibial plateau no more than 5–10 mm distal to the joint line. Proximal tibial osteotomy is performed first using an extramedullary or (preferably) intramedullary guide. Before osteotomy, the height from the less affected tibial plateau (Fig. 2), the native slope (Fig. 3) and the native varus (within the limits of 86-90° of tibial varus), (Fig. 4) are set. Then, based on the individual alignment (within the limits of 3–7° of femoral valgus), a distal femoral osteotomy is performed equivalent to the thickness of the femoral component (Fig. 5). The size of the implant is assessed using a combination (both anterior and posterior) referencing system. The native femoral rotation is estimated based on both the transepicondylar axis and Whiteside’s line and, if necessary, is further adjusted with a special jig (Fig. 6). Posterior bone resection equal to implant thickness (compensating for cartilage loss) is also performed (Fig. 7). The Evolution Medial Pivot (e-MP) TKA (MicroPort Orthopaedics Inc., Arlington, Tennessee), a motion-constrained design which incorporates contemporary kinematics, is used (Fig. 8). The femoral trial component establishes the centre of the medial femoral condyle (the centre of the ball) from which the momentary axis of knee rotation passes (Fig. 9).60,61 Then the tibial trial component with the socket-like medial compartment trial liner is inserted and the native tibial rotation is set following continuous flexion and extension movements. Finally, a trial test for stability is performed. The medial compartment should be stable in both extension and flexion, while lateral laxity of up to 2–3 mm in extension and 3–4 mm in flexion is allowed. In the case of a tight lateral compartment, progressive lateral soft tissue release is performed in both extension and flexion. Finally, a reproducible medial pivot effect with a posterior roll-back ensures the quality of soft tissue balancing.
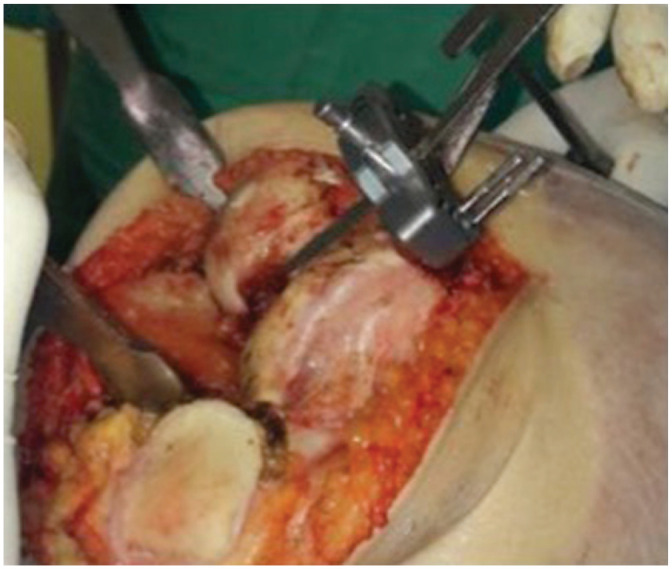
Fig. 2.
The height of the proximal tibial osteotomy is set from the least affected side.
Fig. 3.
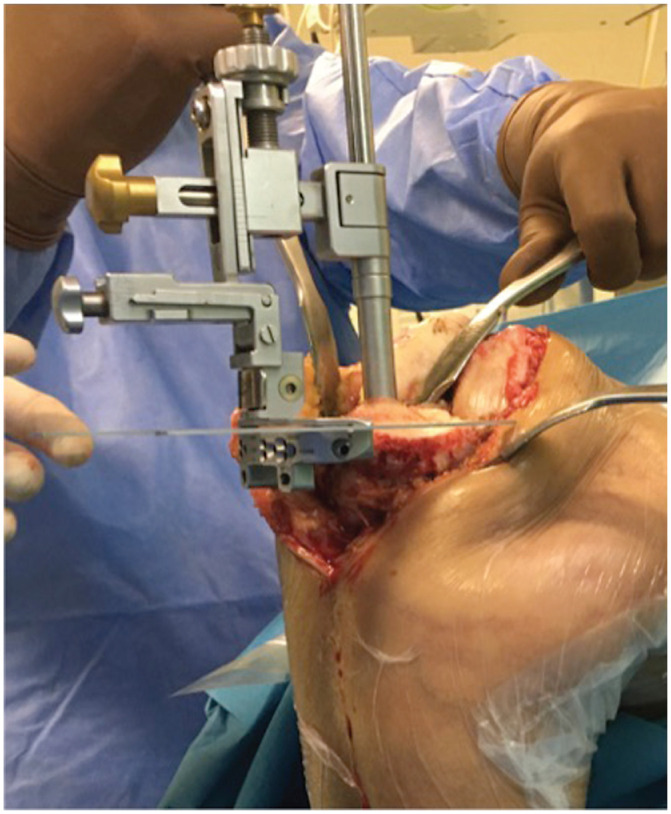
Setting of the native posterior slope is shown.
Fig. 4.
Setting of the ‘native’ varus is shown.
Fig. 5.
The level of the distal femoral resection (equivalent to femoral component thickness) is shown.
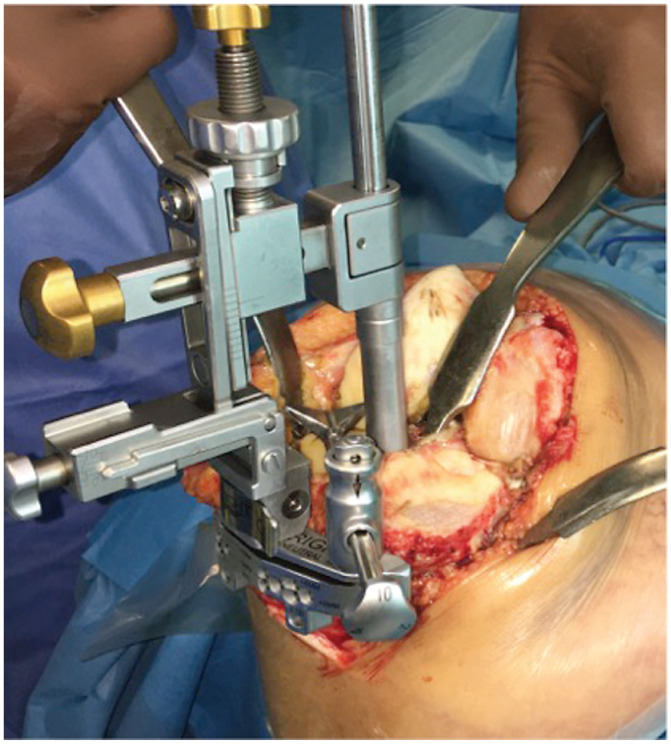
Fig. 6.
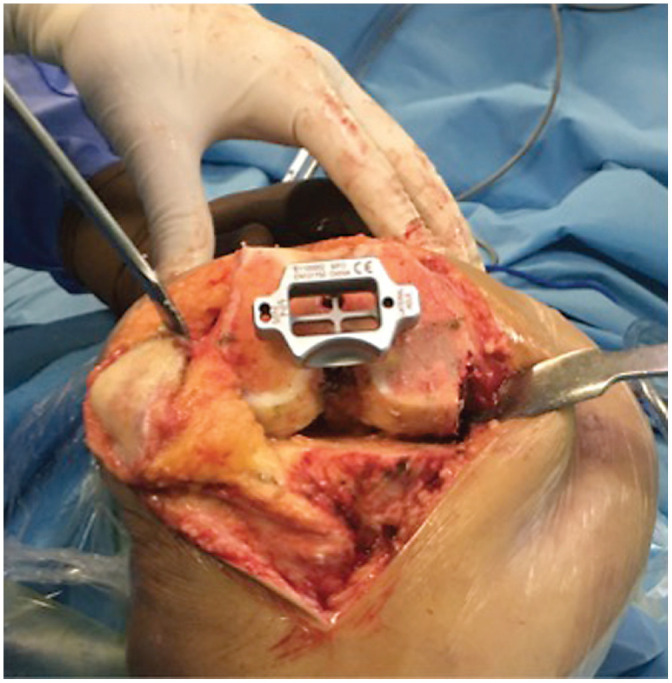
Setting of the ‘native’ femoral rotation.
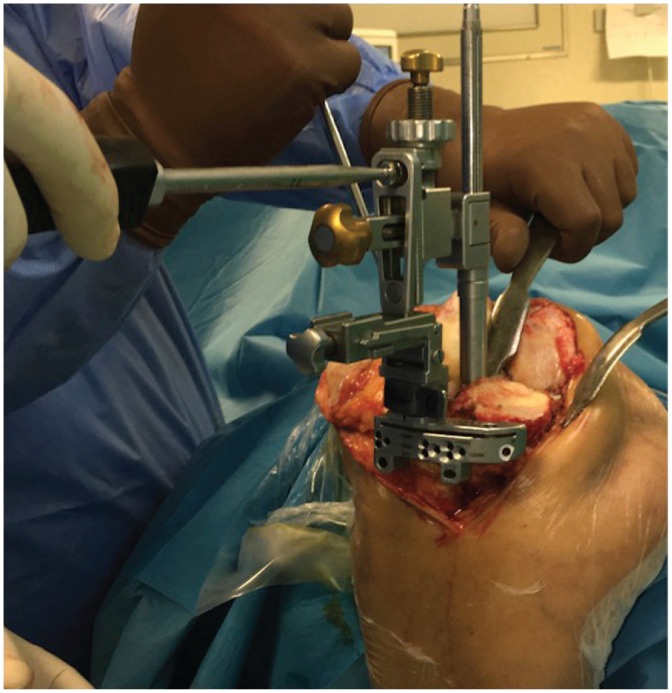
Fig. 7.
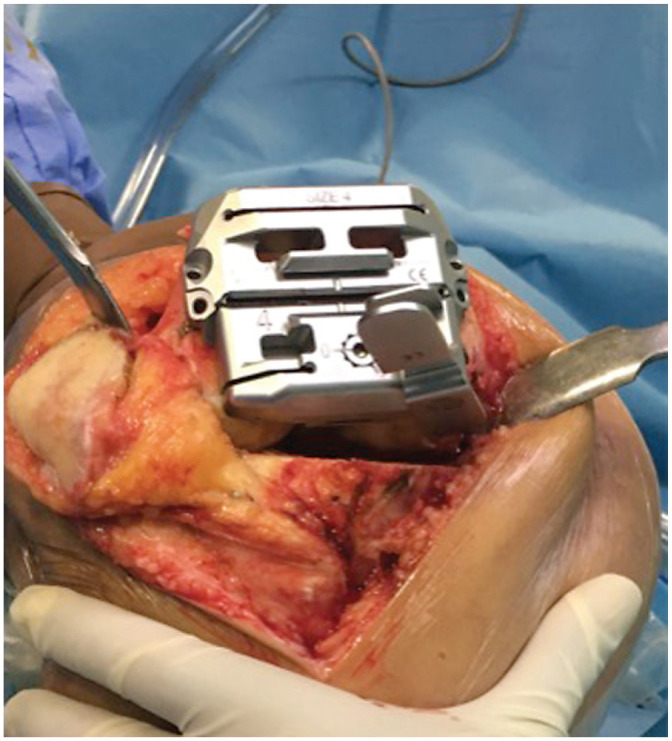
The level of the posterior condyles resection (equivalent to femoral component thickness) is shown.
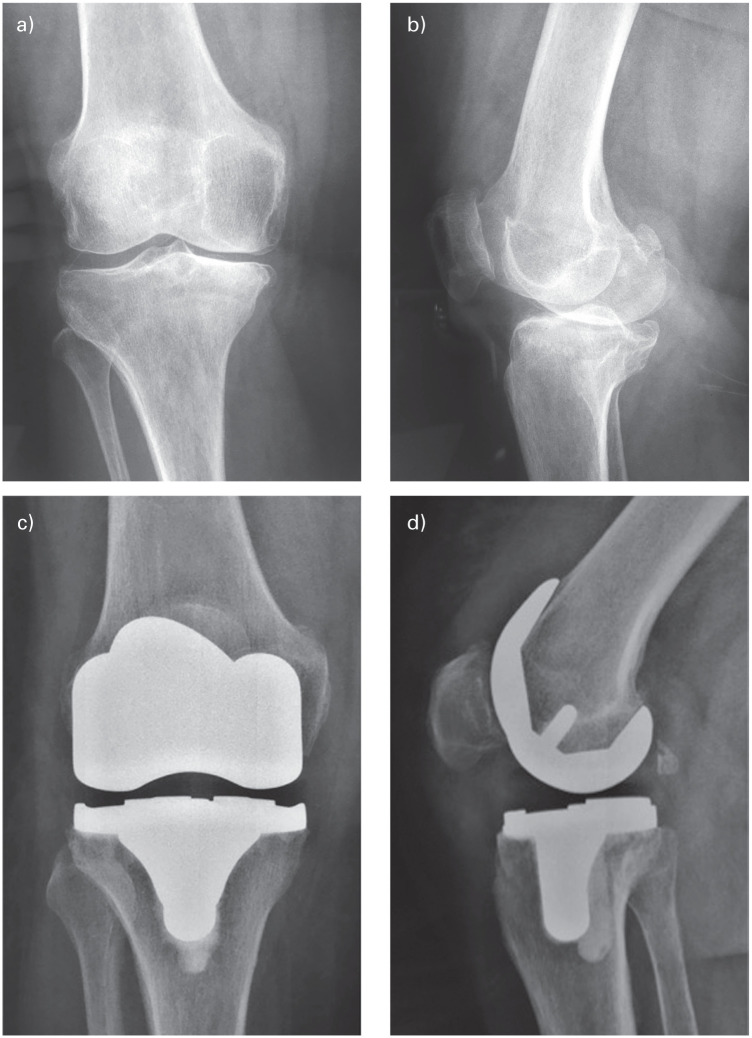
Fig. 8.
Anteroposterior (a) and lateral (b) pre-operative osteoarthritic knee radiographs. Anteroposterior (c) and lateral (d) knee radiographs showing an Evolution Medial Pivot total knee arthroplasty at four years follow up.
Fig. 9.
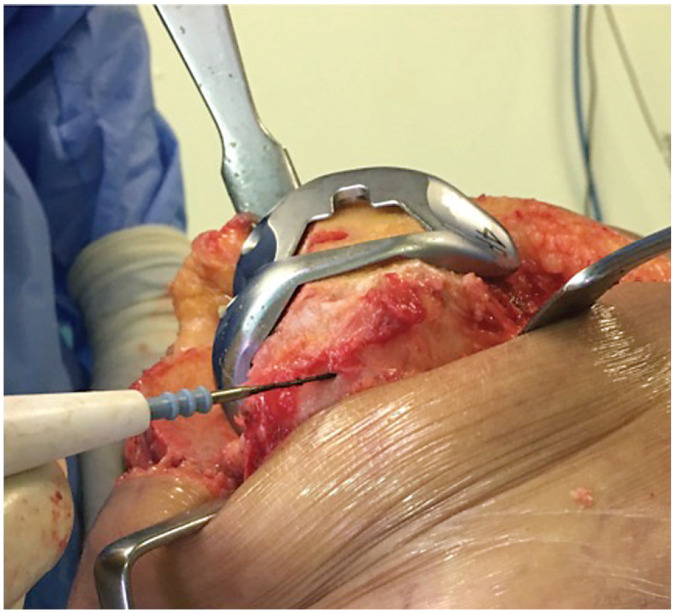
The trial femoral component sets the centre of the medial ball (equivalent to the passing point of the momentary axis of knee rotation through the medial femoral condyle).
Over the last 20 years we have progressively developed the above technique and published satisfactory long-term outcomes using initially the Advance (a-MP) and now the Evolution (e-MP) Medial Pivot TKA designs (MicroPort Orthopaedics Inc., Arlington, Tennessee).3,62 More than 80% of our cases are performed using the above method. For patients with gross deviations from the average anatomy and laxity and in cases of more than 20° of valgus or varus deformity, one should be sceptical about applying this technique, and perhaps in these cases mechanical alignment with more constrained implants is more appropriate.
Footnotes
ICMJE Conflict of interest statement: TK reports consultancy for Microport Orthopaedics; expert testimony for Microport Orthopaedics and Smith & Nephew; grants/grants pending from Microport Orthopaedics, Smith & Nephew and Amgen; payment for lectures/services on speakers’ bureaus from Microport Orthopaedics; and travel/accommodation/meeting expenses from Microport Orthopaedics and Amgen, all outside the submitted work.
GAK declares no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Sheth NP, Husain A, Nelson CL. Surgical techniques for total knee arthroplasty: measured resection, gap balancing, and hybrid. J Am Acad Orthop Surg 2017;25:499–508. [DOI] [PubMed] [Google Scholar]
- 2. Le DH, Goodman SB, Maloney WJ, Huddleston JI. Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop Relat Res 2014;472:2197–2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Karachalios Th, Varitimidis S, Bargiotas K, Hantes M, Roidis N, Malizos KN. An 11- to 15-year clinical outcome study of the Advance Medial Pivot total knee arthroplasty: pivot knee arthoplasty. Bone Joint J 2016;98-B:1050–1055. [DOI] [PubMed] [Google Scholar]
- 4. Papasoulis E, Karachalios Th. A 13- to 16-year clinical and radiological outcome study of genesis II cruciate retaining total knee arthroplasty with oxidised zirconium femoral component. Knee 2019;26:492–499. [DOI] [PubMed] [Google Scholar]
- 5. Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 2014;96-B:96–100. [DOI] [PubMed] [Google Scholar]
- 6. Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 2015;97-B:793–801. [DOI] [PubMed] [Google Scholar]
- 7. Verstraete MA, Meere PA, Salvadore G, Victor J, Walker PS. Contact forces in the tibiofemoral joint from soft tissue tensions: implications to soft tissue balancing in total knee arthroplasty. J Biomech 2017;58:195–202. [DOI] [PubMed] [Google Scholar]
- 8. Deep K. Collateral ligament laxity in knees: what is normal? Clin Orthop Relat Res 2014;472:3426–3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Deep K, Picard F, Clarke JV. Dynamic knee alignment and collateral knee laxity and its variations in normal humans. Front Surg 2015;2:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roth JD, Howell SM, Hull ML. Native knee laxities at 0°, 45°, and 90° of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Joint Surg Am 2015;97:1678–1684. [DOI] [PubMed] [Google Scholar]
- 11. Gu Y, Roth JD, Howell SM, Hull ML. How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? J Bone Joint Surg Am 2014;96:e101. [DOI] [PubMed] [Google Scholar]
- 12. Wylde V, Beswick A, Bruce J, Blom A, Howells N, Gooberman-Hill R. Chronic pain after total knee arthroplasty. EFORT Open Rev 2018;3:461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Walker LC, Clement ND, Ghosh KM, Deehan DJ. What is a balanced knee replacement? EFORT Open Rev 2018;3:614–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Babazadeh S, Stoney JD, Lim K, Choong PF. The relevance of ligament balancing in total knee arthroplasty: how important is it? A systematic review of the literature. Orthop Rev (Pavia) 2009;1:e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nowakowski AM, Majewski M, Müller-Gerbl M, Valderrabano V. Development of a force-determining tensor to measure ‘physiologic knee ligament gaps’ without bone resection using a total knee arthroplasty approach. J Orthop Sci 2011;16:56–63. [DOI] [PubMed] [Google Scholar]
- 16. Gustke KA, Golladay GJ, Roche MW, Elson LC, Anderson CR. A targeted approach to ligament balancing using kinetic sensors. J Arthroplasty 2017;32:2127–2132. [DOI] [PubMed] [Google Scholar]
- 17. ten Ham AM, Heesterbeek PJC, van der Schaaf DB, Jacobs WCH, Wymenga AB. Flexion and extension laxity after medial, mobile-bearing unicompartmental knee arthroplasty: a comparison between a spacer- and a tension-guided technique. Knee Surg Sports Traumatol Arthrosc 2013;21:2447–2452. [DOI] [PubMed] [Google Scholar]
- 18. Chow JC, Breslauer L. The use of intraoperative sensors significantly increases the patient-reported rate of improvement in primary total knee arthroplasty. Orthopedics 2017;40:e648–e651. [DOI] [PubMed] [Google Scholar]
- 19. Howell SM, Hull ML. Kinematic alignment in total knee arthroplasty. In: Norman Scott W. Insall and Scott surgery of the knee. 5th ed London: Churchill Livingston, 2011:1255–1269. [Google Scholar]
- 20. Blaha JD. The rationale for a total knee implant that confers anteroposterior stability throughout range of motion. J Arthroplasty 2004;19:22–26. [DOI] [PubMed] [Google Scholar]
- 21. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 2010;92:2143–2149. [DOI] [PubMed] [Google Scholar]
- 22. Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA. Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med 2014;7:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res 1985;192:13–22. [PubMed] [Google Scholar]
- 24. Hungerford DS, Kenna RV, Krackow KA. The porous-coated anatomic total knee. Orthop Clin North Am 1982;13:103–122. [PubMed] [Google Scholar]
- 25. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat Award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 2012;470:45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Victor JM, Bassens D, Bellemans J, Gürsu S, Dhollander AA, Verdonk PC. Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 2014;472:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Victor J. Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res 2009;95:365–372. [DOI] [PubMed] [Google Scholar]
- 28. Ahmad R, Patel A, Mandalia V, Toms A. Posterior tibial slope: effect on, and interaction with, knee kinematics. JBJS Rev 2016;4:e31–e36. [DOI] [PubMed] [Google Scholar]
- 29. Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res 1990;255:215–227. [PubMed] [Google Scholar]
- 30. Howell SM, Hull ML. Kinematic alignment in total knee arthroplasty. Definition, history, principle, surgical technique, and results of an alignment option for TKA. Arthropaedia 2014;1:44–53. [Google Scholar]
- 31. Lee YS, Howell SM, Won YY, et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:3467–3479. [DOI] [PubMed] [Google Scholar]
- 32. Rivière C, Iranpour F, Auvinet E, et al. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 2017;103:1047–1056. [DOI] [PubMed] [Google Scholar]
- 33. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 2013;21:2325–2330. [DOI] [PubMed] [Google Scholar]
- 34. Rivière C, Lazic S, Boughton O, Wiart Y, Vïllet L, Cobb J. Current concepts for aligning knee implants: patient-specific or systematic? EFORT Open Rev 2018;3:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD. The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Joint J 2016;98-B:1360–1368. [DOI] [PubMed] [Google Scholar]
- 36. Young SW, Walker ML, Bayan A, Briant-Evans T, Pavlou P, Farrington B. The Chitranjan S. Ranawat Award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res 2017;475:9–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J 2017;99-B:640–646. [DOI] [PubMed] [Google Scholar]
- 38. Courtney PM, Lee GC. Early outcomes of kinematic alignment in primary total knee arthroplasty: a meta-analysis of the literature. J Arthroplasty 2017;32:2028–2032.e1. [DOI] [PubMed] [Google Scholar]
- 39. Hutt JR, LeBlanc MA, Massé V, Lavigne M, Vendittoli PA. Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res 2016;102:99–104. [DOI] [PubMed] [Google Scholar]
- 40. Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli PA. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplasty 2017;32:2133–2140. [DOI] [PubMed] [Google Scholar]
- 41. Calliess T, Bauer K, Stukenborg-Colsman C, et al. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2017; 25(6):1743–1748. [DOI] [PubMed] [Google Scholar]
- 42. Jaffe WL, Dundon JM, Camus T. Alignment and balance methods in total knee arthroplasty. J Am Acad Orthop Surg 2018;26:709–716. [DOI] [PubMed] [Google Scholar]
- 43. Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 2010;468:102–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Luyckx T, Peeters T, Vandenneucker H, Victor J, Bellemans J. Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? J Bone Joint Surg Br 2012;94:1271–1276. [DOI] [PubMed] [Google Scholar]
- 45. Daines BK, Dennis DA. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 2014;6:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Risitano S, Indelli PF. Is ‘symmetric’ gap balancing still the gold standard in primary total knee arthroplasty? Ann Transl Med 2017;5:325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Matsuda S, Ito H. Ligament balancing in total knee arthroplasty: medial stabilizing technique. Asia Pac J Sports Med Arthrosc Rehabil Technol 2015;2:108–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McEwen P, Balendra G, Doma K. Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Joint J 2019;101-B:331–339. [DOI] [PubMed] [Google Scholar]
- 49. Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 2009;24:560–569. [DOI] [PubMed] [Google Scholar]
- 50. Barrett WP, Mason JB, Moskal JT, Dalury DF, Oliashirazi A, Fisher DA. Comparison of radiographic alignment of imageless computer-assisted surgery vs conventional instrumentation in primary total knee arthroplasty. J Arthroplasty 2011;26:1273–1284.e1. [DOI] [PubMed] [Google Scholar]
- 51. Xie C, Liu K, Xiao L, Tang R. Clinical outcomes after computer-assisted versus conventional total knee arthroplasty. Orthopedics 2012;35:e647–e653. [DOI] [PubMed] [Google Scholar]
- 52. Sassoon A, Nam D, Nunley R, Barrack R. Systematic review of patient-specific instrumentation in total knee arthroplasty: new but not improved. Clin Orthop Relat Res 2015;473:151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bautista M, Manrique J, Hozack WJ. Robotics in total knee arthroplasty. J Knee Surg 2019;32:600–606. [DOI] [PubMed] [Google Scholar]
- 54. Mugnai R, Digennaro V, Ensini A, Leardini A, Catani F. Can TKA design affect the clinical outcome? Comparison between two guided-motion systems. Knee Surg Sports Traumatol Arthrosc 2014;22:581–589. [DOI] [PubMed] [Google Scholar]
- 55. Meng F, Jaeger S, Sonntag R, Schroeder S, Smith-Romanski S, Kretzer JP. How prosthetic design influences knee kinematics: a narrative review of tibiofemoral kinematics of healthy and joint-replaced knees. Expert Rev Med Devices 2019;16:119–133. [DOI] [PubMed] [Google Scholar]
- 56. Ng JWG, Bloch BV, James PJ. Sagittal radius of curvature, trochlea design and ultracongruent insert in total knee arthroplasty. EFORT Open Rev 2019;4:519–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Coles LG, Gheduzzi S, Miles AW, Gill HS. Kinematics of the natural and replaced knee. In: Karachalios T, ed. Total knee arthroplasty: long term outcomes. London: Springer-Verlag, 2015:7–20. [Google Scholar]
- 58. Iwaki H, Pinskerova V, Freeman MAR. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 2000;82:1189–1195. [DOI] [PubMed] [Google Scholar]
- 59. Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MAR. Tibiofemoral movement 2: the loaded and unloaded living knee studies by MRI. J Bone Joint Surg Br 2001;82A:1196–1198. [DOI] [PubMed] [Google Scholar]
- 60. Eckhoff D, Hogan C, Dimatteo L, Robinson M, Bach J. Difference between the epicondylar and cylindrical axis of the knee. ABJS best papers. Clin Orthop Relat Res 2007;461:238–244. [DOI] [PubMed] [Google Scholar]
- 61. Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res 1993;290:259–268. [PubMed] [Google Scholar]
- 62. Karachalios T, Roidis N, Giotikas D, Bargiotas K, Varitimidis S, Malizos KN. A mid-term clinical outcome study of the Advance Medial Pivot knee arthroplasty. Knee 2009;16:484–488. [DOI] [PubMed] [Google Scholar]
- 63. Fitch DA, Sedacki K, Yang Y. Mid- to long-term outcomes of a medial-pivot system for primary total knee replacement: a systematic review and meta-analysis. Bone Joint Res 2014;3:297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. McMahon S, Scott G. A brief follow-up report on 228 medial rotation total knee replacements at a mean of 8.5 years (0–9). Int J Clin Med 2015;6:928–933. [Google Scholar]
- 65. Macheras GA, Galanakos SP, Lepetsos P, Anastasopoulos PP, Papadakis SA. A long term clinical outcome of the Medial Pivot Knee Arthroplasty System. Knee 2017;24:447–453. [DOI] [PubMed] [Google Scholar]
- 66. Benjamin B, Pietrzak JRT, Tahmassebi J, Haddad FS. A functional comparison of medial pivot and condylar knee designs based on patient outcomes and parameters of gait. Bone Joint J 2018;100-B:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Schwechter EM, Fitz W. Design rationale for customized TKA: a new idea or revisiting the past? Curr Rev Musculoskelet Med 2012;5:303–308. [DOI] [PMC free article] [PubMed] [Google Scholar]